Incidence and Risk Factors for 30-Day Readmission after Inpatient Chemotherapy among Acute Lymphoblastic Leukemia Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
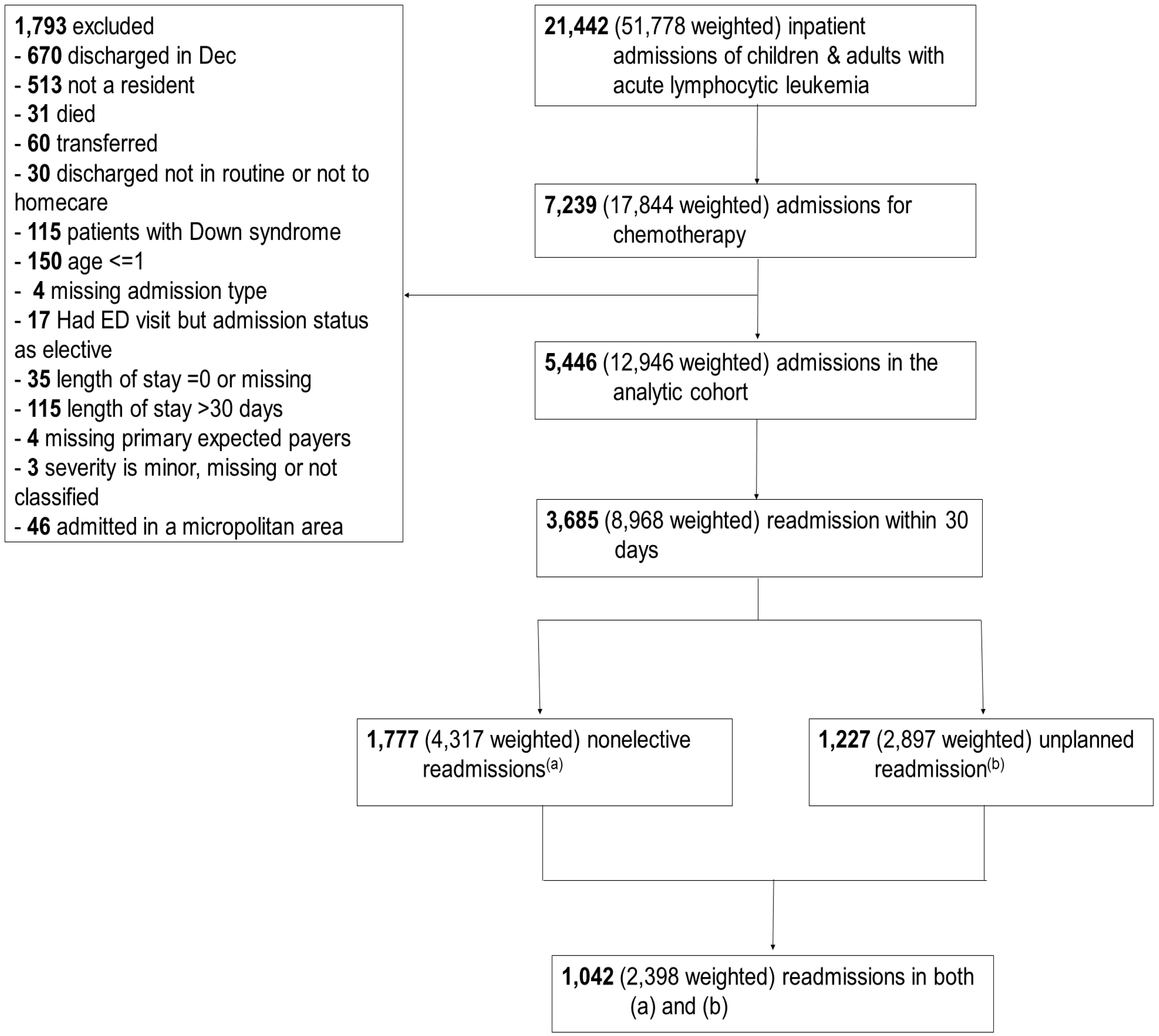
2.2. Study Design and Population
2.3. Exposure
2.4. Outcome
2.5. Covariables
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Reasons for Readmission
3.3. Risk Factors for 30-Day Readmission
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- National Cancer Institute. Definition of Acute Lymphoblastic Leukemia—NCI Dictionary of Cancer Terms. Available online: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/acute-lymphoblastic-leukemia (accessed on 1 April 2020).
- American Cancer Society. What Is Acute Lymphocytic Leukemia (ALL)? Acute Lymphocytic Leukemia (ALL). Available online: https://www.cancer.org/cancer/acute-lymphocytic-leukemia/about/what-is-all.html (accessed on 1 April 2020).
- National Cancer Institute. SEER Cancer Stat Facts: Acute Lymphocytic Leukemia. Available online: https://seer.cancer.gov/statfacts/html/alyl.html (accessed on 1 April 2020).
- National Comprehensive Cancer Network. NCCN Guidlines Version 5.2017 Acute Lymphoblastic Leukemia. Available online: https://oncolife.com.ua/doc/nccn/Acute_Lymphoblastic_Leukemia.pdf (accessed on 1 April 2020).
- Nachman, J.B.; La, M.K.; Hunger, S.P.; Heerema, N.A.; Gaynon, P.S.; Hastings, C.; Mattano, L.A.; Sather, H.; Devidas, M.; Freyer, D.R.; et al. Young adults with acute lymphoblastic leukemia have an excellent outcome with chemotherapy alone and benefit from intensive postinduction treatment: A report from the children’s oncology group. J. Clin. Oncol. 2009, 27, 5189–5194. [Google Scholar] [CrossRef] [PubMed]
- Kaul, S.; Korgenski, E.K.; Ying, J.; Ng, C.F.; Smits-Seemann, R.R.; Nelson, R.E.; Andrews, S.; Raetz, E.; Fluchel, M.; Lemons, R.; et al. A retrospective analysis of treatment-related hospitalization costs of pediatric, adolescent, and young adult acute lymphoblastic leukemia. Cancer Med. 2016, 5, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Wedekind, M.F.; Dennis, R.; Sturm, M.; Koch, T.; Stanek, J.; O’Brien, S.H. The Effects of Hospital Length of Stay on Readmissions for Children with Newly Diagnosed Acute Lymphoblastic Leukemia. J. Pediatr. Hematol. Oncol. 2016, 38, 329–333. [Google Scholar] [CrossRef] [PubMed]
- Dhakal, B.; Giri, S.; Levin, A.; Rein, L.; Fenske, T.S.; Chhabra, S.; Shah, N.N.; Szabo, A.; D’Souza, A.; Pasquini, M.; et al. Factors Associated with Unplanned 30-Day Readmissions After Hematopoietic Cell Transplantation Among US Hospitals. JAMA Netw. Open 2019, 2, e196476. [Google Scholar] [CrossRef] [PubMed]
- Medicare.gov. 30-Day Death and Readmission Measures Data. Available online: https://www.medicare.gov/hospitalcompare/Data/30-day-measures.html (accessed on 1 April 2020).
- Schneider, R.B.; Jimenez-Shahed, J.; Abraham, D.S.; Thibault, D.P.; Mantri, S.; Fullard, M.; Burack, M.A.; Chou, K.L.; Spindler, M.; Jermakowicz, W.J.; et al. Acute readmission following deep brain stimulation surgery for Parkinson’s disease: A nationwide analysis. Parkinsonism Relat. Disord. 2020, 70, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Sanaiha, Y.; Kavianpour, B.; Downey, P.; Morchi, R.; Shemin, R.J.; Benharash, P. National Study of Index and Readmission Mortality and Costs for Thoracic Endovascular Aortic Repair in Patients with Renal Disease. Ann. Thorac. Surg. 2020, 109, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Bilal, M.; Samuel, R.; Khalil, M.K.; Singh, S.; Parupdui, S.; Abougergi, M.S. Nonvariceal upper GI hemorrhage after percutaneous coronary intervention for acute myocardial infarction: A national analysis over 11 months. Gastrointest Endosc. 2020. [Google Scholar] [CrossRef] [PubMed]
- Crispo, J.A.G.; Thibault, D.P.; Fortin, Y.; Krewski, D.; Willis, A.W. Association between medication-related adverse events and non-elective readmission in acute ischemic stroke. BMC Neurol. 2018, 18, 192. [Google Scholar] [CrossRef] [PubMed]
- Healthcare Cost and Utilization Project. Overview of the Nationwide Readmissions Database. Available online: https://www.hcup-us.ahrq.gov/nrdoverview.jsp (accessed on 1 April 2020).
- The Agency for Healthcare Research and Quality. Admission type. Available online: https://ushik.ahrq.gov/ViewItemDetails?system=mdr&itemKey=74569000 (accessed on 1 October 2020).
- Centers for Medicare & Medicaid Services. Measures Inventory Tool: 30-Day Unplanned Readmissions for Cancer Patients. Available online: https://cmit.cms.gov/CMIT_public/ViewMeasure?MeasureId=6030 (accessed on 1 April 2020).
- Muffly, L.S.; Reizine, N.; Stock, W. Management of acute lymphoblastic leukemia in young adults. Clin. Adv. Hematol. Oncol. 2018, 16, 138–146. [Google Scholar] [PubMed]
- Terwilliger, T.; Abdul-Hay, M. Acute lymphoblastic leukemia: A comprehensive review and 2017 update. Blood Cancer J. 2017, 7, e577. [Google Scholar] [CrossRef]
- Healthcare Cost and Utilization Project. Overview of Disease Severity Measures Disseminated with the Nationwide Inpatient Sample (NIS) and Kids’ Inpatient Database (KID). Available online: https://hcup-us.ahrq.gov/db/nation/nis/OverviewofSeveritySystems.pdf (accessed on 19 July 2020).
- Gu, H.-Q.; Li, D.-J.; Liu, C.; Zhen-Zhen, R. %ggBaseline: A SAS macro for analyzing and reporting baseline characteristics automatically in medical research. Ann. Transl. Med. 2018, 6, 326. [Google Scholar] [CrossRef]
- Chen, W.; Qian, L.; Shi, J.; Franklin, M. Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med. Res. Methodol. 2018, 18, 63. [Google Scholar] [CrossRef] [PubMed]
- White, E. The effect of misclassification of disease status in follow-up studies: Implications for selecting disease classification criteria. Am. J. Epidemiol. 1986, 124, 816–825. [Google Scholar] [CrossRef] [PubMed]
- Warrick, K.; Althouse, S.K.; Rahrig, A.; Rupenthal, J.; Batra, S. Factors associated with a prolonged hospital stay during induction chemotherapy in newly diagnosed high risk pediatric acute lymphoblastic leukemia. Leuk. Res. 2018, 71, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Slone, T.L.; Rai, R.; Ahmad, N.; Winick, N.J. Risk factors for readmission after initial diagnosis in children with acute lymphoblastic leukemia. Pediatr. Blood Cancer 2008, 51, 375–379. [Google Scholar] [CrossRef] [PubMed]
- Pulte, D.; Jansen, L.; Gondos, A.; Katalinic, A.; Barnes, B.; Ressing, M.; Holleczek, B.; Eberle, A.; Brenner, H.; Group, G.C.S.W. Survival of adults with acute lymphoblastic leukemia in Germany and the United States. PLoS ONE 2014, 9, e85554. [Google Scholar] [CrossRef] [PubMed]
- Barros, A.J.; Hirakata, V.N. Alternatives for logistic regression in cross-sectional studies: An empirical comparison of models that directly estimate the prevalence ratio. BMC Med. Res. Methodol. 2003, 3, 21. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
| Variables | N (%) or Median (IQR *) | |||
|---|---|---|---|---|
| Remission (N = 1289) | Not Achieved Remission (N = 3506) | Relapse (N = 651) | p-Value | |
| Age group [year] | ||||
| [2–10] | 439 (34.1) | 707 (20.2) | 142 (21.8) | <0.001 |
| [11–18] | 372 (28.9) | 529 (15.1) | 95 (14.6) | |
| [19–40] | 238 (18.5) | 821 (23.4) | 207 (31.8) | |
| >40 | 240 (18.6) | 1449 (41.3) | 207 (31.8) | |
| Admission type (elective) | 884 (68.6) | 2390 (68.2) | 422 (64.8) | 0.200 |
| Readmission type | ||||
| No readmission | 415 (32.2) | 1071 (30.5) | 278 (42.7) | 0.001 |
| Readmission | ||||
| Non-elective | 387 (44.3) | 1179 (48.4) | 211 (56.6) | |
| Elective | 487 (55.7) | 1256 (51.6) | 162 (43.4) | |
| Sex (male) | 766 (59.4) | 2120 (60.5) | 379 (58.2) | 0.509 |
| Admission on a weekend | 40 (3.1) | 157 (4.5) | 39 (6.0) | 0.010 |
| Primary expected payer | ||||
| Public insurance | 623 (48.3) | 1691 (48.2) | 331 (50.8) | 0.677 |
| Private insurance | 598 (46.4) | 1607 (45.8) | 285 (43.8) | |
| Self-pay & others | 68 (5.3) | 208 (5.9) | 35 (5.4) | |
| Teaching status | ||||
| Teaching | 1179 (91.5) | 3280 (93.6) | 620 (95.2) | 0.004 |
| Hospital designation | ||||
| Large metropolitan | 809 (62.8) | 2524 (72.0) | 499 (76.7) | <0.001 |
| Case volume by quintile (number ofadmissions per hospital in 2016) | ||||
| Very high [236–461] | 369 (28.6) | 664 (18.9) | 131 (20.1) | <0.001 |
| High [152–235] | 256 (19.9) | 674 (19.2) | 119 (18.3) | |
| Medium [96–149] | 215 (16.7) | 703 (20.1) | 169 (26.0) | |
| Low [53–94] | 287 (22.3) | 652 (18.6) | 133 (20.4) | |
| Very low [2–52] | 162 (12.6) | 813 (23.2) | 99 (15.2) | |
| Length of stay | ||||
| Median (IQR *) | 4.0 (3.0–4.0) | 4.0 (3.0–5.0) | 5.0 (3.0–10.0) | <0.001 |
| Daily charge (1000 USD **) | ||||
| Median (IQR *) | 8.6 (5.6–12.3) | 9.3 (6.3–13.4) | 11.2 (7.0–17.6) | <0.001 |
| Causes of Readmission Based on Clinical Classifications Software Refined | N = 1227 |
|---|---|
| Diseases of white blood cells (e.g., neutropenia, agranulocytosis) | 27.8% |
| Septicemia | 15.3% |
| Pancytopenia | 11.5% |
| Complications of other surgical or medical care, injury | 3.7% |
| Diseases of mouth; excluding dental | 2.3% |
| Fever | 2.3% |
| Coagulation and hemorrhagic disorders | 2.0% |
| Intestinal infection | 1.8% |
| Viral infection | 1.8% |
| Pneumonia (except that caused by tuberculosis) | 1.5% |
| Others | 30.0% |
| Risk Ratio (95% Confidence Interval) | |||
|---|---|---|---|
| N = 5446 | Unintentional Readmission (N = 1042) | Unplanned Readmission (N = 1227) | Non-Elective Readmission (N = 1777) |
| Disease state (ref remission) | |||
| Not achieved remission | 1.28 (1.10–1.50) * | 1.24(1.08–1.42) * | 1.12 (1.01–1.23) * |
| Relapse | 1.48 (1.20–1.81) * | 1.44 (1.20–1.73) * | 1.08 (0.93–1.24) |
| Age group (ref >40 age) | |||
| [2–10] | 0.68 (0.58–0.81) * | 0.80 (0.69–0.92) * | 0.91 (0.81–1.01) |
| [11–18] | 0.64 (0.53–0.77) * | 0.73 (0.62–0.86) * | 0.88 (0.78–0.99) * |
| [19–40] | 0.90 (0.79–1.04) | 1.00 (0.88–1.13) | 0.96 (0.87–1.06) |
| Admission type (ref elective) | |||
| Nonelective | 1.21 (1.08–1.36) * | 1.08 (0.97–1.20) | 2.05 (1.90–2.22) * |
| Length of stay (days) | 0.96 (0.95–0.98) * | 0.97 (0.95–0.98) * | 0.98 (0.97–0.99) * |
| Severity (ref extreme) | |||
| Moderate | 0.70 (0.55–0.89) * | 0.69 (0.56–0.86) * | 0.89 (0.75–1.05) |
| Major | 0.83 (0.66–1.04) | 0.84 (0.69–1.02) | 0.95 (0.81–1.12) |
| Primary Payers (ref private insurance) | |||
| Public insurance | 1.19 (1.06–1.33) * | 1.18 (1.06–1.30) * | 1.10 (1.02–1.19) * |
| Self-pay & others | 1.07 (0.84–1.37) | 1.04 (0.83–1.29) | 1.07 (0.91–1.25) |
| Sex (ref female) | |||
| Male | 0.89 (0.80–1.00) | 0.90 (0.81–0.99) * | 0.97 (0.90–1.04) |
| Metropolitan hospital (ref nonteaching) | |||
| Large, teaching | 0.77 (0.62–0.95) * | 0.82 (0.67–0.99) * | 0.85 (0.74–0.99) * |
| Small, teaching | 0.87 (0.70–1.08) | 0.93 (0.77–1.14) | 1.05 (0.90–1.21) |
| Case volume (ref very low case volume) | |||
| Very high | 1.13 (0.94–1.36) | 1.01 (0.85–1.20) | 0.99 (0.87–1.12) |
| High | 0.97 (0.81–1.18) | 0.87 (0.74–1.04) | 0.81 (0.71–0.93) * |
| Medium | 0.98 (0.82–1.18) | 0.98 (0.84–1.15) | 0.94 (0.83–1.06) |
| Low | 1.10 (0.92–1.31) | 1.03 (0.88–1.20) | 1.03 (0.93–1.16) |
| Risk Ratio (95% Confidence Interval) | |||
|---|---|---|---|
| Remission (N = 1289) | Not Achieved Remission (N = 3506) | Relapse (N = 651) | |
| Age group (ref >40 age) | |||
| [2–10] | 0.55 (0.38–0.80) * | 0.67 (0.55–0.83) * | 0.85 (0.56–1.27) |
| [11–18] | 0.43 (0.28–0.65) * | 0.64 (0.51–0.81) * | 1.13 (0.74–1.72) |
| [19–40] | 0.72 (0.48–1.08) | 0.92 (0.78–1.09) | 1.02 (0.71–1.46) |
| Admission type (ref elective) | |||
| Non-elective | 1.16 (0.85–1.58) | 1.32 (1.15–1.51) * | 0.92 (0.68–1.24) |
| Length of stay (days) | 0.91 (0.86–0.96) * | 0.97 (0.95–0.98) * | 0.98 (0.96–1.00) |
| Severity (ref extreme) | |||
| Moderate | 0.32 (0.13–0.77) * | 0.69 (0.52–0.91) * | 0.96 (0.57–1.62) |
| Major | 0.45 (0.19–1.07) | 0.78 (0.60–1.02) | 1.10 (0.71–1.72) |
| Primary Payers (ref private insurance) | |||
| Public insurance | 1.03 (0.78–1.38) | 1.22 (1.07–1.41) * | 1.10 (0.83–1.47) |
| Self-pay and others | 1.16 (0.66–2.07) | 1.05 (0.79–1.40) | 0.90 (0.45–1.82) |
| Sex (ref female) | |||
| Male | 0.87 (0.66–1.14) | 0.90 (0.79–1.03) | 0.90 (0.68–1.19) |
| Metropolitan hospital (ref nonteaching) | |||
| Large, teaching | 0.75 (0.46–1.23) | 0.75 (0.59–0.96) * | 1.53 (0.49–4.69) |
| Small, teaching | 0.84 (0.52–1.37) | 0.81 (0.62–1.04) | 2.18 (0.70–6.77) |
| Case volume (ref very low case volume) | |||
| Very high | 1.10 (0.68–1.79) | 1.09 (0.87–1.36) | 2.17 (1.19–3.97) * |
| High | 1.10 (0.66–1.83) | 0.93 (0.75–1.16) | 1.56 (0.82–2.96) |
| Medium | 1.02 (0.61–1.72) | 0.90 (0.72–1.12) | 1.87 (1.03–3.38) * |
| Low | 1.23 (0.78–1.93) | 1.00 (0.82–1.24) | 2.09 (1.15–3.81) * |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tran, P.T.; Slayton, W.B.; Dalal, M.; Brown, J. Incidence and Risk Factors for 30-Day Readmission after Inpatient Chemotherapy among Acute Lymphoblastic Leukemia Patients. Healthcare 2020, 8, 401. https://doi.org/10.3390/healthcare8040401
Tran PT, Slayton WB, Dalal M, Brown J. Incidence and Risk Factors for 30-Day Readmission after Inpatient Chemotherapy among Acute Lymphoblastic Leukemia Patients. Healthcare. 2020; 8(4):401. https://doi.org/10.3390/healthcare8040401
Chicago/Turabian StyleTran, Phuong T., William B. Slayton, Mansi Dalal, and Joshua Brown. 2020. "Incidence and Risk Factors for 30-Day Readmission after Inpatient Chemotherapy among Acute Lymphoblastic Leukemia Patients" Healthcare 8, no. 4: 401. https://doi.org/10.3390/healthcare8040401
APA StyleTran, P. T., Slayton, W. B., Dalal, M., & Brown, J. (2020). Incidence and Risk Factors for 30-Day Readmission after Inpatient Chemotherapy among Acute Lymphoblastic Leukemia Patients. Healthcare, 8(4), 401. https://doi.org/10.3390/healthcare8040401






