The Demand for Elective Neurosurgery at a German University Hospital during the First Wave of COVID-19
Abstract
1. Introduction
2. Methods
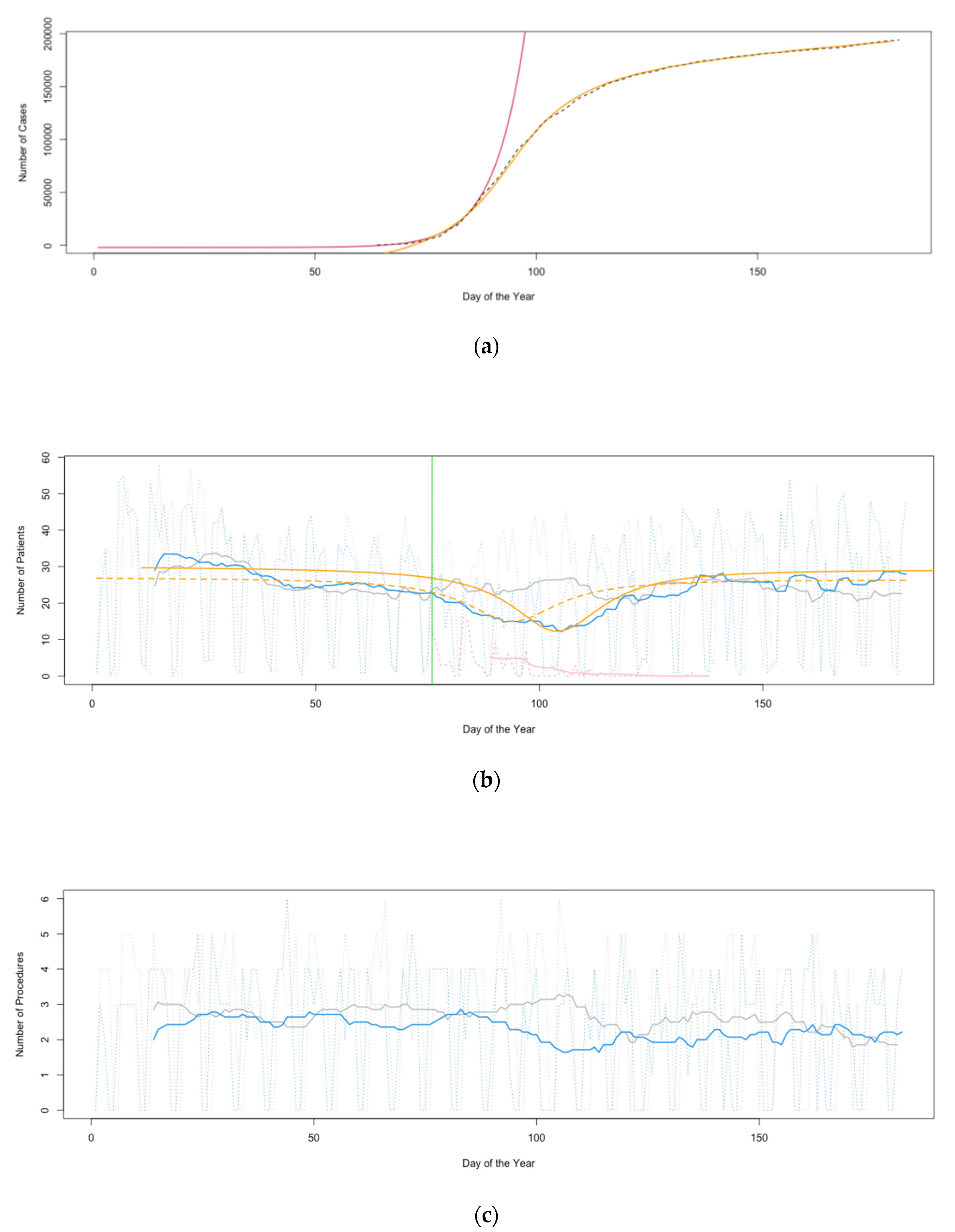
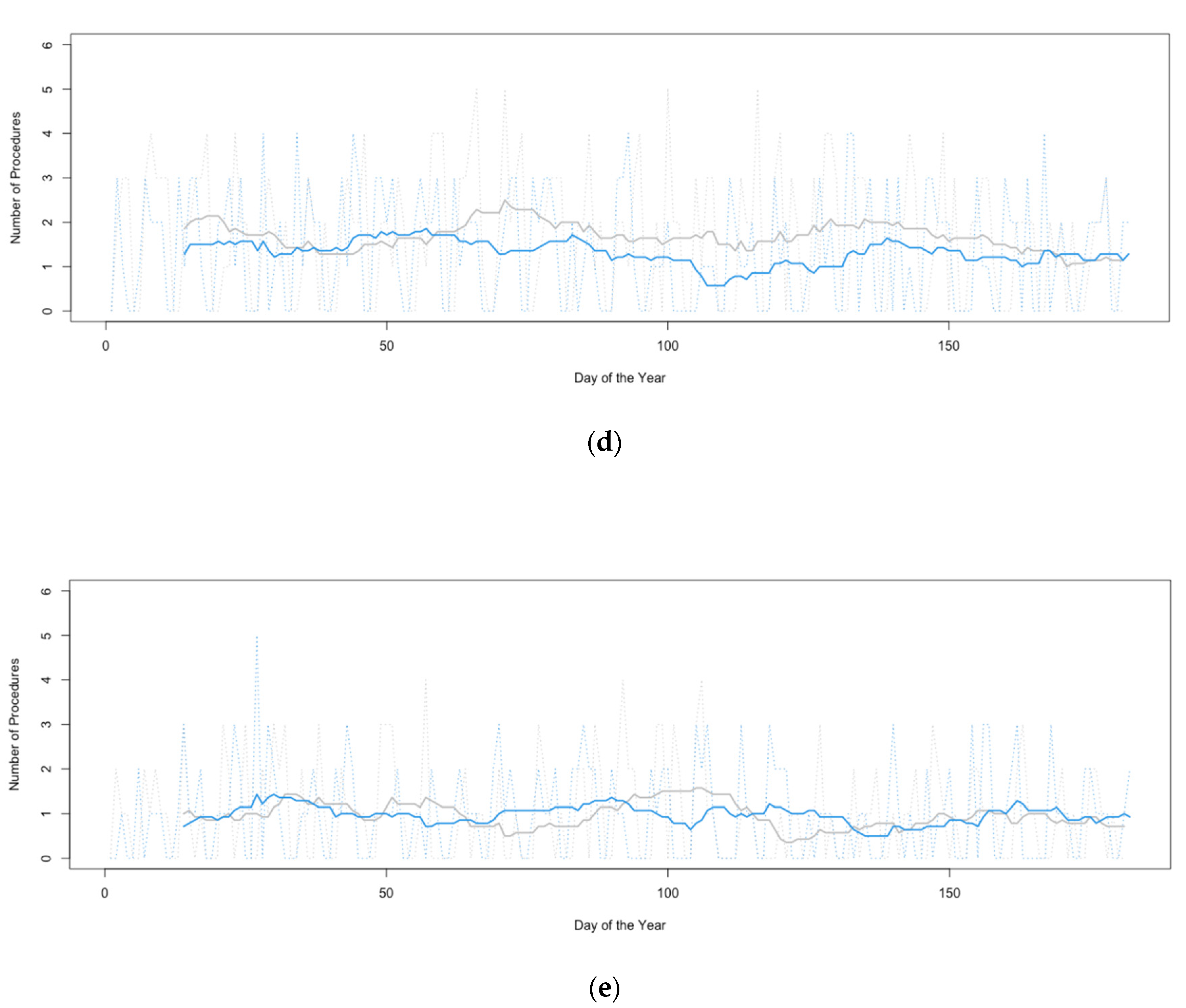
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wong, L.E.; Hawkins, J.E.; Langness, S.; Murrell, K.L.; Iris, P.; Sammann, A. Where Are All the Patients? Addressing COVID-19 Fear to Encourage Sick Patients to Seek Emergency Care. NEJM Catalyst 2020. [Google Scholar] [CrossRef]
- Pessoa-Amorim, G.; Camm, C.F.; Gajendragadkar, P.; De Maria, G.L.; Arsac, C.; Laroche, C.; Zamorano, J.L.; Weidinger, F.; Achenbach, S.; Maggioni, A.P.; et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: A survey by the European Society of Cardiology. Eur. Heart J. Qual. Care Clin. Outcomes 2020, 6, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Lazzerini, M.; Barbi, E.; Apicella, A.; Marchetti, F.; Cardinale, F.; Trobia, G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc. Health 2020, 4, e10–e11. [Google Scholar] [CrossRef]
- Karacin, C.; Bilgetekin, I.; Basal, F.B.; Oksuzoglu, O.B. How does COVID-19 fear and anxiety affect chemotherapy adherence in patients with cancer. Future Oncol. 2020, 16, 2283–2293. [Google Scholar] [CrossRef] [PubMed]
- Musche, V.; Bäuerle, A.; Steinbach, J.; Schweda, A.; Hetkamp, M.; Weismüller, B.; Kohler, H.; Beckmann, M.; Herrmann, K.; Tewes, M.; et al. COVID-19-Related Fear and Health-Related Safety Behavior in Oncological Patients. Front. Psychol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Deo, S.V.S.; Kumar, S.; Kumar, N.; Saikia, J.; Bhoriwal, S.; Bhatnagar, S.; Sharma, A. Guiding Principles for Cancer Surgery during the COVID-19 Pandemic. Indian J. Surg. Oncol. 2020, 6, 1–8. [Google Scholar] [CrossRef]
- Wilson, L.A.; Zhong, H.; Jashvant, P.; Liu, J.; Memtsoudis, S.G. Recommendations for resuming elective spine surgery in the COVID-19 era. Br. J. Anesth. 2020, 125, e339–e341. [Google Scholar] [CrossRef] [PubMed]
- Rizkalla, J.M.; Hotchkiss, W.; Clavenna, A.; Dossett, A.; Syed, I.Y. Triaging Spine Surgery and Treatment during the COVID-19 pandemic. J. Orthop. 2020, 20, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Hecht, N.; Wessels, L.; Werft, F.-O.; Schneider, U.C.; Czabanka, M.; Vajkoczy, P. Need for ensuring care for neuro-emergencies—lessons learned from the COVID-19 pandemic. Acta Neurochir. 2020, 162, 1795–1801. [Google Scholar] [CrossRef] [PubMed]
- Bundesregierung. Available online: http://www.bundesregierung.de (accessed on 12 November 2020).
- Robert Koch Institute (RKI). Available online: http://www.rki.de (accessed on 12 November 2020).
- R Studio. Available online: https://rstudio.com (accessed on 12 November 2020).
- The R Project. Available online: https://www.r-project.org (accessed on 12 November 2020).
- GIMP. Available online: https://www.gimp.org (accessed on 12 November 2020).
- Osterloh, F. Coronaausbruch im Krankenhaus: Ein Restrisiko bleibt bestehen. Dt. Ärztebl. 2020, 117, A-984/B-831. [Google Scholar]
- Mathiesen, T.; Arraez, M.; Asser, T.; Balak, N.; Barazi, S.; Bernucci, C.; Bolger, C.; Broekman, M.L.D.; Demetriades, A.K.; Feldman, Z.; et al. A snapshot of European neurosurgery December 2019 vs. March 2020: Just before and during the COVID-19 pandemic. Acta Neurochir. 2020, 162, 2221–2233. [Google Scholar] [CrossRef] [PubMed]
- Gross, R.E.; Buetefisch, C.M.; Miocinovic, S.; Bullinger, K.L.; Okun, M.S.; Ostrem, J.L.; Foote, K.D.; Starr, P.A. Letter: Evaluation and Surgical Treatment of Functional Neurosurgery Patients with Implanted Deep Brain Stimulation and Vagus Nerve Stimulation Pulse Generators During the COVID-19 Pandemic. Neurosurgery 2020, 87, E222–E226. [Google Scholar] [CrossRef]
- Coffey, A.; Leahy-Warren, P.; Savage, E.; Hegarty, J.; Cornally, N.; Day, M.R.; Sahm, L.; O’Connor, K.; O’Doherty, J.; Liew, A.; et al. Interventions to Promote Early Discharge and Avoid Inappropriate Hospital (Re) Admission: A Systematic Review. Int. J Environ. Res. Public Health 2019, 16, 2457. [Google Scholar] [CrossRef]
- Tahan, H.M. Essential Case Management Practices Amidst the Novel Coronavirus Disease 2019 (COVID-19) Crisis: Part 1. Prof. Case Manag. 2020, 25, 248–266. [Google Scholar] [CrossRef]
- Patel, P.D.; Kelly, K.A.; Reynolds, R.A.; Turer, R.W.; Salwi, S.; Rosenbloom, S.T.; Bonfield, C.M.; Naftel, R.P. Tracking the Volume of Neurosurgical Care During the Coronavirus Disease 2019 Pandemic. World Neurosurg. 2020, 142, e183–e194. [Google Scholar] [CrossRef] [PubMed]
- Daggubati, L.C.; Eichberg, D.G.; Ivan, M.E.; Hanft, S.; Mansouri, A.; Komotar, R.J.; D’Amico, R.S.; Zacharia, B.E. Telemedicine for Outpatient Neurosurgical Oncology Care: Lessons Learned for the Future During the COVID-19 Pandemic. World Neurosurg. 2020, 139, e859–e863. [Google Scholar] [CrossRef] [PubMed]
- Best, M.J.; McFarland, E.G.; Anderson, G.F.; Srikumaran, U. The likely economic impact of fewer elective surgical procedures on US hospitals during the COVID-19 pandemic. Surgery 2020, 168, 962–967. [Google Scholar] [CrossRef] [PubMed]
- von Dercks, N.; Seehofer, D.; Steinert, M.; Krämer, S.; Branzan, D.; Dietrich, A.; Schürmann, O.; Gockel, I. How severe is the effect of the coronavirus pandemic on the department of surgery of a university hospital? Der Chirurg 2020, 91, 755–761. [Google Scholar] [CrossRef] [PubMed]
| Numbers of Patients and Procedures | 2019 | 2020 | p Value |
|---|---|---|---|
| Outpatients, January | 931 | 950 | 0.773 |
| Outpatients, February | 660 | 695 | 0.909 |
| Outpatients, March | 677 | 596 | 0.225 |
| Outpatients, April | 748 | 531 | 0.010 (*) |
| Outpatients, May | 788 | 752 | 1 |
| Outpatients, June | 645 | 815 | 0.085 |
| Outpatients, January–June | 4449 | 4339 | 0.601 |
| Non-oncological elective procedures, January–June | 302 | 240 | 0.032 (*) |
| Oncological elective procedures, January–June | 171 | 174 | 0.697 |
| All elective procedures, January–June | 473 | 414 | 0.023 (*) |
| Main Indications | 2019 | 2020 | Test | p Value |
|---|---|---|---|---|
| March and April | March and April | |||
| Cranial EP | ||||
| Aphasia | 6 | 2 | Fisher’s exact | 0.287 |
| Functional | 18 | 7 | chi square | 0.0699 (§) |
| Hydrocephalus | 32 | 19 | chi square | 0.1507 |
| Incidentaloma | 16 | 6 | chi square | 0.0832 (§) |
| Infectious lesion | 2 | 3 | Fisher’s exact | 0.6679 |
| Motor deficit | 5 | 15 | chi square | 0.0167 (*) |
| Seizures | 8 | 12 | chi square | 0.3251 |
| Tumor progression | 6 | 8 | chi square | 0.6124 |
| Visual disturbance | 2 | 8 | Fisher’s exact | 0.0488 (*) |
| Other | 21 | 16 | ||
| Cranial EP, total | 116 | 103 | ||
| Spinal EP | ||||
| Infectious lesion | 13 | 5 | chi square | 0.3024 |
| Low back pain | 5 | 0 | Fisher’s exact | 0.0748 (§) |
| Motor deficit | 7 | 13 | chi square | 0.0267 (*) |
| Myelopathy | 3 | 1 | Fisher’s exact | 0.64 |
| Radicular pain | 18 | 5 | chi square | 0.0489 (*) |
| Spinal claudication | 1 | 2 | Fisher’s exact | 0.5659 |
| Spinal instability | 1 | 9 | Fisher’s exact | 0.0012 (*) |
| Spinal EP, total | 50 | 35 | ||
| Peripheral nerve EP | ||||
| Peripheral nerve EP, Total | 3 | 1 | ||
| EP, total | 169 | 139 |
| Outcome and Length of Stay | 2019 | 2020 | Test | p Value |
|---|---|---|---|---|
| March and April | March and April | |||
| Patients who received cranial EP | ||||
| Length of stay | 8 (2 … 48) days | 9 (3 … 77) days | Wilcoxon rank sum | 0.0946 (§) |
| Inhouse mortality | 2 | 1 | Fisher’s exact | 1 |
| Discharged to palliative care | 3 | 2 | Fisher’s exact | 1 |
| Discharged to nursing home | 4 | 2 | Fisher’s exact | 0.6955 |
| Discharged home, dependent on care | 5 | 3 | Fisher’s exact | 1 |
| Discharged home, independent | 71 | 60 | chi square | 0.6365 |
| Discharged to rehabilitation facility | 26 | 20 | chi square | 1 |
| Patients who received cranial EP, total | 111 | 88 | ||
| Patients who received spinal EP | ||||
| Length of stay | 9 (3 … 67) days | 12 (3 … 111) days | Wilcoxon rank sum | 0.2674 |
| Inhouse mortality | 2 | 0 | Fisher’s exact | 0.5055 |
| Discharged to palliative care | 0 | 0 | Fisher’s exact | 1 |
| Discharged to nursing home | 0 | 0 | Fisher’s exact | 1 |
| Discharged home, dependent on care | 0 | 2 | Fisher’s exact | 0.1731 |
| Discharged home, independent | 27 | 15 | chi square | 0.2821 |
| Discharged to rehabilitation facility | 11 | 12 | chi square | 0.3429 |
| Patients who received spinal EP, total | 40 | 29 | ||
| Patients who received cranial or spinal EP | ||||
| Length of stay | 8 (2 … 67) days | 10 (3 … 111) days | Wilcoxon rank sum | 0.0497 (*) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rupa, R.; Sass, B.; Morales Lema, M.A.; Nimsky, C.; Voellger, B. The Demand for Elective Neurosurgery at a German University Hospital during the First Wave of COVID-19. Healthcare 2020, 8, 483. https://doi.org/10.3390/healthcare8040483
Rupa R, Sass B, Morales Lema MA, Nimsky C, Voellger B. The Demand for Elective Neurosurgery at a German University Hospital during the First Wave of COVID-19. Healthcare. 2020; 8(4):483. https://doi.org/10.3390/healthcare8040483
Chicago/Turabian StyleRupa, Rosita, Benjamin Sass, Maria Alejandra Morales Lema, Christopher Nimsky, and Benjamin Voellger. 2020. "The Demand for Elective Neurosurgery at a German University Hospital during the First Wave of COVID-19" Healthcare 8, no. 4: 483. https://doi.org/10.3390/healthcare8040483
APA StyleRupa, R., Sass, B., Morales Lema, M. A., Nimsky, C., & Voellger, B. (2020). The Demand for Elective Neurosurgery at a German University Hospital during the First Wave of COVID-19. Healthcare, 8(4), 483. https://doi.org/10.3390/healthcare8040483






