Do Health Professionals Sufficiently Address Patients’ Disposition Toward Changing Their Nutritional and Physical Activity Habits? Findings from a Pilot Study among People with Type 2 Diabetes in Northern Italy
Abstract
1. Introduction
2. Material and Methods
2.1. Population
2.2. Data Collection and Participation
2.3. Instrument
2.4. Statistical Analysis
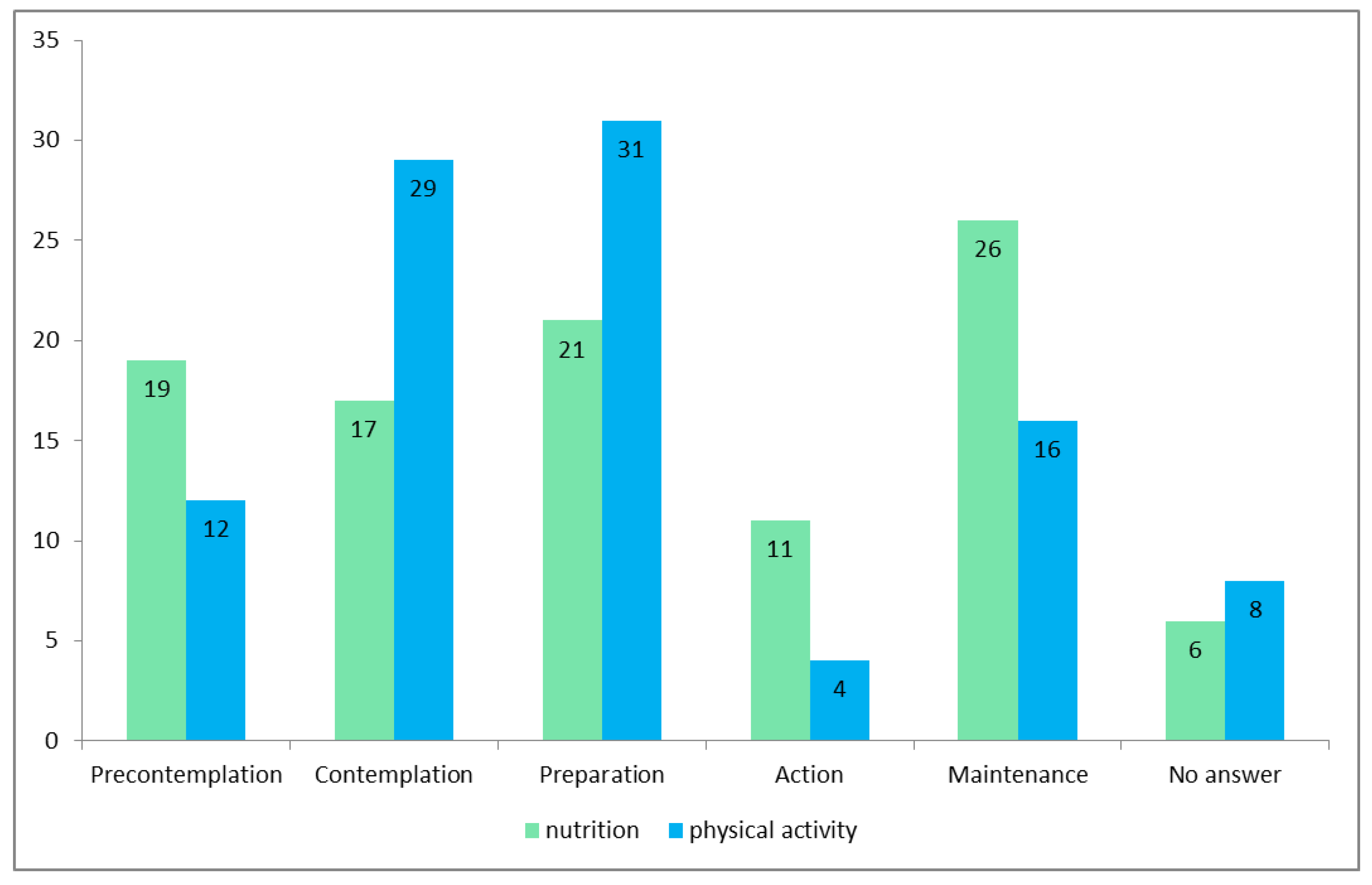
3. Results
- Use more supportive psychological processes such as self-efficacy;
- Have higher health literacy;
- Have better clinical status for both habits.
4. Discussion
5. Strength and Limitations
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethical Issues
References
- Bonora, E.; Sesti, G. Il Diabete in Italia, 1st ed.; Società Ialiana di Diabetologia: Bologna, Italy, 2016. [Google Scholar]
- Sinclair, A.; Dunning, T.; Colagiuri, S. International Diabetes Federation: Managing Older People with Type 2 Diabetes. In Global Guideline; IDF: Brussels, Belgium, 2013. [Google Scholar]
- NICE. Type 2 Diabetes in Adults: Management, National Institute for Health and Care Excellence. Available online: nice.org.uk/guidance/ng28 (accessed on 25 November 2020).
- World Health Organization. Global Report on Diabetes; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Triad Study Group. Health systems, patients factors, and quality of care for diabetes: A synthesis of findings from the TRIAD study. Diabetes Care 2010, 33, 940–947. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C.A.; Shaw, R.L.; Dale, J.; French, D.P. Enhancing delivery of health behaviour change interventions in primary care: A meta-synthesis of views and experiences of primary care nurses. Patient Educ. Couns. 2011, 85, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.L.; Pan, J.H.; Chen, D.; Chen, J.; Chen, F.; Hu, T.T. Efficacy of lifestyle interventions in patients with type 2 diabetes: A systematic review and meta-analysis. Eur. J. Intern. Med. 2016, 27, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Gregg, E.W.; Look AHEAD Research Group. Association of magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: A post-hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2016, 4, 913–921. [Google Scholar]
- Ministero Della Salute. Piano sulla Malattia Diabetica. In Direzione Generale Per La Programmazione Sanitaria; Commissione Nazionale Diabete: Roma, Italy, 2013; pp. 1–78. [Google Scholar]
- Chisholm, A.; Hart, J.; Lam, V.; Peters, S. Current challenges of behavior change talk for medical professionals and trainees. Patient Educ. Couns. 2012, 87, 389–394. [Google Scholar] [CrossRef]
- Frates, E.; Bonnet, J. Collaboration and Negotiation: The key to therapeutic lifestyle change. Am. J. Lifestyle Modif. 2016, 10, 302–312. [Google Scholar] [CrossRef]
- Nicolucci, A.; Kovacs Burns, K.; Holt, R.I.G.; Comaschi, M.; Hermanns, N.; Ishii, H.; Kokoszka, A.; Pouwer, F.; Skovlund, S.E.; Stuckey, H.; et al. Diabetes Attitudes, Wishes and Needs second study (DAWN2): Cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes. Diabet. Med. 2013, 30, 767–777. [Google Scholar] [CrossRef]
- Kelly, M.P.; Barker, M. Why is changing health-related behaviour so difficult? Public Health 2016, 136, 109–116. [Google Scholar] [CrossRef]
- Davis, R.; Campbell, R.; Hildon, Z.; Hobbs, L.; Michie, S. Theories of behaviour and behaviour change across the social and behavioural sciences: A scoping review. Health Psychol. Rev. 2015, 9, 323–344. [Google Scholar] [CrossRef]
- Prochaska, J.O.; DiClemente, C.C.; Norcross, J.C. In search of how people change: Applications to addictive behaviors. Am. Psychol. 1992, 47, 1102–1114. [Google Scholar] [CrossRef]
- Prochaska, J.O. Strong and weak principles for progressing from precontemplation to action on the basis of twelve problem behaviors. Health Psychol. 1994, 13, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.O.; Velicer, W.F. The transtheoretical model of health behavior change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.O.; Velicer, W.F.; Rossi, J.S.; Goldstein, M.G.; Marcus, B.H.; Rakowski, W.; Fiore, C.; Harlow, L.L.; Redding, C.A.; Rosenbloom, D.; et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychol. 1994, 13, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Greene, G.W.; Redding, C.A.; Prochaska, J.O.; Paiva, A.L.; Rossi, J.S.; Velicer, W.F.; Blissmer, B.; Robbins, M.L. Baseline transtheoretical and dietary behavioral predictors of dietary fat moderation over 12 and 24 months. Eat. Behav. 2013, 14, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Lipschitz, J.M.; Yusufov, M.; Paiva, A.; Redding, C.A.; Rossi, J.S.; Johnson, S.; Prochaska, J.O. Transtheoretical principles and processes for adopting physical activity: A longitudinal 24-month comparison of maintainers, relapser, and nonchangers. J. Sport Exerc. Psychol. 2015, 37, 592–606. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.O.; Norcrosss, J.C.; DiClemente, C. Applying the stages of change. Psychother. Aust. 2013, 19, 10–15. [Google Scholar]
- Bandura, A. Self-efficacy: Towards a unifying theory of behavioural change. Adv. Behav. Res. Ther. 1978, 1, 139–161. [Google Scholar] [CrossRef]
- Janis, I.L.; Mann, L. Decision Making: A Psychological Analysis of Conflict, Choice, and Commitment; Free Press: New York, NY, USA, 1977. [Google Scholar]
- Arafat, Y.; Izham, M.; Ibrahim, M.; Awaisu, A. Using the transtheoretical model to enhance self-management activities in patients with type 2 diabetes: A systematic review. J. Pharm. Health Serv. Res. 2016, 7, 149–156. [Google Scholar] [CrossRef]
- Kirk, A.; MacMillan, F.; Webster, N. Application of the transtheoretical model to physical activity in older adults with type 2 diabetes and/or cardiovascular disease. Psychol. Sport Exerc. 2010, 11, 320–324. [Google Scholar] [CrossRef]
- Guicciardi, M.; Lecis, R.; Anziani, C.; Corgiolu, L.; Porru, A.; Pusceddu, M.; Spanu, F. Type 2 diabetes mellitus, physical activity, exercise self-efficacy, and body satisfaction: An application of the transtheoretical model in older adults. Health Psychol. Behav. Med. 2014, 2, 748–758. [Google Scholar] [CrossRef]
- Ataee, M.; ZinatMotlagh, F.; Aghaei, A.; Mohammadi, M.R.; Mahboubi, M.; Ahmadi-Jouybari, T.; Shamohammadi, Z. Understanding physical activity behavior among Iranian type 2 diabetes patients: A test of the transtheoretical model. J. Biol. Today World 2014, 3, 53–56. [Google Scholar]
- Nagaraju, A.S.; Tondore, D.; Gopichandran, V. What makes patients with diabetes adopt physical activity behaviors? A transtheoretical model approach. J. Diabetes Dev. Ctries. 2019, 39, 739–748. [Google Scholar] [CrossRef]
- Centis, E.; Trento, M.; Dei Cas, A.; Pontiroli, A.E.; De Feo, P.; Bruno, A.; Sasdelli, A.S.; Arturi, F.; Strollo, F.; Kreutzenberg, S.V.D.; et al. Stage of change and motivation to healthy diet and habitual physical activity in type 2 diabetes. Acta Diabetol. 2014, 51, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.R.; Rollnick, S. What is motivational interviewing? Behav. Cogn. Psychother. 1995, 23, 325–334. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. Ten Things that motivational interviewing is not. Behav. Cogn. Psychother. 2009, 37, 129–140. [Google Scholar] [CrossRef]
- Spiller, V.; Scaglia, M.; Meneghini, S.; Vanzo, A. Assessing motivation to change towards healthy nutrition and regular physical activity. Validation of two sets of instruments. Mediterr. J. Nutr. Metab. 2009, 2, 41–47. [Google Scholar] [CrossRef]
- Wieser, H.; Piccoliori, G.; Siller, M.; Comploj, E.; Stummer, H. Living on the Own Island? Aligned Collaboration Between Family Physicians, Nurses, Dieticians, and Patients With Diabetes Type 2 in an Outpatient Care Setting in Northern Italy: Findings From a Qualitative Study. Glob. Adv. Health Med. 2020, 16, 1–10. [Google Scholar] [CrossRef]
- Ishikawa, H.; Takeuchi, T.; Yano, E. Measuring functional, communicative, and critical health literacy among diabetic patients. Diabetes Care 2008, 31, 874–879. [Google Scholar] [CrossRef]
- Dwinger, S.; Kriston, L.; Härter, M.; Dirmaier, J. Translation and validation of a multidimensional instrument to assess health literacy. Health Expect. 2015, 18, 2776–2786. [Google Scholar] [CrossRef]
- Wild, D.; Grove, A.; Martin, M.; Eremenco, S.; McElroy, S.; Verjee-Lorenz, A.; Erikson, P. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) measures: Report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health 2005, 8, 94–104. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Ashwell, M.; Gibson, S. Waist-to-height ratio as an indicator of ‘early health risk’: Simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open 2016, 6, e010159. [Google Scholar] [CrossRef] [PubMed]
- Jones, H.; Edwards, L.; Vallis, T.M.; Ruggiero, L.; Rossi, S.R.; Rossi, J.S.; Greene, G.; Prochaska, J.O.; Zinman, B. Changes in diabetes self-care behaviors make a difference in glycemic control. Diabetes Care 2003, 26, 732–737. [Google Scholar] [CrossRef] [PubMed]
| (a) | |
| Variable | Frequency (%) |
| Sex | |
| Male | 57 |
| Female | 40 |
| Missing | 3 |
| Age group (in years) | |
| <64 | 13 |
| 65–69 | 20 |
| ≥70 | 65 |
| Missing | 2 |
| Level of education1 | |
| Compulsory school degree | 53 |
| Secondary or higher degree | 47 |
| Self-evaluation of economic status | |
| Insufficient | 6 |
| Average | 78 |
| Good | 16 |
| Occupational status | |
| Active | 13 |
| Retired | 87 |
| Cohabitation status | |
| Living alone | 16 |
| Living with someone | 78 |
| Missing | 6 |
| Frequency of contact with health the following professions 2 | |
| General practitioner | |
| Never | 27 |
| 1 or 2 times per year | 42 |
| 3 or more times per year | 30 |
| Missing | 1 |
| Nurse in outpatient care | |
| Never | 66 |
| 1 or 2 times per year | 21 |
| 3 or more times per year | 9 |
| Missing | 4 |
| Nurse at hospital | |
| Never | 23 |
| 1 or 2 times per year | 59 |
| 3 or more times per year | 16 |
| Missing | 2 |
| Dietician in outpatient care | |
| Never | 82 |
| 1 or 2 times per year | 10 |
| 3 or more times per year | 5 |
| Missing | 3 |
| Dietician at hospital | |
| Never | 78 |
| 1 or 2 times per year | 8 |
| 3 or more times per year | 12 |
| Missing | 4 |
| Diabetologist at hospital | |
| Never | 16 |
| 1 or 2 times per year | 61 |
| 3 or more times per year | 20 |
| Missing | 3 |
| (b) | |
| Variable | |
| Health literacy3 | |
| Low | 76 |
| High | 22 |
| Missing | 2 |
| Body mass index class * | |
| Normal | 31 |
| Overweight | 40 |
| Obese | 26 |
| Missing | 3 |
| Weight-to-height ratio *,4 | |
| <0.5 | 0 |
| 0.5–0.6 | 34 |
| >0.6 | 34 |
| Missing | 32 |
| Duration of diabetes | |
| <5 years | 11 |
| 5–10 years | 11 |
| >10 years | 78 |
| Insulin dependence? | |
| Yes | 42 |
| No | 57 |
| Missing | 1 |
| Regular self-measurement of blood glucose? | |
| Yes | 93 |
| No | 6 |
| HbA1c level5 | |
| Normal (<7.5) | 51 |
| Not normal (≥7.5) | 22 |
| Missing | 27 |
| Prescribed and taking medication? | |
| Yes | 91 |
| No | 7 |
| Missing | 2 |
| Presence of complications? | |
| Yes | 32 |
| No | 64 |
| Missing | 4 |
| Treatment for high blood pressure?6,7 | |
| Yes | 65 |
| No | 34 |
| Missing | 1 |
| Treatment for high cholesterol?7 | |
| Yes | 62 |
| No | 36 |
| Missing | 2 |
| Coronary heart disease? | |
| Yes | 23 |
| No | 75 |
| Missing | 2 |
| Participating in individual or group training? | |
| Yes | 48 |
| No | 52 |
| Stage of Change | Nutritional Habits | Physical Activity Habits | p | ||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| Precontemplation | 47.6 | ±25.0 | 27.3 | ±24.9 | <0.000 |
| Contemplation | 51.7 | ±25.3 | 50.3 | ±27.5 | 0.650 |
| Preparation | 53.3 | ±28.8 | 62.4 | ±28.2 | 0.030 |
| Action | 52.8 | ±25.9 | 42.0 | ±31.1 | 0.009 |
| Maintenance | 67.3 | ±22.6 | 58.8 | ±31.2 | 0.011 |
| Psychological process | |||||
| Discrepancy | 38.6 | ±23.0 | 42.5 | ±25.7 | 0.134 |
| Importance | 75.9 | ±17.0 | 74.8 | ±17.6 | 0.613 |
| Self-efficacy | 63.7 | ±21.1 | 61.8 | ±21.7 | 0.398 |
| Temptation | 51.1 | ±28.1 | 33.0 | ±23.8 | <0.000 |
| Readiness for change | 48.2 | ±28.6 | 63.8 | ±23.7 | <0.000 |
| Stability of change | 61.2 | ±24.3 | 58.7 | ±25.4 | 0.398 |
| (a) | ||
| Stage of Change or Psychological Process | Clinical or Sociodemographic Variable (Higher Mean Score of Stage of Change and Psychological Process) | p |
| Precontemplation | Sex (Male = 52.2) | 0.018 |
| HbA1c level1 (Not normal = 55.2) | 0.036 | |
| Contemplation | Cardiovascular disease2 (No = 55.3) | 0.036 |
| Attendance of a training course2 (No = 58.29) | 0.018 | |
| Preparation | Cardiovascular disease2 (No = 56.0) | 0.018 |
| Time since diagnosis3 (<10 years = 63.5) | 0.036 | |
| Action | Time since diagnosis3 (<10 years = 65.8) | 0.018 |
| Maintenance | Health literacy level4 (Well informed = 80.2) | 0.018 |
| Discrepancy | Sex (Female = 44.2) | 0.018 |
| HbA1c level1 (Not normal = 49.4) | 0.036 | |
| Temptation | Complications2 (Yes = 58.8) | 0.018 |
| Readiness for change | Sex (Female = 56.7) | 0.018 |
| (b) | ||
| Communication or Interaction Variable (Higher Mean Score of Stage of Change and Psychological Process) | p | |
| Precontemplation | We talk about my nutritional habits5 (DIAB) (Sometimes/Often = 51.1) | 0.012 |
| We talk about my physical activity habits5 (DIAB) (Sometimes/Often = 55.6) | 0.024 | |
| We talk about my physical activity habits5 (NH) (Sometimes/Often = 53.8) | 0.036 | |
| Contemplation | There is enough time for each meeting5 (NH) (Never/Rarely = 76.2) | 0.012 |
| Preparation | We decide together what changes I will undertake5 (NH) 1(Sometimes/Often = 61.3) | 0.012 |
| Maintenance | I feel that he or she understands me5 (NH) (Sometimes/Often = 71.3) | 0.012 |
| There is enough time for each meeting5 (NH) (Sometimes/Often = 71.7) | 0.024 | |
| Discrepancy | I feel that he or she understands me5 (GP) (Never/Rarely = 52.6) | 0.012 |
| Self-efficacy | I feel that he or she understands me5 (GP) 1 (Sometimes/Often = 66.3) | 0.012 |
| He or she listens to me carefully5 (NH) (Sometimes/Often = 67.4) | 0.024 | |
| Temptation | There is enough time for each meeting5 (NH) (Never/Rarely = 75.6) | 0.012 |
| We talk about my physical activity habits5 (GP) (Never/Rarely = 57.6) | 0.024 | |
| Stability of change | I feel that he or she understands me5 (GP) (Sometimes/Often = 64.7) | 0.012 |
| (a) | ||
| Stage of Change or Psychological Process | Clinical or Sociodemographic Variable (Higher Mean Score of Stage of Change or Psychological Process) | p |
| Precontemplation | Sex (Male = 32.5) | 0.018 |
| BMI class1 (Obese = 37.9) | 0.036 | |
| Contemplation | Self-evaluation of economic status2 (Insufficient = 59.7) | 0.018 |
| HL level3 (Poorly informed = 54.6) | 0.036 | |
| Preparation | BMI class1 (Normal = 69.3) | 0.018 |
| WtHR4 (Low risk = 73.4) | 0.036 | |
| Maintenance | HL level3 (Well informed = 72.6) | 0.018 |
| Discrepancy | Self-evaluation of economic status2 (Insufficient = 65.0) | 0.018 |
| WtHR4 (High risk = 49.4) | 0.036 | |
| Importance | WtHR4 (Low risk = 83.1) | 0.018 |
| HbA1c level5 (Normal = 78.7) | 0.036 | |
| Self-efficacy | WtHR4 (Low risk = 70.3) | 0.018 |
| BMI class1 (Normal = 71.0) | 0.036 | |
| Temptation | Age class6 (<70 years = 43.0) | 0.018 |
| Readiness for change | WtHR4 (Low risk = 72.0) | 0.018 |
| Stability of change | WtHR4 (Low risk = 68.6) | 0.018 |
| (b) | ||
| Communication or Interaction Variable (Higher Mean Score of Stage of Change or Psychological Process) | p | |
| Precontemplation | He or she allows me to ask questions7(NH) (Sometimes/Often = 28.6) | 0.012 |
| He or she listens to me carefully7 (NH) (Sometimes/Often = 27.2) | 0.024 | |
| I feel that he or she understands me7 (NH) (Sometimes/Often = 26.6) | 0.036 | |
| We decide together what changes I will undertake7(GP) (Sometimes/Often = 31.2) | 0.048 | |
| Discrepancy | I feel that he or she understands me7 (GP) (Never/Rarely = 54.8) | 0.012 |
| Self-efficacy | I feel that he or she understands me7 (GP) (Never/Rarely = 72.5) | 0.012 |
| We decide together what changes I will undertake7 (GP) (Never/Rarely = 68.2) | 0.024 | |
| Temptation | We talk about my physical activity habits7 (GP) (Never/Rarely = 40.4) | 0.012 |
| Psychological Processes | Nutritional Habits | Physical Activity Habits | ||||
|---|---|---|---|---|---|---|
| Passive Stage | Active Stage | p | Passive Stage | Active Stage | p | |
| Discrepancy | 49.2 | 31.9 | <0.000 | 56.9 | 31.0 | <0.000 |
| Importance | 67.8 | 81.3 | <0.000 | 68.3 | 80.2 | 0.001 |
| Self-efficacy | 48.8 | 73.0 | <0.000 | 52.2 | 70.5 | <0.000 |
| Temptation | 61.8 | 42.3 | 0.002 | 43.4 | 26.1 | <0.000 |
| Readiness for change | 44.3 | 51.6 | 0.145 | 54.3 | 71.9 | <0.000 |
| Stability of change | 47.2 | 70.2 | <0.000 | 45.5 | 69.4 | <0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wieser, H.; Vittadello, F.; Comploj, E.; Stummer, H. Do Health Professionals Sufficiently Address Patients’ Disposition Toward Changing Their Nutritional and Physical Activity Habits? Findings from a Pilot Study among People with Type 2 Diabetes in Northern Italy. Healthcare 2020, 8, 524. https://doi.org/10.3390/healthcare8040524
Wieser H, Vittadello F, Comploj E, Stummer H. Do Health Professionals Sufficiently Address Patients’ Disposition Toward Changing Their Nutritional and Physical Activity Habits? Findings from a Pilot Study among People with Type 2 Diabetes in Northern Italy. Healthcare. 2020; 8(4):524. https://doi.org/10.3390/healthcare8040524
Chicago/Turabian StyleWieser, Heike, Fabio Vittadello, Evi Comploj, and Harald Stummer. 2020. "Do Health Professionals Sufficiently Address Patients’ Disposition Toward Changing Their Nutritional and Physical Activity Habits? Findings from a Pilot Study among People with Type 2 Diabetes in Northern Italy" Healthcare 8, no. 4: 524. https://doi.org/10.3390/healthcare8040524
APA StyleWieser, H., Vittadello, F., Comploj, E., & Stummer, H. (2020). Do Health Professionals Sufficiently Address Patients’ Disposition Toward Changing Their Nutritional and Physical Activity Habits? Findings from a Pilot Study among People with Type 2 Diabetes in Northern Italy. Healthcare, 8(4), 524. https://doi.org/10.3390/healthcare8040524






