Dental Students’ Oral Health-Related Quality of Life and Temporomandibular Dysfunction-Self-Rating versus Clinical Assessment
Abstract
:1. Introduction
2. Material and Methods
2.1. Ethics Approval and Trial Registration
2.2. Subjects
2.3. Clinical Parameters and Data Acquisition
2.4. Statistical Analysis
3. Results
3.1. Sample Sharacteristics
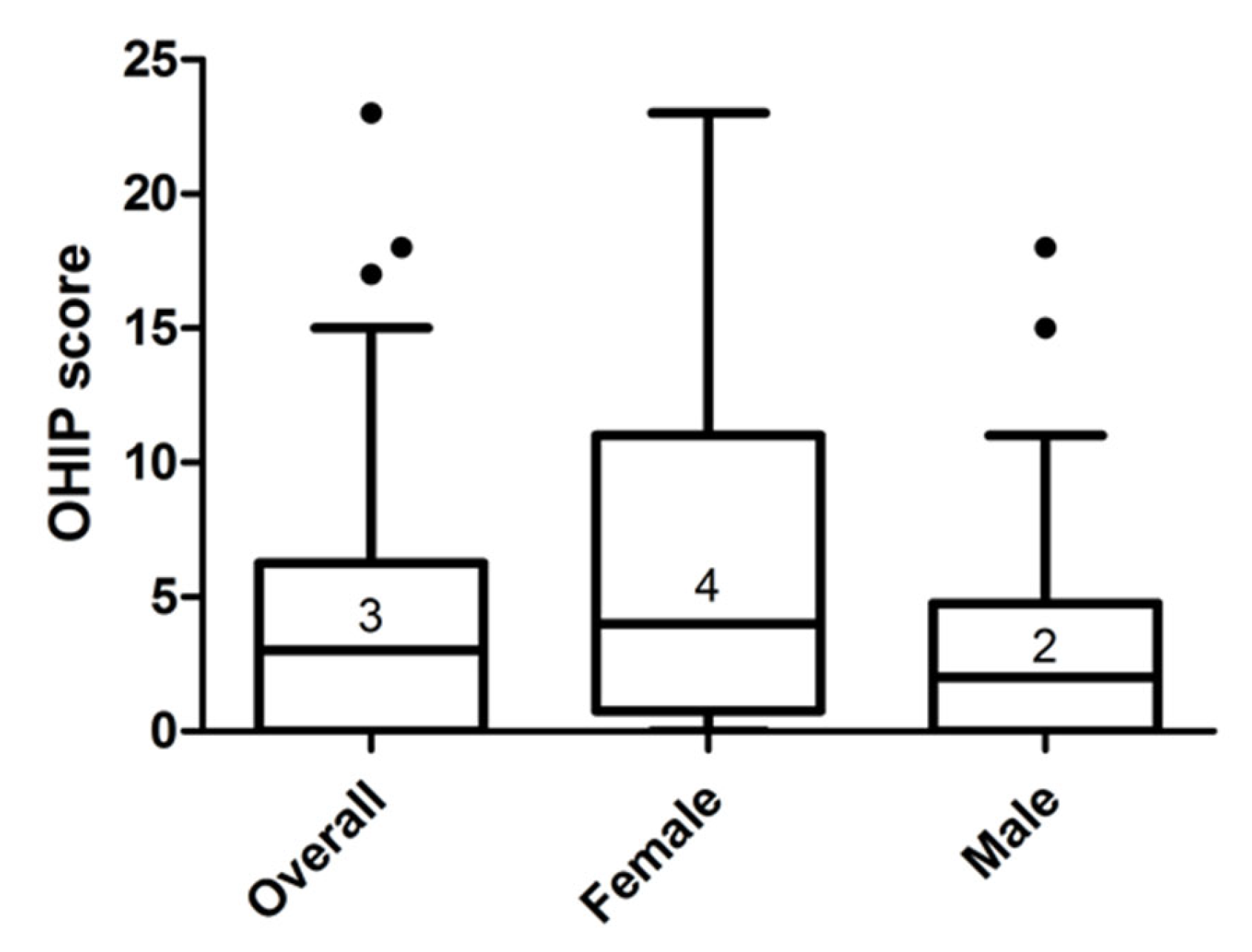
3.2. Oral Health Impact Profile-German-14
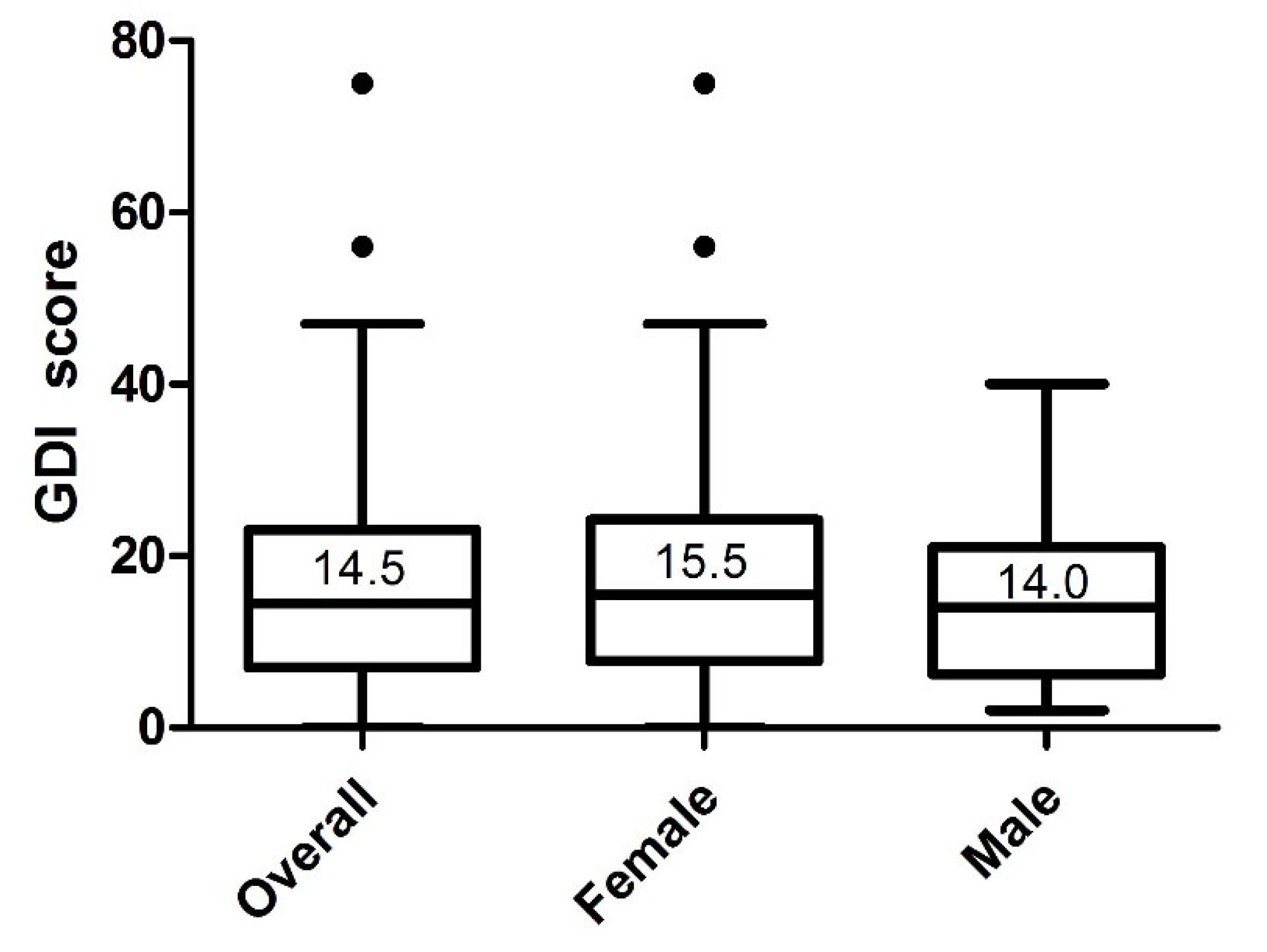
3.3. Graz Dysfunction Index
4. Discussion
4.1. Main Results and Comparison with Other Studies
4.2. Advantages and Disadvantages of the Study
4.3. Clinical Relevance
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Humphris, G.; Blinkhorn, A.; Freeman, R.; Gorter, R.; Hoad-Reddick, G.; Murtomaa, H.; O’Sullivan, R.; Splieth, C. Psychological stress in undergraduate dental students: Baseline results from seven European dental schools. Eur. J. Dent. Educ. 2002, 6, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Polychronopoulou, A.; Divaris, K. Dental students’ perceived sources of stress: A multi-country study. J Dent. Educ. 2009, 73, 631–639. [Google Scholar] [CrossRef]
- Gorter, R.; Freeman, R.; Hammen, S.; Murtomaa, H.; Blinkhorn, A.; Humphris, G. Psychological stress and health in undergraduate dental students: Fifth year outcomes compared with first year baseline results from five European dental schools. Eur. J. Dent. Educ. 2008, 12, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Divaris, K.; Mafla, A.C.; Villa-Torres, L.; Sánchez-Molina, M.; Gallego-Gómez, C.L.; Vélez-Jaramillo, L.F.; Tamayo-Cardona, J.A.; Pérez-Cepeda, D.; Vergara-Mercado, M.L.; Simancas-Pallares, M.Á.; et al. Psychological distress and its correlates among dental students: A survey of 17 Colombian dental schools. BMC Med. Educ. 2013, 13, 91. [Google Scholar] [CrossRef] [Green Version]
- Wieckiewicz, M.; Grychowska, N.; Wojciechowski, K.; Pelc, A.; Augustyniak, M.; Sleboda, A.; Zietek, M. Prevalence and correlation between TMD based on RDC/TMD diagnoses, oral parafunctions and psychoemotional stress in Polish university students. Biomed. Res. Int. 2014, 2014, 472346. [Google Scholar] [CrossRef]
- Rocha, C.O.; Peixoto, R.F.; Resende, C.M.; Alves, A.C.; Oliveira, Â.G.; Barbosa, G.A. Psychosocial aspects and temporomandibular disorders in dental students. Quintessence Int. 2014, 48, 241–249. [Google Scholar]
- Ahuja, V.; Ranjan, V.; Passi, D.; Jaiswal, R. Study of stress-induced temporomandibular disorders among dental students: An institutional study. Natl. J. Maxillofac. Surg. 2018, 9, 147–154. [Google Scholar]
- Chuang, S.Y. Incidence of temporomandibular disorders (TMDs) in senior dental students in Taiwan. J. Oral Rehabil. 2002, 29, 1206–1211. [Google Scholar] [CrossRef] [PubMed]
- Karthik, R.; Hafila, M.I.F.; Saravanan, C.; Vivek, N.; Priyadarsini, P.; Ashwath, B. Assessing Prevalence of Temporomandibular Disorders among University Students: A Questionnaire Study. J. Int. Soc. Prev. Community Dent. 2017, 7, S24–S29. [Google Scholar]
- John, M.T.; Reissmann, D.R.; Schierz, O.; Wassell, R.W. Oral health-related quality of life in patients with temporomandibular disorders. J. Orofac. Pain. 2007, 21, 46–54. [Google Scholar]
- Bitiniene, D.; Zamaliauskiene, R.; Kubilius, R.; Leketas, M.; Gailius, T.; Smirnovaite, K. Quality of life in patients with temporomandibular disorders. A systematic review. Stomatologija 2018, 20, 3–9. [Google Scholar]
- Slade, G.D.; Spencer, A.J. Development and evaluation of the Oral Health Impact Profile. Community Dent. Health. 1994, 11, 3–11. [Google Scholar] [PubMed]
- Hanna, K.; Nair, R.; Amarasena, N.; Armfield, J.M.; Brennan, D.S. Temporomandibular dysfunction experience is associated with oral health-related quality of life: An Australian national study. BMC Oral Health. 2021, 21, 432. [Google Scholar] [CrossRef]
- Lei, J.; Yap, A.U.; Zhang, M.; Fu, K.Y. Temporomandibular disorder subtypes, emotional distress, impaired sleep, and oral health-related quality of life in Asian patients. Community Dent. Oral Epidemiol. 2021. [Google Scholar] [CrossRef]
- Yap, A.U.; Marpaung, C.; Rahmadini, E.D. Self-reported symptoms of temporomandibular disorders: Relationship to psychological wellbeing, psychological distress, and oral health-related quality of life. Int. J. Prosthodont. 2021. [Google Scholar] [CrossRef]
- Onoda, N.; Mikami, T.; Saito, N.; Kobayashi, T. Evaluation of oral health-related quality of life in patients with temporomandibular disorders. Cranio 2021. [Google Scholar] [CrossRef]
- Brogårdh-Roth, S.; Paulsson, L.; Larsson, P.; Ekberg, E. Do preterm-born adolescents have a poorer oral health-related quality of life? BMC Oral Health. 2021, 21, 440. [Google Scholar] [CrossRef]
- Karaman, A.; Sapan, Z. Evaluation of temporomandibular disorders, quality of life, and oral habits among dentistry students. Cranio 2020. [Google Scholar] [CrossRef] [PubMed]
- Locker, D. Measuring oral health: A conceptual framework. Community Dent. Health. 1988, 5, 3–18. [Google Scholar]
- Slade, G.D. Derivation and validation of a short-form oral health impact profile. Community Dent. Oral Epidemiol. 1997, 25, 284–290. [Google Scholar] [CrossRef] [PubMed]
- John, M.T.; Miglioretti, D.L.; LeResche, L.; Koepsell, T.D.; Hujoel, P.; Micheelis, W. German short forms of the Oral Health Impact Profile. Community Dent. Oral Epidemiol. 2006, 34, 277–288. [Google Scholar] [CrossRef]
- John, M.T.; Micheelis, W.; Biffar, R. Reference values in oral health-related quality of life for the abbreviated version of the Oral Health Impact Profile. Schweiz. Monatsschr. Zahnmed. 2004, 114, 784–791. [Google Scholar]
- Riegler, H.; Haas, M. Der Grazer Dysfunktionsindex—Eine Methode zur Einschätzung des Funktionszustandes im stomatognathen System. Stomatologie 1995, 7, 371–383. [Google Scholar]
- Lin, L.I. A concordance correlation coefficient to evaluate reproducibility. Biometrics 1989, 45, 255–268. [Google Scholar] [CrossRef]
- Müller, R.; Büttner, P. A critical discussion of intraclass correlation coefficients. Stat. Med. 1994, 13, 2465–2476. [Google Scholar] [CrossRef] [PubMed]
- Magnusson, T.; Egermark, I.; Carlsson, G.E. A longitudinal epidemiologic study of signs and symptoms of temporomandibular disorders from 15 to 35 years of age. J. Orofac. Pain. 2000, 14, 310–319. [Google Scholar] [PubMed]
- Helkimo, M. Studies on function and dysfunction of the masticatory system. IV. Age and sex distribution of symptoms of dysfunction of the masticatory system in Lapps in the north of Finland. Acta Odontol. Scand. 1974, 32, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Yamane-Takeuchi, M.; Ekuni, D.; Mizutani, S.; Kataoka, K.; Taniguchi-Tabata, A.; Azuma, T.; Furuta, M.; Tomofuji, T.; Iwasaki, Y.; Morita, M. Associations among oral health-related quality of life, subjective symptoms, clinical status, and self-rated oral health in Japanese university students: A cross-sectional study. BMC Oral Health. 2016, 16, 127. [Google Scholar] [CrossRef] [Green Version]
- Natu, V.P.; Yap, A.U.; Su, M.H.; Irfan Ali, N.M.; Ansari, A. Temporomandibular disorder symptoms and their association with quality of life, emotional states and sleep quality in South-East Asian youths. J. Oral Rehabil. 2018, 45, 756–763. [Google Scholar] [CrossRef] [PubMed]
- Dworkin, S.F.; LeResche, L. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique. J. Craniomandib. Disord. 1992, 6, 301–355. [Google Scholar]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Gabler, M.; Reiber, T.H.; John, M. Die mehrdimensionale Charakterisierung einer Patientenpopulation mit kraniomandibulären Dysfunktionen. Dtsch. Zahnärztliche Z. 2001, 56, 332–334. [Google Scholar]
- Helkimo, M. Studies on function and dysfunction of the masticatory system. II. Index for anamnestic and clinical dysfunction and occlusal state. Sven. Tandlak. Tidskr. 1974, 67, 101–121. [Google Scholar]
- Dyrbye, L.N.; Thomas, M.R.; Shanafelt, T.D. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad. Med. 2006, 81, 354–373. [Google Scholar] [CrossRef]
- Hope, V.; Henderson, M. Medical student depression, anxiety and distress outside North America: A systematic review. Med. Educ. 2014, 48, 963–979. [Google Scholar] [CrossRef] [PubMed]
- Mechanic, D. Social psychologic factors affecting the presentation of bodily complaints. N. Engl. J. Med. 1972, 286, 1132–1139. [Google Scholar] [CrossRef] [PubMed]
- Azuri, J.; Ackshota, N.; Vinker, S. Reassuring the medical students’ disease--health related anxiety among medical students. Med. Teach. 2010, 32, e270–e275. [Google Scholar] [CrossRef] [PubMed]
- Waterman, L.Z.; Weinman, J.A. Medical student syndrome: Fact or fiction? A cross-sectional study. JRSM Open. 2014, 5, 2042533313512480. [Google Scholar] [CrossRef] [PubMed]
| Graz Dysfunction Index Score | |||
|---|---|---|---|
| Gender | Females (n = 38) | Males (n = 36) | p-Value * |
| Anamnesis and inspection | 4 (4–6) | 4 (2.5–8) | 0.93 |
| Pain | 0 (0–0) | 0 (0–0) | 0.09 |
| Joint mobility | 4 (0–7) | 3 (0–6) | 0.42 |
| Joint noise | 0.5 (0–8) | 0 (0–8.5) | 0.68 |
| Occlusion | 1.5 (0–5) | 1 (0–3) | 0.78 |
| Muscle pain on palpation | 0 (0–1.25) | 0 (0–0) | 0.22 |
| Dysfunction Group | Total | ||||
|---|---|---|---|---|---|
| Normal Function | Adaptation | CompenSation | DysFunction | ||
| Males, n (%) | 21 (58.3) | 14 (38.9) | 1 (2.8) | 0 (0) | 36 (100) |
| Females, n (%) | 16 (42.1) | 18 (47.4) | 3 (7.9) | 1 (2.6) | 38 (100) |
| Total, n (%) | 37 (50.0) | 32 (43.2) | 4 (5.4) | 1 (1.4) | 74 (100) |
| Dysfunction Group (GDI) | OHIP Median (IQR) |
|---|---|
| Normal function (n = 37) | 1 (0–4) |
| Adaptation (n = 32) | 4 (1.25–10.75) |
| Compensation (n = 4) | 4.5 (17.5–5.75) |
| Dysfunction (n = 1) | 6 (6–6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schnabl, D.; Sandbichler, P.; Neumaier, M.; Girstmair, J.; Barbieri, F.; Kapferer-Seebacher, I.; Steiner, R.; Laimer, J.; Grunert, I. Dental Students’ Oral Health-Related Quality of Life and Temporomandibular Dysfunction-Self-Rating versus Clinical Assessment. Healthcare 2021, 9, 1348. https://doi.org/10.3390/healthcare9101348
Schnabl D, Sandbichler P, Neumaier M, Girstmair J, Barbieri F, Kapferer-Seebacher I, Steiner R, Laimer J, Grunert I. Dental Students’ Oral Health-Related Quality of Life and Temporomandibular Dysfunction-Self-Rating versus Clinical Assessment. Healthcare. 2021; 9(10):1348. https://doi.org/10.3390/healthcare9101348
Chicago/Turabian StyleSchnabl, Dagmar, Philipp Sandbichler, Maximilian Neumaier, Johannes Girstmair, Fabian Barbieri, Ines Kapferer-Seebacher, René Steiner, Johannes Laimer, and Ingrid Grunert. 2021. "Dental Students’ Oral Health-Related Quality of Life and Temporomandibular Dysfunction-Self-Rating versus Clinical Assessment" Healthcare 9, no. 10: 1348. https://doi.org/10.3390/healthcare9101348
APA StyleSchnabl, D., Sandbichler, P., Neumaier, M., Girstmair, J., Barbieri, F., Kapferer-Seebacher, I., Steiner, R., Laimer, J., & Grunert, I. (2021). Dental Students’ Oral Health-Related Quality of Life and Temporomandibular Dysfunction-Self-Rating versus Clinical Assessment. Healthcare, 9(10), 1348. https://doi.org/10.3390/healthcare9101348






