Burnout Syndrome in Paediatric Oncology Nurses: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Study Aims
3. Material and Method
3.1. Search Sources and Search Strategy
3.2. Inclusion and Exclusion Criteria
3.3. Study Selection and Procedure
3.4. Variables and Data Encoding
3.5. Data Analysis
4. Results
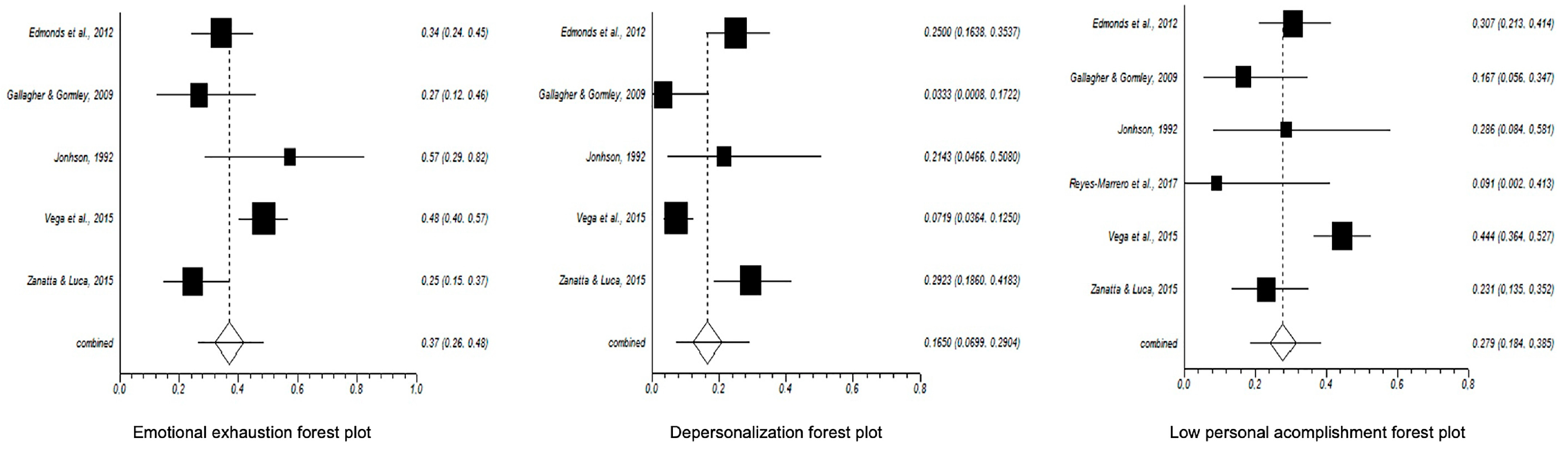
4.1. Burnout Prevalence and Meta-Analytical Estimation
4.2. Levels of Burnout
4.3. Risk Factors for Burnout in Paediatric Oncology Nurses
5. Discussion
5.1. Implications for Healthcare Practice
5.2. Study Limitations
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Iserson, K.V. Burnout syndrome: Global medicine volunteering as a possible treatment strategy. J. Emerg. Med. 2018, 54, 516–521. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M. Maslach Burnout Inventory Manual; Mind Garden: Menlo Park, CA, USA, 2016. [Google Scholar]
- Jo, I.; Lee, S.; Sung, G.; Kim, M.; Lee, S.; Park, J.; Lee, K. Relationship between burnout and PTSD symptoms in firefighters: The moderating effects of a sense of calling to firefighting. Int. Arch. Occup. Environ. Health 2018, 91, 117–123. [Google Scholar] [CrossRef] [PubMed]
- De la Fuente, E.I.; Lozano, L.M.; García-Cueto, E.; San Luis, C.; Vargas, C.; Cañadas, G.R.; Cañadas-De la Fuente, G.A.; Hambleton, R.K. Development and validation of the granada burnout questionnaire in spanish police. Int. J. Clin. Health. Psychol. 2013, 13, 216–225. [Google Scholar] [CrossRef]
- Hu, Q.; Schaufeli, W.B.; Taris, T.W. How are changes in exposure to job demands and job resources related to burnout and engagement? A longitudinal study among Chinese nurses and police officers. Stress Health 2017, 33, 631–644. [Google Scholar] [CrossRef] [PubMed]
- Stearns, S.; Shoji, K.; Benight, C.C. Burnout among US military behavioral health providers. J. Nerv. Ment. Dis. 2018, 206, 398–409. [Google Scholar] [CrossRef] [PubMed]
- Shen, B.; McCaughtry, N.; Martin, J.; Gran, A.; Kulik, N.; Fahlman, M. The relationship between teacher burnout and student motivation. Br. J. Educ. Psychol. 2015, 85, 519–532. [Google Scholar] [CrossRef]
- Van den Berg, J.W.; Mastenbroek, N.J.J.M.; Scheepers, R.A.; Jaarsma, A.D.C. Work engagement in health professions education. Med. Teach. 2017, 39, 1110–1118. [Google Scholar] [CrossRef]
- Abdulrahman, M.; Farooq, M.M.; Al Kharmiri, A.; Al Marzooqi, F.; Carrick, F.R. Burnout and depression among medical residents in the United Arab Emirates: A multicenter study. J. Family Med. Prim Care 2018, 7, 435–441. [Google Scholar] [CrossRef]
- Anandarajah, A.P.; Quill, T.E.; Privitera, M.R. Adopting the quadruple aim: The University of Rochester Medical Center Experience: Moving from physician burnout to physician resilience. Am. J. Med. 2018, 131, 979–986. [Google Scholar] [CrossRef]
- Monsalve-Reyes, C.S.; San Luis-Costas, C.; Gómez-Urquiza, J.L.; Albendín-García, L.; Aguayo, R.; Cañadas-De la Fuente, G.A. Burnout syndrome and its prevalence in primary care nursing: A systematic review and meta-analysis. BMC Fam. Pract. 2018, 19, 59. [Google Scholar] [CrossRef] [PubMed]
- Hunsaker, S.; Chen, H.C.; Maughan, D.; Heaston, S. Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. J. Nurs. Scholarsh. 2015, 47, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Urquiza, J.L.; De la Fuente-Solana, E.I.; Albendín-García, L.; Vargas-Pecino, C.; Ortega-Campos, E.M.; Cañadas-De la Fuente, G.A. Prevalence of burnout syndrome in emergency nurses: A meta-analysis. Crit. Care Nurse 2017, 37, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kandelman, N.; Mazars, T.; Levy, A. Risk factors for burnout among caregivers working in nursing homes. J. Clin. Nurs. 2018, 27, E147–E153. [Google Scholar] [CrossRef] [PubMed]
- Masiero, M.; Cutica, I.; Russo, S.; Mazzocco, K.; Pravettoni, G. Psycho-cognitive predictors of burnout in healthcare professionals working in emergency departments. J. Clin. Nurs. 2018, 27, 2691–2698. [Google Scholar] [CrossRef]
- Vargas, C.; Cañadas-De la Fuente, G.A.; Aguayo, R.; Fernández-Castillo, R.; De la Fuente, E.I. Which occupational risk factors are associated with burnout in nursing? A meta-analytic study. Int. J. Clin. Health Psychol. 2014, 14, 28–38. [Google Scholar] [CrossRef]
- Arrogante, O.; Aparicio, E. Burnout and health among critical care professionals: The meditational role of resilience. Intensive Crit. Care Nurs. 2017, 42, 110–115. [Google Scholar] [CrossRef]
- Martínez, M.C.; Oliveira Latorre, M.R.D.; Fischer, F.M. A cohort study of psychosocial work stressors on work ability among Brazilian hospital workers. Am. J. Ind. Med. 2015, 58, 796–806. [Google Scholar] [CrossRef]
- Galleta, M.; Portoghese, I.; D´Aloja, E.; Mereu, A.; Contu, P.; Coppola, R.C.; Campagna, M. Relationship between job burnout, psychosocial factors and health care-associated infections in critical care units. Intensive Crit. Care Nurs. 2016, 34, 51–58. [Google Scholar] [CrossRef]
- Organización Mundial de la Salud. La organización del trabajo y el estrés. Ginebra, Suiza. 2019. Available online: https://www.who.int/occupational_health/publications/stress/es/ (accessed on 28 August 2020).
- Demerouti, E.; Bakker, A.B.; Nachreiner, F.; Schaufeli, B.W. A model of Burnout and life satisfaction amongst nurse. J. Adv. Nurs. 2000, 32, 454–464. [Google Scholar] [CrossRef]
- Cañadas-De la Fuente, G.A.; Vargas, C.; San Luis, C.; García, I.; Cañadas, G.R.; De la Fuente, E.I. Risk factors and prevalence of burnout syndrome in the nursing profession. Int. J. Nurs. Stud. 2015, 52, 240–249. [Google Scholar] [CrossRef] [PubMed]
- Albendín, L.; Gómez, J.L.; Cañadas-de la Fuente, G.A.; Cañadas, G.R.; San Luis, C.; Aguayo, R. Bayesian prevalence and burnout levels in emergency nurses. A Syst. Rev. Rev. Latinom. Psicol. 2016, 48, 137–145. [Google Scholar] [CrossRef]
- Losa Iglesias, M.E.; Becerro de Bengoa Vallejo, R. Prevalence and relationship between burnout, job satisfaction, stress, and clinical manifestations in Spanish critical care nurses. Dimens. Crit. Care Nurs. 2013, 32, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Ortega-Campos, E.; Cañadas-De la Fuente, G.A.; Albendín-García, L.; Gómez-Urquiza, J.L.; Monsalve-Reyes, C.; de la Fuente-Solana, E.I. A multicentre study of psychological variables and the prevalence of burnout among primary health care nurses. Int. J. Environ. Res. Public Health 2019, 16, 3242. [Google Scholar] [CrossRef] [PubMed]
- López-López, I.M.; Gómez-Urquiza, J.L.; Cañadas, G.R.; De la Fuente, E.I.; Albendín-García, L.; Cañadas-De la Fuente, G.A. Prevalence of burnout in mental health nurses and related factors: A systematic review and meta-analysis. Int. J. Ment. Health Nurs. 2019, 28, 1032–1041. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Baena, L.; Ortega-Campos, E.; Gómez-Urquiza, J.L.; Cañadas-De la Fuente, G.R.; De la Fuente-Solana, E.I.; Cañadas-De la Fuente, G.A. A multicentre study of burnout prevalence and related psychological variables in medical area hospital nurses. J. Clin. Med. 2019, 8, 92. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Urquiza, J.L.; Aneas-López, A.B.; Fuente-Solana, E.I.; Albendín-García, L.; Díaz-Rodríguez, L.; Cañadas-De la Fuente, G.A. Prevalence, risk factors, and levels of burnout among oncology nurses: A systematic review. Oncol. Nurs. Forum. 2016, 43, E104–E120. [Google Scholar] [CrossRef]
- Chinomso, U.; Foluso, O. Potential stressors in cancer care: Perceptions of oncology nurses in selected teaching hospitals in Southwest Nigeria. Afr. J. Med. Health Sci. 2015, 14, 130–134. [Google Scholar] [CrossRef]
- Pearson, H.N. “You’ve only got one chance to get it right”: Children’s cancer nurses’ experiences of providing palliative care in the acute hospital setting. Issues Compr. Pediatr. Nurs. 2013, 36, 188–211. [Google Scholar] [CrossRef]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron CMoher, D. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef]
- Centre for Evidence-Based Medicine. Oxford: CEBM. 2009. Available online: https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels-evidence (accessed on 10 March 2018).
- Vega, P.; González-Rodríguez, R.; Santibáñez-Galdámez, N.; Ferrada-Molina, C.; Spicto-Orellana, J.; Sateler-Villanueva, A.; Bustos-Melo, J. Supporting in grief and burnout of the nursing team from pediatric units in Chilean hospitals. Rev. Esc. Enferm. USP. 2015, 51, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J. Perceived social support and burnout among nurses working with chronically and dying pediatric patients. Sr. Res. Proj. 1992, 142, 1–36. [Google Scholar]
- Edmonds, C.; Lockwood, G.; Bezjak, A.; Nyhof-Young, J. Alleviating emotional exhaustion in oncology nurses: An evaluation of Wellspring’s “Care for the professional caregiver program”. J. Cancer Educ. 2012, 27, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, R.; Gormley, D.K. Perceptions of stress, burnout, and support systems in pediatric bone marrow transplantation nursing. Clin. J. Oncol. Nurs. 2009, 13, 681–685. [Google Scholar] [CrossRef]
- Zanatta, A.B.; Luca, S.R. Prevalence of burnout syndrome in health professionals of an onco-hematological pediatric hospital. Rev. Esc. Enferm. USP 2015, 49, 253–260. [Google Scholar] [CrossRef]
- Italia, S.; Favara-Scacco, C.; Di Cataldo, A.; Russo, G. Evaluation and art therapy treatment of the burnout syndrome in oncology units. Psycho-Oncology 2008, 17, 676–680. [Google Scholar] [CrossRef]
- Liakopoulou, M.; Panaretaki, I.; Papadakis, V.; Katsika, A.; Sarafidou, J.; Laskari, H.; Haidas, S. Burnout, staff support, and coping in pediatric oncology. Support. Care Cancer 2008, 16, 143–150. [Google Scholar] [CrossRef]
- Reyes-Marrero, D.; Camejo-Díaz, J.G.; Coro-Carrasco, Z. Síndrome de burnout en servicio de oncohematología pediátrica. Rev. Cienc. Médicas 2017, 21, 538–544. [Google Scholar]
- Colville, G.A.; Smith, J.G.; Brierley, J.; Citron, K.; Nguru, N.; Shaunak, P.D.; Perkins-Porras, L. Coping with staff burnout and work-related posttraumatic stress in intensive care. Pediatr. Crit. Care Med. 2017, 18, 267–273. [Google Scholar] [CrossRef]
- Tuna, R.; Baykal, U. The relationship between job stress and burnout levels of oncology nurses. Asia Pac. J. Oncol. Nurs. 2014, 1, 33–39. [Google Scholar] [CrossRef]
- Neumann, J.L.; Mau, L.W.; Virani, S.; Denzen, E.M.; Boyle, D.A.; Boyle, N.J.; Burns, L.J. Burnout, moral distress, work–life balance, and career satisfaction among hematopoietic cell transplantation professionals. Biol. Blood Marrow Transplant. 2018, 24, 849–860. [Google Scholar] [CrossRef] [PubMed]
- Kash, K.M.; Holland, J.C.; Breitbart, W.; Berenson, S.; Dougherty, J.; Ouellette-Kobasa, S.; Lesko, L. Stress and burnout in oncology. Oncology 2000, 14, 1621–1633. [Google Scholar] [PubMed]
- Corsino, L.; Gomes, A.C.; Lavynnya, E.; Goncalves, A.K. Burnout syndrome in health-care professionals in a university hospital. Clinics 2017, 72, 305–309. [Google Scholar] [CrossRef]
- Hu, H.X.; Liu, L.T.; Zhao, F.J.; Yao, Y.Y.; Gao, Y.X.; Wang, G.R. Factors related to job burnout among community nurses in Changchun, China. J. Nurs. Res. 2015, 23, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, L.; Lukasse, M. Burnout among Norwegian midwives and the contribution of personal and work-related factors: A cross-sectional study. Sex. Reprod. Healthc. 2016, 9, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Ferri, P.; Guerra, E.; Marcheselli, L.; Cunico, L.; Di Lorenzo, R. Empathy and burnout: An analytic cross-sectional study among nurses and nursing students. Acta Biomed. 2015, 86, 104–115. [Google Scholar]
- Mollart, L.; Skinner, V.M.; Newing, C.; Foureur, M. Factors that may influence midwives’ work-related stress and burnout. Women Birth. 2013, 26, 26–32. [Google Scholar] [CrossRef]
- Taleghani, F.; Ashouri, E.; Saburi, M. Empathy, burnout, demographic variables and their relationships in oncology nurses. Iran. J. Nurs. Midwifery Res. 2017, 22, 41–45. [Google Scholar] [CrossRef]
- Adwan, J.Z. Pediatric nurses’ grief experience, burnout and job satisfaction. J. Pediatr. Nurs. 2014, 29, 329–336. [Google Scholar] [CrossRef]
- Knopp-Sihota, J.A.; Niehaus, L.; Squires, J.E.; Norton, P.G.; Estabrooks, C.A. Factors associated with rushed and missed resident care in western Canadian nursing homes: A cross-sectional survey of health care aides. J. Clin. Nurs. 2015, 24, 2815–2825. [Google Scholar] [CrossRef]
- Cañadas-De la Fuente, G.A.; Albendín-García, L.; De la Fuente, E.I.; San Luis, C.; Gómez-Urquiza, J.L.; Cañadas, G.R. Síndrome de burnout en profesionales de enfermería que realizan jornada física complementaria en servicios de cuidados críticos y urgencias. Rev. Esp. Salud Pública. 2016, 90, 1–9. [Google Scholar]
- Wang, P.H.; Ku, Y.C.; Chen, C.C.; Jeang, S.R.; Chou, F.H. Work-related frustration among senior nurses at a medical centre. J. Clin. Nurs. 2016, 25, 2040–2051. [Google Scholar] [CrossRef]
- Woodhead, E.L.; Northrop, L.; Edelstein, B. Stress, social support, and burnout among long-term care nursing staff. J. Appl. Gerontol. 2016, 35, 84–105. [Google Scholar] [CrossRef] [PubMed]
- Gulliver, P.; Towell, D.; Peck, E. Staff morale in the merger of mental health and social care organizations in England. J. Psychiatr. Ment. Health Nurs. 2003, 10, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Freimann, T.; Merisalu, E. Work-related psychosocial risk factors and mental health problems amongst nurses at a university hospital in Estonia: A cross-sectional study. Scand. J. Public Health. 2015, 43, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Pradas-Hernández, L.; Ariza, T.; Gómez-Urquiza, J.L.; Albendín-García, L.; De la Fuente, E.I.; Cañadas-De la Fuente, G.A. Prevalence of burnout in paediatric nurses: A systematic review and meta-analysis. PLoS ONE 2018, 13, E0195039. [Google Scholar] [CrossRef]
- Vidotti, V.; Ribeiro, R.P.; Galdino, M.J.Q.; Martins, J.T. Burnout syndrome and shift work among the nursing staff. Rev. Latino-Am. Enfermagem. 2018, 26, E3022. [Google Scholar] [CrossRef]
- Zencirci, A.D.; Arslan, S. Morning-evening type and burnout level as factors influencing sleep quality of shift nurses: A questionnaire study. Croat. Med. J. 2011, 52, 527–537. [Google Scholar] [CrossRef]
- Kousloglou, S.A.; Mouzas, O.D.; Bonotis, K.; Roupa, Z.; Vasilopoulos, A.; Angelopoulos, N.V. Insomnia and burnout in Greek nurses. Hippokratia 2014, 18, 150–155. [Google Scholar]
- Cañadas-De la Fuente, G.A.; Gómez-Urquiza, J.L.; Ortega-Campos, E.M.; Cañadas, G.R.; Albendín-García, L.; De la Fuente-Solana, E.I. Prevalence of burnout syndrome in oncology nursing: A meta-analytic study. Psycho-oncology 2018, 27, 1426–1433. [Google Scholar] [CrossRef]
- Papathanasiou, I.V.; Tsaras, K.; Kleisiaris, C.F.; Fradelos, E.C.; Tsaloglidou, A.; Damigos, D. Anxiety and depression in staff of mental units: The role of burnout. Adv. Exp. Med. Biol. 2017, 987, 185–197. [Google Scholar] [CrossRef] [PubMed]
- Trifiletti, E.; Pedrazza, M.; Berlanda, S.; Pyszczynski, T. Burnout disrupts anxiety buffer functioning among nurses: A three-way interaction model. Front. Psychol. 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Giorgi, F.; Mattei, A.; Notarnicola, I.; Petrucci, C.; Lancia, L. Can sleep quality and burnout affect the job performance of shift-work nurses? A hospital cross-sectional study. J. Adv. Nurs. 2018, 74, 698–708. [Google Scholar] [CrossRef] [PubMed]
- Alexander, G.K.; Rollins, K.; Walker, D.; Wong, L.; Pennings, J. Yoga for self-care and burnout prevention among nurses. Workplace Health Saf. 2015, 63, 462–470. [Google Scholar] [CrossRef] [PubMed]
- Dyrbye, L.N.; Shanafelt, T.D.; Johnson, P.O.; Johnson, L.A.; Satele, D.; West, C.P. A cross-sectional study exploring the relationship between burnout, absenteeism, and job performance among American nurses. BMC Nurs. 2019, 18, 57. [Google Scholar] [CrossRef] [PubMed]
- Velando-Soriano, A.; Ortega-Campos, E.; Gómez-Urquiza, J.L.; Ramírez-Baena, L.; De La Fuente, E.I.; Cañadas-De La Fuente, G.A. Impact of social support in preventing burnout syndrome in nurses: A systematic review. Jpn. J. Nurs. Sci. 2020, 17, e12269. [Google Scholar] [CrossRef] [PubMed]
- Mefoh, P.C.; Ude, E.N.; Chukwuorji, J.C. Age and burnout syndrome in nursing professionals: Moderating role of emotion-focused coping. Psychol. Health Med. 2019, 24, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Burger, K.G.; Lockhart, J.S. Meditation’s effect on attentional efficiency, stress, and mindfulness characteristics of nursing students. J. Nurs. Educ. 2017, 56, 430–434. [Google Scholar] [CrossRef] [PubMed]
- Duarte, J.; Pinto-Gouveia, J. Effectiveness of a mindfulness-based intervention on oncology nurses’ burnout and compassion fatigue symptoms: A non-randomized study. Int. J. Nurs. Stud. 2016, 64, 98–107. [Google Scholar] [CrossRef]
- Zadeh, S.; Gamba, N.; Hudson, C.; Wiener, L. Taking care of care providers: A wellness program for pediatric nurses. J. Pediatr. Oncol. Nurs. 2012, 29, 294–299. [Google Scholar] [CrossRef]
- Wei, R.; Ji, H.; Li, J.; Zhang, L. Active intervention can decrease burnout in ED nurses. J. Emerg. Nurs. 2017, 43, 145–149. [Google Scholar] [CrossRef] [PubMed]
- Hersch, R.K.; Cook, R.F.; Deitz, D.K.; Kaplan, S.; Hughes, D.; Friesen, M.A.; Vezina, M. Reducing nurses’ stress: A randomized controlled trial of a web-based stress management program for nurses. Appl. Nurs. Res. 2016, 32, 18–25. [Google Scholar] [CrossRef] [PubMed]

| Author, Year. Country | Sample n | % of High EE | % of High D | % of Low PA |
|---|---|---|---|---|
| [36] | 88 | 34.1% | 25% | 30.7% |
| [37] | 30 | 26.7% | 3.3% | 16.7% |
| [35] | 14 | 57.1% | 21.4% | 28.5% |
| [41] | 11 | - | - | 13.3% |
| [34] | 153 | 48.8% | 16% | 41% |
| [38] | 65 | 24.6% | 29.8% | 22.8% |
| Author, Year | EE (%) | D (%) | PA (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| High | Medium | Low | High | Medium | Low | High | Medium | Low | |
| [37] | 26.7 | 46.7 | 26.7 | 3.3 | 33.3 | 63.3 | 50 | 33.3 | 16.7 |
| [38] | 24.6 | 49.1 | 26.3 | 29.8 | 43.9 | 26.3 | 24.6 | 52.6 | 22.8 |
| Author, Year, Country | Study Type | OCEBM | n | Version of MBI | Mean EE | Mean D | Mean PA | Risk Factors |
|---|---|---|---|---|---|---|---|---|
| [36] | Descriptive, cross-sectional | LE: 2C GR: B | 88 | MBI | 22.3 | 6.1 | 35.9 | - Younger nurses reported significantly higher rates of EE. - Work experience affects the burnout levels. Nurses with less experience present higher levels of EE. - Psychological morbidity correlates with the EE. |
| [37] | Exploratory, descriptive | LE: 2C GR: B | 30 | MBI-HSS | 26.7 | 3.3 | 16.7 | - Novice nurses have higher levels of EE and D and lower levels of PA. - The complexity and critical nature reported high levels of EE. - Support systems are associated positively with PA. - Shift work, in particular night shift work, is associated with high levels of EE and D. |
| [39] | Pilot study | LE: 2C GR: B | 16 | MBI-HSS | ND | ND | ND | - Older nurses experience high levels of burnout. |
| [35] | Descriptive, correlational | LE: 2C GR: B | 14 | MBI-HSS | 26.4 | 8.2 | 34.7 | - Overwork correlate positively with EE more than D. - Demanding role with stressed parents tends to score higher in EE. - Lack of companionship and co-worker gossip are correlated with higher level of EE than D. - Levels of frustration are related to EE levels more so than D levels. |
| [40] | Comparative and descriptive, correlational | LE: 2C GR: B | 37 | MBI-HSS | 27.5 ± 9.5 | 5.2 ± 4.9 | 37.8 ± 5.8 | - D is related to not having children. - D increases in nurses with less experience. - Decreased role clarity is positively correlated with EE and negatively with PA. |
| [41] | Descriptive, cross-sectional | LE: 2C GR: B | 11 | MBI | SD | SD | SD | - The female gender is associated with higher levels of burnout. - Burnout levels are associated with the nurses’ age. Nurses older than 40 years have an average level of burnout. - Nurses on the night shift have higher levels of burnout. - Burnout levels are related to less work experience. |
| [34] | Descriptive, cross-sectional | LE: 2C GR: B | 153 | MBI | 48.4 | 16 | 41 | - Burnout among females is significantly higher. - Older nurses (more than 40 years old) present higher levels of burnout. - Demographic variables such as marital status, age, years of experience and number of children are not related to burnout prevalence. |
| [38] | Descriptive, cross-sectional | LE: 2C GR: B | 57 | MBI | 24.6 | 29.8 | 22.8 | - Marital status is related to EE. Married nurses are more prone to EE. - Health problems are related to high levels of EE. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De la Fuente-Solana, E.I.; Pradas-Hernández, L.; Ramiro-Salmerón, A.; Suleiman-Martos, N.; Gómez-Urquiza, J.L.; Albendín-García, L.; Cañadas-De la Fuente, G.A. Burnout Syndrome in Paediatric Oncology Nurses: A Systematic Review and Meta-Analysis. Healthcare 2020, 8, 309. https://doi.org/10.3390/healthcare8030309
De la Fuente-Solana EI, Pradas-Hernández L, Ramiro-Salmerón A, Suleiman-Martos N, Gómez-Urquiza JL, Albendín-García L, Cañadas-De la Fuente GA. Burnout Syndrome in Paediatric Oncology Nurses: A Systematic Review and Meta-Analysis. Healthcare. 2020; 8(3):309. https://doi.org/10.3390/healthcare8030309
Chicago/Turabian StyleDe la Fuente-Solana, Emilia Inmaculada, Laura Pradas-Hernández, Alicia Ramiro-Salmerón, Nora Suleiman-Martos, José Luis Gómez-Urquiza, Luis Albendín-García, and Guillermo Arturo Cañadas-De la Fuente. 2020. "Burnout Syndrome in Paediatric Oncology Nurses: A Systematic Review and Meta-Analysis" Healthcare 8, no. 3: 309. https://doi.org/10.3390/healthcare8030309
APA StyleDe la Fuente-Solana, E. I., Pradas-Hernández, L., Ramiro-Salmerón, A., Suleiman-Martos, N., Gómez-Urquiza, J. L., Albendín-García, L., & Cañadas-De la Fuente, G. A. (2020). Burnout Syndrome in Paediatric Oncology Nurses: A Systematic Review and Meta-Analysis. Healthcare, 8(3), 309. https://doi.org/10.3390/healthcare8030309










