The Level of Health Literacy of Seniors Living in Eastern Region of Poland. Preliminary Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Aim
2.2. Study Participants and Setting
2.3. Research Instruments
2.4. Analysis
2.5. Ethical Aspects
3. Results
3.1. Characteristics of the Studied Group
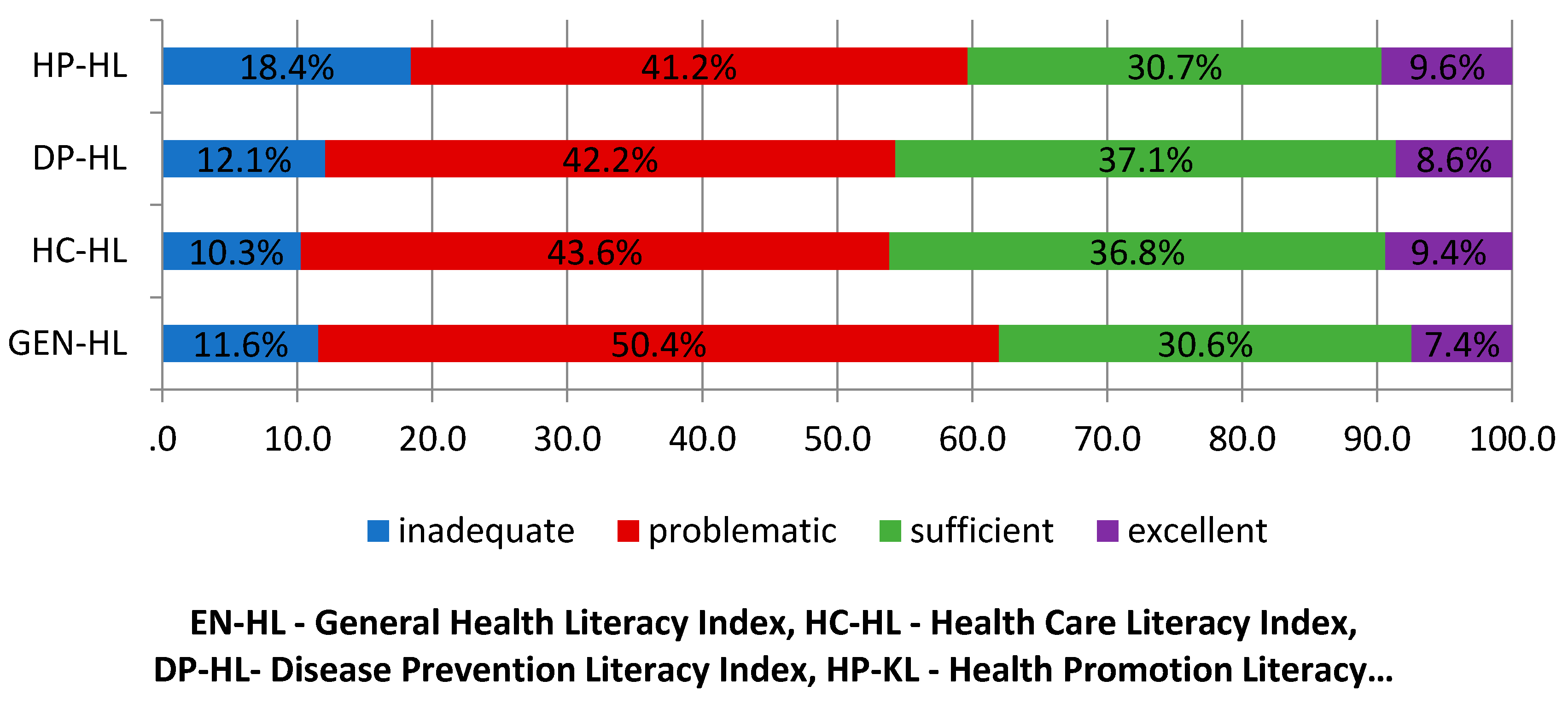
3.2. The General Level of Health Literacy Among Seniors
3.3. HLS-EU Health Literacy Indices of Seniors vs Their Sociodemographic Characteristics
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Couture, E.M.; Chouinard, M.-C.; Fortin, M.; Hudo, C. The relationship between health literacy and quality of life among frequent users of health care services: A cross-sectional study. Health Qual. Life Outcomes 2017, 15, 137. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- Nutbeam, D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef]
- Zhang, N.J.; Terry, A.; McHorney, C.A. Impact of health literacy on medication adherence: A systematic review and meta-analysis. Ann. Pharmacother. 2014, 48, 741–751. [Google Scholar] [CrossRef] [PubMed]
- Irwin, S.; Jungeblut, K.; Jenkins, L.; Kolstad, A. Adult Literacy in America a First Look at the Findings of the National Adult Literacy Survey, 3rd ed.; Department of Education Office of Educational Research and Improvement: Washington, DC, USA, 2002. [Google Scholar]
- Bonaccorsi, G.; Lorini, C.; Baldasseroni, A.; Porchia, B.R.; Capecchi, L. Health services and health literacy: From the rationale to the many facets of a fundamental concept. A literature review. Ann. Ist. Super. Sanità 2016, 52, 114–118. [Google Scholar] [PubMed]
- Palumbo, R. Designing health-literate health care organization: A literature review. Health Serv. Manag. Res. 2016, 29, 79–87. [Google Scholar] [CrossRef]
- Berkman, N.; Sheridan, S.; Donahue, K.; Halpern, D.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef]
- Ishikawa, H.; Yamaguchi, I.; Nutbeam, D.; Kato, M.; Okuhara, T.; Okada, M.; Kiuchi, T. Improving health literacy in a Japanese community population-A pilot study to develop an educational programme. Health Expect. 2018, 21, 814–821. [Google Scholar] [CrossRef]
- Çaylan, A.; Yayla, K.; Öztora, S.; Dağdeviren, H.N. Assessing health literacy, the factors affecting it and their relation to some health behaviors among adults. Biomed. Res. 2017, 28, 6803–6807. [Google Scholar]
- Baker, D.W.; Gazmararian, J.A.; Williams, M.V.; Scott, T.; Parker, R.M.; Green, D.; Ren, J.; Peel, J. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am. J. Public Health 2002, 92, 1278–1283. [Google Scholar] [CrossRef]
- Batterham, R.W.; Hawkins, M.; Collins, P.A.; Buchbinder, R.; Osborne, R.H. Health literacy: Applying current concepts to improve health services and reduce health inequalities. Public Health 2016, 132, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Morris, N.S.; Field, T.S.; Wagner, J.L.; Cutrona, S.L.; Roblin, D.W.; Gaglio, B. The association between health literacy and cancer-related attitudes, behaviors, and knowledge. J. Health Commun. 2013, 18, 223–241. [Google Scholar] [CrossRef] [PubMed]
- Muir, K.W.; Santiago-Turla, C.; Stinnett, S.S.; Herndon, L.W.; Allingham, R.R.; Challa, P.; Lee, P.P. Health literacy and adherence to glaucoma therapy. Am. J. Ophthalmol. 2006, 142, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Taggart, J.; Williams, A.; Dennis, S.; Newall, A.; Shortus, T.; Zwar, N.; Denney-Wilson, E.; Harris, M.F. A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors. BMC Fam. Pract. 2012, 13, 49. [Google Scholar] [CrossRef]
- Feinberg, I.; Tighe, E.L.; Greenberg, D.; Mavreles, M. Health Literacy and Adults with Low Basic Skills. Adult Educ. Q. 2018, 68, 297–315. [Google Scholar] [CrossRef]
- Alkhaldi, T.M.; Al-Jumaili, A.A.; Alnemer, K.A.; Alharbi, K.; Al-Akeel, E.S.; Alharbi, M.H.; Alshabanah, O.; Juwair, A.B.; Khoja, A. Measuring the health literacy level of Arabic speaking population in Saudi Arabia using translated health literacy instruments. J. Pharm. Pract. 2018, 16, 1223. [Google Scholar] [CrossRef]
- Sørensen, K.; Pelikan, J.M.; Rothlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. HLS-EU Consortium. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef]
- Nakayama, K.; Osaka, W.; Togari, T.; Ishikawa, H.; Yonekura, Y.; Sekido, A.; Matsumoto, M. Comprehensive health literacy in Japan is lower than in Europe: A validated Japanese- language assessment of health literacy. BMC Public Health 2015, 15, 505. [Google Scholar] [CrossRef]
- Van der Heide, I.; Uiters, E.; Sørensen, K.; Rothlin, F.; Pelikan, J.; Rademakers, J.; Boshuizen, H. Health literacy in Europe: The development and validation of health literacy prediction models. Eur. J. Public Health 2016, 26, 906–991. [Google Scholar] [CrossRef]
- Manafo, E.; Wong, S. Health literacy programs for older adults: A systematic literature review. Health Educ. Res. 2012, 27, 947–960. [Google Scholar] [CrossRef]
- Geboers, B.; de Winter, A.F.; Spoorenberg, S.L.W.; Wynia, K.; Reijneveld, S.A. The association between health literacy and self-management abilities in adults aged 75 and older, and its moderators. Qual. Life Res. 2016, 25, 2869–2877. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M.; Jin, H.; Shi, N.; Duan, C.; Wang, D.; Yu, X.; Li, X. The relationship between health literacy and quality of life: A systematic review and meta-analysis. Health Qual. Life Outcomes 2018, 16, 201. [Google Scholar] [CrossRef] [PubMed]
- Storms, H.; Claes, N.; Aertgeerts, B.; Van den Broucke, S. Measuring health literacy among low literate people: An exploratory feasibility study with the HLS-EU questionnaire. BMC Public Health 2017, 17, 475. [Google Scholar] [CrossRef] [PubMed]
- Safeer, R.S.; Keenan, J. Health literacy: The gap between physicians and patients. Am. Fam. Physician 2005, 72, 463–468. [Google Scholar] [PubMed]
- Kutner, M.; Greenberg, E.; Jin, Y.; Paulsen, C. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy; United States Department of Education; National Center for Education Statistics: Washington, DC, USA, 2006. Available online: https://nces.ed.gov/pubs2006/2006483.pdf (accessed on 4 July 2020).
- Javadzade, S.; Sharifirad, G.; Radjati, F.; Mostafavi, F.; Reisi, M.; Hasanzade, A. Relationship between health literacy, health status, and healthy behaviors among older adults in Isfahan, Iran. Educ. Health Promot. 2012, 1, 31. [Google Scholar]
- European Commission Directorate-General for Economic and Financial Affairs. The 2015 Ageing Report Underlying Assumptions and Projection Methodologies. Available online: https://ec.europa.eu/economy_finance/publications/european_economy/2014/pdf/ee8_en.pdf (accessed on 4 July 2020).
- Serper, M.; Patzer, R.E.; Curtis, L.M.; Smith, S.G.; O’Conor, R.; Baker, D.W.; Wolf, M.S. Health literacy, cognitive ability, and functional health status among older adults. Health Serv. Res. 2014, 49, 1249–1267. [Google Scholar] [CrossRef]
- Cutilli, C.C. Health literacy in geriatric patients: An integrative review of the literature. Orthop. Nurs. 2007, 26, 43–48. [Google Scholar] [CrossRef]
- Kobayashi, L.C.; Wardle, J.; Wolf, M.S.; von Wagner, C. Cognitive function and health literacy decline in a cohort of aging English adults. J. Gen. Intern. Med. 2015, 30, 958–964. [Google Scholar] [CrossRef]
- Słońska, Z.A.; Borowiec, A.A.; Aranowska, A.E. Health literacy and health among the elderly: Status and challenges in the context of the Polish population aging process. Anthropol. Rev. 2015, 78, 297–307. [Google Scholar] [CrossRef]
- Duplaga, M. Determinants and consequences of limited health literacy in Polish society. Int. J. Environ. Res. Public Health 2020, 17, 642. [Google Scholar] [CrossRef]
- Statistics Poland. Sytuacja Demograficzna Osób Starszych i Konsekwencje Starzenia się Ludności Polski w Świetle proGnozy na Lata 2014–2050. In Demographic Situation of the Elderly and the Consequences of the Aging of the Polish Population in the Light of the Forecast for 2014–2050; Główny Urząd Statystyczny: Warsaw, Poland, 2014. Available online: https://stat.gov.pl/files/gfx/portalinformacyjny/pl/defaultaktualnosci/5468/18/1/1/ludnosc_w_starszym_wieku.pdf (accessed on 6 August 2020).
- Adamczyk, M. The Specificity of Ageing Processes of Population of the Lubelskie Voivodship. In Demographic Situation of Lubelskie Voivodship as a Challenge for Social and Economic Policy; Hrynkiewicz, J., Potrykowska, A., Eds.; The Government Population Council: Warsaw, Poland, 2017; pp. 101–117. [Google Scholar]
- Montreal Cognitive Assessment Test (MoCA). Available online: https://www.mocatest.org/ (accessed on 9 July 2020).
- Sørensen, K.; Van den Broucke, S.; Pelikan, J.M.; Fullam, J.; Doyle, G.; Slonska, Z.; Kondilis, B.; Stoffels, V.; Osborne, R.H.; Brand, H. Measuring health literacy in populations: Illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q). BMC Public Health 2013, 13, 948. [Google Scholar] [CrossRef] [PubMed]
- Orimo, H.; Ito, H.; Suzuki, T.; Araki, A.; Hosoi, T.; Sawabe, M. Reviewing the definition of “elderly”. Geriatr. Gerontol. Int. 2006, 6, 149–158. [Google Scholar] [CrossRef]
- Okan, O.; Lopes, E.; Bollweg, T.M.; Bröder, J.; Messer, M.; Bruland, D.; Bond, E.; Carvalho, G.S.; Sørensen, K.; Saboga-Nunes, L.; et al. Generic health literacy measurement instruments for children and adolescents: A systematic review of the literature. BMC Public Health 2018, 18, 166. [Google Scholar] [CrossRef] [PubMed]
- McDougall, G.J.; Mackert, M.; Becker, H. Memory performance, health literacy, and instrumen- tal activities of daily living of community residing older adults. Nurs. Res. 2012, 61, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Wolf, M.S.; Feinglass, J.; Thompson, J.; Baker, D.W. In search of “low health literacy”: Threshold vs. gradient effect of literacy on health status and mortality. Soc. Sci. Med. 2010, 70, 1335–1341. [Google Scholar] [CrossRef]
- Lee, E.J.; Lee, H.J.; Chung, S. Age Differencesin Health Literacy: Korean Adults Havea Higher Level of Health Literacy than Older Korean Adults? Health Soc. Work 2017, 42, 133–141. [Google Scholar] [CrossRef]
- Ganzer, C.A.; Insel, K.C.; Ritter, L.S. Associations between working memory, health literacy, and recall of the signs of stroke among older adults. J. Neurosci. Nurs. 2012, 44, 236–243. [Google Scholar] [CrossRef]
- Brooks, C.; Ballinger, C.; Nutbeam, D.; Adams, J. The importance of building trust and tailoring interactions when meeting older adults’ health literacy needs. Disabil. Rehabil. 2017, 39, 2428–2435. [Google Scholar] [CrossRef]
- Von Wagner, C.; Knight, K.; Steptoe, A.; Wardle, J. Functional health literacy and health-promoting behavior in a national sample of British adults. J. Epidemiol. Community Health 2007, 61, 1086–1090. [Google Scholar] [CrossRef]
- Liu, Y.B.; Liu, L.; Li, Y.F.; Chen, Y.L. Relationship between Health Literacy, Health-Related Behaviors and Health Status: A Survey of Elderly Chinese. Int. J. Environ. Res. Public Health 2015, 12, 9714–9725. [Google Scholar] [CrossRef]
- Cordasco, K.M.; Homeier, D.C.; Franco, I.; Wang, P.C.; Sarkisian, C.A. Health literacy screening of geriatric monolingual Spanish-speaking patients using single-item literacy screening questions and education. Health Educ. J. 2012, 71, 597–605. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.J.; Joel, S.; Rovena, G.; Pedireddy, S.; Saad, S.; Rachmale, R.; Shukla, M.; Deol, B.B.; Cardozo, L. Testing the utility of the newest vital sign (NVS) health literacy assessment tool in older African-American patients. Patient Educ. Couns. 2011, 85, 505–507. [Google Scholar] [CrossRef] [PubMed]
- Chesser, A.K.; Keene Woods, N.; Smothers, K.; Rogers, N. Health literacy and older adults: A systematic review. Gerontol. Geriatr. Med. 2016, 2, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Lynch, M.A.M.; Franklin, G.V. Health Literacy: An Intervention to Improve Health. In Strategies to Reduce Hospital Mortality in Lower and Middle Income Countries (LMICs) and Resource-Limited Settings; Mullings, J., Ed.; IntechOpen: London, UK, 2019; Available online: https://www.intechopen.com/books/strategies-to-reduce-hospital-mortality-in-lower-and-middle-income-countries-lmics-and-resource-limited-settings (accessed on 6 August 2020).
- De Walt, D.A.; Broucksou, K.A.; Hawk, V.; Brach, C.; Hink, A.; Rudd, R.; Callahan, L. Developing and testing the health literacy universal precautions toolkit. Nurs. Outlook 2011, 59, 85–94. [Google Scholar] [CrossRef]
| Demographic and Socio-economic Variables (n = 138) | n | % |
|---|---|---|
| Gender | ||
| Male | 48 | 34.8 |
| Female | 90 | 65.2 |
| Age * | ||
| Up to 74 | 85 | 61.6 |
| 75 and older | 53 | 38.4 |
| Education | ||
| Primary education | 56 | 40.6 |
| Secondary education | 59 | 42.8 |
| Tertiary education | 23 | 16.7 |
| Place of residence | ||
| Rural residents | 60 | 43.5 |
| Urban residents | 78 | 56.5 |
| Household living situation | ||
| Alone | 44 | 31.9 |
| With spouse or partner | 6 | 4.3 |
| With family | 55 | 39.9 |
| With spouse or partner and with family | 33 | 23.9 |
| Participated in activities run by Daily Center for the Elderly or other organisations/institutions | ||
| Yes | 44 | 31.9 |
| No | 94 | 68.1 |
| Self-assessment of health condition | ||
| Very good | 9 | 6.5 |
| Good | 52 | 37.7 |
| Fair | 68 | 49.3 |
| Bad | 9 | 6.5 |
| HL Indices | Descriptive Statistics | The Level of HL | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Inadequate | Problematic | Sufficient | Excellent | |||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | |
| GEN-HL | 31.70 | 6.63 | 20.35 | 3.99 | 29.73 | 2.27 | 35.76 | 2.31 | 46.10 | 2.44 |
| HC-HL | 32.82 | 6.99 | 20.33 | 3.62 | 29.92 | 1.76 | 35.54 | 2.53 | 46.13 | 1.91 |
| DP-HL | 31.83 | 7.86 | 17.71 | 5.49 | 28.96 | 2.21 | 35.52 | 2.68 | 44.26 | 2.27 |
| HP-HL | 31.02 | 7.71 | 20.05 | 4.07 | 29.36 | 1.95 | 34.78 | 2.13 | 47.10 | 2.28 |
| HL Indices | Gender | |||||||
| Male | Female | Statistic | ||||||
| M | SD | M | SD | Z | p | |||
| GEN-HL | 30.93 | 7.27 | 32.10 | 6.28 | −0.690 | 0.490 | ||
| HC-HL | 31.47 | 7.75 | 33.43 | 6.58 | −0.900 | 0.368 | ||
| DP-HL | 30.65 | 8.82 | 32.47 | 7.27 | −1.037 | 0.300 | ||
| HP-HL | 31.03 | 7.71 | 31.01 | 7.76 | −0.015 | 0.988 | ||
| Level of Education | ||||||||
| Primary Education | Secondary Education | Tertiary Education | H | p | ||||
| M | SD | M | SD | M | SD | |||
| GEN-HL | 29.66 | 5.94 | 32.45 | 7.22 | 34.34 | 5.18 | 6.211 | 0.045 |
| HC-HL | 30.44 | 6.30 | 33.10 | 6.89 | 36.90 | 6.79 | 10.183 | 0.006 |
| DP-HL | 29.32 | 7.60 | 33.30 | 8.27 | 34.11 | 5.66 | 5.319 | 0.070 |
| HP-HL | 29.30 | 6.27 | 31.32 | 8.58 | 34.47 | 7.47 | 3.935 | 0.140 |
| Rural Area | Urban Area | Z | p | |||||
| M | SD | M | SD | |||||
| GEN-HL | 29.72 | 6.11 | 33.06 | 6.66 | −2.179 | 0.029 | ||
| HC-HL | 30.69 | 6.74 | 34.20 | 6.84 | −2.257 | 0.024 | ||
| DP-HL | 29.56 | 6.97 | 33.41 | 8.11 | −2.265 | 0.024 | ||
| HP-HL | 28.54 | 6.75 | 32.89 | 7.90 | −2.653 | 0.008 | ||
| Age | ||||||||
| Up to 74 | 75 and Older | Z | p | |||||
| M | SD | M | SD | |||||
| GEN-HL | 32.17 | 6.91 | 31.04 | 6.21 | −0.679 | 0.497 | ||
| HC-HL | 33.19 | 7.36 | 32.24 | 6.42 | −0.643 | 0.521 | ||
| DP-HL | 32.30 | 7.87 | 31.12 | 7.88 | −0.242 | 0.809 | ||
| HP-HL | 31.42 | 8.26 | 30.45 | 6.89 | −1.044 | 0.296 | ||
| Participation in Activities Run by Daily Center for the Elderly or Other Organisations/Institutions | ||||||||
| Yes | No | Z | p | |||||
| M | SD | M | SD | |||||
| GEN-HL | 34.25 | 6.97 | 30.49 | 6.14 | −2.133 | 0.033 | ||
| HC-HL | 34.99 | 7.14 | 31.72 | 6.69 | −1.845 | 0.065 | ||
| DP-HL | 35.17 | 7.53 | 30.19 | 7.54 | −2.528 | 0.011 | ||
| HP-HL | 34.35 | 8.78 | 29.29 | 6.50 | −2.337 | 0.019 | ||
| Self-Assessment of Health Condition | ||||||||
| Very Good/Good | Fair/Bad | Z | p | |||||
| M | SD | M | SD | |||||
| GEN-HL | 33.17 | 7.13 | 30.70 | 6.11 | −2.327 | 0.020 | ||
| HC-HL | 34.31 | 7.47 | 31.74 | 6.46 | −2.181 | 0.029 | ||
| DP-HL | 32.28 | 8.39 | 31.49 | 7.50 | −0.947 | 0.344 | ||
| HP-HL | 33.21 | 8.23 | 29.42 | 6.94 | −2.568 | 0.010 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kosicka, B.; Deluga, A.; Bąk, J.; Chałdaś-Majdańska, J.; Bieniak, M.; Machul, M.; Chrzan-Rodak, A.; Jurek, K.; Dobrowolska, B. The Level of Health Literacy of Seniors Living in Eastern Region of Poland. Preliminary Study. Healthcare 2020, 8, 277. https://doi.org/10.3390/healthcare8030277
Kosicka B, Deluga A, Bąk J, Chałdaś-Majdańska J, Bieniak M, Machul M, Chrzan-Rodak A, Jurek K, Dobrowolska B. The Level of Health Literacy of Seniors Living in Eastern Region of Poland. Preliminary Study. Healthcare. 2020; 8(3):277. https://doi.org/10.3390/healthcare8030277
Chicago/Turabian StyleKosicka, Bogumiła, Alina Deluga, Jadwiga Bąk, Justyna Chałdaś-Majdańska, Monika Bieniak, Michał Machul, Agnieszka Chrzan-Rodak, Krzysztof Jurek, and Beata Dobrowolska. 2020. "The Level of Health Literacy of Seniors Living in Eastern Region of Poland. Preliminary Study" Healthcare 8, no. 3: 277. https://doi.org/10.3390/healthcare8030277
APA StyleKosicka, B., Deluga, A., Bąk, J., Chałdaś-Majdańska, J., Bieniak, M., Machul, M., Chrzan-Rodak, A., Jurek, K., & Dobrowolska, B. (2020). The Level of Health Literacy of Seniors Living in Eastern Region of Poland. Preliminary Study. Healthcare, 8(3), 277. https://doi.org/10.3390/healthcare8030277






