Age-Friendly Health Care: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Literature Search
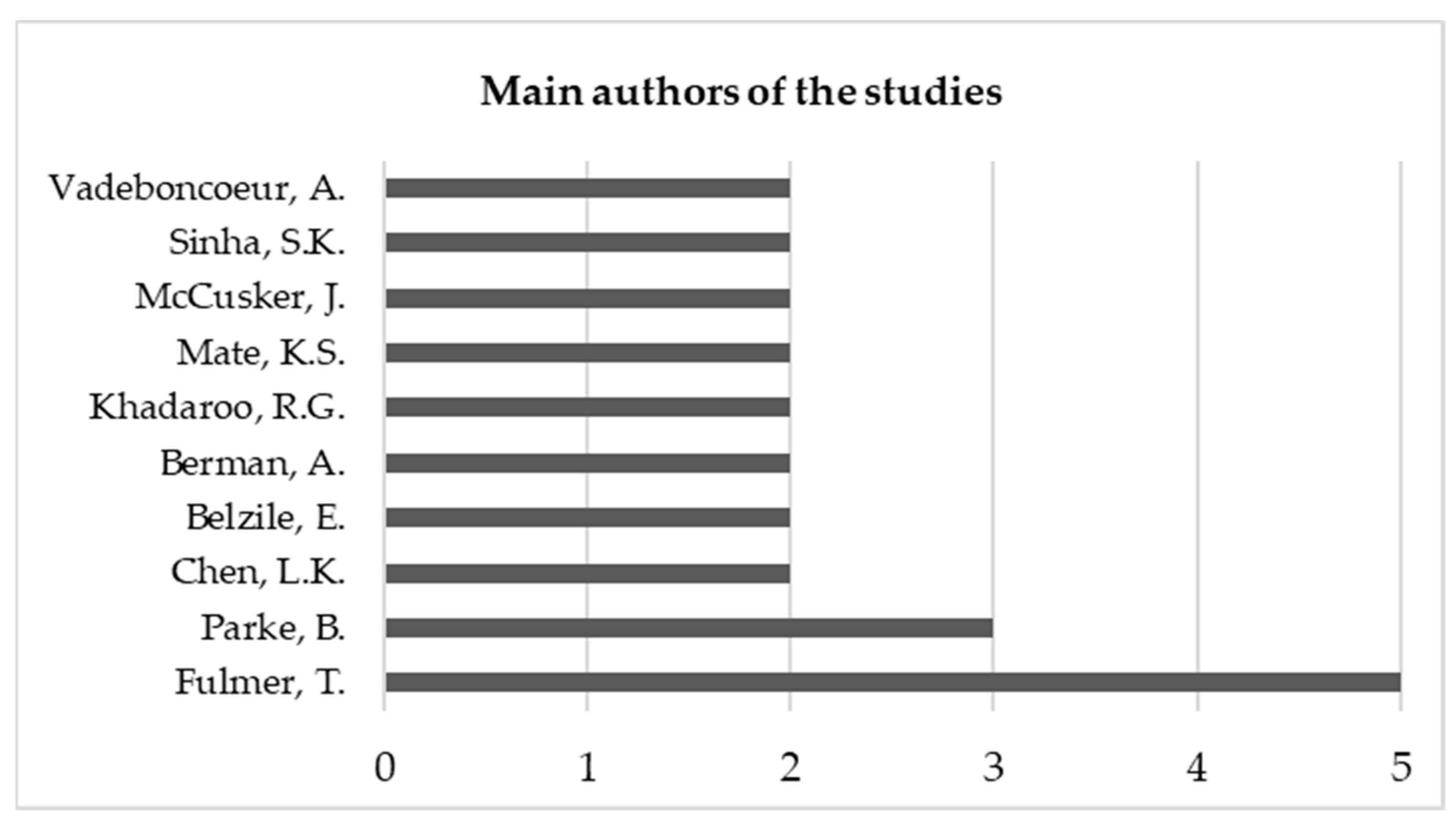
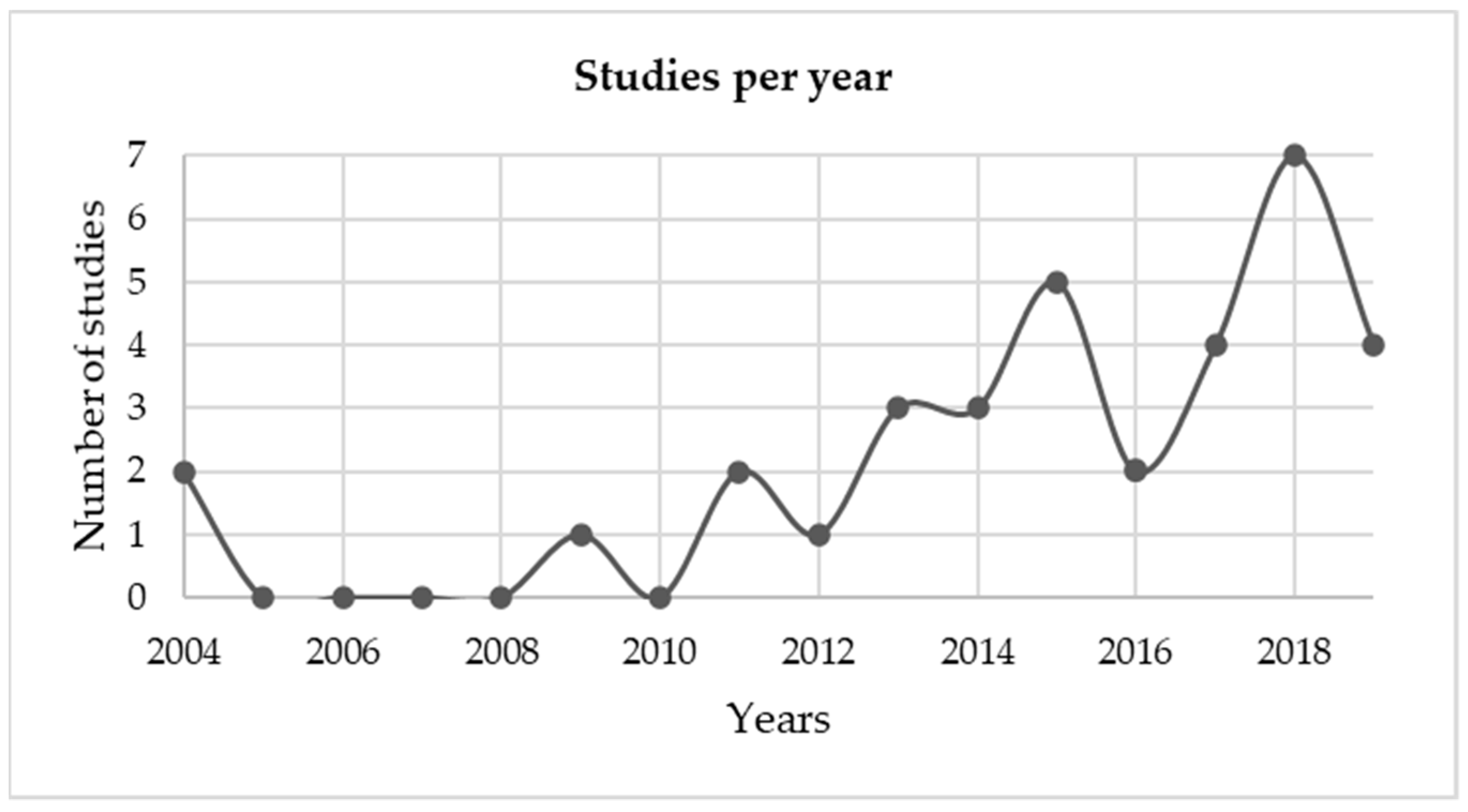
3.2. Characterization of the Studies
3.3. Nature of Care
3.4. Fields of Action
3.5. Level of Conformance
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| WHO Principles | Article Domains |
|---|---|
| Information, Education, Communication and Training | (i) Staffing, (ii) Human resources, (iii) Continuing education, (iv) Education, (v) Information and training, (vi) Social climate, (vii) Communication and services, (viii) Health management information systems, and (ix) Information, education, and training |
| Health Care Management Systems | (i) Care processes, (ii) Screening and assessment, (iii) Clinical protocols, (iv) Discharge planning, (v) Quality assessment, (vi) Policies and procedures, (vii) Systems and processes of care, (viii) Community services, (ix) Care philosophy, (x) Evaluation and monitoring, (xi) Transitions of care, (xii) Quality improvement, (xii) Service policies, (xiv) Management policies, (xv) Medical care services, (xvi) Impatient services, (xvii) Services, (xviii) Geriatric care delivery, (xix) Management systems, and (xx) Health care system |
| Physical Environment | (i) Physical design, (ii) Accessibility, (iii) Equipment/supplies, (iv) Environment, (v) Physical environment, (vi) Physical environment and accessibility, and (vii) Design |
Appendix B
| First Author, Year | Objective |
|---|---|
| Ahmadi, 2015 [40] | To examine the age compatibility of public hospitals in Iran. |
| Alhamdan, 2015 [49] | To evaluate the health care provided to older adults in primary health care and the simple use of these services. |
| Boltz, 2013 [27] | To describe, in the nurse’s opinion, what should be improved in the care of older adults in the emergency department. |
| Campmany, 2019 [28] | To develop a program to assist fragility in the emergency department. |
| Chiou, 2009 [41] | To describe the concept of an age-friendly hospital and present the structure defined in Taiwan. |
| Fulmer, 2018 [53] | To demonstrate how an age-friendly health system can reduce the abuse on older adults. |
| Fulmer, 2018 [54] | To explain how an age-friendly health system can benefit older adults with dementia. |
| Fulmer, 2018 [55] | To explain what motivated the John A. Hartford Foundation to create the “age-friendly health care system” initiative |
| Hanson, 2017 [34] | To assess barriers and facilitators for the implementation of age-friendly surgical interventions in urgent situations. |
| Huisman, 2018 [52] | To present a structural approach to long-term care facilities for older adults in fragile health conditions. |
| Isaacs, 2019 [56] | To present the initiative “age-friendly health systems” developed by the John A. Hartford Foundation. |
| Kanevetci, 2018 [50] | To assess the health needs of older adults cared for in primary health care. |
| Kelley, 2011 [29] | To evaluate the current healthcare practices provided to older adults in the emergency department, identifying the gaps to become an age-friendly caregiver. |
| Khadaroo, 2015 [35] | To realize the impact of age-friendly approaches on the surgical environment in older adults undergoing acute care surgeries. |
| Kim D., 2014 [42] | To explore perceptions about the design elements of an age-friendly hospital. |
| Kim Y., 2017 [48] | To develop a Korean age-friendly hospital structure. |
| Kuo Y., 2019 [44] | To implement an age-friendly hospital certification process and assess changes in professionals’ knowledge and attitudes. |
| Kuo R., 2011 [38] | To assess the quality of outpatient services for older adult patients. |
| Mate, 2018 [57] | To describe the process of creating the John A Hartford Foundation’s “age-friendly healthcare systems” initiative. |
| Mcclelland, 2015 [30] | To review nursing interventions in the management of older adults’ patients in the emergency department. |
| McCusker, 2015 [31] | To develop and validate a preliminary assessment scale for the age-friendly emergency service. |
| McCusker, 2018 [32] | To develop a comprehensive quality assessment tool for an age-friendly emergency service. |
| O’Keeffe, 2004 [43] | To present guidelines for an age-friendly environment based on a literature review. |
| Parke, 2004 [45] | To develop personalized strategies that should be implemented in age-friendly hospitals. |
| Persoon, 2015 [46] | To develop a questionnaire to measure the care that older adults receive at the hospital, the nurses’ attitudes, and the perceptions of older adults’ about said care. |
| Rashmi, 2016 [47] | To develop the criteria for an age-friendly hospital and assess its validity. |
| Santos, 2016 [33] | To identify and analyze the aspects necessary to provide age-friendly health care in the emergency department, from the nurses’ perspective. |
| Sinha, 2014 [36] | To provide guidance on how the age-friendly acute care service can be replicated throughout the hospital. |
| Ssensamba, 2019 [58] | To explore Uganda’s public health system’s readiness to offer age-friendly health care. |
| Tavares, 2017 [39] | To evaluate policies and environments that promote functionality and physical activity in a hospital environment. |
| Verma, 2017 [37] | To analyze the development of models and practices of age-friendly care in the acute care service. |
| Wong, 2014 [5] | To self-assess age-friendly hospitals, by identifying promising practices and initiatives to improve the quality of the system. |
| Woo, 2013 [59] | To identify the needs of older adults and understand how healthcare services are suited to those needs. |
| Woo, 2013 [51] | To assess the compatibility of primary health care with age. |
References
- WHO Methods and Data Sources for Global Burden of Disease Estimates 2000–2016. Available online: https://www.who.int/healthinfo/global_burden_disease/GlobalDALY_method_2000_2016.pdf (accessed on 15 September 2020).
- Parker, M.; Thorslund, M. Health Trends in the Elderly Population: Getting Better and Getting Worse. Gerontologist 2007, 47, 150–158. [Google Scholar] [CrossRef]
- Saad, P. Envelhecimento Populacional: Demandas e Possibilidades na Área da Saúde. In Demografia dos negócios: Campo de estudo, perspectivas e aplicações, 1st ed.; Guimarães, J., Ed.; AEBP Campinas: Campinas, Brazil, 2006; pp. 153–166. [Google Scholar]
- Adams, J.; Gerson, L. A New Model for Emergency Care of Geriatric Patients. Acad. Emerg. Med. 2003, 10, 271–274. [Google Scholar] [CrossRef] [Green Version]
- Wong, K.; Ryan, D.; Liu, B. A System-Wide Analysis Using a Senior-Friendly Hospital Framework Identifies Current Practices and Opportunities for Improvement in the Care of Hospitalized Older Adults. J. Am. Geriatr. Soc. 2014, 62, 2163–2170. [Google Scholar] [CrossRef]
- Rockwood, K.; Song, X.; Macknight, C.; Bergman, H.; Hogan, D.; Mcdowell, I.; Mitnitski, A. A global clinical measure of fitness and frailty in elderly people. Can. Med. Assoc. J. 2005, 173, 489–495. [Google Scholar] [CrossRef] [Green Version]
- Émond, M.; Boucher, V.; Carmichael, P.; Voyer, P.; Pelletier, M.; Gouin, É.; Daoust, R.; Berthelot, S.; Lamontagne, M.; Morin, M.; et al. Incidence of delirium in the Canadian emergency department and its consequences on hospital length of stay: A prospective observational multicentre cohort study. BMJ Open 2018, 8, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Marcantonio, E.; Kiely, D.; Simon, S.; Orav, J.; Jones, R.; Murphy, K.; Bergmann, M. Outcomes of Older People Admitted to Postacute Facilities with Delirium. J. Am. Geriatr. Soc. 2005, 53, 963–969. [Google Scholar] [CrossRef] [PubMed]
- Morris, R.; Riordan, S. Prevention of falls in hospital. J. Clin. Med. 2017, 17, 360–362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gill, E. Reducing hospital acquired pressure ulcers in intensive care. BMJ Qual. Improv. Rep. 2015, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Shulver, W.; Killington, M.; Morris, C.; Crotty, M. “Well, if the kids can do it, I can do it”: Older rehabilitation patients’ experiences of telerehabilitation. Health Expectat. 2017, 20, 120–129. [Google Scholar] [CrossRef]
- Liebzeit, D.; Bratzke, L.; Boltz, M.; Purvis, S.; King, B. Getting Back to Normal: A Grounded Theory Study of Function in Post-hospitalized Older Adults. Gerontologist 2020, 60, 704–714. [Google Scholar] [CrossRef]
- World Health Organization. Global Age-friendly Cities: A Guide. 2007. Available online: https://www.who.int/ageing/publications/Global_age_friendly_cities_Guide_English.pdf (accessed on 18 September 2020).
- Buffel, T.; Phillipson, C. A Manifesto for the Age-Friendly Movement: Developing a New Urban Agenda. J. Aging Soc. Policy 2018, 30, 173–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, M.; Quesnel-Vallée, A. The Structural Burden of Caregiving: Shared Challenges in the United States and Canada. Gerontologist 2017, 57, 19–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parke, B.; Stevenson, L. Creating an Elder-Friendly Hospital. Healthc. Manage. Forum 1999, 12, 45–48. [Google Scholar] [CrossRef]
- World Health Organization. Towards Age-friendly Primary Health Care. Available online: https://www.who.int/ageing/publications/phc/en/ (accessed on 21 August 2020).
- Story, M. Maximizing Usability: The Principles of Universal Design. Assist. Technol. 1998, 10, 4–12. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Age-friendly Primary Health Care Centres Toolkit. Available online: https://www.who.int/ageing/publications/upcoming_publications/en/ (accessed on 26 October 2020).
- International Network of Health Promoting Hospitals and Health Services (Vienna). Task Force on HPH and Age-Friendly Health Care. Available online: https://www.euro.who.int/__data/assets/pdf_file/0009/99801/E90777.pdf (accessed on 26 October 2020).
- Bianchetti, A.; Bellelli, G.; Guerini, F.; Magenroni, A.; Padovani, A.; Rozzini, R.; Trabucchi, M. Improving the care of older patients during the COVID-19 pandemic. Aging Clin. Exp. Res. 2020, 32, 1883–1888. [Google Scholar] [CrossRef]
- Fhon, J.; Silva, L.; Leitón-Espinoza, Z.; Matiello, F.; Araújo, J.; Rodrigues, R. Hospital care for elderly COVID-19 patients. Rev. Latino-Am. Enfermagem 2020, 28. [Google Scholar] [CrossRef]
- De Leo, D.; Trabucchi, M. The fight against COVID-19: A report from the Italian trenches. Int. Psychogeriatr. 2020, 20, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Egger, M.; Davey-Smith, G.; Altman, D. Systematic Reviews in Health Care: Meta-Analysis in Context, 3rd ed.; BMJ Publishing Group: London, UK, 2003; pp. 1–506. [Google Scholar]
- Clarke, M.; Horton, R. Bringing it all together: Lancet -Cochrane collaborate on systematic reviews. Lancet. 2001, 357, 1728. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [Green Version]
- Boltz, M.; Parke, B.; Shuluk, J.; Capezuti, E.; Galvin, J. Care of the Older Adult in the Emergency Department: Nurses Views of the Pressing Issues. Gerontologist 2013, 53, 441–453. [Google Scholar] [CrossRef] [Green Version]
- Campmany, M.; Romeu, J.; Andión, M.; Vales, S. Development of a comprehensive, multidisciplinary program of care for frailty in an emergency department. Eur. Geriatr. Med. 2019, 10, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Kelley, M.; Parke, B.; Jokinen, N.; Stones, M.; Renaud, D. Senior-Friendly Emergency Department Care: An Environmental Assessment. J. Health Serv. Res. Pol. 2011, 16, 6–12. [Google Scholar] [CrossRef]
- Mcclelland, M.; Sorrell, J. Enhancing care of older adults in the emergency department: Old problems and new solutions. J. Psychosoc. Nurs. Ment. Health Serv. 2015, 53, 18–21. [Google Scholar] [CrossRef]
- McCusker, J.; Verdon, J.; Vadeboncoeur, A.; Lévesque, F.; Sinha, S.; Kim, K. The Elder-Friendly Emergency Department Assessment Tool: Development of a Quality Assessment Tool for Emergency Department—Based Geriatric Care. J. Am. Geriatr. Soc. 2015, 60, 1534–1539. [Google Scholar] [CrossRef] [PubMed]
- McCusker, J.; Vu, T.; Veillette, N.; Cossette, S.; Vadeboncoeur, A.; Ciampi, A. Elder-Friendly Emergency Department: Development and Validation of a Quality Assessment Tool. J. Am. Geriatr. Soc. 2018, 66, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.; Lima, M.; Zucatti, P. Elder-friendly emergency services in Brazil: Necessary conditions for care. J. Sch. Nurs. 2016, 50, 594–601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanson, H.; Warkentin, L.; Wilson, R.; Sandhu, N.; Slaughter, S.; Khadaroo, R. Facilitators and barriers of change toward an elder-friendly surgical environment: Perspectives of clinician stakeholder groups. BMC Health Serv. Res. 2017, 17, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Khadaroo, R.; Padwal, R.; Wagg, A.; Clement, F.; Warkentin, L.; Holroyd-Leduc, J. Optimizing senior’s surgical care—Elder-friendly Approaches to the Surgical Environment (EASE) study: Rationale and objectives. BMC Health Serv. Res. 2015, 15. [Google Scholar] [CrossRef] [Green Version]
- Sinha, S.; Oakes, S.; Chaudhry, S.; Suh, T. How to use the ACE unit to improve hospital safety and quality for older patients: From ACE units to elder-friendly hospitals. In Acute Care for Elders: A Model for Interdisciplinary Care, 1st ed.; Malone, M., Capezuti, E., Palmer, R., Eds.; Springer: New York, NY, USA, 2014; pp. 131–156. [Google Scholar]
- Verma, J.; Connor, P.; Hodge, J.; Abrams, H.; Bennett, J.; Sinha, S. Healthcare for the Aging Citizen and the Aging Citizen for Healthcare: Involving Patient Advisors in Elder-Friendly Care Improvement. Healthc. Q. 2017, 20, 14–17. [Google Scholar] [CrossRef] [Green Version]
- Kuo, R.; Wu, Y.; Hsu, T.; Chen, L. Improving outpatient services for elderly patients in Taiwan: A qualitative study. Arch. Gerontol. Geriatr. 2011, 53, 209–217. [Google Scholar] [CrossRef]
- Tavares, J.; Grácio, J.; Nunes, L. Assessment of hospital environments and policies: Seeking an age-friendly hospital. Rev. Bras. Geriatr. Gerontol. 2017, 20, 254–258. [Google Scholar] [CrossRef] [Green Version]
- Ahmadi, A.; Seyedin, H.; Fadaye-Vatan, R. Towards Age-Friendly Hospitals in Developing Countries: A Case Study in Iran. Health. Promot. Perspect. 2015, 5, 42–51. [Google Scholar] [CrossRef] [PubMed]
- Chiou, S.; Chen, L. Towards age-friendly hospitals and health services. Arch. Gerontol. Geriatr. 2009, 49, S3–S6. [Google Scholar] [CrossRef]
- Kim, D.; Lee, J.; Ha, M. Exploring perceptions of designers and medical staff in south korea about design elements for the elder-friendly hospital. J. Interior. Des. 2014, 39, 15–32. [Google Scholar] [CrossRef]
- O’Keeffe, J. Creating a Senior Friendly Physical Environment in our Hospitals. Can. Geriatr. J. 2004, 7, 49–52. [Google Scholar]
- Kuo, Y.; Id, I. Facilitating a change model in age-friendly hospital certification: Strategies and effects. PLoS ONE 2019, 14, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Parke, B.; Brand, P. An Elder-Friendly Hospital: Translating a dream into reality. Nurse. Lead. 2004, 17, 62–76. [Google Scholar] [CrossRef]
- Persoon, A.; Bakker, F.; Wal-huisman, H.; Rikkert, M. Development and Validation of the Geriatric In-Hospital. J. Am. Geriatr. Soc. 2015, 63, 327–334. [Google Scholar] [CrossRef]
- Rashmi, M.; Kasthuri, A.; Rashmi, R. Senior Friendly Hospitals: Development and Application of Criteria: A Descriptive Study. Indian J. Community Med. 2016, 41, 256–262. [Google Scholar] [CrossRef]
- Kim, Y.; Han, S.; Hwang, J.; Park, J.; Lee, J.; Choi, J.; Moon, Y.; Kim, H.; Shin, G.; Lee, J.; et al. Development of the Korean framework for senior-friendly hospitals: A Delphi study. BMC Health Serv. Res. 2017, 17, 528. [Google Scholar] [CrossRef]
- Alhamdan, A.; Alshammari, S.; Al-Amoud, M.; Hameed, T.; Al-Muammar, M.; Bindawas, S.; Al-Orf, S.; Mohamed, A.; Al-Ghamdi, E.; Calder, P. Evaluation of health care services provided for older adults in primary health care centers and its internal environment: A step towards age-friendly health centers. Saudi. Med. J. 2015, 36, 1091–1096. [Google Scholar] [CrossRef] [Green Version]
- Kanevetci, Z.; Yaman, H. Health Needs of Elderly People at Primary Health Care. Fam. Med. J. 2018, 16, 4–9. [Google Scholar]
- Woo, J.; Mak, B.; Yeung, F. Age-Friendly Primary Health Care: An Assessment of Current service Provision for Older Adults in Hong Kong. Health Serv. Insights 2013, 6, 69–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huisman, E.; Appel-Meulenbroek, R.; Kort, H. A structural approach for the redesign of a small-scale care facility as a guideline for decision-makers. Intell. Build. Int. 2018, 12, 32–43. [Google Scholar] [CrossRef]
- Fulmer, T. The Rosalie Wolf Memorial Lecture: Abuse-free Care in a World of Age-friendly Health Systems. J. Elder Abuse Negl. 2018, 30, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Fulmer, T.; Li, N. Age-Friendly Health Systems for Older Adults with Dementia. J. Nurse Pract. 2018, 14, 160–165. [Google Scholar] [CrossRef]
- Fulmer, T.; Mate, K.; Berman, A. The Age-Friendly Health System Imperative. J. Am. Geriatr. Soc. 2018, 66, 22–24. [Google Scholar] [CrossRef]
- Isaacs, S.; Jellinek, P.; Fulmer, T. The John A. Hartford foundation and the growth of geriatrics. Health Aff. 2019, 38, 164–168. [Google Scholar] [CrossRef]
- Mate, K.; Berman, A.; Laderman, M.; Kabcenell, A.; Fulmer, T. Creating Age-Friendly Health Systems–A vision for better care of older adults. Healthcare 2018, 6, 4–6. [Google Scholar] [CrossRef]
- Ssensamba, J.; Mukuru, M.; Nakafeero, M.; Ssenyonga, R.; Kiwanuka, S. Health systems readiness to provide geriatric friendly care services in Uganda: A cross-sectional study. BMC Geriatr. 2019, 19, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Woo, J.; Chau, P.; Mak, B. Elder-Friendly Service Delivery Models. In Aging in Hong Kong: A Comparative Perspective, 1st ed.; Woo, J., Ed.; Springer: Boston, MA, USA, 2013; Volume 5, pp. 211–234. [Google Scholar]
- World Health Organization. Integration of Health Care Delivery: Report of a Who Study Group. Available online: https://apps.who.int/iris/handle/10665/38408 (accessed on 19 November 2020).
- Code Plus: Physical Design Components for an Elder Friendly Hospital. Available online: https://runnymedehc.ca/files/7813/7934/1677/2012-2014_Associated_Appendices.pdf (accessed on 26 November 2020).



| First Author, Year | Domains | WHO Principles |
|---|---|---|
| Ahmadi, 2015 [40] | (i) Information and training, (ii) Management systems, and (iii) Physical environment and accessibility | 1, 2, 3 |
| Alhamdan, 2015 [49] | (i) Services and (ii) Environment | 2, 3 |
| Boltz, 2013 [27] | (i) Social climate, (ii) Policies and procedures, (iii) Systems and processes of care, and (iv) Physical design | 1, 2, 3 |
| Chiou, 2009 [41] | (i) Management policy, (ii) Communication and services, (iii) Care processes, and (iv) Physical environment | 1, 2, 3 |
| Huisman, 2018 [52] | (i) Design | 3 |
| Kelley, 2011 [29] | (i) Social climate, (ii) Policies and procedures, (iii) Health care system, and (iv) Physical environment | 1, 2, 3 |
| Kim D., 2014 [42] | (i) Design | 3 |
| Kim Y., 2017 [48] | (i) Management policy, (ii) Communication and services, (iii) Care processes, and (iv) Physical environment | 1, 2, 3 |
| Kuo, 2019 [44] | (i) Management policy, (ii) Communication and services, (iii) Care processes, and (iv) Physical environment | 1, 2, 3 |
| Mcclelland, 2015 [30] | (i) Staffing, (ii) Policies and procedures, (iii) Transitions of care, (iv) Education, (v) Quality improvement, and (vi) Equipment/supplies | 1, 2, 3 |
| McCusker, 2015 [31] | (i) Screening and assessment, (ii) Staffing, (iii) Discharge planning, (iv) Community services, (v) Care philosophy, (vi) Evaluation and monitoring, and (vii) Physical environment | 1, 2, 3 |
| McCusker, 2018 [32] | (i) Screening and assessment, (ii) Clinical protocols, (iii) Staffing, (iv) Discharge planning, (v) Continuing education, (vi) Quality assessment, and (vii) Physical environment | 1, 2, 3 |
| O’Keeffe, 2004 [43] | (i) Physical environment | 3 |
| Rashmi, 2016 [47] | (i) Medical care services, (ii) Impatient services, (iii) Accessibility, (iv) Physical environment, and (v) Spiritual environment a | 1, 2, 3 |
| Santos, 2016 [33] | (i) Social climate, (ii) Policies and procedures, (iii) Systems and processes of care, and (iv) Physical environment | 1, 2, 3 |
| Ssensamba, 2019 [58] | (i) Leadership and governance a, (ii) Health financing a, (iii) Human resources, (iv), Geriatric care delivery, (vi) Health management information systems, and (vii) Commodities and equipment a | 1, 2 |
| Tavares, 2017 [39] | (i) Service policies and (ii) Environment | 2, 3 |
| Wong, 2014 [5] | (i) Organizational support a, (ii) Care processes, (iii) Emotional and behavioral environment a, (iv) Ethics in clinical care and research a, and (v) Physical environment | 1, 2, 3 |
| Woo, 2013 [51] | (i) Information, education, and training, (ii) Health care management systems and (iii) Physical environment | 1, 2, 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tavares, J.; Santinha, G.; Rocha, N.P. Age-Friendly Health Care: A Systematic Review. Healthcare 2021, 9, 83. https://doi.org/10.3390/healthcare9010083
Tavares J, Santinha G, Rocha NP. Age-Friendly Health Care: A Systematic Review. Healthcare. 2021; 9(1):83. https://doi.org/10.3390/healthcare9010083
Chicago/Turabian StyleTavares, Jéssica, Gonçalo Santinha, and Nelson P. Rocha. 2021. "Age-Friendly Health Care: A Systematic Review" Healthcare 9, no. 1: 83. https://doi.org/10.3390/healthcare9010083
APA StyleTavares, J., Santinha, G., & Rocha, N. P. (2021). Age-Friendly Health Care: A Systematic Review. Healthcare, 9(1), 83. https://doi.org/10.3390/healthcare9010083







