Attitudes and Behavior towards Interprofessional Collaboration among Healthcare Professionals in a Large Academic Medical Center
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey Design
2.2. Ethical Considerations
2.3. Study Site and Study Population
2.4. Survey Administration
2.5. Statistical Analysis
3. Results
3.1. Characteristics of Study Participants
3.2. Attitudes toward Interprofessional Collaboration
3.2.1. Attitudes toward Interprofessional Collaboration Regarding Patient Care
3.2.2. Attitudes toward Interprofessional Collaboration Regarding Healthcare Team
3.3. Interprofessional Collaboration Behavior and Experience
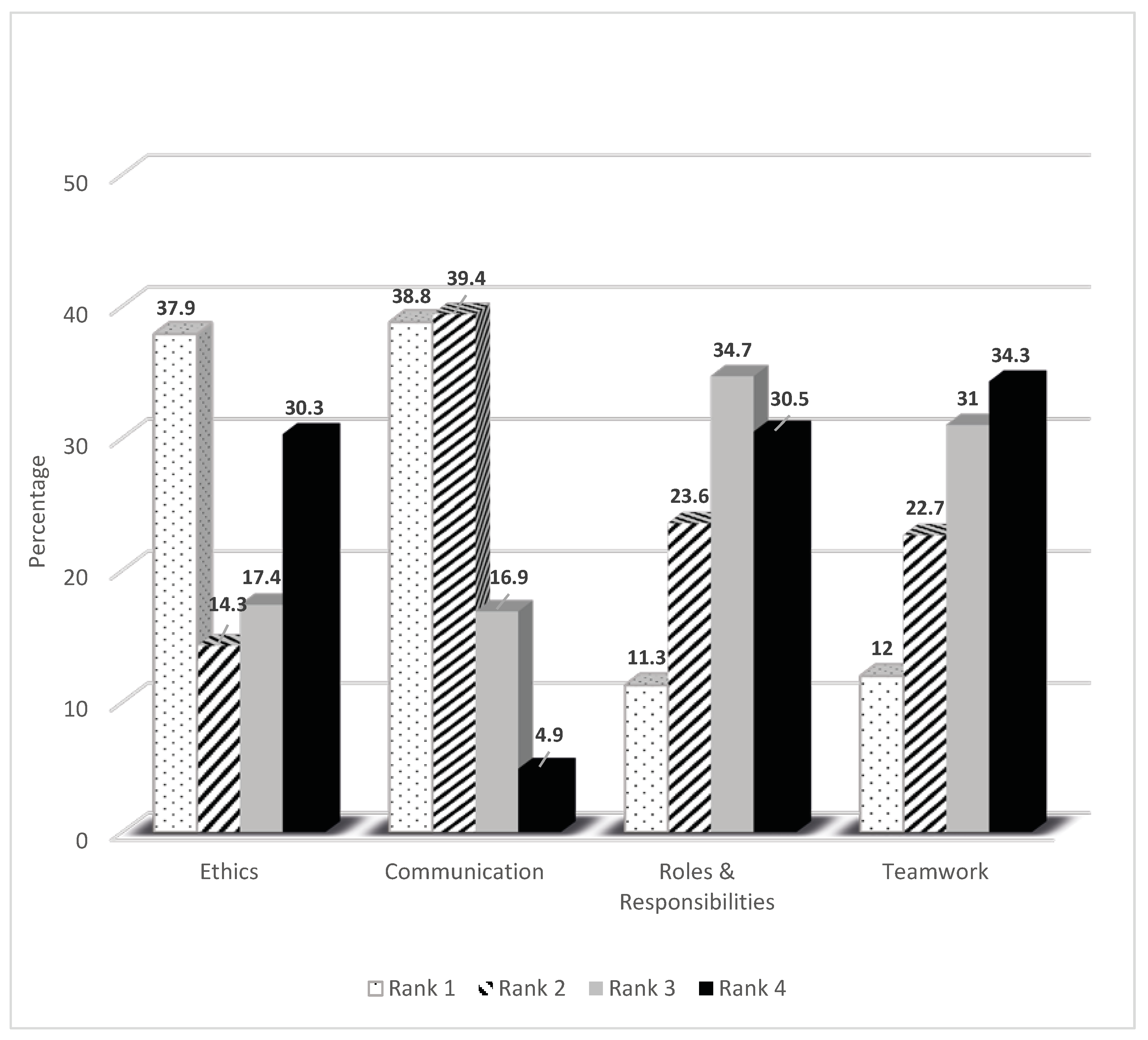
3.4. Ranking of IPEC Competencies
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Marinez-Moyano, I.J.; Schuman, S. Creating a Culture of Collaboration: The International Association of Facilitators Handbook; Jossey-Bass/Wiley: Hoboken, NJ, USA, 2006; p. 83. ISBN 0-7879-8116-8. [Google Scholar]
- World Health Organization. Framework for Action on Interprofessional Education and Collaborative Practice; World Health Organization: Geneva, Switzerland, 2010; Available online: https://www.who.int/hrh/resources/framework_action/en/ (accessed on 31 July 2020).
- Busari, J.O.; Moll, F.M.; Duits, A.J. Understanding the impact of interprofessional collaboration on the quality of care: A case report from a small-scale resource limited health care environment. J. Multidiscip. Healthc. 2017, 10, 227–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franklin, C.M.; Bernhardt, J.M.; Lopez, R.P.; Long-Middleton, E.R.; Davis, S. Interprofessional Teamwork and Collaboration between Community Health Workers and Healthcare Teams. Health Serv. Res. Manag. Epidemiol. 2015, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bridges, D.R.; Davidson, R.A.; Odegard, P.S.; Maki, I.V.; Tomkowiak, J. Interprofessional collaboration: Three best practice models of interprofessional education. Med. Educ. Online 2011, 16, 766. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Interprofessional Educational Collaborative. Core Competencies for Interprofessional Collaborative: 2016 Update; Interprofessional Educational Collaborative: Washington, DC, USA, 2016; Available online: https://hsc.unm.edu/ipe/resources/ipec-2016-core-competencies.pdf (accessed on 31 July 2020).
- Nancarrow, S.A.; Booth, A.; Ariss, S.M.B.; Smith, T.; Enderby, P.; Roots, A. Ten principles of good interdisciplinary team work. Hum. Resour. Health 2013, 11, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bosch, B.; Mansell, H. Interprofessional collaboration in health care. Can. Pharm. J. 2015, 148, 176–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wheelan, S.A.; Burchill, C.N.; Tilin, F. The Link between Teamwork and Patients’ Outcomes in Intensive Care Units. Am. J. Crit. Care 2003, 12, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Mickan, S.; Hoffman, S.J.; Nasmith, L.; on behalf of the World Health Organization Study Group on Interprofessional Education. Collaborative practice in a global health context: Common themes from developed and developing countries. J. Interprof. Care 2010, 24, 492–502. [Google Scholar] [CrossRef] [PubMed]
- Tsou, P.; Shih, J.; Ho, M.-J. A comparative study of professional and interprofessional values between health professional associations. J. Interprof. Care 2015, 29, 628–633. [Google Scholar] [CrossRef]
- Wagner, E.H. The role of patient care teams in chronic disease management. BMJ 2000, 320, 569–572. [Google Scholar] [CrossRef] [Green Version]
- Gougeon, L.; Johnson, J.; Morse, H. Interprofessional collaboration in health care teams for the maintenance of community-dwelling seniors’ health and well-being in Canada: A systematic review of trials. J. Interprof. Educ. Pract. 2017, 7, 29–37. [Google Scholar] [CrossRef]
- Epstein, N. Multidisciplinary in-hospital teams improve patient outcomes: A review. Surg. Neurol. Int. 2014, 5, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Pantilat, S.Z.; Lindenauer, P.K.; Katz, P.P.; Wachter, R.M. Primary care physician attitudes regarding communication with hospitalists. Am. J. Med. 2001, 111, 15–20. [Google Scholar] [CrossRef]
- Øvretveit, J. Does Clinical Coordination Improve Quality and Save Money? The Health Foundation: London, UK, 2011. [Google Scholar]
- Vernon, M.M.; Moore, N.; Mazzoli, A.; De Leo, G. Respiratory therapy faculty perspectives on interprofessional education: Findings from a cross-sectional online survey. J. Interprof. Care 2017, 32, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Vernon, M.M.; Moore, N.M.; Cummins, L.-A.; Reyes, S.E.; Mazzoli, A.J.; Heboyan, V.; De Leo, G. Respiratory Therapy Faculty Knowledge of and Attitudes toward Interprofessional Education. Respir. Care 2017, 62, 873–881. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tolle, S.L.; Vernon, M.M.; McCombs, G.; De Leo, G. Interprofessional Education in Dental Hygiene: Attitudes, barriers and practices of program faculty. J. Dent. Hyg. 2019, 93, 13–22. [Google Scholar]
- Patton, Z.; Vernon, M.; Haymond, K.; Anglin, J.; Heboyan, V.; De Leo, G. Evaluation of Interprofessional Education Implementation among Nutrition Program Directors in the United States. Top. Clin. Nutr. 2018, 33, 196–204. [Google Scholar] [CrossRef]
- Kent, F.; Glass, S.; Courtney, J.; Thorpe, J.; Nisbet, G. Sustainable interprofessional learning on clinical placements: The value of observing others at work. J. Interprof. Care 2020, 1–7. [Google Scholar] [CrossRef]
- Armstrong, K.J.; Walker, S.E.; Feld, S.D.; Weidner, T.G. Athletic training students’ engagement in interprofessional education in the classroom and during clinical education. J. Interprof. Care 2019, 1–6. [Google Scholar] [CrossRef]
- Zechariah, S.; Ansa, B.E.; Johnson, S.; Gates, A.; De Leo, G. Interprofessional Education and Collaboration in Healthcare: An Exploratory Study of the Perspectives of Medical Students in the United States. Healthcare 2019, 7, 117. [Google Scholar] [CrossRef] [Green Version]
- Curran, V.; Sharpe, D.; Forristall, J. Attitudes of health sciences faculty members towards interprofessional teamwork and education. Med. Educ. 2007, 41, 892–896. [Google Scholar] [CrossRef]
- Hepp, S.L.; Suter, E.; Jackson, K.; Deutschlander, S.; Makwarimba, E.; Jennings, J.; Birmingham, L. Using an interprofessional competency framework to examine collaborative practice. J. Interprof. Care 2014, 29, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Clay-Williams, R.; Plumb, J.; Luscombe, G.; Hawke, C.; Dalton, H.; Shannon, G.; Johnson, J. Improving Teamwork and Patient Outcomes with Daily Structured Interdisciplinary bedside Rounds: A Multimethod Evaluation. J. Hosp. Med. 2018, 13, 311–317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hughes, J.K.; Allen, A.; McLane, T.; Stewart, J.L.; Heboyan, V.; De Leo, G. Interprofessional Education among Occupational Therapy Programs: Faculty Perceptions of Challenges and Opportunities. Am. J. Occup. Ther. 2019, 73. [Google Scholar] [CrossRef] [PubMed]
- Alcusky, M.; Ferrari, L.; Rossi, G.; Liu, M.; Hojat, M.; Maio, V. Attitudes Toward Collaboration among Practitioners in Newly Established Medical Homes. Am. J. Med. Qual. 2016, 31, 526–535. [Google Scholar] [CrossRef]
- Braithwaite, D.; Emery, J.; De Lusignan, S.; Sutton, S. Using the Internet to conduct surveys of health professionals: A valid alternative? Fam. Pract. 2003, 20, 545–551. [Google Scholar] [CrossRef]
- Cifuentes, M.; Boyer, J.; Gore, R.; D’Errico, A.; Scollin, P.; Tessler, J.; Lerner, D.; Kriebel, D.; Punnett, L.; Slatin, C.; et al. Job strain predicts survey response in healthcare industry workers. Am. J. Ind. Med. 2008, 51, 281–289. [Google Scholar] [CrossRef] [Green Version]
| Healthcare Professions | |||||||
|---|---|---|---|---|---|---|---|
| Variables | Total | Advanced Nurse Practitioners | Physicians (MD, Fellows, Residents) | Nursing | Allied Health (RD, PA, PT, OT, SLP, SW, RT) | Pharmacist | Other Professional |
| N = 551 (%) | N = 15 (%) | N = 138 (%) | N = 316 (%) | N = 65 (%) | N = 14 (%) | N = 3 (%) | |
| Gender | |||||||
| Males | 126 (22.9) | 1 (6.7) | 87 (63.0) | 23 (7.3) | 10 (15.4) | 4 (28.6) | 1 (33.3) |
| Females | 425 (77.1) | 14 (93.3) | 51 (37.0) | 293 (92.7) | 55 (84.6) | 10 (71.4) | 2 (66.7) |
| Age in Years | |||||||
| 20–29 | 76 (13.8) | 2 (13.3) | 25 (18.1) | 26 (8.2) | 17 (26.2) | 6 (42.9) | 0 (0) |
| 30–39 | 135 (24.5) | 3 (20.0) | 51 (37.0) | 63 (19.9) | 15 (23.1) | 3 (21.4) | 0 (0) |
| 40–49 | 138 (25.0) | 7 (46.7) | 20 (14.5) | 91 (28.8) | 15 (23.1) | 3 (21.4) | 2 (66.7) |
| 50–59 | 140 (25.4) | 1 (6.7) | 23 (16.7) | 100 (31.6) | 16 (24.6) | 0 (0) | 0 (0) |
| 60–69 | 54 (9.8) | 2 (13.3) | 14 (10.1) | 33 (10.4) | 2 (3.1) | 2 (14.3) | 1 (33.3) |
| >69 | 8 (1.5) | 0 (0) | 5 (3.6) | 3 (0.9) | 0 (0) | 0 (0) | 0 (0) |
| Ethnic Background | |||||||
| White, non-Hispanic | 408 (74.0) | 12 (80) | 93 (67.4) | 237 (75.0) | 52 (80.0) | 12 (85.7) | 2 (66.7) |
| Black, non-Hispanic | 68 (12.3) | 2 (13.3) | 11 (8.0) | 48 (15.2) | 7 (10.8) | 0 (0) | 0 (0) |
| Hispanic | 16 (2.9) | 0 (0) | 13 (9.4) | 3 (0.9) | 0 (0) | 0 (0) | 0 (0) |
| Asian/non-Pacific Islander, non-Hispanic | 34 (6.2) | 0 (0) | 16 (11.6) | 13 (4.1) | 3 (4.6) | 1 (7.1) | 1 (33.3) |
| Multiple races | 20 (3.6) | 1 (6.7) | 3 (2.2) | 13 (4.1) | 2 (3.1) | 1 (7.1) | 0 (0) |
| Other | 5 (0.9) | 0 (0) | 2 (1.4) | 2 (0.6) | 1 (1.5) | 0 (0) | 0 (0) |
| Highest Degree | |||||||
| Associates | 104 (18.9) | 0 (0) | 0 (0) | 96 (30.4) | 8 (12.3) | 0 (0) | 0 (0) |
| Bachelors | 198 (35.9) | 0 (0) | 0 (0) | 171 (54.1) | 25 (38.5) | 1 (7.1) | 1 (33.3) |
| Masters | 76 (13.8) | 11 (73.3) | 0 (0) | 40 (12.7) | 24 (36.9) | 1 (7.1) | 0 (0) |
| Doctoral | 30 (5.4) | 4 (26.7) | 2 (1.4) | 2 (0.6) | 8 (12.3) | 12 (85.7) | 2 (66.7) |
| Medical | 136 (24.7) | 0 (0) | 136 (98.6) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| No Response | 7 (1.3) | 0 (0) | 0 (0) | 7 (2.2) | 0 (0) | 0 (0) | 0 (0) |
| Years of Practice | |||||||
| <5 | 84 (15.2) | 0 (0) | 37 (26.8) | 26 (8.2) | 16 (24.6) | 5 (35.7) | 0 (0) |
| 5–10 | 97 (17.6) | 3 (20.0) | 32 (23.2) | 44 (13.9) | 14 (21.5) | 4 (28.6) | 0 (0) |
| 11–15 | 66 (12.0) | 4 (26.7) | 15 (10.9) | 38 (12.0) | 7 (10.8) | 1 (7.1) | 1 (33.3) |
| 16–20 | 69 (12.5) | 1 (6.7) | 11 (8.0) | 45 (14.2) | 10 (15.4) | 1 (7.1) | 1 (33.3) |
| >20 | 235 (42.6) | 7 (46.7) | 43 (31.2) | 163 (51.6) | 18 (27.7) | 3 (21.4) | 1 (33.3) |
| Area of work | |||||||
| Inpatient | 291 (52.8) | 9 (60.0) | 67 (48.6) | 164 (51.9) | 45 (69.2) | 6 (42.9) | 0 (0) |
| Outpatient | 144 (26.1) | 4 (26.7) | 44 (31.9) | 74 (23.4) | 16 (24.6) | 6 (42.9) | 0 (0) |
| Emergency | 36 (6.5) | 1 (6.7) | 16 (11.6) | 19 (6.0) | 0 (0) | 0 (0) | 0 (0) |
| Other Locations | 80 (14.5) | 1 (6.7) | 11 (8.0) | 59 (18.7) | 4 (6.2) | 2 (14.3) | 3 (100.0) |
| A: Attitudes Toward Interprofessional Collaboration Regarding Patient Care | ||||||
| Questions | Responses (N = 551) | |||||
| Strongly Disagree N (%) | Disagree N (%) | Neither Agree nor Disagree N (%) | Agree N (%) | Strongly Agree N (%) | Mean ± SD | |
| Patients receiving interprofessional care are more likely than others to be treated as a whole person | 3 (0.5) | 14 (2.5) | 41 (7.4) | 202 (36.7) | 291 (52.8) | 4.39 ± 0.78 |
| Patients would ultimately benefit if health care professionals worked together to solve patient problems | 1 (0.2) | 1 (0.2) | 3 (0.5) | 120 (21.8) | 426 (77.3) | 4.76 ± 0.48 |
| The “give and take” among team members helps providers make better patient care decisions | 2 (0.4) | 10 (1.8) | 43 (7.8) | 231 (41.9) | 265 (48.1) | 4.36 ± 0.73 |
| The interprofessional approach makes the delivery of patient care more efficient | 4 (0.7) | 11 (2.0) | 59 (10.7) | 176 (31.9) | 301 (54.6) | 4.38 ± 0.81 |
| Reporting observations to a multidisciplinary team helps team members better understand the role of other health care professionals | 1 (0.2) | 7 (1.3) | 34 (6.2) | 197 (35.8) | 312 (56.6) | 4.47 ± 0.69 |
| Interprofessional collaboration increases the health care teams ability to understand clinical problems | 1 (0.2) | 1 (0.2) | 26 (4.7) | 206 (37.4) | 317 (57.5) | 4.52 ± 0.61 |
| Working in an interprofessional manner unnecessarily complicates patient care | 157 (28.5) | 212 (38.5) | 59 (10.7) | 59 (10.7) | 64 (11.6) | 2.38 ± 1.31 |
| B: Attitudes Toward Interprofessional Collaboration regarding the Healthcare Team | ||||||
| Questions | Responses (N = 551) | |||||
| Interprofessional collaboration helps healthcare professionals think positively about the health care team | 2 (0.4) | 9 (1.6) | 82 (14.9) | 255 (46.3) | 203 (36.8) | 4.18 ± 0.77 |
| Communication skills are critical for the healthcare team for improved patient outcomes | 0 (0) | 1 (0.2) | 8 (1.5) | 121 (22.0) | 421 (76.4) | 4.75 ± 0.48 |
| Interprofessional collaboration allows healthcare professionals to understand their role limitations | 2 (0.4) | 24 (4.4) | 93 (16.9) | 248 (45.0) | 184 (33.4) | 4.07 ± 0.84 |
| For interprofessional collaboration to be effective, the healthcare team needs to trust and respect each other | 2 (0.4) | 0 (0) | 9 (1.6) | 148 (26.9) | 392 (71.1) | 4.68 ± 0.54 |
| Team meetings foster communication among members from different professions and disciplines | 0 (0) | 6 (1.1) | 42 (7.6) | 234 (42.5) | 269 (48.8) | 4.39 ± 0.68 |
| Working in an interprofessional environment keeps health professionals enthusiastic and interested in their jobs | 3 (0.5) | 14 (2.5) | 124 (22.5) | 228 (41.4) | 182 (33.0) | 4.04 ± 0.84 |
| Working in an interprofessional manner requires additional time | 18 (3.3) | 89 (16.2) | 143 (26.0) | 196 (35.6) | 105 (19.1) | 3.51 ± 1.07 |
| For interprofessional collaboration to be effective, members of the healthcare team must work within their scope of practice | 0 (0) | 12 (2.2) | 52 (9.4) | 258 (46.8) | 229 (41.6) | 4.28 ± 0.72 |
| Questions | Responses | ||||||
|---|---|---|---|---|---|---|---|
| N * | Strongly Disagree N (%) | Disagree N (%) | Neither Agree nor Disagree N (%) | Agree N (%) | Strongly Agree N (%) | Mean ± SD | |
| I am included in patient care decision making | 533 | 11 (2.1) | 34 (6.4) | 55 (10.3) | 236 (44.3) | 197 (37.0) | 4.08 ± 0.95 |
| I participate in multi-disciplinary patient care rounds | 464 | 25 (5.4) | 80 (17.2) | 62 (13.4) | 166 (35.8) | 131 (28.2) | 3.64 ± 1.21 |
| My recommendations for patient care are routinely implemented | 525 | 17 (3.2) | 36 (6.9) | 107 (20.4) | 242 (46.1) | 123 (23.4) | 3.80 ± 0.98 |
| I attend multi-disciplinary education sessions (i.e., grand rounds, journal clubs, seminars) | 468 | 47 (10.0) | 117 (25.0) | 65 (13.9) | 133 (28.4) | 106 (22.7) | 3.29 ± 1.33 |
| I am encouraged to raise concerns regarding patient care | 540 | 14 (2.6) | 25 (4.6) | 50 (9.3) | 247 (45.7) | 204 (37.8) | 4.11 ± 0.94 |
| I value the role of other healthcare professionals | 548 | 1 (0.2) | 1 (0.2) | 9 (1.6) | 177 (32.3) | 360 (65.7) | 4.63 ± 0.55 |
| I feel there is a climate of mutual respect within the healthcare team | 543 | 31 (5.7) | 82 (15.1) | 93 (17.1) | 232 (42.7) | 105 (19.3) | 3.55 ± 1.13 |
| I value input from members of the healthcare team who are outside my own professional role | 546 | 1 (0.2) | 3 (0.5) | 10 (1.8) | 232 (42.5) | 300 (54.9) | 4.51 ± 0.58 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ansa, B.E.; Zechariah, S.; Gates, A.M.; Johnson, S.W.; Heboyan, V.; De Leo, G. Attitudes and Behavior towards Interprofessional Collaboration among Healthcare Professionals in a Large Academic Medical Center. Healthcare 2020, 8, 323. https://doi.org/10.3390/healthcare8030323
Ansa BE, Zechariah S, Gates AM, Johnson SW, Heboyan V, De Leo G. Attitudes and Behavior towards Interprofessional Collaboration among Healthcare Professionals in a Large Academic Medical Center. Healthcare. 2020; 8(3):323. https://doi.org/10.3390/healthcare8030323
Chicago/Turabian StyleAnsa, Benjamin E., Sunitha Zechariah, Amy M. Gates, Stephanie W. Johnson, Vahé Heboyan, and Gianluca De Leo. 2020. "Attitudes and Behavior towards Interprofessional Collaboration among Healthcare Professionals in a Large Academic Medical Center" Healthcare 8, no. 3: 323. https://doi.org/10.3390/healthcare8030323






