Designing a Randomized Trial with an Age Simulation Suit—Representing People with Health Impairments
Abstract
1. Introduction
- (1)
- confirming the use of GERT as a possible way to retrieve reference data by reducing the physical performance of young and healthy participants and consequently generating pilot data; therefore, the generated data is compared with previously collected physical activity data on real patients with chronic heart failure,
- (2)
- examining, how subjective experience and well-being influence the objective physiological parameters under two kinds of physical activity while wearing GERT and
- (3)
- evaluating several sensors/fitness trackers regarding their usability to perform measurements to obtain a part of the reference data.
2. Materials and Methods
2.1. The Age Simulation Suit GERT
2.2. Participants
- persons who already have physical (i.e., cardiovascular), neurological (i.e., epilepsy) or psychological diseases,
- pregnant women,
- persons with electrical or metallic implants and
- persons with other acute diseases or impairments which might endanger their own safety, present a risk of contagion or affect their mobility.
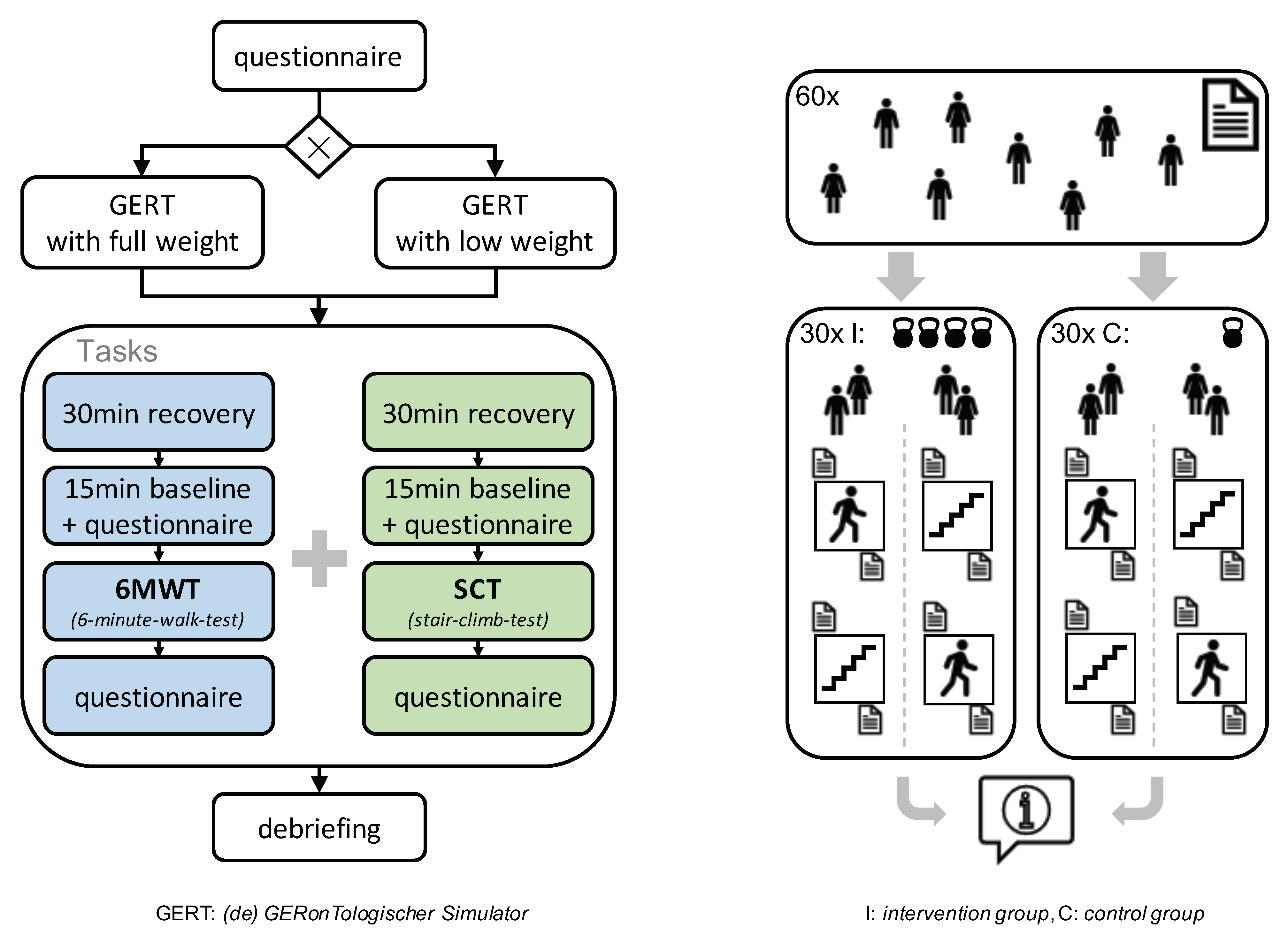
2.3. Experiment Plan
2.4. Questionnaires
2.5. Analysis Plan
3. Conclusions
4. Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rothgang, H.; Müller, R.; Unger, R. Themenreport “Pflege 2030”: Was ist zu erwarten-was ist zu tun? Bertelsmann Stiftung, 2012. Available online: https://www.bertelsmann-stiftung.de/fileadmin/files/BSt/Publikationen/GrauePublikationen/GP_Themenreport_Pflege_2030.pdf (accessed on 29 December 2020).
- Statistisches Bundesamt. Pflege im Rahmen der Pflegeversicherung Deutschlandergebnisse. Pflegestatistik 2013. Available online: https://www.statistischebibliothek.de/mir/receive/DEHeft_mods_00028953 (accessed on 29 December 2020).
- Statistisches Bundesamt. Pflege im Rahmen der Pflegeversicherung Deutschlandergebnisse. Pflegestatistik 2015. Available online: https://www.statistischebibliothek.de/mir/receive/DEHeft_mods_00096673 (accessed on 29 December 2020).
- Global Issues: Ageing. 2017. Available online: www.un.org/en/sections/issues-depth/ageing/ (accessed on 18 February 2020).
- Schwinger, A.; Tsiasioti, C. Pflegebedürftigkeit in Deutschland; Pflege-Report 2018; Springer: Berlin/Heidelberg, Germany, 2018; pp. 173–204. [Google Scholar]
- Bean, J.; Kiely, D.K.; Leveille, S.G.; Morris, J. Associating the onset of motor impairments with disability progression in nursing home residents. Am. J. Phys. Med. Rehabil. 2002, 81, 696–704. [Google Scholar] [CrossRef]
- Downing, J.; Balady, G.J. The role of exercise training in heart failure. J. Am. Coll. Cardiol. 2011, 58, 561–569. [Google Scholar] [CrossRef]
- McMurray, J.J.V.; Adamopoulos, S.; Anker, S.D.; Auricchio, A.; Böhm, M.; Dickstein, K.; Falk, V.; Filippatos, G.; Fonseca, C.; Gomez Sanchez, M.A.; et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012. Rev. Esp. Cardiol. 2012, 65, 938. [Google Scholar] [CrossRef]
- Jeong, S.W.; Kim, S.H.; Kang, S.H.; Kim, H.J.; Yoon, C.H.; Youn, T.J.; Chae, I.H. Mortality reduction with physical activity in patients with and without cardiovascular disease. Eur. Heart J. 2019, 40, 3547–3555. [Google Scholar] [CrossRef]
- Braude, P.; Reedy, G.; Dasgupta, D.; Dimmock, V.; Jaye, P.; Birns, J. Evaluation of a simulation training programme for geriatric medicine. Age Ageing 2015, 44, 677–682. [Google Scholar] [CrossRef]
- Fisher, J.M.; Walker, R.W. A new age approach to an age old problem: Using simulation to teach geriatric medicine to medical students. Age Ageing 2014, 43, 424–428. [Google Scholar] [CrossRef]
- Smith, D.; Meshkati, N.; Robertson, M. Automotive Ergonomics. Chapter 21. The Older Driver and Passenger; Publication of Taylor And Francis Ltd.: Abingdon, UK, 1993. [Google Scholar]
- Madden, D.J. Adult age differences in the attentional capacity demands of visual search. Cogn. Dev. 1986, 1, 335–363. [Google Scholar] [CrossRef]
- Hitchcock, D.R.; Lockyer, S.; Cook, S.; Quigley, C. Third age usability and safety—An ergonomics contribution to design. Int. J. Hum.-Comput. Stud. 2001, 55, 635–643. [Google Scholar] [CrossRef]
- Groza, H.; Sebesi, S.; Mandru, D. Age simulation suits for training, research and development. In Proceedings of the International Conference on Advancements of Medicine and Health Care through Technology, Cluj-Napoca, Romania, 12–15 October 2016; Vlad, S., Roman, N., Eds.; Springer: Cham, Switzerland, 2017; pp. 77–80. [Google Scholar]
- Oikonomou, T.; Votis, K.; Tzovaras, D.; Korn, P.S.C. International Conference on Universal Access in Human-Computer Interaction; Springer: Berlin/Heidelberg, Germany, 2009; pp. 135–144. [Google Scholar]
- Prindle, D. Hands on: Genworth R70i Exoskeleton. 2016. Available online: https://www.digitaltrends.com/cool-tech/genworth-r70i-exoskeleton/ (accessed on 30 September 2020).
- Vieweg, J.; Schaefer, S. How an Age Simulation Suit affects Motor and Cognitive Performance and Self-perception in Younger Adults. Exp. Aging Res. 2020, 46, 273–290. [Google Scholar] [CrossRef]
- Scherf, C. Entwicklung, Herstellung und Evaluation des Modularen AlterssimulationsanzugseXtra (MAX). 2014. Available online: https://nbn-resolving.org/urn:nbn:de:bsz:ch1-qucosa-139623 (accessed on 18 December 2020).
- Lee, S.W.H.; Teh, P.L. “Suiting Up” to Enhance Empathy Toward Aging: A Randomized Controlled Study. Front. Public Health 2020, 8, 376. [Google Scholar] [CrossRef]
- Lauenroth, A.; Schulze, S.; Ioannidis, A.; Simm, A.; Schwesig, R. Effect of an Age Simulation Suit on Younger Adults’ Gait Performance Compared to Older Adults’ Normal Gait. Res. Gerontol. Nurs. 2017, 10, 227–233. [Google Scholar] [CrossRef]
- Lavalliere, M.; D’Ambrosio, L.; Gennis, A.; Burstein, A.; Godfrey, K.M.; Waerstad, H.; Puleo, R.M.; Lauenroth, A.; Coughlin, J.F. Walking a mile in another’s shoes: The impact of wearing an age suit. Gerontol. Geriatr. Educ. 2017, 38, 171–187. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Wang, Y.C.; Gershon, R.C. Two-minute walk test performance by adults 18 to 85 years: Normative values, reliability, and responsiveness. Arch. Phys. Med. Rehabil. 2015, 96, 472–477. [Google Scholar] [CrossRef]
- Steffen, T.M.; Hacker, T.A.; Mollinger, L. Age-and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speed. Phys. Ther. 2002, 82, 128–137. [Google Scholar]
- Stephens, J.M.; Goldie, P.A. Walking speed on parquetry and carpet after stroke: Effect of surface and retest reliability. Clin. Rehabil. 1999, 13, 171–181. [Google Scholar] [CrossRef]
- Moll, W. Produkt + Projekt. Available online: https://www.produktundprojekt.de/alterssimulationsanzug/alterssimulationsanzug.html (accessed on 30 September 2020).
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Kirk, R.E. Experimental design. In Handbook of Psychology, 2nd ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2012; Volume 2. [Google Scholar]
- Pollentier, B.; Irons, S.L.; Benedetto, C.M.; DiBenedetto, A.M.; Loton, D.; Seyler, R.D.; Tych, M.; Newton, R.A. Examination of the six minute walk test to determine functional capacity in people with chronic heart failure: A systematic review. Cardiopulm. Phys. Ther. J. 2010, 21, 13. [Google Scholar] [CrossRef]
- Bennell, K.; Dobson, F.; Hinman, R. Measures of physical performance assessments: Self-Paced Walk Test (SPWT), Stair Climb Test (SCT), Six-Minute Walk Test (6MWT), Chair Stand Test (CST), Timed Up & Go (TUG), Sock Test, Lift and Carry Test (LCT), and Car Task. Arthritis Care Res. 2011, 63, S350–S370. [Google Scholar]
- Tan, F.; Aziz, A.R.; Teh, K.C.; Chia, M. Reliability of the stair-climb test (SCT) of cardiorespiratory fitness. Adv. Exerc. Sports Physiol. 2004, 10, 77–83. [Google Scholar]
- Ahmad, S.; Brown, A.; King, C.; Shlobin, O.; Weir, N.; Stayrook, S.; Nathan, S. The six minute walk test comparison to a stair climb test. Eur. Respir. J. 2015, 46, PA2239. [Google Scholar]
- Iijima, H.; Shimoura, K.; Eguchi, R.; Aoyama, T.; Takahashi, M. Concurrent validity and measurement error of stair climb test in people with pre-radiographic to mild knee osteoarthritis. Gait Posture 2019, 68, 335–339. [Google Scholar] [CrossRef]
- Schulz, K.F.; Grimes, D.A. Reihe Epidemiologi 6: Generierung von Randomisierungslisten in randomisierten Studien: Zufall, nicht Auswahl. Z. Arztl. Fortbild. Qual. Gesundheitswesen-Ger. J. Qual. Health Care 2007, 101, 419–426. [Google Scholar]
- Move 3–Aktivitätssensor. Available online: https://www.movisens.com/de/produkte/aktivitatssensor-move-3/ (accessed on 20 August 2020).
- Tao, W.; Liu, T.; Zheng, R.; Feng, H. Gait analysis using wearable sensors. Sensors 2012, 12, 2255–2283. [Google Scholar] [CrossRef]
- Xie, J.; Wen, D.; Liang, L.; Jia, Y.; Gao, L.; Lei, J. Evaluating the validity of current mainstream wearable devices in fitness tracking under various physical activities: Comparative study. JMIR mHealth uHealth 2018, 6, e94. [Google Scholar] [CrossRef]
- El-Amrawy, F.; Nounou, M.I. Are currently available wearable devices for activity tracking and heart rate monitoring accurate, precise, and medically beneficial? Healthc. Inform. Res. 2015, 21, 315–320. [Google Scholar] [CrossRef]
- Borg, G. Anstrengungsempfinden und körperliche Aktivität. Deutsches Ärzteblatt 2004, 101, 1016–1021. [Google Scholar]
- Kleinert, J. Adjektivliste zur Erfassung der wahrgenommenen körperlichen Verfassung (WKV): Skalenkonstruktion und erste psychometrische Befunde. Z. Sportpsychol. 2006, 13, 156–164. [Google Scholar] [CrossRef]
- Krohne, H.W.; Egloff, B.; Kohlmann, C.W.; Tausch, A. Untersuchung mit einer deutschen Form der Positive und Negative Affect Schedule. Diagnostika 1996, 42, 139–156. [Google Scholar]
- Leue, A.; Beauducel, A. The PANAS structure revisited: On the validity of a bifactor model in community and forensic samples. Psychol. Assess. 2011, 23, 215–225. [Google Scholar] [CrossRef]
- Wilhelm, P.; Schoebi, D. Assessing Mood in Daily Life: Structural Validity, Sensitivity to Change, and Reliability of a Short-Scale to Measure Three Basic Dimensions of Mood. Eur. J. Psychol. Assess. 2007, 23, 258–267. [Google Scholar] [CrossRef]
- Hoffmann, J.M.; Hellwig, S.; Brandenburg, V.M.; Spaderna, H. Measuring fear of physical activity in patients with heart failure. Int. J. Behav. Med. 2018, 25, 294–303. [Google Scholar] [CrossRef]
- Hoffmann, J.M.; Finke, J.B.; Schächinger, H.; Schulz, A.; Vögele, C.; Spaderna, H. Modulation of startle and heart rate responses by fear of physical activity in patients with heart failure and in healthy adults. Physiol. Behav. 2020, 225, 113044. [Google Scholar] [CrossRef]
- Spaderna, H.; Hoffman, J.M.; Hellwig, S.; Brandenburg, V.M. Fear of physical activity, anxiety, and depression: Barriers to physical activity in outpatients with heart failure? Eur. J. Health Psychol. 2020, 27, 3–13. [Google Scholar] [CrossRef]
- Fuchs, R.; Klaperski, S.; Gerber, M.; Seelig, H. Messung der bewegungs-und sportaktivität mit dem BSA-fragebogen: Eine methodische zwischenbilanz. Z. Gesundheitspsychologie 2015, 23, 60–76. [Google Scholar] [CrossRef]
- Krohne, H.W.; Egloff, B. Das Angstbewältigungs-Inventar (ABI); Swets Test Services: Frankfurt am Main, Germany, 1999. [Google Scholar]
- Krohne, H.W.; Egloff, B.; Varner, L.J.; Burns, L.R.; Weidner, G.; Ellis, H.C. The assessment of dispositional vigilance and cognitive avoidance: Factorial structure, psychometric properties, and validity of the Mainz Coping Inventory. Cogn. Ther. Res. 2000, 24, 297–311. [Google Scholar] [CrossRef]
- Gross, M.; Lindemann, U.; Kampe, K.; Dautel, A.; Kohler, M.; Albrecht, D.; Büchele, G.; Hautzinger, M.; Becker, C.; Pfeiffer, K. German version of the outcome expectations for exercise scale-2: Psychometric properties in geriatric patients after hip or pelvic fractures with fear of falling. Z. Gerontol. Geriatr. 2020. [Google Scholar] [CrossRef]
- R: The R Project for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 18 December 2020).
- Poulain, M.; Durand, F.; Palomba, B.; Ceugniet, F.; Desplan, J.; Varray, A.; Préfaut, C. 6-minute walk testing is more sensitive than maximal incremental cycle testing for detecting oxygen desaturation in patients with COPD. Chest 2003, 123, 1401–1407. [Google Scholar] [CrossRef]
- Gentner, T.; Neitzel, T.; Schulze, J.; Buettner, R. A Systematic Literature Review of Medical Chatbot Research from a Behavior Change Perspective. In Proceedings of the 2020 IEEE 44th Annual Computers, Software, and Applications Conference (COMPSAC), Madrid, Spain, 13–17 July 2020; pp. 735–740. [Google Scholar]
- Rodermund, S.C.; Lorig, F.; Timm, I.J. Ethical Challenges in Modeling and Simulation of Nudging in Care. In Proceedings of the First International Workshop on Ethics and Morality in Business Informatics/Ethik und Moral in der Wirtschaftsinformatik (EMoWI’19), Siegen, Germany, 24 February 2019; pp. 35–41. [Google Scholar]
- King, A.; Ahn, D.; Oliveira, B.; Atienza, A.; Castro, C.; Gardner, C. Promoting Physical Activity Through Hand-Held Computer Technology. Am. J. Prev. Med. 2008, 34, 138–142. [Google Scholar] [CrossRef]
- Brach, M.; hauer, K.; Korn, P.; Konrad, R.; Unkauf, S.; Hardy, S.; Göbel, S. Motivotion60+: Entwicklung eines computeranimierten Systems zum Kraft- und Balancetraining für Senioren (P53). In Proceedings of the Technik für ein selbstbestimmtes Leben (AAL 2012): 5 Deutscher AAL-Kongress, Berlin, Germany, 18 January 2012. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Timm, I.J.; Spaderna, H.; Rodermund, S.C.; Lohr, C.; Buettner, R.; Berndt, J.O. Designing a Randomized Trial with an Age Simulation Suit—Representing People with Health Impairments. Healthcare 2021, 9, 27. https://doi.org/10.3390/healthcare9010027
Timm IJ, Spaderna H, Rodermund SC, Lohr C, Buettner R, Berndt JO. Designing a Randomized Trial with an Age Simulation Suit—Representing People with Health Impairments. Healthcare. 2021; 9(1):27. https://doi.org/10.3390/healthcare9010027
Chicago/Turabian StyleTimm, Ingo J., Heike Spaderna, Stephanie C. Rodermund, Christian Lohr, Ricardo Buettner, and Jan Ole Berndt. 2021. "Designing a Randomized Trial with an Age Simulation Suit—Representing People with Health Impairments" Healthcare 9, no. 1: 27. https://doi.org/10.3390/healthcare9010027
APA StyleTimm, I. J., Spaderna, H., Rodermund, S. C., Lohr, C., Buettner, R., & Berndt, J. O. (2021). Designing a Randomized Trial with an Age Simulation Suit—Representing People with Health Impairments. Healthcare, 9(1), 27. https://doi.org/10.3390/healthcare9010027




