A Drive-through Simulation Tool for Mass Vaccination during COVID-19 Pandemic
Abstract
1. Introduction
2. Background
2.1. Drive-through in Public Health and Mass Vaccination
2.2. Design and Operational Challenges of Drive-through Facilities for Mass Vaccination
2.3. Drive-through Mass Vaccination Modeling and Simulation Tools
3. Materials and Methods
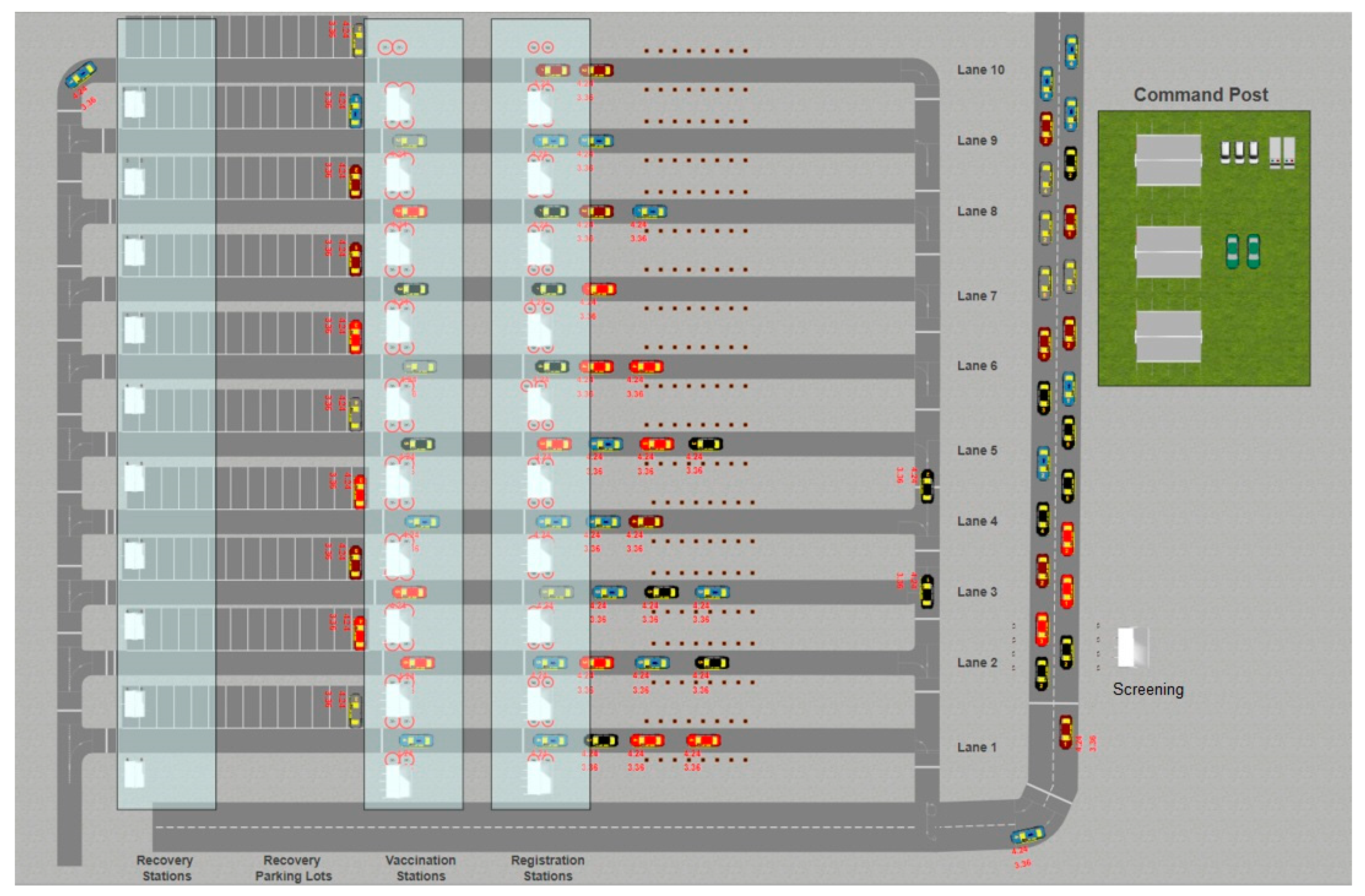
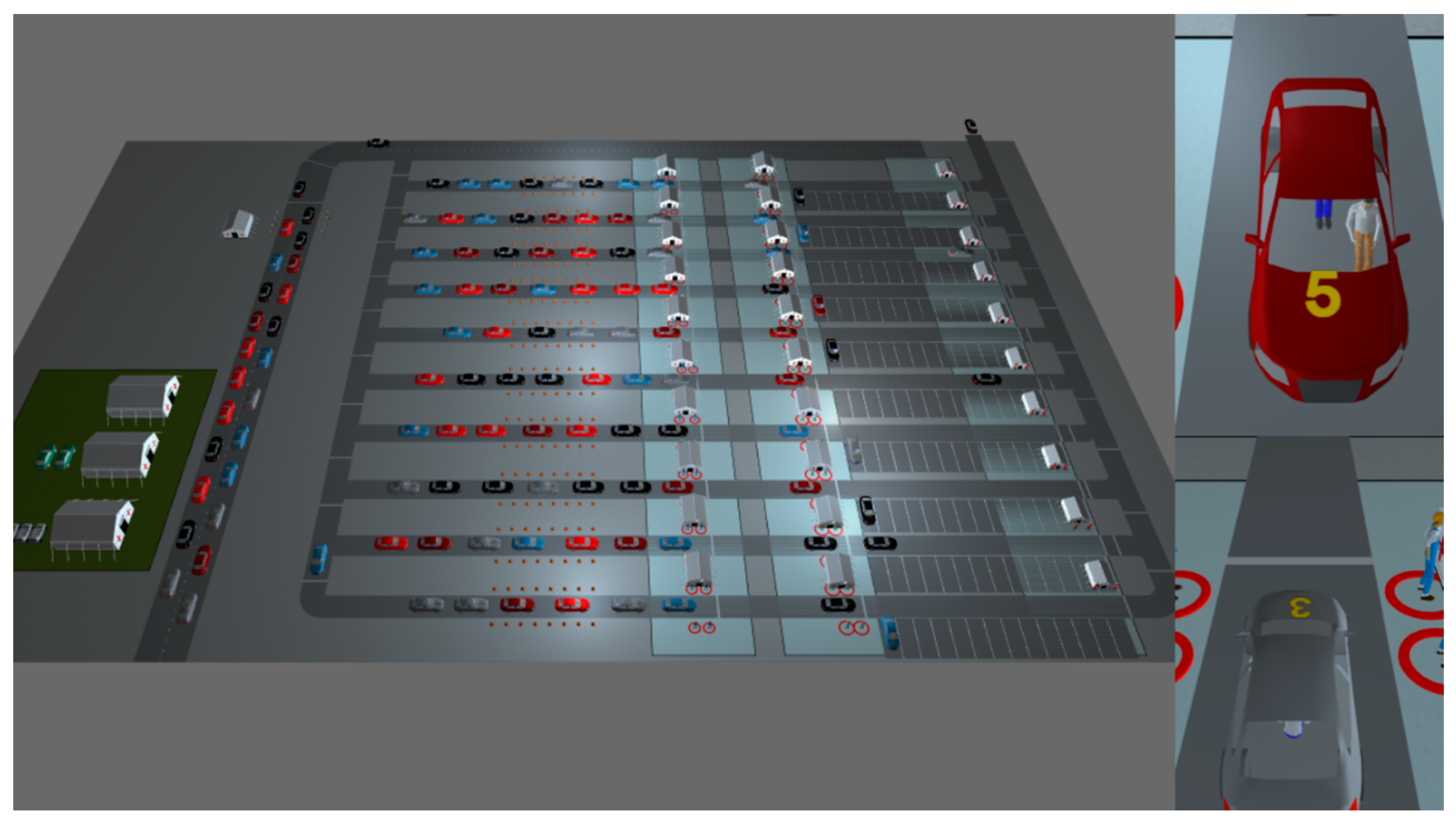
3.1. Drive-through Layout
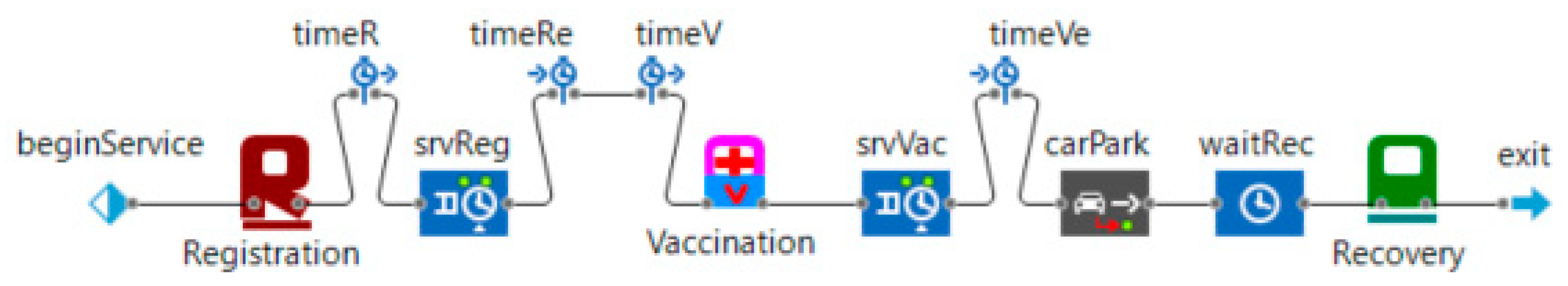
3.2. Drive-through Model Agents and Processes
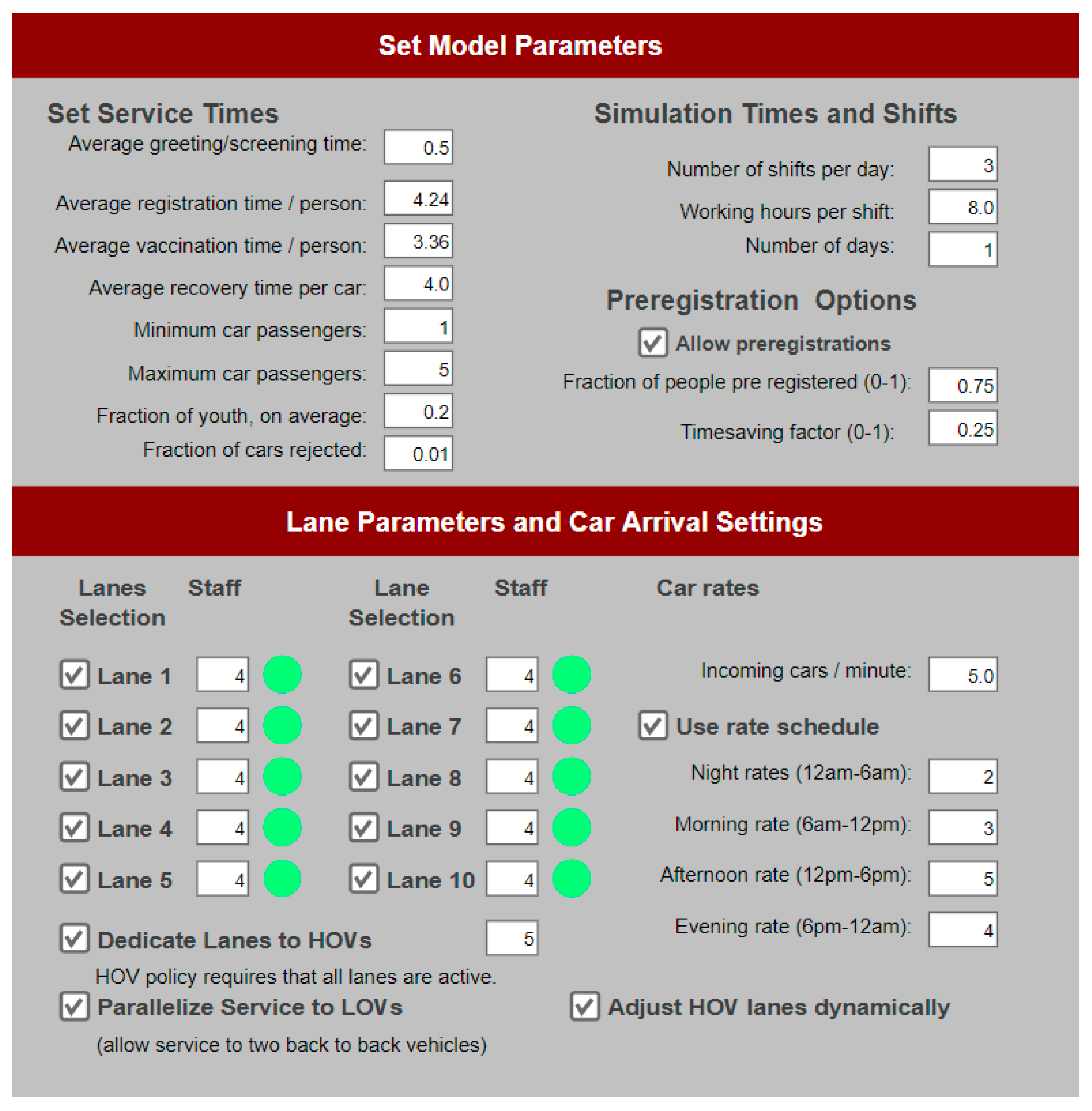
3.3. Simulation Inputs and Outputs
- Open service lanes (minimum: 1; maximum: 10; default: 10).
- Number of staff serving in each open service lane (minimum: 2; maximum: 4; default: 4).
- Choice to dedicate lanes to High Occupancy Vehicles (HOVs) to allocate specific lanes to them or not. This policy requires and enforces that all ten service lanes be in operation.
- Number of lanes assigned to the HOVs (minimum: 1; maximum: 9; default: 5).
- Choice to automatically optimize the number of HOV lanes according to the last hour queue patterns.
- Choice to parallelize service where possible (if enough staff are available at the LOV station) to Low Occupancy Vehicles (LOVs). This policy choice is only available if the HOV choice is selected.
- Choice to allow pre-registration of clients (default: false), as well as the fraction of clients (at car level) that preregister (default if pre-registration is chosen: 75%), and the timesaving factor that becomes effective for the pre-registered clients (default if pre-registration is chosen: 25%);
- Average registration and vaccination times per person (default: 6.44 and 5.36 min respectively).
- Average recovery time per car (default: 5 min).
- Minimum and maximum passengers in a car (default: 1 and 5, respectively).
- Fraction of dependent children (except the driver) on average (default: 20%).
- Number of incoming cars per minute (default: 5).
- Fraction of cars rejected from the screening booth (default: 1%).
- Number of shifts per day.
- Working hours per shift.
- Number of days (for the whole simulation run).
4. Results
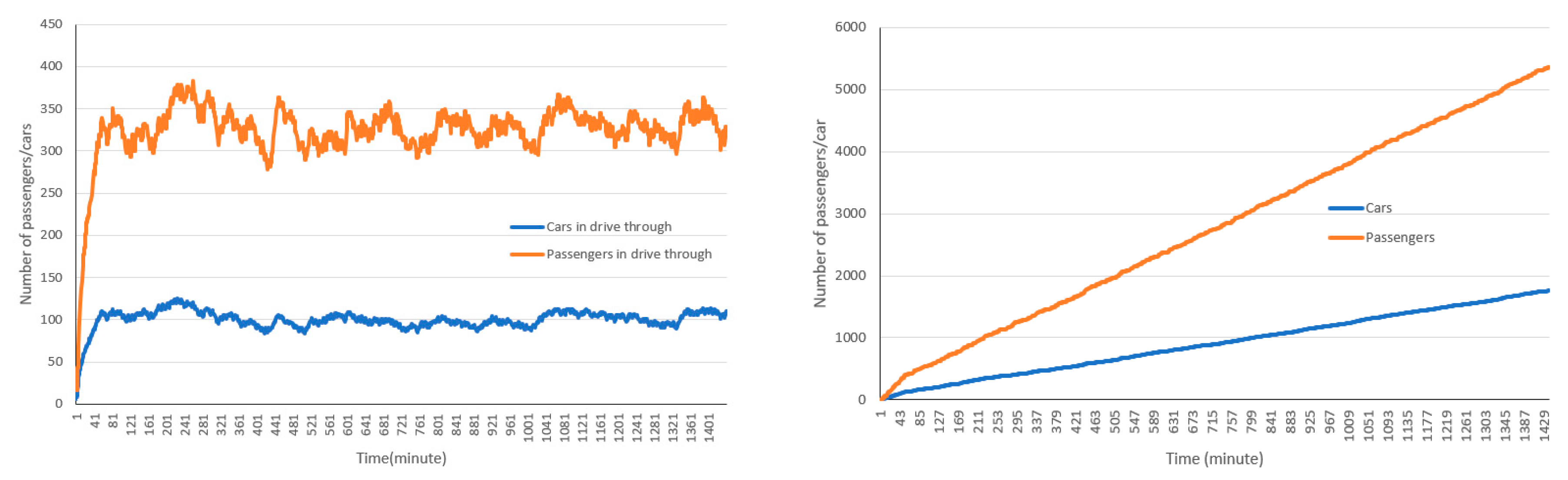
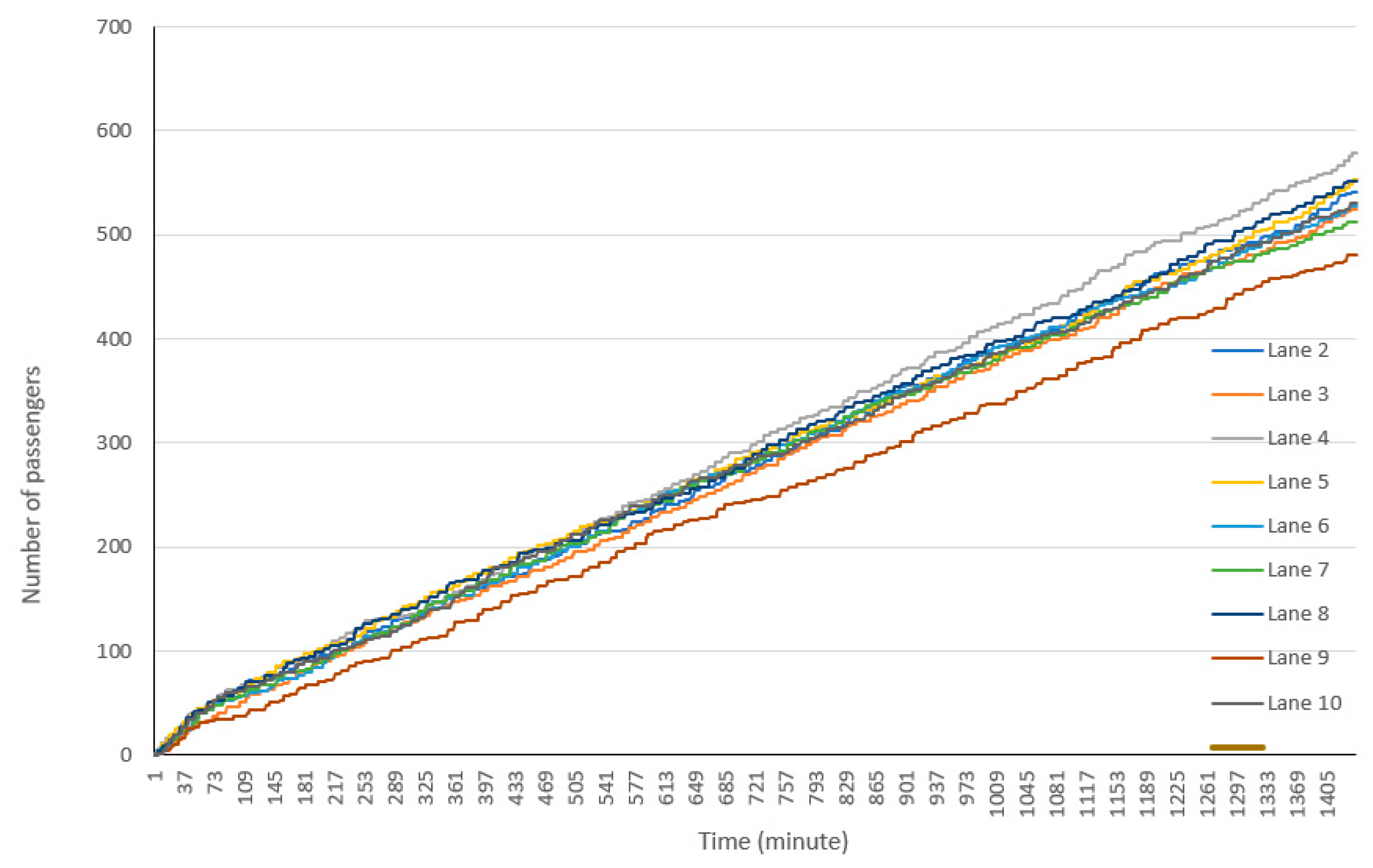
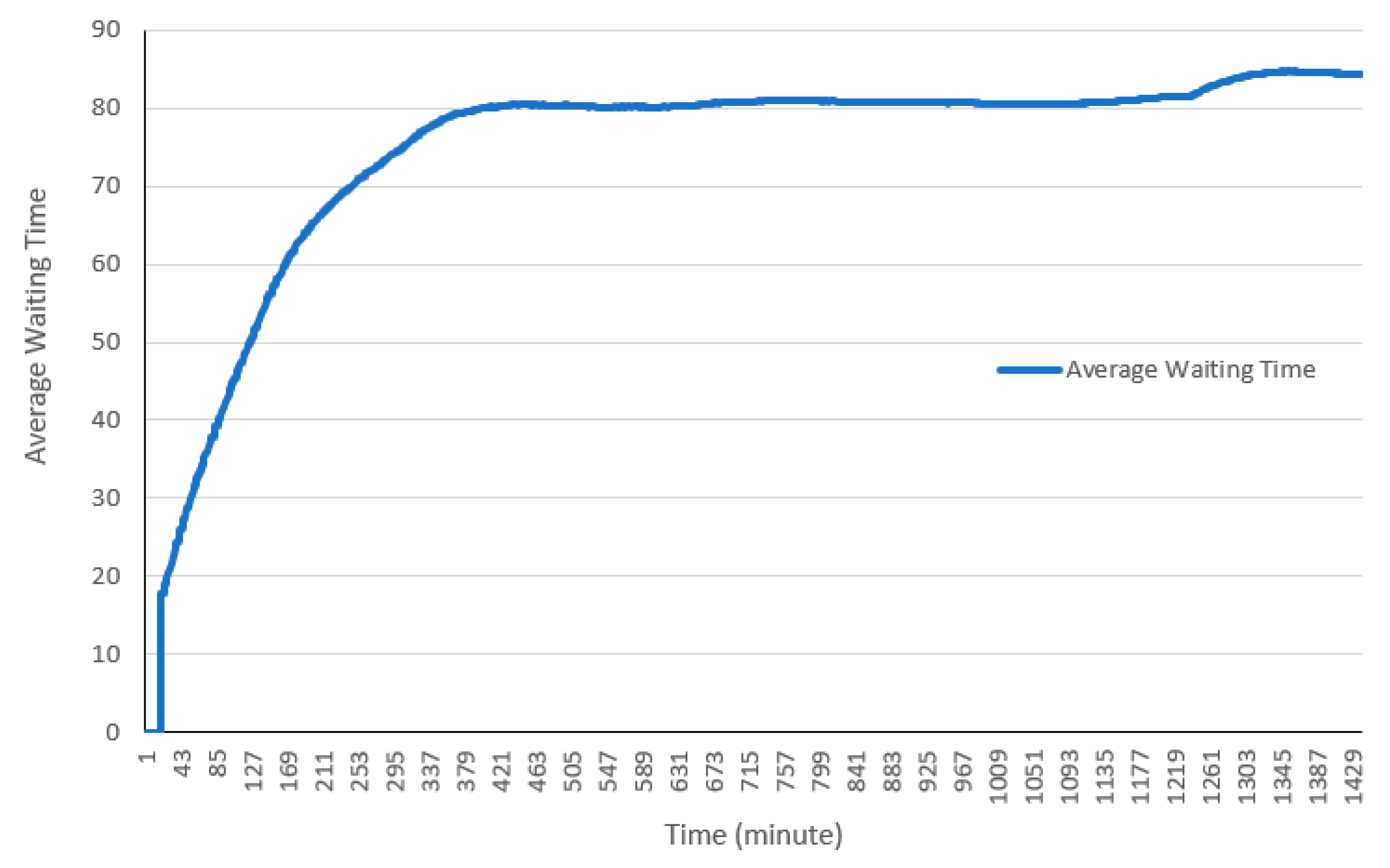
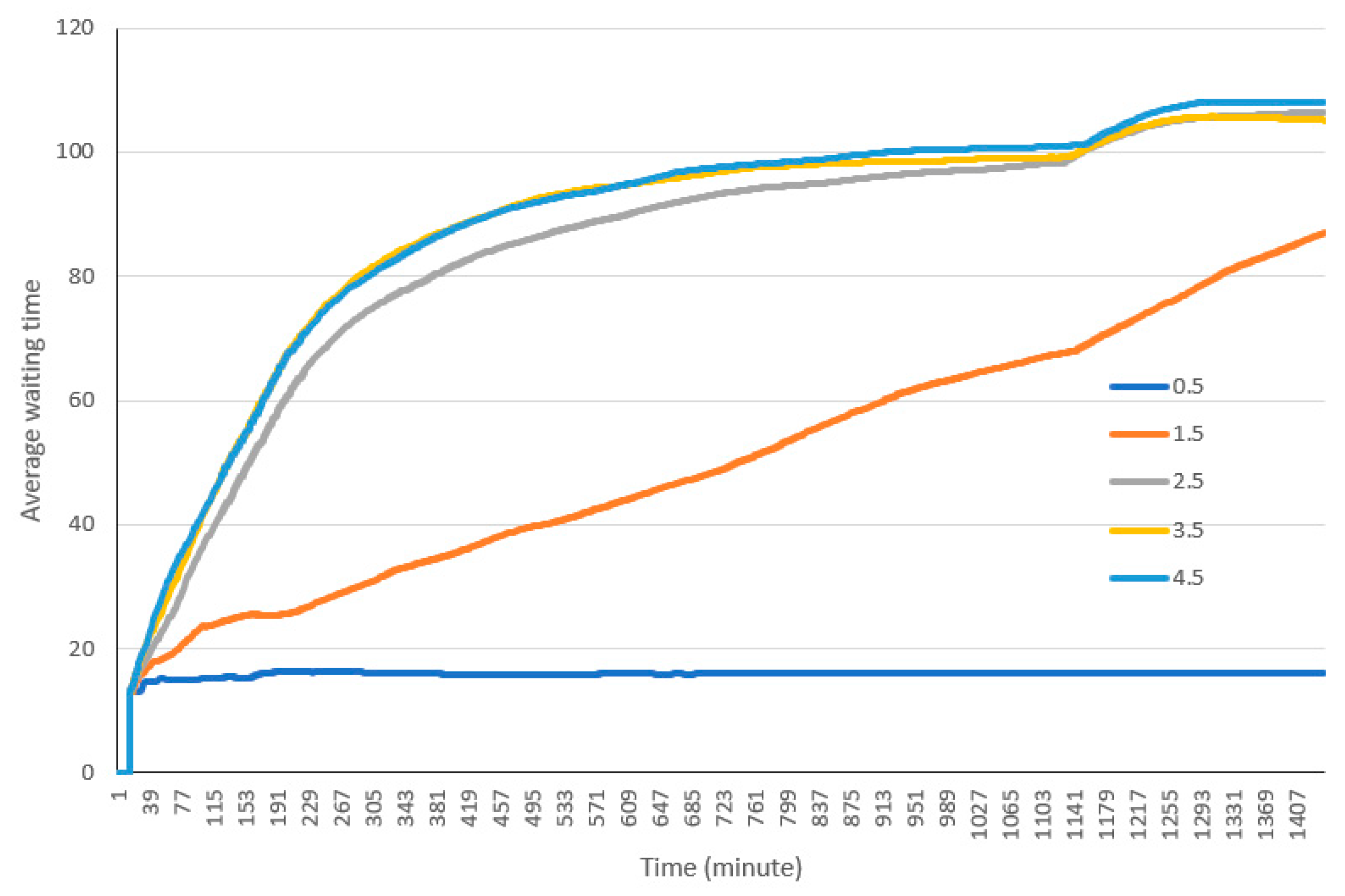
4.1. Base Experiment
4.2. Parameter Variations and Sensitivity Analyses
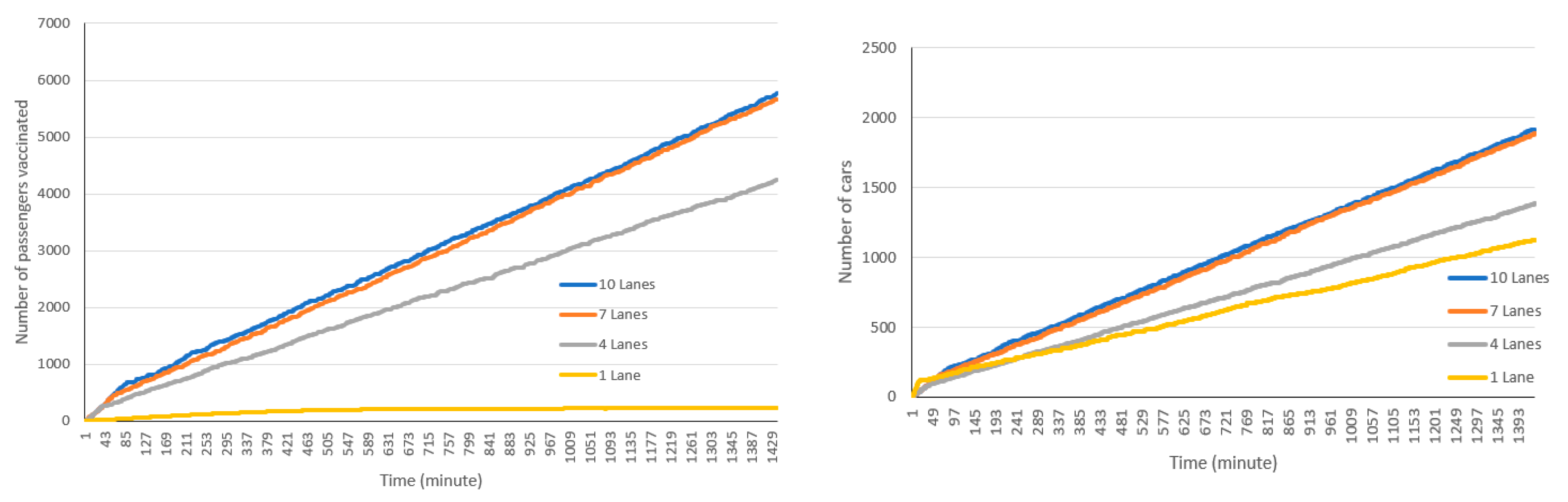
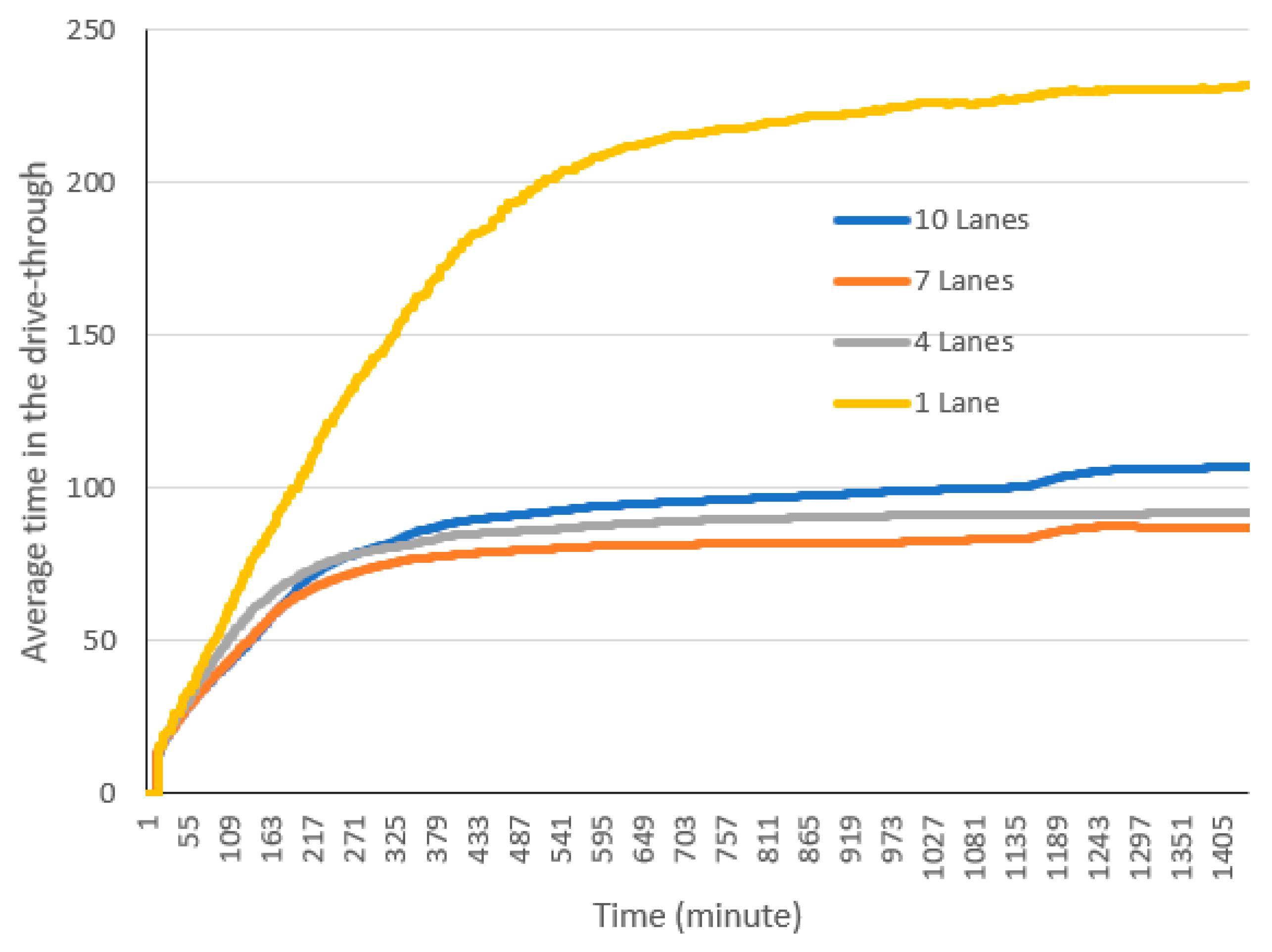
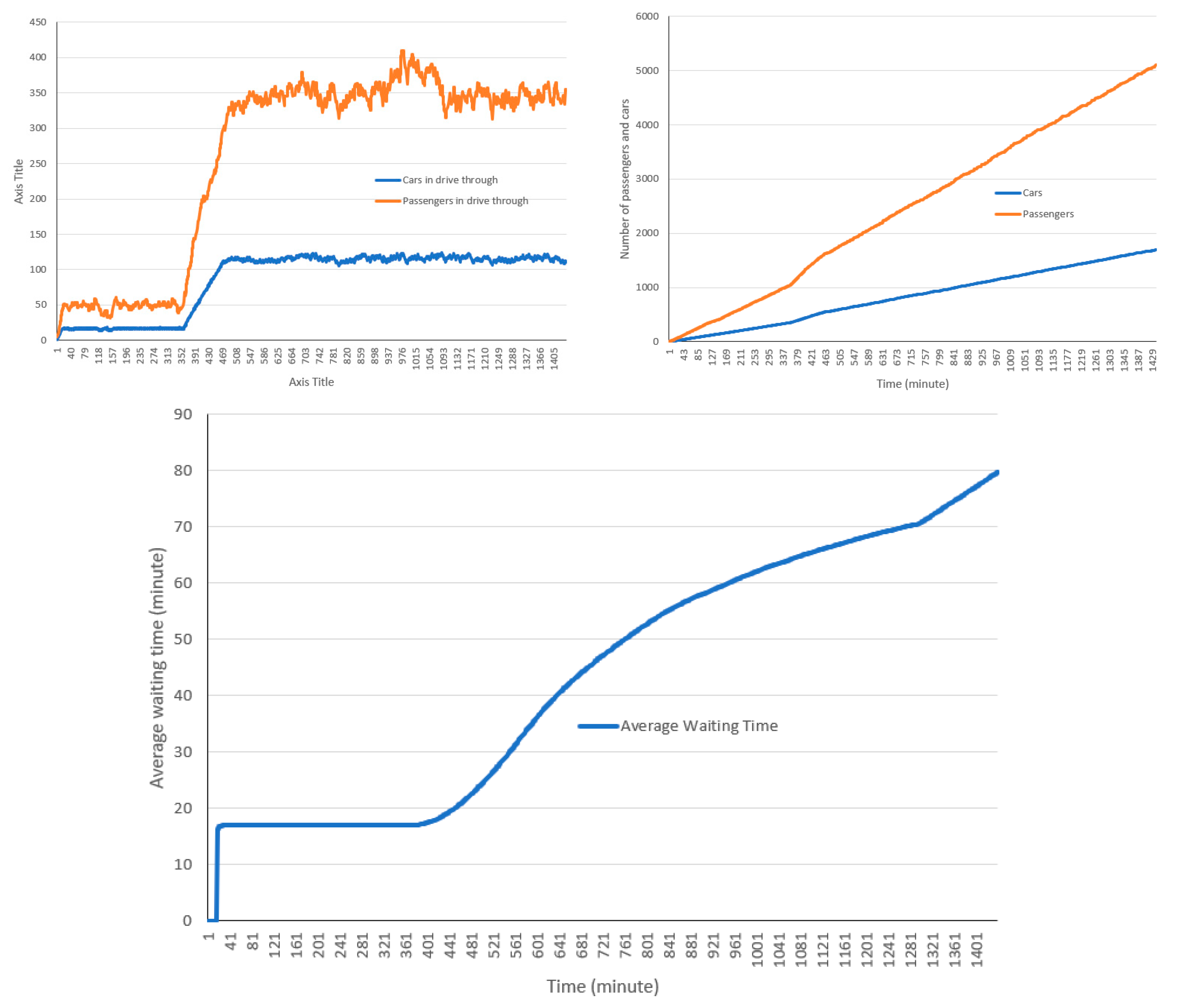
4.2.1. Number of Lanes
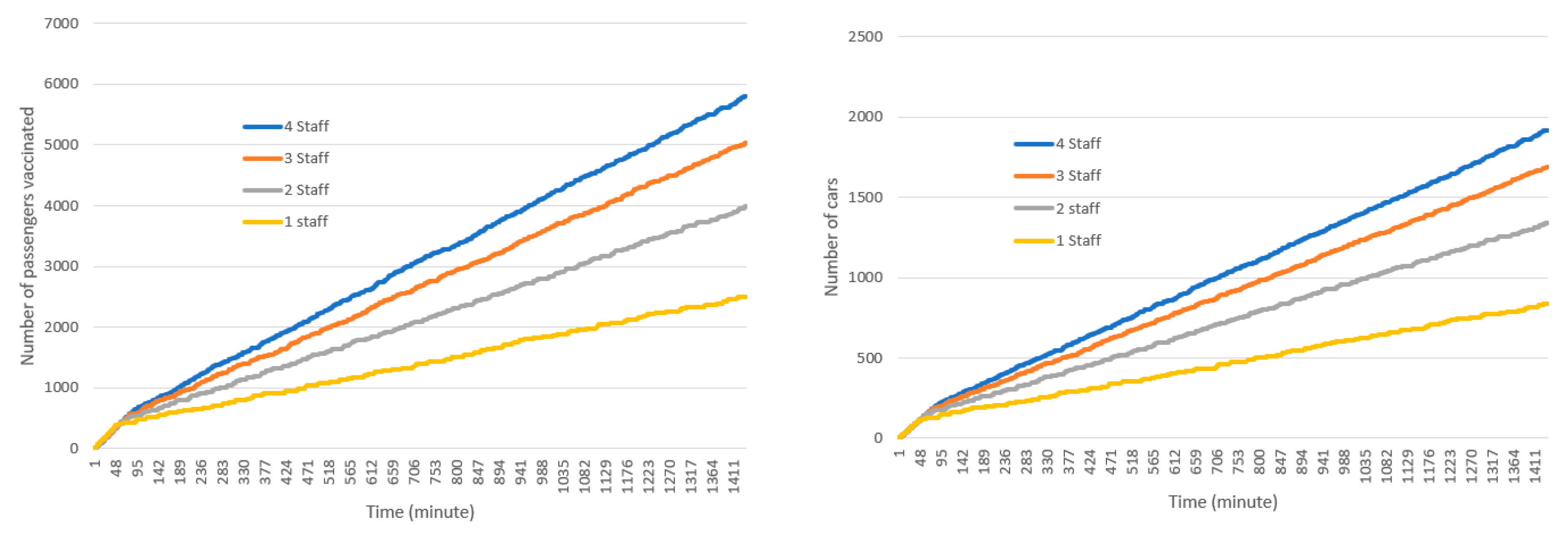
4.2.2. Number of Staff in Each Station
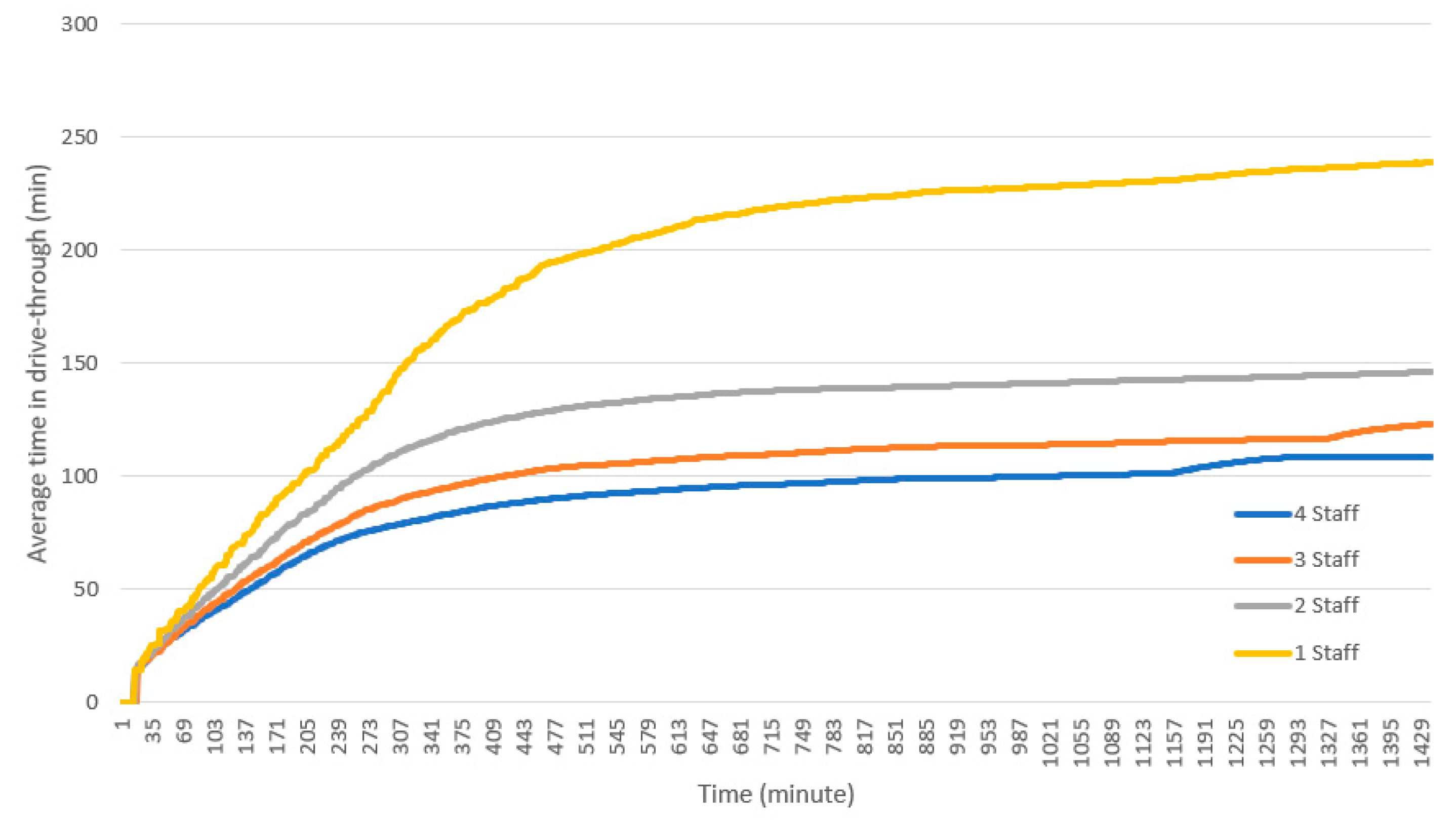
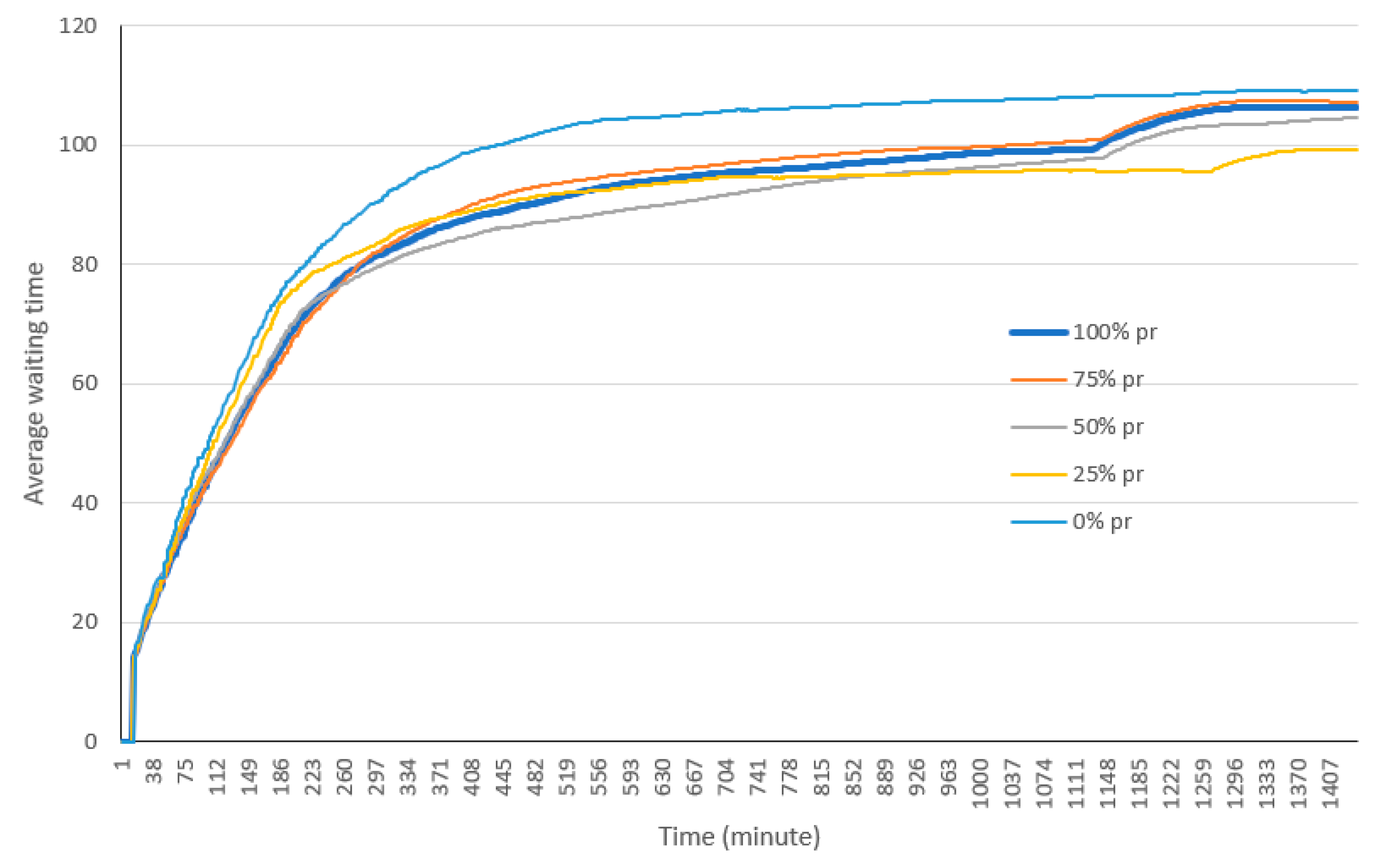
4.2.3. Pre-Registration
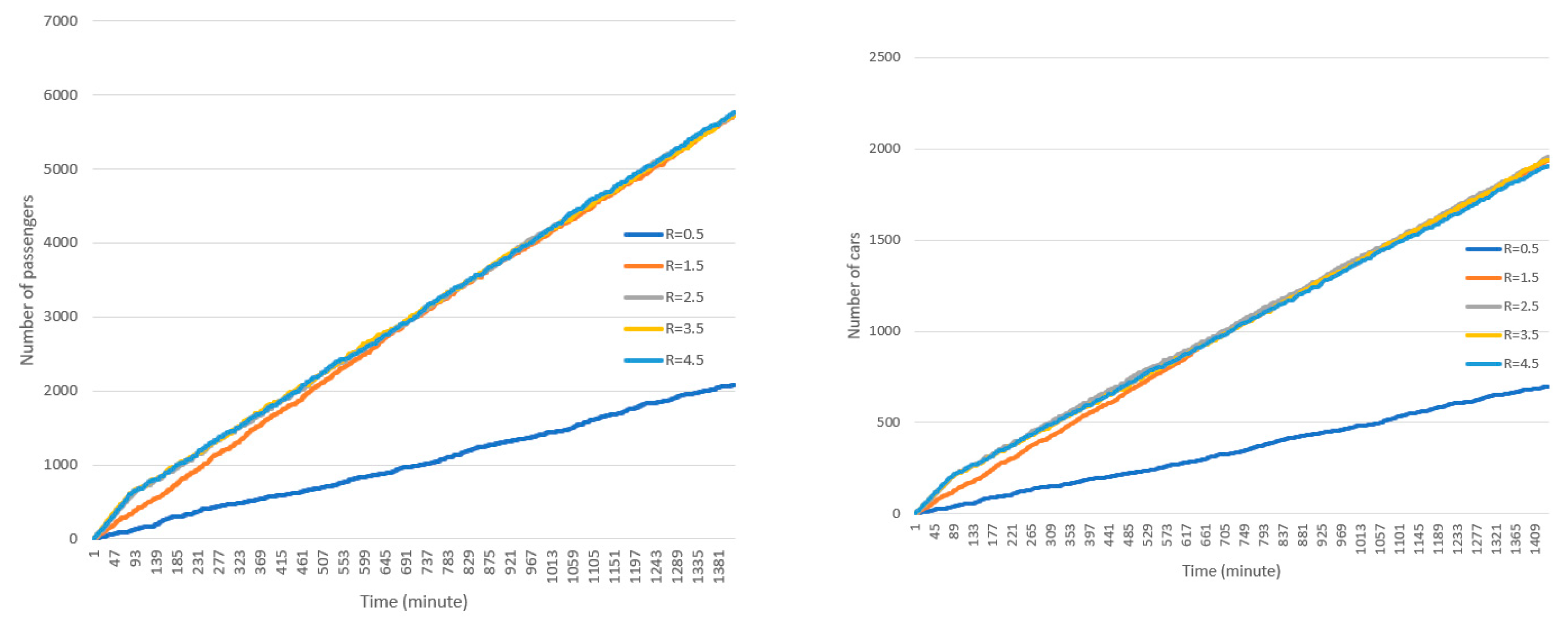
4.2.4. Arrival Rate and Schedule
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- DeRoo, S.S.; Pudalov, N.J.; Fu, L.Y. Planning for a COVID-19 Vaccination Program. JAMA 2020, 323, 2458–2459. [Google Scholar] [CrossRef] [PubMed]
- New York Times, Coronavirus Vaccine Tracker. Available online: https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html (accessed on 23 August 2020).
- Schwartz, B.; Wortley, P. Mass Vaccination for Annual and Pandemic Influenza; Plotkin, S.A., Ed.; Springer: Berlin, Germany, 2006; pp. 131–152. [Google Scholar]
- Kaplan, E.H.; Craft, D.L.; Wein, L.M. Emergency response to a smallpox attack: The case for mass vaccination. Proc. Natl. Acad. Sci. USA 2002, 99, 10935–10940. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Evans, G.W.; Heragu, S.S. Simulation and optimization modeling for drive-through mass vaccination—A generalized approach. Simul. Model. Pract. Theory. 2013, 37, 99–106. [Google Scholar] [CrossRef]
- National Coronavirus Response: A Road Map to Reopening. Available online: https://www.aei.org/research-products/report/national-coronavirus-response-a-road-map-to-reopening (accessed on 10 August 2020).
- Weiss, E.A.; Ngo, J.; Gilbert, G.H.; Quinn, J.V. Drive-Through Medicine: A Novel Proposal for Rapid Evaluation of Patients During an Influenza Pandemic. Ann. Emerg. Med. 2010, 55, 268–273. [Google Scholar] [CrossRef] [PubMed]
- What Are the Efficiencies of a Mass Vaccination Drive-Through Clinic Compared to a Walk-In Clinic? Available online: https://www.hsdl.org/?abstract&did=804516 (accessed on 10 August 2020).
- Wiggers, J.; van de Kracht, T.; Gupta, A.; Heragu, S.S. Design and Analysis of a Simulation Model for Drive-Through Mass Vaccination. In Proceedings of the 2011 Industrial Engineering Research Conference, Reno, NV, USA, 21–25 May 2011; Doolen, T., Van Aken, E., Eds.; [Google Scholar]
- Yaylali, E.; Ivy, J.S.; Taheri, J. Systems Engineering Methods for Enhancing the Value Stream in Public Health Preparedness: The Role of Markov Models, Simulation, and Optimization. Public Health Rep. 2014, 129, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Schoch-Spana, M.; Brunson, E.; Long, R.; Ravi, S.; Ruth, A.; Trotochaud, M. on behalf of the Working Group on Readying Populations for COVID-19 Vaccine, The Public’s Role in COVID-19 Vaccination: Planning Recommendations Informed by Design Thinking and the Social, Behavioral, and Communication Sciences. Available online: https://www.centerforhealthsecurity.org/our-work/publications/the-publics-role-in-covid-19-vaccination (accessed on 10 August 2020).
- Carrico, R. Drive-Thru Flu Shots—A Model for Mass Immunization; Spectrum Press: Chicago, IL, USA, 2002. [Google Scholar]
- Drive-Thru Dispensing Clinic on Kauai. Available online: https://list.nih.gov/archives/sns_program-l.html (accessed on 5 June 2006).
- Carrico, R.; McKinney, W.P.; Watson, N.A.; Wiemken, T.; Myers, J. Drive-thru influenza immunization: Fifteen years of experience. J. Emerg. Manag. 2012, 10, 228. [Google Scholar] [CrossRef]
- Delivering Mass Vaccinations During COVID-19. A Logistical Guide for General Practice. Available online: https://www.rcgp.org.uk/-/media/Files/Policy/A-Z-policy/2020/covid19/RCGP-guidance/RCGP-Mass-Vaccination-at-a-time-of-COVID-V15.ashx (accessed on 10 August 2020).
- Flynn, E.F.; Kuhn, E.; Shaik, M.; Tarr, E.; Scattolini, N.; Ballantine, A. Drive-Through COVID-19 Testing During the 2020 Pandemic: A Safe, Efficient, and Scalable Model for Pediatric Patients and Health Care Workers. Acad. Pediatr. 2020, 20, 753–755. [Google Scholar] [CrossRef]
- Lee, E.K.; Pietz, F.; Benecke, B.; Mason, J.; Burel, G. Advancing Public Health and Medical Preparedness with Operations Research. Interfaces 2013, 43, 79–98. [Google Scholar] [CrossRef]
- Shim, E.; Meyers, L.; Galvani, A.P. Optimal H1N1 vaccination strategies based on self-interest versus group interest. BMC Public Health 2011, 11, S1–S4. [Google Scholar] [CrossRef]
- Qeadan, F.; Honda, T.; Gren, L.H.; Dailey-Provost, J.; Benson, L.S.; VanDerslice, J.A.; Porucznik, C.A.; Waters, A.B.; Lacey, S.; Shoaf, K. Naive Forecast for COVID-19 in Utah Based on the South Korea and Italy Models-the Fluctuation between Two Extremes. Int. J. Environ. Res. Public Health 2020, 17, 2750. [Google Scholar] [CrossRef]
- Nicola, M.; Sohrabi, C.; Mathew, G.; Kerwan, A.; Al-Jabir, A.; Griffin, M.; Agha, M.; Agha, R. Health policy and leadership models during the COVID-19 pandemic: A review. Int. J. Surg. 2020, 81, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Turrentine, M.; Ramirez, M.; Monga, M.; Gandhi, M.; Swaim, L.; Tyer-Viola, L.; Birsinger, M.; Belfort, M. Rapid Deployment of a Drive-Through Prenatal Care Model in Response to the Coronavirus Disease 2019 (COVID-19) Pandemic. Obstet. Gynecol. 2020, 136, 29–32. [Google Scholar] [CrossRef] [PubMed]
- Hussain, R.; Dawoud, D.M.; Babar, Z.-U.-D. Drive-thru pharmacy services: A way forward to combat COVID-19 pandemic. Res. Soc. Adm. Pharm. in press. [CrossRef]
- Bailey, L.C.; Barrett, N.R.; Thorne, M.; Ford, F.M.; Elizabeth, W.; Psevdos, G. Successful Drive-thru Point-of-Distribution Influenza Vaccination Program for Veterans Affairs Medical Center Employees. Am. J. Infect. Control 2020, 48, S31. [Google Scholar] [CrossRef]
- Decaro, N.; Martella, V.; Saif, L.J.; Buonavoglia, C. COVID-19 from veterinary medicine and one health perspectives: What animal coronaviruses have taught us. Res. Vet. Sci. 2020, 131, 21–23. [Google Scholar] [CrossRef] [PubMed]
- Garrison, G. Here’s What a Birmingham Clinic CEO Learned from 2,200 COVID-19 Tests. Available online: https://www.al.com/coronavirus/2020/03/heres-what-a-birmingham-clinic-ceo-learned-from-2200-covid-19-tests.html (accessed on 2 April 2020).
- Ton, A.N.; Jethwa, T.; Waters, K.; Speicher, L.L.; Francis, D. COVID-19 drive through testing: An effective strategy for conserving personal protective equipment. Am. J. Infect. Control 2020, 48, 731–732. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Lee, J. Testing on the move: South Korea’s rapid response to the COVID-19 pandemic. Transp. Res. Interdiscip. Perspect. 2020, 5, 100111. [Google Scholar] [CrossRef]
- Pate, J. Drive-Thru PODs: An Alternate Method of Mass Prophylaxis; Public Health Preparedness Summit: Washington, DC, USA, 2007.
- Richter, A.; Khan, S. Pilot Model: Judging Alternate Modes of Dispensing Prophylaxis in Los Angeles County. Interfaces 2009, 39, 228–240. [Google Scholar] [CrossRef]
- Khan, S.; Richter, A. Dispensing Mass Prophylaxis—The Search for the Perfect Solution. Available online: https://www.hsaj.org/articles/206 (accessed on 10 August 2020).
- Wessex Local Medical Committees. Operational Aspects of Influenza Immunisation 2020/21; Wessex Local Medical Committees: Eastleigh, UK, 2020.
- Lee, E.K.; Chen, C.-H.; Pietz, F.; Benecke, B. Modeling and Optimizing the Public-Health Infrastructure for Emergency Response. Interfaces 2009, 39, 476–490. [Google Scholar] [CrossRef]
- CRI Alternative Dispensing Guide—A Collection of Model Practices and Pilot Projects. Available online: https://www.hsdl.org/?view&did=773065 (accessed on 10 August 2020).
- Lee, E.K.; Smalley, H.K.; Zhang, Y.; Pietz, F.; Benecke, B. Facility location and multi-modality mass dispensing strategies and emergency response for biodefence and infectious disease outbreaks. Int. J. Risk Assess. Manag. 2009, 12, 311. [Google Scholar] [CrossRef]
- Knox, D. Davenport, Dispensing Emergency Medications and Supplies; Fielding, J.E., Teutsch, S.M., Eds.; Oxford University Press: Oxford, UK, 2012; pp. 243–253. [Google Scholar]
- Aaby, K.; Abbey, R.L.; Herrmann, J.W.; Treadwell, M.; Jordan, C.S.; Wood, K. Embracing Computer Modeling to Address Pandemic Influenza in the 21st Century. J. Public Health Manag. Pract. 2006, 12, 365–372. [Google Scholar] [CrossRef][Green Version]
- Beeler, M.F.; Aleman, D.M.; Carter, M.W. A simulation case study to improve staffing decisions at mass immunization clinics for pandemic influenza. J. Oper. Res. Soc. 2014, 65, 497–511. [Google Scholar] [CrossRef]
- Fryhofer, S.A.; Fryhofer, G.W. Vaccination-Induced Bursitis: Technique Matters. Ann. Intern. Med. 2020, 173, 308–310. [Google Scholar] [CrossRef]
- Hupert, N.; Mushlin, A.I.; Callahan, M.A. Modeling the Public Health Response to Bioterrorism: Using Discrete Event Simulation to Design Antibiotic Distribution Centers. Med. Decis. Making 2002, 22, 17–25. [Google Scholar] [CrossRef]
- Hupert, N.; Xiong, W.; King, K.; Castorena, M.; Hawkins, C.; Wu, C.; Muckstadt, J.A. Uncertainty and Operational Considerations in Mass Prophylaxis Workforce Planning. Disaster Med. Public Health Prep. 2009, 3, S121–S131. [Google Scholar] [CrossRef]
- Hernandez, I.; Ramirez-Marquez, J.E.; Starr, D.; McKay, R.; Guthartz, S.; Motherwell, M.; Barcellona, J. Optimal staffing strategies for points of dispensing. Comput. Ind. Eng. 2015, 83, 172–183. [Google Scholar] [CrossRef]
- Ramirez-Nafarrate, A.; Lyon, J.D.; Fowler, J.W.; Araz, O.M. Point-of-Dispensing Location and Capacity Optimization via a Decision Support System. Prod. Oper. Manag. 2015, 24, 1311–1328. [Google Scholar] [CrossRef]
- Dispensing Medical Countermeasures in Public Health Emergencies via Home Health Agencies and Points of Distribution. Available online: http://scholarworks.uark.edu/ineguht/59 (accessed on 10 August 2020).
- Araz, O.M.; Fowler, J.W.; Nafarrate, A.R. Optimizing service times for a public health emergency using a genetic algorithm: Locating dispensing sites and allocating medical staff. IIE Trans. Healthc. Syst. Eng. 2014, 4, 178–190. [Google Scholar] [CrossRef]
- Chiquoine, R.M. Travel Behaviors during a Public Health Biological Emergency Requiring Points of Dispensing. Available online: https://udspace.udel.edu/handle/19716/24916 (accessed on 10 August 2020).
- Washington, M.L.; Mason, J.; Meltzer, M.I. Maxi-Vac: Planning Mass Smallpox Vaccination Clinics. J. Public Health Manag. Pract. 2005, 11, 542–549. [Google Scholar] [CrossRef]
- Glass, P.R. The Effects of Computer Simulation on Reducing the Incidence of Medical Errors Associated with Mass Distribution of Chemoprophylaxis as a Result of a Bioterrorism Event. Ph.D. Thesis, Purdue University, West Lafayette, IN, USA, 2019. [Google Scholar]
- Gorman, S.E.; Pesik, N.T. Mass Dispensing of Antibiotics and Vaccines; Koenig, K.L., Schultz, C.H., Eds.; Cambridge University Press: Cambridge, UK, 2009; pp. 213–227. [Google Scholar] [CrossRef]
- Asgary, A.; Najafabadi, M.M. Drive Through Mass Vaccination Sim for COVID-19. Available online: https://cloud.anylogic.com/model/583c2075-6a8b-41be-8a03-d692eba71683?mode=SETTINGS (accessed on 10 August 2020).
| Parameters | Value |
|---|---|
| Greeting and screening time per car (minute) | Uniform (0.25, 0.5) |
| Average registration time (minute) per passenger | 4.24 * |
| Average vaccination/dispensing time per passenger (minute) | 3.36 * |
| Minimum number of passengers | 1 |
| Maximum number of passengers | 5 |
| Fraction of non-adult passengers | 0.2 |
| Number of incoming cars per minute | 5 |
| Fraction of cars rejected at the screening | 0.01 |
| Number of shifts per day | 3 |
| Hours of operations in each shift | 8 |
| Number of days | 1 |
| Lanes open | 1, 2, 3, 4, 5, 6, 7, 8, 9, 10 |
| Staff in each station | 4 |
| Pre-registration | No |
| High occupancy vehicle lane | No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asgary, A.; Najafabadi, M.M.; Karsseboom, R.; Wu, J. A Drive-through Simulation Tool for Mass Vaccination during COVID-19 Pandemic. Healthcare 2020, 8, 469. https://doi.org/10.3390/healthcare8040469
Asgary A, Najafabadi MM, Karsseboom R, Wu J. A Drive-through Simulation Tool for Mass Vaccination during COVID-19 Pandemic. Healthcare. 2020; 8(4):469. https://doi.org/10.3390/healthcare8040469
Chicago/Turabian StyleAsgary, Ali, Mahdi M. Najafabadi, Richard Karsseboom, and Jianhong Wu. 2020. "A Drive-through Simulation Tool for Mass Vaccination during COVID-19 Pandemic" Healthcare 8, no. 4: 469. https://doi.org/10.3390/healthcare8040469
APA StyleAsgary, A., Najafabadi, M. M., Karsseboom, R., & Wu, J. (2020). A Drive-through Simulation Tool for Mass Vaccination during COVID-19 Pandemic. Healthcare, 8(4), 469. https://doi.org/10.3390/healthcare8040469







