A Comparative Analysis of Student and Practising Nurses’ Health Literacy Knowledge in Ghana
Abstract
1. Introduction
1.1. Aims of This Study
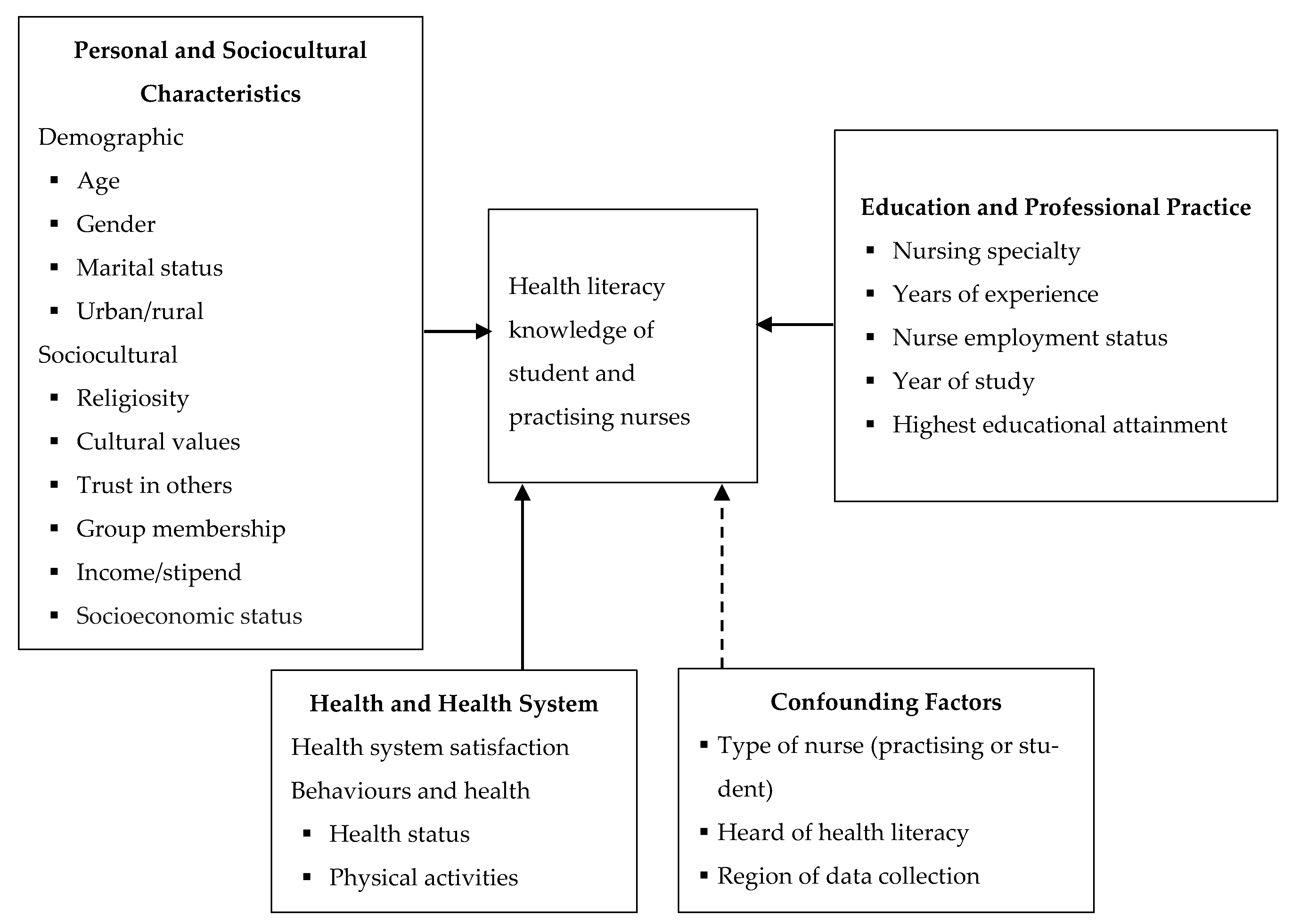
1.2. What Accounts for Health Literacy and Health Literacy Knowledge? Conceptual Perspectives
2. Methods
2.1. Study Design
2.2. Sampling
2.3. Measures
2.3.1. Dependent Variable
2.3.2. Independent Variables
2.4. Data Analyses
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nutbeam, D.; McGill, B.; Premkumar, P. Improving health literacy in community populations: A review of progress. Health Promot. Int. 2017, 33, 901–911. [Google Scholar] [CrossRef] [PubMed]
- Cafiero, M. Nurse Practitioners’ Knowledge, Experience, and Intention to Use Health Literacy Strategies in Clinical Practice. J. Health Commun. 2013, 18 (Supp1. S1), 70–81. [Google Scholar] [CrossRef]
- Wittenberg, E.; Ferrell, B.; Kanter, E.; Buller, H. Health Literacy: Exploring Nursing Challenges to Providing Support and Understanding. Clin. J. Oncol. Nurs. 2018, 22, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Kennard, D.K. Health Literacy Concepts in Nursing Education. Nurs. Educ. Perspect. 2016, 37, 118–119. [Google Scholar] [PubMed]
- McCleary-Jones, V. Assessing nursing students’ knowledge of health literacy. Nurse Educ. 2012, 37, 214–217. [Google Scholar] [CrossRef]
- Asamani, J.A.; Amertil, N.P.; Ismaila, H.; Francis, A.A.; Chebere, M.M.; Nabyonga-Orem, J. Nurses and midwives demographic shift in Ghana—The policy implications of a looming crisis. Hum. Resour. Health 2019, 17, 32. [Google Scholar] [CrossRef]
- Knight, G.D. An Evaluation of the Health Literacy Knowledge and Experience of Registered Nurses in Georgia. Ph.D. Thesis, Auburn University, Auburn, AL, USA, 2011. [Google Scholar]
- Torres, R.; Nichols, J. Health literacy knowledge and experiences of associate degree nursing students: A pedagogical study. Teach. Learn. Nurs. 2014, 9, 84–92. [Google Scholar] [CrossRef]
- Williamson, S.S.; Chopak-Foss, J. Differences in Health Literacy Knowledge and Experiences among Senior Nursing Students. J. Ga. Public Health Assoc. 2015, 5, 184–190. [Google Scholar]
- Nielsen-Bohlman, L.; Panzer, A.M.; Kindig, D.A. Health Literacy: A Prescription to End Confusion; Institute of Medicine of The National Academies: Washington, DC, USA, 2004. [Google Scholar]
- Nutbeam, D. The evolving concept of health literacy. Soc. Sci. Med. 2008, 67, 2072–2078. [Google Scholar] [CrossRef]
- Sorensen, K.; Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12. [Google Scholar] [CrossRef]
- Nutbeam, D. Health literacy as a population strategy for health promotion. Jpn. J. Health Educ. Promot. 2017, 25, 210–222. [Google Scholar] [CrossRef]
- Amoah, P.A.; Phillips, D.R. Health literacy and health: Rethinking the strategies for universal health coverage in Ghana. Public Health 2018, 159, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Sentell, T.L.; Tsoh, J.Y.; Davis, T.; Davis, J.; Braun, K.L. Low health literacy and cancer screening among Chinese Americans in California: A cross-sectional analysis. BMJ Open 2015, 5. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Viera, A.; Crotty, K.; Viswanathan, M. Health Literacy Interventions and Outcomes: An Updated Systematic Review; AHRQ Publication Number 11-E006; Rockville, M.A., Ed.; RTI International–University of North Carolina Evidence-Based Practice Center: Rockville, MD, USA, 2011. [Google Scholar]
- Cormier, C.M.; Kotrlik, J.W. Health literacy knowledge and experiences of senior baccalaureate nursing students. J. Nurs. Educ. 2009, 48, 237–248. [Google Scholar] [CrossRef]
- Nesari, M.; Olson, J.K.; Nasrabadi, A.N.; Norris, C. Registered Nurses’ Knowledge of and Experience with Health Literacy. Health Lit. Res. Pract. 2019, 3, e268–e279. [Google Scholar] [CrossRef]
- Ozen, N.; Bal Ozkaptan, B.; Coskun, S.; Terzioglu, F. Health literacy of nursing students and its effective factors. Nurs. Forum. 2019, 54, 396–402. [Google Scholar] [CrossRef]
- Macabasco-O’Connell, A.; Fry-Bowers, E.K. Knowledge and perceptions of health literacy among nursing professionals. J. Health Commun. 2011, 16 (Supppl. S3), 295–307. [Google Scholar] [CrossRef]
- Koduah, O.A.; Leung, Y.M.A.; Leung, Y.L.D.; Liu, Y.W.J. “I Sometimes Ask Patients to Consider Spiritual Care”: Health Literacy and Culture in Mental Health Nursing Practice. Int. J. Environ. Res. Public Health 2019, 16, 3589. [Google Scholar] [CrossRef]
- Kennard, D. Emergency Room Nurses Knowledge of and Experience with Health Literacy and Their Patient Teaching Methods; Seton Hall University: South Orange, NJ, USA, 2017. [Google Scholar]
- McCleary-Jones, V. A Systematic Review of the Literature on Health Literacy in Nursing Education. Nurse Educ. 2016, 41, 93–97. [Google Scholar] [CrossRef]
- Cormier, C.M.; Kotrlik, J.W. Health literacy knowledge and experiences of senior level baccalaureate nursing students. J. Nurs. Educ. 2006, 48. [Google Scholar] [CrossRef]
- McClintock, H.; Schrauben, S.; Andrews, A.; Wiebe, D. Measurement of health literacy to advance global health research: A study based on Demographic and Health Surveys in 14 sub-Saharan countries. Lancet Glob. Health 2017, 5, S18. [Google Scholar] [CrossRef]
- Nantsupawat, A.; Wichaikhum, O.A.; Abhicharttibutra, K.; Kunaviktikul, W.; Nurumal, M.S.B.; Poghosyan, L. Nurses’ knowledge of health literacy, communication techniques, and barriers to the implementation of health literacy programs: A cross-sectional study. Nurs. Health Sci. 2020, 22, 577–585. [Google Scholar] [CrossRef] [PubMed]
- Amoah, P.A.; Phillips, D.R.; Gyasi, R.M.; Koduah, A.O.; Edusei, J. Health literacy and self-perceived health status among street youth in Kumasi, Ghana. Cogent Med. 2017, 4, 1–13. [Google Scholar] [CrossRef]
- Amoah, P.A.; Koduah, A.O.; Gyasi, R.; Gwenzi, G.; Anaduaka, S.U. The relationship between functional health literacy, health-related behaviours and socio-demographic characteristics of street-involved youth in Ghana. Int. J. Health Promot. Educ. 2018, 56, 116–132. [Google Scholar] [CrossRef]
- Ansu-Yeboah, E.; Edusei, A.; Gulis, G. Comprehensive Health Literacy Among Undergraduates: A Ghanaian University-Based Cross-Sectional Study. HLRP Health Lit. Res. Pract. 2019, 3, e227–e237. [Google Scholar] [CrossRef]
- Lori, J.R.; Dahlem, C.H.Y.; Ackah, J.V.; Adanu, R.M.K. Examining Antenatal Health Literacy in Ghana. J. Nurs. Scholarsh. 2014, 46, 432–440. [Google Scholar] [CrossRef]
- Amoah, P.A. Social Capital, Health Literacy and Access to Healthcare: A Study among Rural and Urban Populations in Ghana. Ph.D. Thesis, Lingnan University, Hong Kong, 2017. Available online: http://commons.ln.edu.hk/soc_etd/41/ (accessed on 1 December 2018).
- Amoah, P.A. Social participation, health literacy, and health and well-being: A cross-sectional study in Ghana. SSM Popul. Health 2018, 4, 263–270. [Google Scholar] [CrossRef]
- Budhathoki, S.S.; Pokharel, P.K.; Jha, N.; Moselen, E.; Dixon, R.; Bhattachan, M.; Osborne, R.H. Health literacy of future healthcare professionals: A cross-sectional study among health sciences students in Nepal. Int. Health 2019, 11, 15–23. [Google Scholar] [CrossRef]
- Monette, D.R.; Sullivan, T.J.; Dejong, C. Applied Social Research: A Tool for the Human Services; Brooks/Cole: Belmont, TN, USA, 2008. [Google Scholar]
- De Coster, J.; Iselin, A.-M. Logistic Coefficient to Odds Ratio. 2005. Available online: http://stat-help.com/spreadsheets.html (accessed on 1 December 2018).
- Amoah, P.A.; Phillips, D.R. Socio-Demographic and Behavioral Correlates of Health Literacy: A Gender Perspective in Ghana. Women Health 2020, 60, 123–139. [Google Scholar] [CrossRef]
- Kim, Y.C.; Lim, J.Y.; Park, K. Effects of Health Literacy and Social Capital on Health Information Behavior. J. Health Commun. 2015, 20, 1084–1094. [Google Scholar] [CrossRef]
- Valente, T.W. Social Networks and Health: Models, Methods and Applications; Oxford University Press: Oxford, UK, 2010. [Google Scholar]
- Kirkman, A.; Wilkinson, J.; Scahill, S. Thinking about health care differently: Nurse practitioners in primary health care as social entrepreneurs. J. Prim. Health Care 2018, 10, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Dawson-Rose, C.; Cuca, Y.P.; Webel, A.R.; Báez, S.S.S.; Holzemer, W.L.; Rivero-Méndez, M.; Lindgren, T. Building Trust and Relationships Between Patients and Providers: An Essential Complement to Health Literacy in HIV Care. J. Assoc. Nurs. AIDS Care 2016, 27, 574–584. [Google Scholar] [CrossRef]
- Chen, X.; Hay, J.L.; Waters, E.A.; Kiviniemi, M.T.; Biddle, C.; Schofield, E.; Orom, H. Health Literacy and Use and Trust in Health Information. J. Health Commun. 2018, 23, 724–734. [Google Scholar] [CrossRef] [PubMed]
- Razazi, R.; Aliha, J.; Amin, A.; Taghavi, S.; Ghadrdoost, B.; Naderi, N. The relationship between health literacy and knowledge about heart failure with recurrent admission of heart failure patients. Res. Cardiovasc. Med. 2018, 7, 123–129. [Google Scholar] [CrossRef]
- Rikard, R.V.; Thompson, M.S.; McKinney, J.; Beauchamp, A. Examining health literacy disparities in the United States: A third look at the National Assessment of Adult Literacy (NAAL). BMC Public Health 2016, 16, 975. [Google Scholar] [CrossRef]
- Adler, N.E.; Newman, K. Socioeconomic Disparities In Health: Pathways and Policies. Health Aff. 2002, 21, 60–76. [Google Scholar] [CrossRef]
- Tang, C.; Wu, X.; Chen, X.; Pan, B.; Yang, X. Examining income-related inequality in health literacy and health-information seeking among urban population in China. BMC Public Health 2019, 19, 221. [Google Scholar] [CrossRef] [PubMed]
| Variable | Student Nurses N = 477 | Practising Nurses (N = 399) | p-Value | Overall (N = 876) |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| Age (in years) | 0.001a | |||
| Mean (SD) | 23.3 (3.4) | 29.0 (5.1) | 26.2 (4.3) | |
| Minimum–Maximum values | 18–46 | 21–59 | ||
| Sex | 0.035 | |||
| Male | 224 (47.0) | 156 (39.3) | 380 (43.5) | |
| Female | 253 (53.0) | 241 (60.7) | 494 (56.5) | |
| Region of work/school | 0.008 | |||
| Ashanti Region | 78 (16.4) | 88 (22.3) | 166 (19.1) | |
| Central Region | 10 (2.1) | 8 (2.0) | 18 (2.1) | |
| Eastern Region | 12 (2.5) | 13 (3.3) | 25 (2.9) | |
| Greater Accra Region | 207 (43.5) | 97 (24.6) | 304(34.9) | |
| Northern Region | 61 (12.8) | 132 (33.4) | 193 (22.2) | |
| Upper East | 38 (8.0) | 13 (3.3) | 51 (5.9) | |
| Upper West | 2 (0.4) | 2 (0.5) | 4 (0.5) | |
| Brong Ahafo Region | 24 (5.0) | 27 (6.8) | 51 (5.9) | |
| Western Region | 6 (1.3) | 7 (1.8) | 13 (1.5) | |
| Volta Region | 38 (8.0) | 8 (2.0) | 46 (5.3) | |
| Area of residence | 0.168 | |||
| Urban | 348 (73.0) | 308 (77.2) | 656 (74.9) | |
| Rural | 129 (27.0) | 91 (22.8) | 220 (25.1) | |
| Educational attainment | 0.005 | |||
| Certificate in nursing | 84 (17.6) | 104 (26.0) | 188 (21.5) | |
| Diploma in nursing | 311 (65.2) | 211 (53.1) | 522 (59.6) | |
| Bachelor’s degree | 74 (15.5) | 76 (18.9) | 150 (17.1) | |
| Master’s degree | 8 (1.7) | 8 (2.1) | 16 (1.8) | |
| Marital status | 0.001L | |||
| Married | 32 (6.7) | 151 (37.8) | 173 (19.7) | |
| Divorced | 10 (2.1) | 6 (1.5) | 16 (1.8) | |
| Windowed | 1 (0.2) | 2 (0.6) | 4 (0.4) | |
| Separated | 11 (2.3) | 14 (3.5) | 25 (2.8) | |
| Living together as married | 5 (1.1) | 10 (2.4) | 14 (1.6) | |
| Monthly Income/stipend (if employed) GH¢ | 0.001a | |||
| Mean (SD) | 392.28 (81.38) | 1150 (705.94) | ||
| Minimum–Maximum values | 0–740 | 0–4000 | ||
| Religiosity | 0.001 | |||
| Strongly agree | 114 (23.9) | 127 (31.9) | 238 (27.2) | |
| agree | 200 (42.1) | 186 (46.6) | 385 (44.0) | |
| Neither agree nor disagree | 80 (16.8) | 46 (11.5) | 128 (14.6) | |
| Disagree | 48 (10.1) | 20 (5.0) | 70 (8.0) | |
| Strongly disagree | 20 (4.2) | 20 (5.0) | 55 (6.3) | |
| Cultural values | 0.995 | |||
| Strongly agree | 45 (9.5) | 17 (4.2) | 85 (9.7) | |
| agree | 237 (49.6) | 201 (50.3) | 438 (50.0) | |
| Neither agree nor disagree | 83 (17.3) | 69 (17.2) | 151 (17.2) | |
| Disagree | 72 (15.0) | 57 (14.2) | 128 (14.6) | |
| Strongly disagree | 41 (8.6) | 33 (8.3) | 74 (8.5) | |
| Trust in others | 0.001 | |||
| Yes | 198 (41.5) | 103 (25.7) | 301 (34.4) | |
| No | 279 (58.5) | 296 (74.3) | 575 (65.6) | |
| Membership of an association | 0.251 | |||
| Yes | 321 (67.3) | 253 (63.4) | 574 (65.5) | |
| No | 156 (32.7) | 146 (36.6) | 302 (34.5) | |
| Socioeconomic Status (SES) | 0.005a | |||
| Mean (SD) | 5.3 (2.0) | 5.7 (1.7) | 5.5(1.9) | |
| Minimum–Maximum values | 0–10 | 0–10 | 0–10 | |
| Nursing speciality | 0.001 | |||
| General Nursing | 265 (55.9) | 184 (46.2) | 449 (51.4) | |
| Midwifery | 71 (14.5) | 48 (12.1) | 119 (13.6) | |
| Mental Health Nursing | 49 (10.3) | 125 (31.4) | 174 (19.9) | |
| Community Nursing | 41 (8.6) | 28 (7.0) | 69 (7.9) | |
| Public Health Nurse | 28 (5.9) | 9 (2.3) | 37 (4.2) | |
| Occupational therapy | 19 (4.0) | -- | 19 (2.2) | |
| Clinical nurse assistant | 2 (0.4) | 2 (0.5) | 4 (0.5) | |
| Ophthalmology | -- | 2 (0.5) | 2 (0.2) | |
| Years of experience ^ | -- | |||
| Mean (SD) | -- | 4.8 (3.8) | 4.8 (3.8) | |
| Minimum–Maximum values | -- | 1–27 | 1–27 | |
| Year of study ^^ | -- | |||
| 2 | 219 (46.4) | -- | 219 (46.4) | |
| 3 | 227 (48.1) | -- | 227 (48.1) | |
| 4 | 26 (5.5) | -- | 26 (5.5) | |
| Health status | 0.790 | |||
| Poor | 33 (6.9) | 22 (5.5) | 55 (6.3) | |
| Fair | 96 (20.1) | 87 (21.8) | 183 (20.9) | |
| Good | 204 (42.8) | 157 (39.3) | 361 (41.2) | |
| Very good | 100 (21.0) | 103 (25.8) | 203 (23.2) | |
| Excellent | 44 (9.2) | 30 (7.5) | 74 (8.4) | |
| Physical activities | 0.024 | |||
| Never | 96 (20.1) | 97 (24.5) | 193 (22.1) | |
| Once | 139 (29.1) | 112 (28.3) | 251 (28.8) | |
| Several times in the month | 81 (17.0) | 101 (25.5) | 182 (20.8) | |
| Several times a week | 104 (21.8) | 41 (10.4) | 145 (16.6) | |
| Daily | 57 (11.9) | 45 (11.4) | 102 (11.7) | |
| Use of curative healthcare | 0.001 | |||
| Never | 85 (17.9) | 77 (19.3) | 162 (18.5) | |
| Not often | 232 (48.8) | 271 (67.9) | 496 (56.8) | |
| Often | 128 (26.9) | 40 (10.0) | 174 (19.9) | |
| Countless times | 30 (6.3) | 11 (2.8) | 42 (4.8) | |
| Health system satisfaction | 0.001 | |||
| Completely dissatisfied | 59 (12.9) | 78 (19.5) | 137 (16.0) | |
| Very dissatisfied | 95 (20.1) | 82 (20.6) | 177 (20.7) | |
| Fairly dissatisfied | 77 (16.8) | 91 (22.8) | 168 (19.6) | |
| Neither satisfied nor dissatisfied | 51 (11.1) | 38 (9.5) | 89 (10.4) | |
| Fairly satisfied | 138 (30.1) | 91 (22.8) | 229 (26.7) | |
| Very satisfied | 24 (5.2) | 11 (2.7) | 35(4.1) | |
| Completely satisfied | 14 (3.1) | 8 (2.0) | 22 (2.6) | |
| Heard of health literacy | 0.038 | |||
| Yes | 372 (78.3) | 285 (71.4) | 659 (75.4) | |
| No | 103 (21.7) | 114 (28.6) | 215 (24.6) | |
| Health literacy knowledge (HLKES) | 0.001a | |||
| Mean (SD) | 5.8 (2.6) | 7.4 (3.0) | 6.6 (2.9) | |
| Minimum –Maximum values | 0–13 | 0–17 | 0–17 |
| Student Nurses ^ | Practising Nurses | Overall Sample ^ | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | 95% CI | Stand. Error | Odds Ratio b | B | 95% CI | Stand. Error | Odds Ratio b | B | 95% CI | Stand. Error | Odds Ratio b | |
| Personal and socio-cultural characteristics | ||||||||||||
| Age | -- | -- | -- | -- | −0.007 | −0.106, 0.091 | 0.050 | 0.993 | 0.055 | −0.016, 0.127 | 0.037 | 1.057 |
| Sex | ||||||||||||
| Male | −0.499 ** | −0.876, −0.122 | 0.192 | 0.607 | -- | -- | -- | -- | −0.394 | −0.851, 0.062 | 0.233 | 0.674 |
| Female (ref) | ||||||||||||
| Marital status ^^ | ||||||||||||
| Married | -- | -- | -- | -- | −0.148 | −2.006, 1.709 | 0.948 | 0.862 | −1.930* | −3.780, −0.080 | 0.944 | 0.145 |
| Divorced | -- | -- | -- | -- | −0.830 | −4.091, 2.432 | 1.664 | 0.436 | −1.563 | −3.631, 0.505 | 1.055 | 0.210 |
| Separated | -- | -- | -- | -- | −1.655 | −4.032, 0.723 | 1.213 | 0.191 | −1.050 | −2.333, 0.233 | 0.655 | 0.350 |
| Living together as married | -- | -- | -- | -- | −0.655 | −2.530, 1.220 | 0.957 | 0.519 | −1.357 * | −2.642, −0.071 | 0.656 | 0.257 |
| Single (ref) | ||||||||||||
| Income | 0.526 | −0.153, 1.206 | 0.347 | 1.692 | 0.504 | −0.699, 1.706 | 0.614 | 1.655 | 0.001 ** | 0.000, 0.001 | <0.001 | 1.001 |
| Religiosity | 0.112 | −0.043, 0.267 | 0.079 | 1.119 | 0.123 | −0.167, 0.412 | 0.148 | 1.131 | 0.173 | −0.054, 0.401 | 0.116 | 1.1889 |
| Trust in others | ||||||||||||
| Yes | −0.874 *** | −1.265, −0.483 | 0.199 | 0.417 | −1.252 ** | −1.978, −0.526 | 0.370 | 0.286 | −0.939 *** | −1.257, −0.621 | 0.162 | 0.391 |
| Membership of an association | ||||||||||||
| Yes | −0.297 | −0.704, 0.110 | 0.208 | 0.743 | -- | -- | -- | 0.161 | −0.315, 0.637 | 0.243 | 1.175 | |
| SES | -- | -- | -- | -- | -- | -- | −0.221 ** | −0.361, −0.082 | 0.071 | 0.802 | ||
| Cultural values | 0.276 *** | 0.113, 0.439 | 0.083 | 1.318 | 0.357** | 0.065, 0.650 | 0.149 | 1.429 | 0.378 ** | 0.156, 0.601 | 0.114 | 1.459 |
| Area of residency | ||||||||||||
| Rural | -- | -- | -- | −0.025 | −0.685, 0.636 | 0.337 | 0.975 | -- | -- | -- | ||
| Urban (ref) | ||||||||||||
| Nurse Characteristics | ||||||||||||
| Practicing experience | -- | -- | -- | 0.612 ** | 0.386, 0.974 | 0.260 | 1.844 | −0.045 | −0.129, 0.038 | 0.043 | 0.956 | |
| Year of study | 0.244 * | 0.101, 0.568 | 0.094 | 1.276 | -- | -- | -- | -- | -- | -- | -- | |
| Type of nurse | ||||||||||||
| Student nurse | -- | -- | -- | -- | -- | −0.577 * | −0.912, −0.384 | 0.260 | 0.562 | |||
| Practising nurse (Ref) | ||||||||||||
| Educational attainment | ||||||||||||
| Certificate in nursing | −0.461 | −2.256, 1.334 | 0.916 | 0.631 | -- | -- | -- | -- | -- | -- | -- | |
| Diploma in nursing | −0.155 | −1.914, 1.604 | 0.898 | 0.856 | -- | -- | -- | -- | -- | -- | -- | |
| Bachelor’s degree | 0.030 | −1.785, 1.844 | 0.926 | 1.030 | -- | -- | -- | -- | -- | -- | -- | |
| Masters (ref) | ||||||||||||
| Health and health system | ||||||||||||
| Health status | -- | -- | -- | 0.158 | −0.180, 0.496 | 0.173 | 1.171 | 0.147 | −0.086, 0.381 | 0.119 | 1.158 | |
| Use of curative care use | −0.236 * | −0.457, −0.015 | 0.113 | 0.790 | -- | -- | −0.146 | 0.496, −0.205 | 0.179 | 0.864 | ||
| Physical activities | 0.175 | −0.078, 0.428 | 0.129 | 1.191 | -- | -- | -- | |||||
| Nagelkerke’s R2 | 0.263 | 0.245 | 0.275 | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koduah, A.O.; Amoah, P.A.; Nkansah, J.O.; Leung, A.Y.M. A Comparative Analysis of Student and Practising Nurses’ Health Literacy Knowledge in Ghana. Healthcare 2021, 9, 38. https://doi.org/10.3390/healthcare9010038
Koduah AO, Amoah PA, Nkansah JO, Leung AYM. A Comparative Analysis of Student and Practising Nurses’ Health Literacy Knowledge in Ghana. Healthcare. 2021; 9(1):38. https://doi.org/10.3390/healthcare9010038
Chicago/Turabian StyleKoduah, Adwoa Owusuaa, Padmore Adusei Amoah, Jacob Oppong Nkansah, and Angela Y. M. Leung. 2021. "A Comparative Analysis of Student and Practising Nurses’ Health Literacy Knowledge in Ghana" Healthcare 9, no. 1: 38. https://doi.org/10.3390/healthcare9010038
APA StyleKoduah, A. O., Amoah, P. A., Nkansah, J. O., & Leung, A. Y. M. (2021). A Comparative Analysis of Student and Practising Nurses’ Health Literacy Knowledge in Ghana. Healthcare, 9(1), 38. https://doi.org/10.3390/healthcare9010038






