A Qualitative Study Investigating the Barriers to the Implementation of the ‘Sepsis Six Care Bundle’ in Maternity Wards
Abstract
1. Introduction
2. Materials and Methods
2.1. The Quality Criterion
- Research team and reflexivity
- The interviews were conducted by the main author (N.A.), a female doctorate student who was experienced with conducting and analysing interviews. The interviewer had previously undertaken an observational study in the same ward [12] and had become familiar with ward staff and gained the trust of the midwives who were aware of the reason for her presence and subsequent interviews.
- Study design
- The study methodological orientation was based on grounded theory [14] convenience sampling was used to recruit interviewees who were working between 0900 and 1700 when the interviewer was present in the ward. Sampling was conducted over a seven-week period with a target to include a minimum of one midwife from each maternity ward. Face-to-face interviews were conducted with 13 midwives; data on interviewees’ clinical experience within maternity wards was collected. Interviews ceased once data saturation was achieved, in other words, when similarities of information appeared with no new details emerging from the interviews. All interviews were conducted in a quiet area of either the maternity ward or the High Dependency Unit (HDU), depending on each participant’s area of practice.
- Data analysis
- Interviews were audio recorded, transcribed verbatim, and checked for accuracy, although “field notes” had not been taken during any interviews. The interviewees did not review the transcripts due to time and logistical issues. The data were analysed using a thematic analysis approach with the help of NVivo V11 software (QSR International Pty Ltd., Doncaster, Victoria, Australia). The data were independently verified by G.A., who reviewed two of the original transcripts and consensus around emerging codes and themes was obtained.
2.2. The Interview Guide
2.3. Ethics and Consent
3. Results
3.1. Sepsis: A Difficult Diagnosis
“Somebody who commences Sepsis Six for maternal temperature in labour while their body is doing a lot of work, I expect their temperature to be raised. So, I think there’s far too many women who are commenced on Sepsis Six but they don’t have to be, and a lot of babies get antibiotic cover as well.”Participant 4, postnatal ward, >10 years experience.
“Certainly, we don’t have a problem reviewing people, but sometimes when you jump in too quickly it can be. somebody’s due paracetamol at that point. It’s a whole variety of... When sick people come in you know that they’re sick. If they are walking in smiling, then you know that they are not septic.”Participant 10, maternity assessment unit, >10 years experience.
“... We should not be giving people too much antibiotics. That causes its own problems .... But that’s what you have to (do), act on the side of caution, because sepsis is such a serious thing.”Participant 9, postnatal ward, <10 years experience.
“With it being so important ... I would rather be treated when it’s needed treated, to save anything from getting worse.”Participant 13, postnatal ward, >10 years experience.
“I think we overprescribe antibiotics, so we get a lot of people in- just caution ... Now when these women are coming in and we are treating them because the community midwives will go out, check their temperature, the temperature setting at 37.6 or something, their pulse is slightly raised. That’s a normal physiological thing during breast feeding. All these women are coming in getting IV antibiotics, they’re absolutely fine when their inflammatory markers come back. So it is just a matter of experience of knowing ‘is that breast milk or is it sepsis?”Participant 10, maternity assessment unit, >10 years experience.
3.2. Pre-conditions Phase: Suitability of the SSCB in a Maternity Setting
“I think the fact that it’s a set of guidelines for sort of immediate initial management for patients over a one-hour period ... I can kind of get that, that would fit everybody, because it’s almost like an emergency response as a first response and you will do all of these, and then once we’ve got the results of all these investigations, we can then tailor the plan from there.”Participant 9, postnatal ward, <10 years experience.
“If ever it’s needed, it’s all there, but you can use it, or the medical staff can use their judgement to say ‘Right. Actually, she does not need that’.”Participant 13, postnatal ward, >10 years experience.
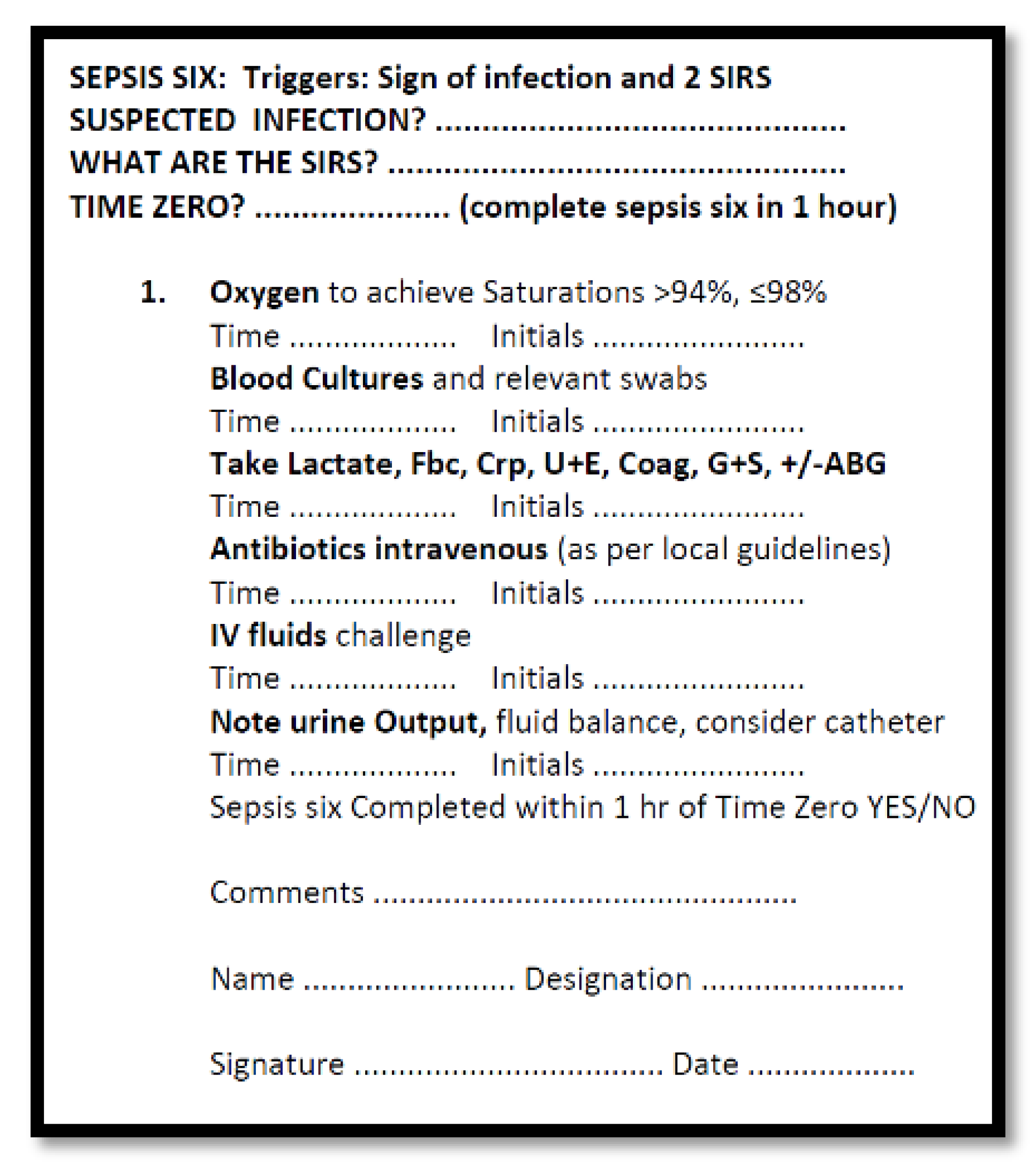
“I think four out of the six, because we don’t always give oxygen, we don’t always do urine. It just depends.”Participant 10, maternity assessment unit, >10 years experience.
“You wouldn’t get into trouble … for it. They would maybe just get you to read up your protocol again but you would not be doing anybody any harm.”Participant 12, HDU/labour ward, <10 years experience.
“Somebody in a postnatal ward who requires a Sepsis Six sticker, to me, should not be in the postnatal ward. She should be transferred out of the postnatal ward, if they require all the criteria that is on it.”Participant 4, postnatal ward, >10 years experience.
“If it’s a new midwife ..., we’ll say ‘Look, she might not need that. Do you want to discuss that with ... a doctor?’ Or if it’s maybe a junior doctor (and) we felt what happened, in our experience, that we wouldn’t normally do that, we’d say ‘Can you just double check with your registrar?’ ... So we’ll get them to check with somebody more senior”Participant 13, postnatal ward, >10 years experience.
“Some people will be catheterized unnecessarily or possibly commenced on IV antibiotics unnecessarily. So that’s my concern of having the sticker.”Participant 4, postnatal ward, >10 years experience.
“None of us have a crystal ball that can tell what’s going to happen in the future, so you just have to go with the protocol and (against) your judgment sometimes.”Participant 13, postnatal ward, >10 years experience.
3.3. Pre-Implementation Phase: Staff Training
“If they want to introduce it to the postnatal ward (it’s essential) that they explain it to people before they do, because I was just told ‘Sepsis Six–there is a drawer with packs in it’.”Participant 4, postnatal ward, >10 years experience.
“Someone who’s unwell, would I go and get the sticker so I could follow the list, or would I wait until everything had been dealt with and then get the sticker, so ‘I did that, I did that’.”Participant 9, postnatal ward, <10 years experience.
“I don’t think that I can tell you what the sticker looks like. I’m not sure that anyone has ever shown me the sticker and what to do with it.”Participant 9, postnatal ward, <10 years experience.
“I suppose with it being a sticker, then you have to go and get it, and stick it in. Whether this is the best thing, or should it be something somewhere in the notes, a page that you turn to, ‘We are now doing sepsis’.”Participant 9, postnatal ward, <10 years experience.
“We don’t have the sticker so we do not follow it the way that they possibly do.”Participant 4, postnatal ward, >10 years experience.
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B
- ❖ How can you identify a patient with sepsis in your ward?
- ❖ Elaborate on each element in the care bundle
- ❖ Elaborate on antibiotic de-escalation
References
- Bonet, M.; Brizuela, V.; Abalos, E.; Cuesta, C.; Baguiya, A.; Chamillard, M.; Fawole, B.; Knight, M.; Kouanda, S.; Lumbiganon, P.; et al. Frequency and management of maternal infection in health facilities in 52 countries (GLOSS): A 1-week inception cohort study. Lancet Glob. Health 2020, 8, e661–e671. [Google Scholar] [CrossRef]
- Acosta, C.D.; Harrison, D.A.; Rowan, K.; Lucas, D.N.; Kurinczuk, J.J.; Knight, M. Maternal morbidity and mortality from severe sepsis: A national cohort study. BMJ Open 2016, 6, 1–8. [Google Scholar] [CrossRef]
- Acosta, C.D.; Bhattacharya, S.; Tuffnell, D.; Kurinczuk, J.J.; Knight, M. Maternal sepsis: A Scottish population-based case–control study. BJOG Int. J. Obstet. Gynaecol. 2012, 119, 474–483. [Google Scholar] [CrossRef]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Resar, R.; Griffin, F.A.; Haraden, C.; Nolan, T.W. Using Care Bundles to Improve Health Care Quality. In IHI Innovation Series white paper; Institute for Healthcare Improvement: Cambridge, MA, USA, 2012; Available online: www.IHI.org (accessed on 17 April 2020).
- Fulbrook, P.; Mooney, S. Care bundles in critical care: A practical approach to evidence-based practice. Nurs. Crit. Care. 2003, 8, 249–255. [Google Scholar] [CrossRef]
- The UK Sepsis Trust. ED/AMU Sepsis Screening & Action Tool. Available online: https://sepsistrust.org/wp-content/uploads/2018/06/ED-adult-NICE-Final-1107.pdf (accessed on 19 May 2020).
- Proctor, E.K.; Powell, B.J.; McMillen, J.C. Implementation strategies: Recommendations for specifying and reporting. Implement. Sci. 2013, 8, 139. [Google Scholar] [CrossRef]
- Powell, B.J.; Beidas, R.S.; Lewis, C.C.; Aarons, G.A.; McMillen, J.C.; Proctor, E.K.; Mandell, D.S. Methods to improve the selection and tailoring of implementation strategies. J. Behav. Health Serv. Res. 2017, 44, 177–194. [Google Scholar] [CrossRef]
- Kilbourne, A.M.; Neumann, M.S.; Pincus, H.A.; Bauer, M.S.; Stall, R. Implementing evidence-based interventions in health care: Application of the replicating effective programs framework. Implement. Sci. 2007, 2, 42. [Google Scholar] [CrossRef]
- Scottish Antimicrobial Prescribing Group & NHS Education for Scotland. Exploring the Role of Nurses and Midwives in Antimicrobial Stewardship. 2014. Available online: http://www.nes.scot.nhs.uk/about-us/whats-new/exploring-the-role-of-nurses-and-midwives-in-antimicrobial-stewardship.aspx (accessed on 23 April 2020).
- Abutheraa, N. Antimicrobial Stewardship in the Management of Sepsis in Maternity Hospitals: A Mixed Methodology Study. Ph.D. Thesis, University of Strathclyde, Glasgow, UK, 2018. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care. 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Charmaz, K. Constructing Grounded Theory; Sage: London, UK, 19 March 2014. [Google Scholar]
- Turi, S.K.; Von Ah, D. Implementation of early goal-directed therapy for septic patients in the emergency department: A review of the literature. J. Emerg. Nurs. 2013, 39, 13–19. [Google Scholar] [CrossRef]
- The National Institute for Health and Care Excellence. Procalcitonin testing for diagnosing and monitoring sepsis (ADVIA Centaur BRAHMS PCT assay, BRAHMS PCT Sensitive Kryptor assay, Elecsys BRAHMS PCT assay, LIAISON BRAHMS PCT assay and VIDAS BRAHMS PCT assay). In Diagnostics Guidance [DG18]; NICE Guidance: London, UK, 2015; Available online: https://www.nice.org.uk/guidance/dg18 (accessed on 23 April 2020).
- Guinn, D.A.; Abel, D.E.; Tomlinson, M.W. Early goal directed therapy for sepsis during pregnancy. Obstet. Gynecol. Clin. North Am. 2007, 34, 459–479. [Google Scholar] [CrossRef] [PubMed]
- Daniels, R.; Nutbeam, T.; McNamara, G.; Galvin, C. The sepsis six and the severe sepsis resuscitation bundle: A prospective observational cohort study. Emerg. Med. J. 2011, 28, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Say, L.; Chou, D.; Gemmill, A.; Tunçalp, Ö.; Moller, A.-B.; Daniels, J.; Gülmezoglu, A.M.; Temmerman, M.; Alkema, L. Global causes of maternal death: A WHO systematic analysis. Lancet Glob. Health 2014, 2, e323–e333. [Google Scholar] [CrossRef]
- Lewis, C.C.; Klasnja, P.; Powell, B.J.; Lyon, A.R.; Tuzzio, L.; Jones, S.; Walsh-Bailey, C.; Weiner, B. From classification to causality: Advancing understanding of mechanisms of change in implementation science. Front. Public Health 2018, 6, 136. [Google Scholar] [CrossRef] [PubMed]
- Huynh, A.K.; Hamilton, A.B.; Farmer, M.M.; Bean-Mayberry, B.; Stirman, S.W.; Moin, T.; Finley, E.P. A pragmatic approach to guide implementation evaluation research: Strategy mapping for complex interventions. Front. Public Health 2018, 6, 134. [Google Scholar] [CrossRef]
- Gilissen, J.; Pivodic, L.; Smets, T.; Gastmans, C.; Vander Stichele, R.; Deliens, L.; Van den Block, L. Preconditions for successful advance care planning in nursing homes: A systematic review. Int. J. Nurs. Stud. 2017, 66, 47–59. [Google Scholar] [CrossRef]
- Chen, G.; Klimoski, R.J. Training and development of human resources at work: Is the state of our science strong? Hum. Resour. Manag. Rev. 2007, 17, 180–190. [Google Scholar] [CrossRef]
- Chaghari, M.; Saffari, M.; Ebadi, A.; Ameryoun, A. Empowering education: A new model for in-service training of nursing staff. J. Adv. Med. Educ. Prof. 2017, 5, 26. [Google Scholar]
- Roberts, N.; Hooper, G.; Lorencatto, F.; Storr, W.; Spivey, M. Barriers and facilitators towards implementing the Sepsis Six care bundle (BLISS-1): A mixed methods investigation using the theoretical domains framework. Scand. J. Trauma. Resusc. Emerg. Med. 2017, 25, 96. [Google Scholar] [CrossRef]
- Aggarwal, R.; Deutsch, L.; Harrison, S.; Stapleton, C.; Stanley, S.; Wright, A. ‘Sepsis six’-adaptation of a trust innovation in maternity. BJOG Int. J. Obstet. Gynaecol. 2015, 122, 233. [Google Scholar]
- Lehane, E.; Leahy-Warren, P.; O’Riordan, C.; Savage, E.; Drennan, J.; O’Tuathaigh, C.; O’Connor, M.; Corrigan, M.; Burke, F.; Hayes, M.; et al. Evidence-based practice education for healthcare professions: An expert view. BMJ Evid. Based Med. 2019, 24, 103–108. [Google Scholar] [CrossRef]
- Livorsi, D.; Comer, A.; Matthias, M.S.; Perencevich, E.N.; Bair, M.J. Factors influencing antibiotic-prescribing decisions among inpatient physicians: A qualitative investigation. Infect. Control. Hosp. Epidemiol. 2015, 36, 1065–1072. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abutheraa, N.; Mullen, A.B.; Grant, J.; Akram, G. A Qualitative Study Investigating the Barriers to the Implementation of the ‘Sepsis Six Care Bundle’ in Maternity Wards. Healthcare 2020, 8, 374. https://doi.org/10.3390/healthcare8040374
Abutheraa N, Mullen AB, Grant J, Akram G. A Qualitative Study Investigating the Barriers to the Implementation of the ‘Sepsis Six Care Bundle’ in Maternity Wards. Healthcare. 2020; 8(4):374. https://doi.org/10.3390/healthcare8040374
Chicago/Turabian StyleAbutheraa, Nouf, Alexander B. Mullen, June Grant, and Gazala Akram. 2020. "A Qualitative Study Investigating the Barriers to the Implementation of the ‘Sepsis Six Care Bundle’ in Maternity Wards" Healthcare 8, no. 4: 374. https://doi.org/10.3390/healthcare8040374
APA StyleAbutheraa, N., Mullen, A. B., Grant, J., & Akram, G. (2020). A Qualitative Study Investigating the Barriers to the Implementation of the ‘Sepsis Six Care Bundle’ in Maternity Wards. Healthcare, 8(4), 374. https://doi.org/10.3390/healthcare8040374




