Construction of a Medical Resource Sharing Mechanism Based on Blockchain Technology: Evidence from the Medical Resource Imbalance of China
Abstract
1. Introduction
2. Background: Medical Services and the Development Situation of Blockchain in China
3. Methodology
3.1. Kernel Density Estimation
3.2. Data Envelopment Analysis Model
4. Results
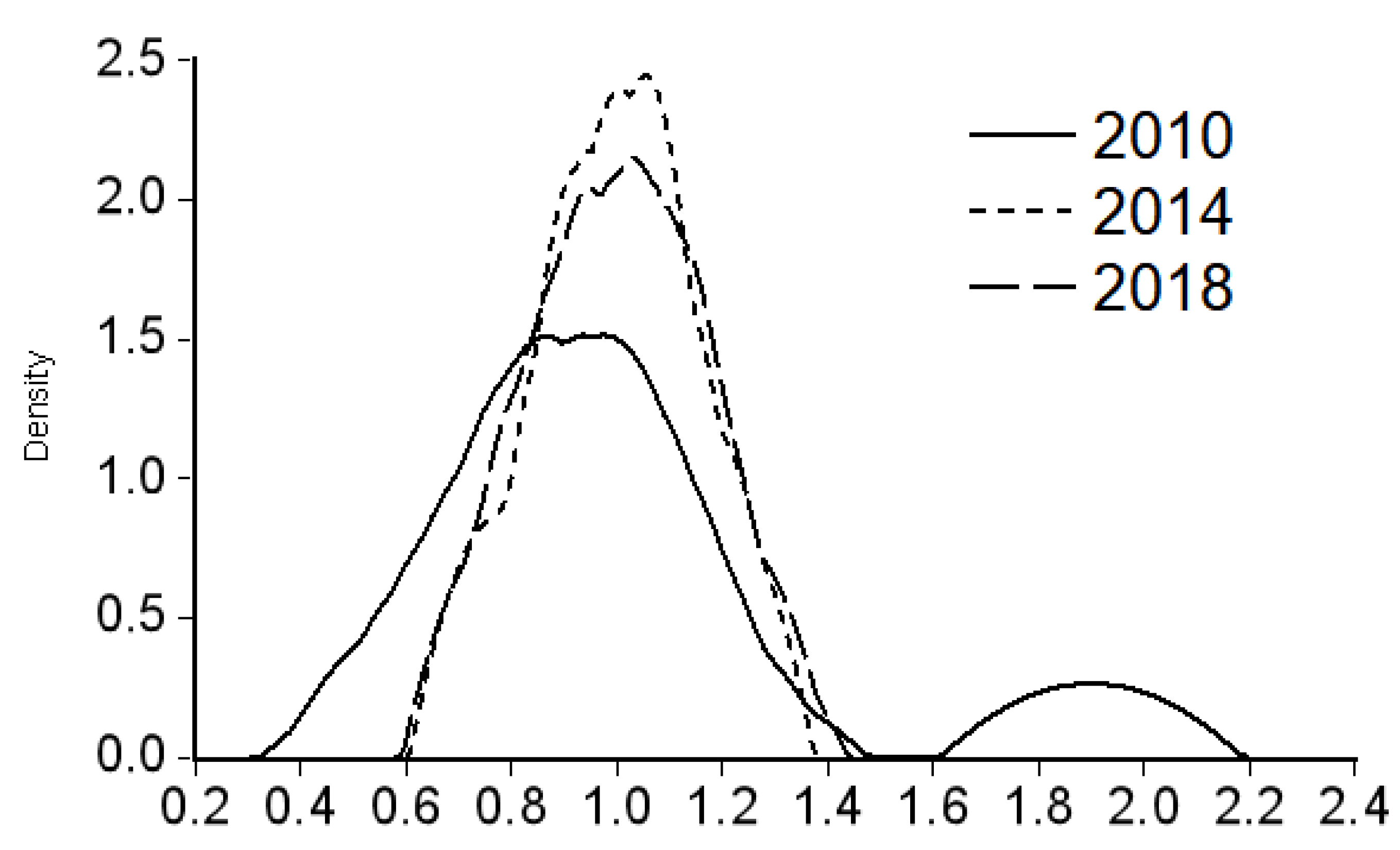
4.1. Kernel Density Estimation
4.2. Data Envelopment Analysis
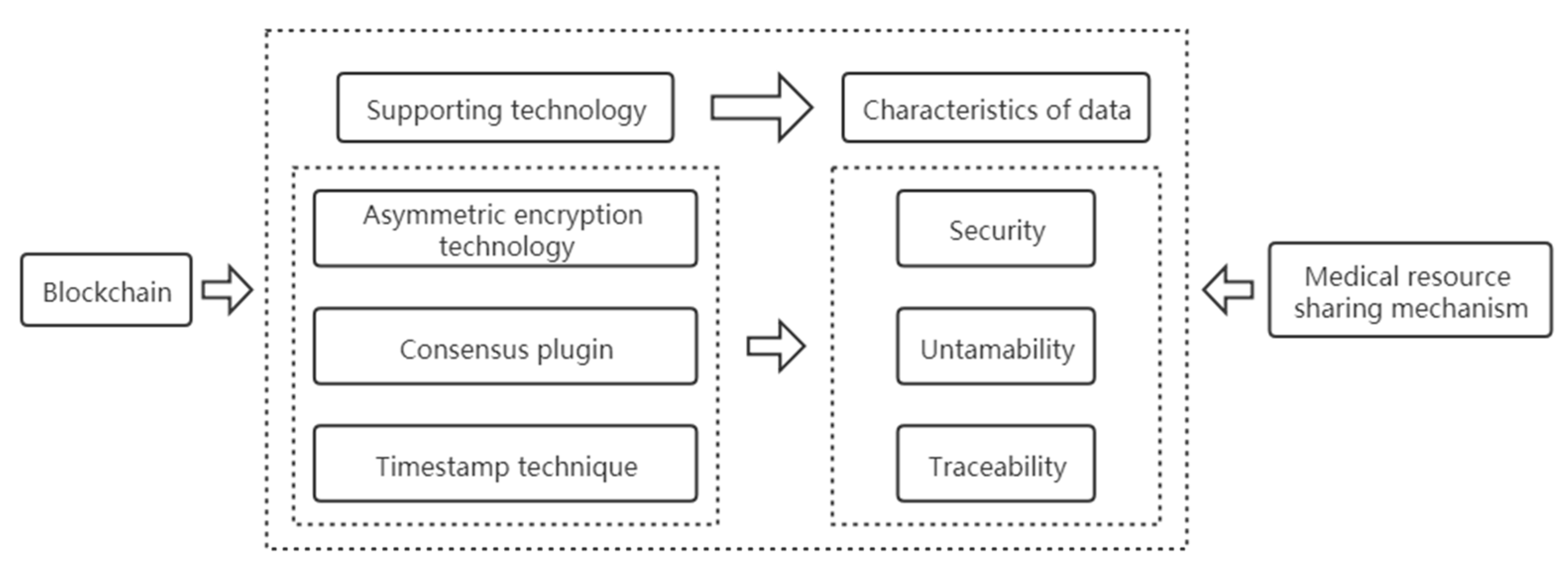
5. Coupling Analysis of Blockchain and Medical Resource Sharing Mechanism
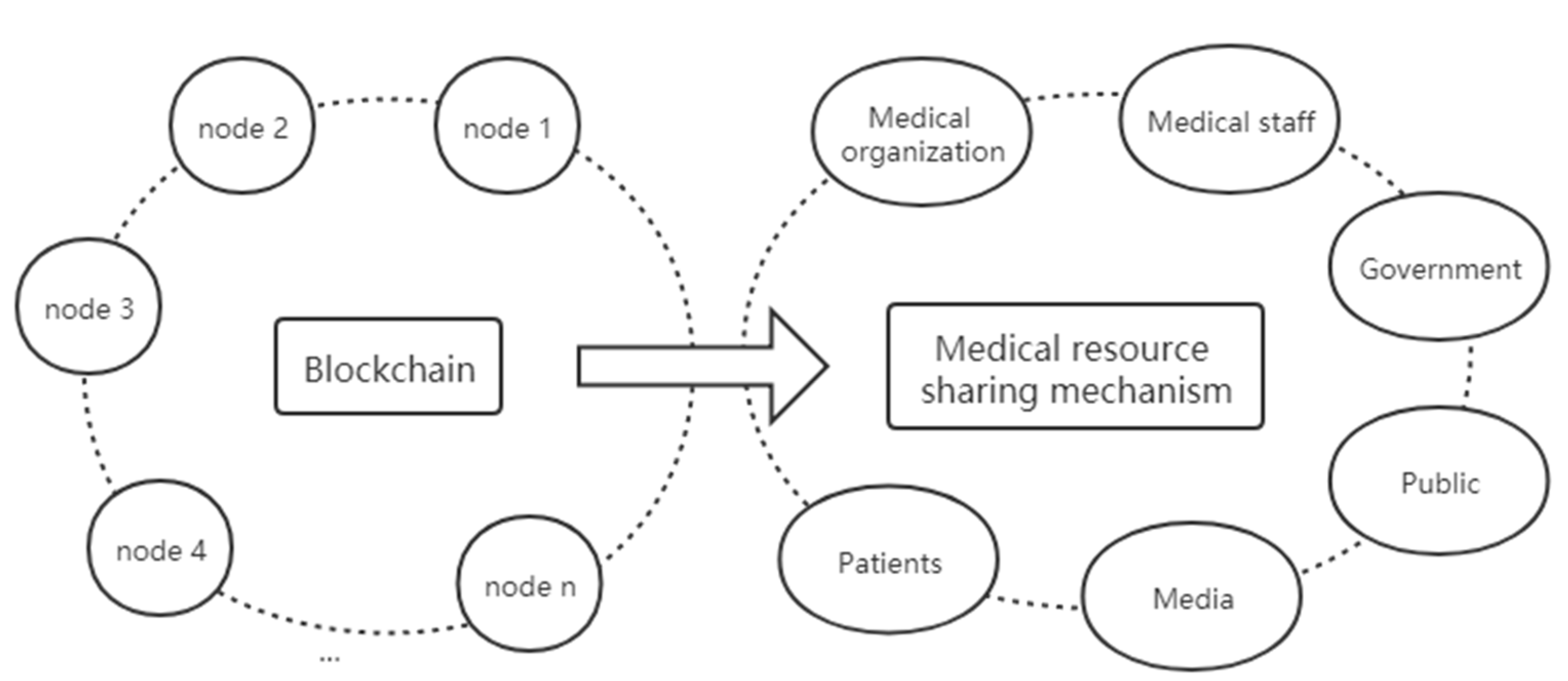
5.1. Application Principal Coupling
5.2. Transaction Mechanism Coupling
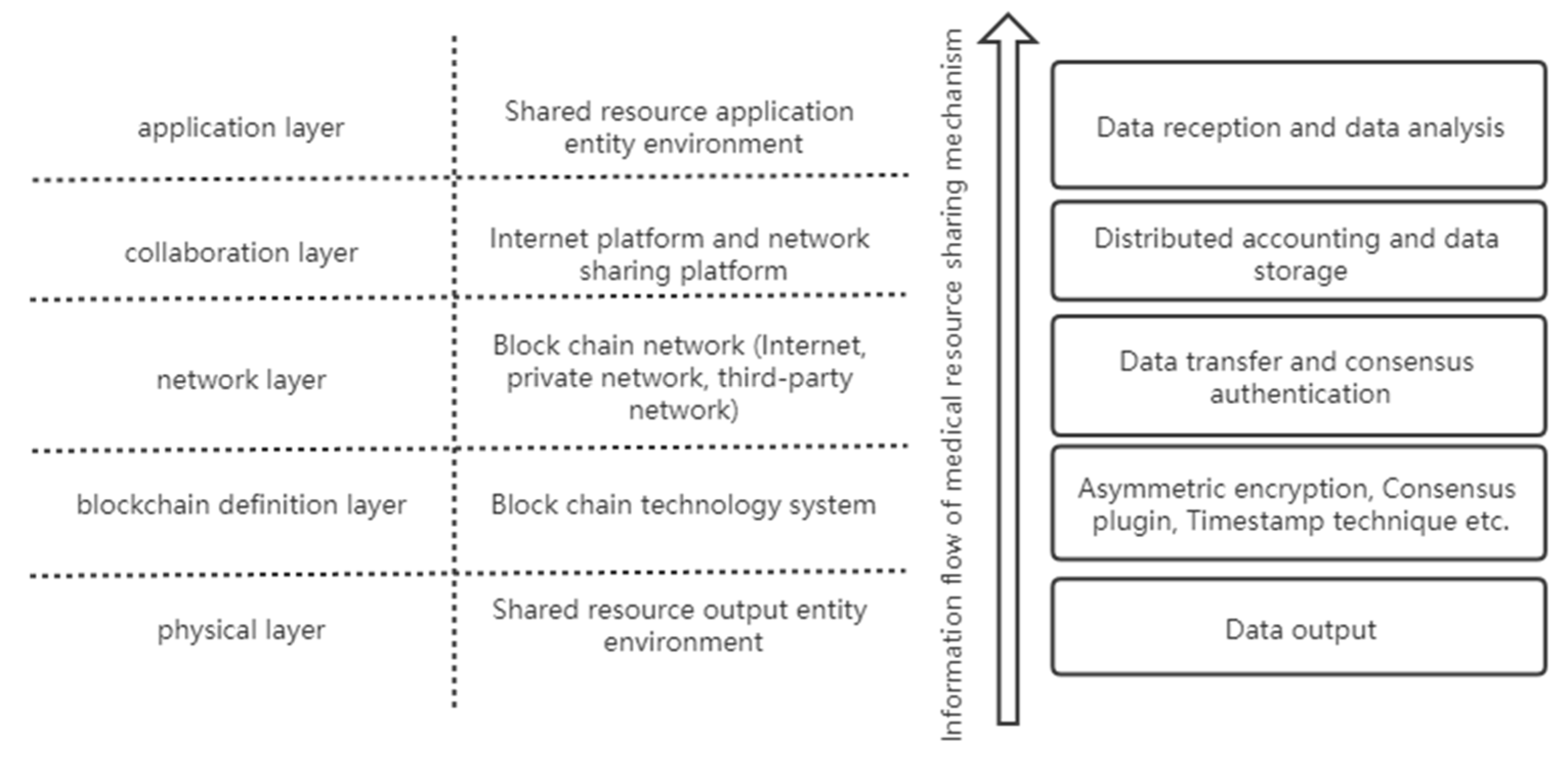
5.3. Information Flow Level Coupling
6. Construction of the Medical Resource Sharing Mechanism
- (1)
- Medical resource storage mechanism. Based on the consensus mechanism, blockchain technology enables data and information to be stored on the chain in an untamperable manner, effectively preventing information loss or malicious tampering and building a secure, trusted, and untamperable medical resource information library on the basis of the security and reliability of blockchain technology.
- (2)
- Medical resource circulation mechanism. Based on the distributed storage structure of blockchain, data circulation can verify and execute value exchanges on the computer network without a central institution. In the process of resource circulation, the point-to-point transaction and intelligent contract between nodes greatly reduce the transaction cost and improves the transaction efficiency. The data in the blockchain system is open to all nodes, and data records can be queried through the exposed interface while ensuring a high degree of information liquidity.
- (3)
- Medical resource supervision mechanism. Based on the timestamp technology, the time dimension is added to data on the chain, which makes the data traceable. It can not only record the time sequence of transactions but also trace data on the chain according to the timestamp, which is convenient for supervision and tracking.
- (4)
- Medical resource protection mechanism. Based on the collective maintenance and anonymity of blockchain technology, the data in the system are jointly maintained by all participating nodes with maintenance functions. The fault of any node will not affect the operation of the whole system, ensuring stable operation of the whole system. There is no need to disclose identities between nodes, and information can be transmitted anonymously to protect user privacy.
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef]
- Li, R.; Pei, S.; Chen, B.; Song, Y.; Zhang, T.; Yang, W.; Shaman, J. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science 2020, 368, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.T.; Leung, K.; Leung, G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: A modelling study. Lancet 2020, 395, 689–697. [Google Scholar] [CrossRef]
- Nakamoto, S. Bitcoin: A Peer-to-Peer Electronic Cash System. Available online: https://bitcoin.org/bitcoin.pdf (accessed on 31 December 2020).
- Swan, M. Blockchain: Blueprint for a New Economy; O′Reilly: Newton, MA, USA, 2015. [Google Scholar]
- Gupta, S.; Sadoghi, M. Blockchain Transaction Processing. In Encyclopedia of Big Data Technologies; Springer International Publishing: New York, NY, USA, 2018; pp. 1–11. [Google Scholar]
- Yaga, D.; Mell, P.; Roby, N.; Scarfone, K. Blockchain technology overview. arXiv 2018, arXiv:1906.11078. [Google Scholar]
- Risius, M.; Spohrer, K. A Blockchain Research Framework: What We (don′t) Know, Where We Go from Here, and How We Will Get There. Bus. Inf. Syst. Eng. 2017, 59, 385–409. [Google Scholar] [CrossRef]
- Christidis, K.; Devetsikiotis, M. Blockchains and Smart Contracts for the Internet of Things. Bus. Inf. Syst. Eng. 2016, 4, 2292–2303. [Google Scholar] [CrossRef]
- Korpela, K.; Hallikas, J.; Dahlberg, T. Digital Supply Chain Transformation toward Blockchain Integration. In Proceedings of the Hawaii International Conference on System Sciences (HICSS), Hilton Waikoloa Village, HI, USA, 4–7 January 2017. [Google Scholar]
- Holotiuk, F.; Pisani, F.; Moormann, J. The Impact of Blockchain Technology on Business Models in the Payments Industry. In Proceedings of the International Conference on Wirtschaftsinformatik, St. Gallen, Switzerland, 12–15 February 2017. [Google Scholar]
- Yermack, D. Corporate Governance and Blockchains. Rev. Financ. 2015, 21, 7–31. [Google Scholar]
- Lnes, S. Beyond Bitcoin Enabling Smart Government Using Blockchain Technology. In Proceedings of the International Conference on Electronic Government and the Information Systems Perspective, Porto, Portugal, 5–8 September 2016. [Google Scholar]
- J-HLee, P.M. How the Blockchain Revolution Will Reshape the Consumer Electronics Industry [Future Directions]. IEEE Consum. Electron. Mag. 2017, 6, 19–23. [Google Scholar]
- Yuan, Y.; Wang, F.Y. Towards blockchain-based intelligent transportation systems. In Proceedings of the IEEE International Conference on Intelligent Transportation Systems, Rio de Janeiro, Brazil, 1–4 November 2016. [Google Scholar]
- Sikorski, J.J.; Haughton, J.; Kraft, M. Blockchain technology in the chemical industry: Machine-to-machine electricity market. Appl. Energy 2017, 195, 234–246. [Google Scholar] [CrossRef]
- Azaria, A.; Ekblaw, A.; Vieira, T.; Lippman, A. MedRec: Using Blockchain for Medical Data Access and Permission Management. In Proceedings of the International Conference on Open & Big Data, Vienna, Austria, 22–24 August 2016. [Google Scholar]
- Lane, H.; Sarkies, M.; Martin, J.; Haines, T. Medicine. Equity in healthcare resource allocation decision making: A systematic review. Soc. Sci. Med. 2017, 175, 11–27. [Google Scholar] [CrossRef]
- Liu, W.; Liu, Y.; Twum, P.; Li, S. National equity of health resource allocation in China: Data from 2009 to 2013. Int. J. Equity Health 2016, 15, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wang, Q.; Jiang, T.; Wang, J. Equity and efficiency of primary health care resource allocation in mainland China. Int. J. Equity Health 2018, 17, 1–12. [Google Scholar] [CrossRef]
- Yan, K.; Jiang, Y.; Qiu, J.; Zhong, X.; Wang, Y.; Deng, J.; Lian, J.; Wang, T.; Cao, C. The equity of China′s emergency medical services from 2010–2014. Int. J. Equity Health 2017, 16, 10. [Google Scholar] [CrossRef]
- Jianhua, C. Study on the Status and Equity of Health Resource Allocation in Jiangsu. Med. Soc. 2013, 12, 12. [Google Scholar]
- Zhang, Y.; Zhang, C.; Wang, Z. Research on the Equity and Influencing Factors of Health Resource Allocation in Xinjiang from 2004 to 2016: A Comprehensive Perspective Based on “Population Fairness” and “Geographical Equality”. Chin. Health Serv. Manag. 2019, 36, 499–509. [Google Scholar]
- Hou, X.; Deng, X.; Zhao, W. Research on status and countermeasures of medical and health information resources allocation in China. Chinese Health Resour. 2014, 17, 274–277. [Google Scholar]
- Liu, H.; Gong, X.; Zhang, J. Does Internet Use Affect Individuals′ Medical Service Satisfaction? Evidence from China. Healthcare 2020, 8, 81. [Google Scholar] [CrossRef]
- Zhang, J.; Cheng, M.; Yu, N. Internet Use and Lower Life Satisfaction: The Mediating Effect of Environmental Quality Perception. Ecol. Econ. 2020, 176, 106725. [Google Scholar] [CrossRef]
- Zhang, J.; Cheng, M.; Mei, R.; Wang, F. Internet use and individuals’ environmental quality evaluation: Evidence from China. Sci. Total. Environ. 2019, 710, 136290. [Google Scholar] [CrossRef]
- Gong, X.; Zhang, J.; Zhang, H.; Cheng, M.; Yu, N. Internet use encourages pro-environmental behavior: Evidence from China. J. Clean. Prod. 2020, 256, 120725. [Google Scholar] [CrossRef]
- Ekblaw, A.; Azaria, A.; Halamka, J.; Lippman, A. A Case Study for Blockchain in Healthcare: MedRec prototype for electronic health records and medical research data. In Proceedings of the IEEE Open & Big Data Conference, Washington, DC, USA, 5–8 December 2016. [Google Scholar]
- Xia, Q.; Sifah, E.B.; Asamoah, K.O.; Gao, J.; Du, X.; Guizani, M. MeDShare: Trust-Less Medical Data Sharing Among Cloud Service Providers via Blockchain. IEEE Access 2017, 5, 14757–14767. [Google Scholar] [CrossRef]
- Kai, F.; Shangyang, W.; Yanhui, R.; Hui, L.; Yintang, Y. MedBlock: Efficient and Secure Medical Data Sharing Via Blockchain. J. Med Syst. 2018, 42, 136. [Google Scholar]
- Dubovitskaya, A.; Xu, Z.; Ryu, S.; Schumacher, M.; Wang, F. Secure and Trustable Electronic Medical Records Sharing using Blockchain. AMI Annu. Symp. Proc. AMIA Symp. 2017, 2017, 650–659. [Google Scholar]
- Li, H.; Zhu, L.; Shen, M.; Gao, F.; Liu, S. Blockchain-Based Data Preservation System for Medical Data. J. Med Syst. 2018, 42, 141–141:13. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Ding, S.; Xu, Z.; Zheng, H.; Yang, S. Blockchain-Based Medical Records Secure Storage and Medical Service Framework. J. Med Syst. 2018, 43, 5. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Li, S. Research on Efficiency of Urban Agglomeration Based on DEA Model—An Empirical Study of the Pearl River Delta City Group. Soft Sci. 2011, 5, 91–95. [Google Scholar]



| Index Type | Index Name | Variable | Unit |
|---|---|---|---|
| Input indicators | Number of medical and health institutions | X1 | per ten thousand persons |
| Number of beds in medical and health institutions | X2 | per ten thousand persons | |
| Number of health technicians | X3 | per ten thousand persons | |
| Output indicators | Total number of visits | Y1 | - |
| Total number of discharged patients | Y2 | - |
| Region | Crste | Vrste | Scale | R-S | |
|---|---|---|---|---|---|
| Eastern | Liaoning Province | 0.479 | 0.6 | 0.798 | drs |
| Jilin Province | 0.297 | 0.458 | 0.649 | drs | |
| Heilongjiang Province | 0.41 | 0.609 | 0.673 | drs | |
| Shanghai | 1 | 1 | 1 | - | |
| Jiangsu Province | 0.887 | 1 | 0.887 | drs | |
| Zhejiang Province | 0.947 | 1 | 0.947 | drs | |
| Anhui Province | 0.7 | 0.841 | 0.833 | drs | |
| Fujian Province | 0.419 | 0.497 | 0.844 | drs | |
| Jiangxi Province | 0.558 | 0.611 | 0.913 | drs | |
| Shandong Province | 0.837 | 0.905 | 0.925 | drs | |
| Middle | Beijing | 0.915 | 0.919 | 0.995 | irs |
| Tianjin | 0.611 | 0.634 | 0.964 | irs | |
| Hebei Province | 0.587 | 0.59 | 0.995 | irs | |
| Shanxi Province | 0.27 | 0.311 | 0.867 | drs | |
| Inner Mongolia Autonomous Region | 0.206 | 0.322 | 0.639 | drs | |
| Henan Province | 1 | 1 | 1 | - | |
| Hubei Province | 0.629 | 0.91 | 0.692 | drs | |
| Hunan Province | 0.814 | 0.845 | 0.964 | drs | |
| Guangdong Province | 1 | 1 | 1 | - | |
| Guangxi Zhuang Autonomous Region | 0.589 | 0.787 | 0.749 | drs | |
| Hainan Province | 0.21 | 0.236 | 0.889 | drs | |
| Western | Chongqing | 0.44 | 0.715 | 0.616 | drs |
| Sichuan Province | 0.943 | 1 | 0.943 | drs | |
| Guizhou Province | 0.482 | 0.677 | 0.712 | drs | |
| Yunnan Province | 0.659 | 0.94 | 0.702 | drs | |
| Tibet Autonomous Region | 0.112 | 1 | 0.112 | irs | |
| Shaanxi Province | 0.456 | 0.595 | 0.766 | drs | |
| Gansu Province | 0.299 | 0.405 | 0.737 | drs | |
| Qinghai Province | 0.169 | 0.22 | 0.77 | drs | |
| Ningxia Hui Autonomous Region | 0.074 | 0.145 | 0.511 | drs | |
| Xinjiang Uygur Autonomous Region | 1 | 1 | 1 | - | |
| Average | 0.580 | 0.702 | 0.809 | - | |
| Region | X1 | X2 | X3 | Y1 | Y2 | |
|---|---|---|---|---|---|---|
| Eastern | Liaoning Province | 0.000 | 0.000 | 1.336 | 1.199 | 0.000 |
| Jilin Province | 0.000 | 1.476 | 1.586 | 0.796 | 0.000 | |
| Heilongjiang Province | 0.000 | 1.187 | 3.169 | 0.886 | 0.000 | |
| Shanghai | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | |
| Jiangsu Province | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | |
| Zhejiang Province | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | |
| Anhui Province | 0.000 | 0.000 | 1.034 | 0.577 | 0.000 | |
| Fujian Province | 0.000 | 0.290 | 0.000 | 0.139 | 0.000 | |
| Jiangxi Province | 0.000 | 0.000 | 1.131 | 1.426 | 0.000 | |
| Shandong Province | 1.650 | 0.975 | 0.000 | 0.159 | 0.000 | |
| Middle | Beijing | 0.000 | 5.049 | 0.000 | 0.000 | 0.021 |
| Tianjin | 0.000 | 1.049 | 0.000 | 0.000 | 0.026 | |
| Hebei Province | 2.472 | 0.000 | 0.000 | 0.365 | 0.000 | |
| Shanxi Province | 0.000 | 0.000 | 0.675 | 1.324 | 0.000 | |
| Inner Mongolia Autonomous Region | 0.000 | 1.789 | 1.550 | 0.499 | 0.000 | |
| Henan Province | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | |
| Hubei Province | 0.000 | 1.079 | 0.481 | 1.293 | 0.000 | |
| Hunan Province | 0.000 | 0.394 | 0.143 | 2.395 | 0.000 | |
| Guangdong Province | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | |
| Guangxi Zhuang Autonomous Region | 0.000 | 1.850 | 0.000 | 1.230 | 0.000 | |
| Hainan Province | 0.000 | 5.034 | 2.069 | 0.000 | 0.000 | |
| Western | Chongqing | 0.000 | 1.887 | 3.180 | 0.798 | 0.000 |
| Sichuan Province | 1.310 | 0.410 | 0.910 | 0.190 | 0.000 | |
| Guizhou Province | 0.000 | 0.697 | 1.529 | 1.145 | 0.000 | |
| Yunnan Province | 0.000 | 0.874 | 1.474 | 0.710 | 0.000 | |
| Tibet Autonomous Region | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | |
| Shaanxi Province | 0.000 | 4.191 | 0.000 | 1.270 | 0.000 | |
| Gansu Province | 0.000 | 0.430 | 1.401 | 1.073 | 0.000 | |
| Qinghai Province | 0.000 | 7.631 | 4.730 | 0.160 | 0.000 | |
| Ningxia Hui Autonomous Region | 0.000 | 17.922 | 18.126 | 0.000 | 0.000 | |
| Xinjiang Uygur Autonomous Region | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, H.; Liu, Y. Construction of a Medical Resource Sharing Mechanism Based on Blockchain Technology: Evidence from the Medical Resource Imbalance of China. Healthcare 2021, 9, 52. https://doi.org/10.3390/healthcare9010052
Liu H, Liu Y. Construction of a Medical Resource Sharing Mechanism Based on Blockchain Technology: Evidence from the Medical Resource Imbalance of China. Healthcare. 2021; 9(1):52. https://doi.org/10.3390/healthcare9010052
Chicago/Turabian StyleLiu, Hu, and Yuxuan Liu. 2021. "Construction of a Medical Resource Sharing Mechanism Based on Blockchain Technology: Evidence from the Medical Resource Imbalance of China" Healthcare 9, no. 1: 52. https://doi.org/10.3390/healthcare9010052
APA StyleLiu, H., & Liu, Y. (2021). Construction of a Medical Resource Sharing Mechanism Based on Blockchain Technology: Evidence from the Medical Resource Imbalance of China. Healthcare, 9(1), 52. https://doi.org/10.3390/healthcare9010052




