Study of the Effects of Recognition of Stress on Symptoms and Regular Hospital Visits: An Analysis from Japanese National Statistics
Abstract
1. Introduction
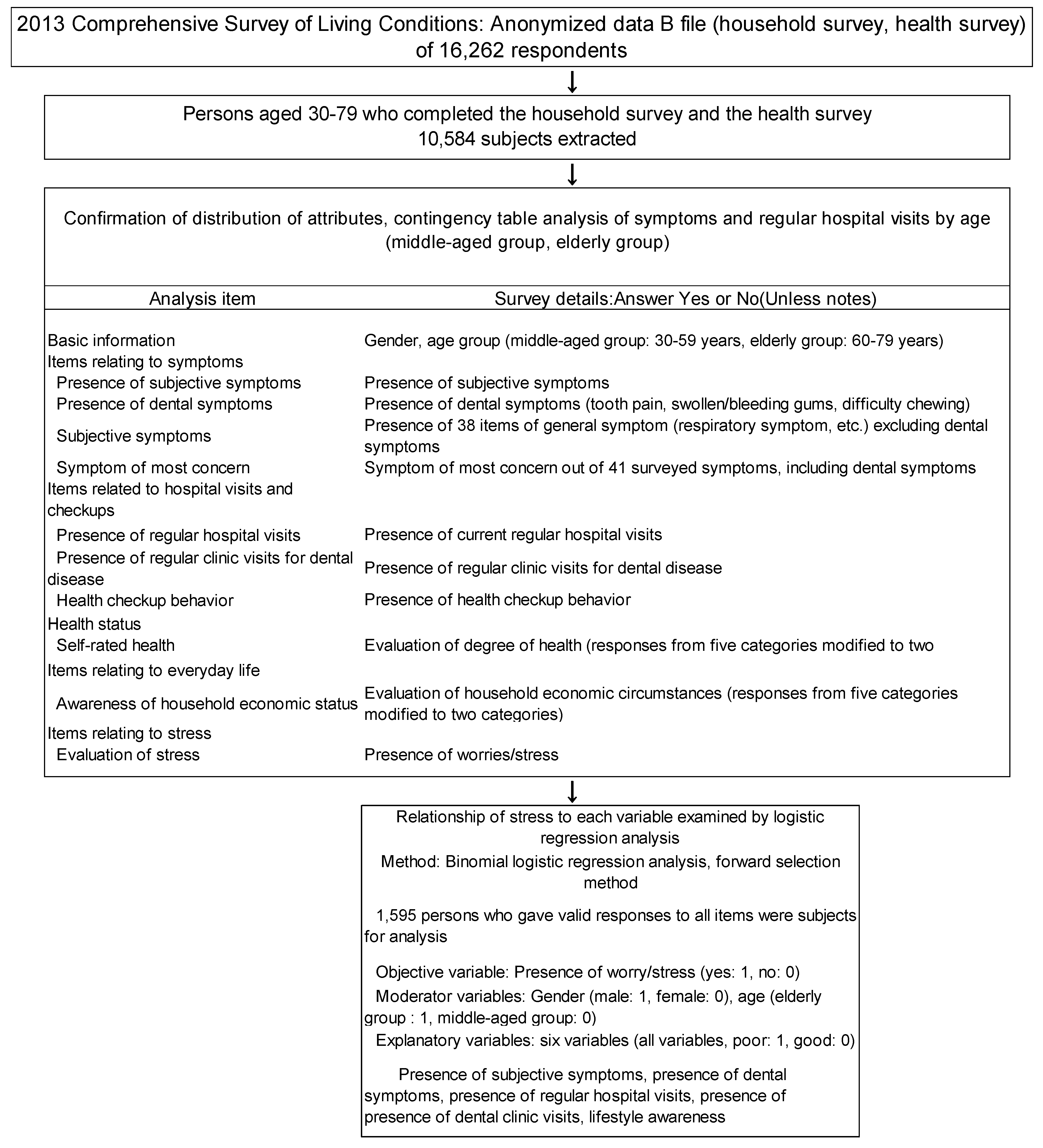
2. Materials and Methods
2.1. Study Population
2.2. Study Design
2.3. Statistical Analysis
2.4. Ethical Considerations
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- McEwen, B.S. Neurobiological and systemic effects of chronic stress. Chronic Stress (Thousand Oaks) 2017, 1, 1–18. [Google Scholar]
- Imamura, K.; Asai, Y.; Watanabe, K. Effect of the National Stress Check Program on mental health among workers in Japan: A 1-year retrospective cohort study. J. Occup. Health 2018, 25, 293–306. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, N.; Tsutsumi, A. The Stress Check Program: A new national policy for monitoring and screening psychosocial stress in the workplace in Japan. J. Occup. Health 2016, 58, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Larson, P.J.; Carrieri-Kohlman, V.; Dodd, M.J.; Douglas, M.; Faucett, J.; Froelicher, E.; Gortner, S.; Halliburton, P.; Janson, S.; Lee, K.A. A model for symptom management. Image J. Nurs. Scholarsh. 1994, 26, 272–276. [Google Scholar]
- McEwen, B.S.; Stellar, E. Stress and the individual. Mechanisms leading to disease. Arch. Int. Med. 1993, 27, 2093–2101. [Google Scholar] [CrossRef]
- Turcu-Stiolica, A.; Subtirelu, M.-S.; Ciurea, P.L.; Cristian, D.S.; Bogdan, M.; Barbulescu, A.L.; Glavan, D.-G.; Turcu-Stiolica, R.-A.; Firulescu, S.C.; Chisalau, B.A.; et al. The Influence of Socio-Demographic Factors, Lifestyle and Psychiatric Indicators on Adherence to Treatment of Patients with Rheumatoid Arthritis: A Cross-Sectional Study. Medicina 2020, 56, 178. [Google Scholar] [CrossRef]
- Ilacqua, A.; Izzo, G.; Emerenziani, G.P.; Baldari, C.; Aversa, A. Lifestyle and fertility: The influence of stress and quality of life on male fertility. Reprod. Biol. Endocrinol. 2018, 16, 116. [Google Scholar] [CrossRef]
- International Labour Office. Stress Prevention at Work Checkpoints; International Labour Office: Geneva, Switzerland, 2012. [Google Scholar]
- World Health Organization. Raising Awareness of Psychological Harassment at Work; Protecting Workers Series No 4; World Health organization: Milano, Italy, 2003. [Google Scholar]
- Zorigt, G.; Enkh-Amgalan, N.; Yu, T. Use of best-worst scaling to estimate the magnitude of stressful life events in older adults. Psychogeriatrics 2019, 19, 212–218. [Google Scholar] [CrossRef]
- Kolappa, K.; Henderson, D.C.; Kishore, S.P. No physical health without mental health: Lessons unlearned? World Health Organ. 2013, 91, 3–3A. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare. Annual Health, Labour and Welfare Report 2018; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2018. [Google Scholar]
- Ministry of Health, Labour and Welfare. A Basic Direction for Comprehensive Implementation of National Health Promotion; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2012. [Google Scholar]
- Puschmann, A.K.; Drießlein, D.; Beck, H.; Arampatzis, A.; Catalá, M.M.; Schiltenwolf, M.; Mayer, F.; Wippert, P.-M. Stress and Self-Efficacy as Long-Term Predictors for Chronic Low Back Pain: A Prospective Longitudinal Study. J. Pain Res. 2020, 13, 613–621. [Google Scholar] [CrossRef]
- Theorell, T. A long-term perspective on cardiovascular job stress research. J. Occup. Health 2019, 6, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Dolcini-Catania, L.G.; Byrne, M.L.; Whittle, S.; Schwartz, O.; Simmons, J.G.; Allen, N.B. Temperament and Symptom Pathways to the Development of Adolescent Depression. J. Abnorm. Child Psychol. 2020, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Parwani, R.; Parwani, S.R. Does stress predispose to periodontal disease? Dent. Update 2014, 41, 260–264, 268, 271–272. [Google Scholar] [CrossRef] [PubMed]
- Ohrbach, R.; Michelotti, A. The Role of Stress in the Etiology of Oral Parafunction and Myofascial Pain. Oral. Maxillofac. Surg. Clin. N. Am. 2018, 30, 369–379. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. ICD-11 for Mortality and Morbidity Statistics. Disorders Specifically Associated with Stress. 2018. Available online: http://id.who.int/icd/entity/991786158 (accessed on 27 April 2020).
- Weathers, F.W. Redefining posttraumatic stress disorder for DSM-5. Curr. Opin. Psychol. 2017, 14, 122–126. [Google Scholar] [CrossRef]
- Abdallah, C.G.; Geha, P. Chronic Pain and Chronic Stress: Two Slides of the Same Coin? Chronic Stress 2017. [Google Scholar] [CrossRef]
- Iwasaki, M.; Sato, M.; Minagawa, K.; Manz, M.C.; Yoshihara, A.; Miyazaki, H. Longitudinal relationship between metabolic syndrome and periodontal disease among Japanese adults aged ≥70 years: The Niigata Study. J. Periodontol. 2015, 86, 491–498. [Google Scholar] [CrossRef]
- Kondo, N.; Kawachi, I.; Hirai, H.; Kondo, K.; Subramanian, S.V.; Hanibuchi, T.; Yamagata, Z. Relative deprivation and incident function disability among older Japanese women and man: Prospective cohort study. J. Epidemiol. Community Health 2009, 63, 461–467. [Google Scholar] [CrossRef]
- Oates, G.R.; Juarez, L.D.; Hansen, B.; Kiefe, C.I.; Shikany, J.M. Social Risk Factors for Medication Nonadherence: Findings from the CARDIA Study. Am. J. Health Behav. 2020, 44, 232–243. [Google Scholar] [CrossRef]
- Klein, E.M.; Brähler, E.; Dreier, M. The German version of the Perceived Stress Scale-psychometric characteristics in a representative German community sample. BMC Psychiatry 2016, 16, 159. [Google Scholar] [CrossRef]
- Kalmbach, D.A.; Abelson, J.L.; Arnedt, J.T.; Zhao, Z.; Schubert, J.R.; Sen, S. Insomnia symptoms and short sleep predict anxiety and worry in response to stress exposure: A prospective cohort study of medical interns. Sleep Med. 2019, 55, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Zamkah, A.; Hui, T.; Andrews, S.; Dey, N.; Shi, F.; Sherratt, R.S. Identification of Suitable Biomarkers for Stress and Emotion Detection for Future Personal Affective Wearable Sensors. Biosensors 2020, 10, 40. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, S.; Li, Y.S.; Kawasaki, Y.; Kawai, K. Workers’ Lifestyles and Urinary 8-hydroxydeoxyguanosine as an Oxidative Stress Marker. J. UOEH 2019, 41, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Fueda, Y.; Matsuda, F.; Kataoka, T. Assessment of noninvasive positive pressure ventilation in healthy young volunteers using salivary stress biomarkers. Future Sci. OA 2020, 6, 1–9. [Google Scholar] [CrossRef] [PubMed]
| Gender | Age Group | |||||
|---|---|---|---|---|---|---|
| Middle-Aged (30–59 Years) | Elderly (60–79 Years) | Total | ||||
| Male | 2925 | (48.2) | 2167 | (48.0) | 5092 | (48.1) |
| Female | 3143 | (51.8) | 2349 | (52.0) | 5492 | (51.9) |
| Total | 6068 | (100.0) | 4516 | (100.0) | 10,584 | (100.0) |
| Attributes | Middle-Aged Group | (%) | Elderly Group | (%) | Total | (%) | p Value (χ2 Test) |
|---|---|---|---|---|---|---|---|
| Presence of worries/stress | |||||||
| Yes | 3286 | 54.2 | 1829 | 40.5 | 5115 | 48.3 | <0.001 |
| No | 2782 | 45.8 | 2687 | 59.5 | 5469 | 51.7 | |
| Presence of subjective symptoms | |||||||
| Yes | 1758 | 29.0 | 1895 | 42.0 | 3653 | 34.5 | <0.001 |
| No | 4310 | 71.0 | 2621 | 58.0 | 6931 | 65.5 | |
| Symptoms: tooth pain a | |||||||
| Yes | 114 | 6.5 | 97 | 5.1 | 211 | 5.8 | 0.077 |
| No | 1644 | 93.5 | 1798 | 94.9 | 3442 | 94.2 | |
| Symptoms: swollen/bleeding gums a | |||||||
| Yes | 104 | 5.9 | 140 | 7.4 | 244 | 6.7 | 0.075 |
| No | 1654 | 94.1 | 1755 | 92.6 | 3409 | 93.3 | |
| Symptoms: difficulty chewing a | |||||||
| Yes | 51 | 2.9 | 154 | 8.1 | 205 | 5.6 | <0.001 |
| No | 1707 | 97.1 | 1741 | 91.9 | 3448 | 94.4 | |
| Presence of regular hospital visits | |||||||
| Yes | 1844 | 30.4 | 2991 | 66.2 | 4835 | 45.7 | <0.001 |
| No | 4219 | 69.5 | 1523 | 33.7 | 5742 | 54.3 | |
| Presence of regular dental clinic visits b | |||||||
| Yes | 278 | 15.1 | 324 | 10.8 | 602 | 12.5 | <0.001 |
| No | 1566 | 84.9 | 2667 | 89.2 | 4233 | 87.5 | |
| Self-rated health | |||||||
| Poor | 648 | 10.7 | 820 | 18.2 | 1468 | 13.9 | <0.001 |
| Regular/good | 5420 | 89.3 | 3696 | 81.8 | 9116 | 86.1 | |
| Smoking | |||||||
| Yes | 1672 | 27.6 | 698 | 15.5 | 2370 | 22.4 | <0.001 |
| No | 4396 | 72.4 | 3818 | 84.5 | 8214 | 77.6 | |
| Drinking alcohol | |||||||
| Yes | 2005 | 33.0 | 1450 | 32.1 | 3455 | 32.6 | 0.311 |
| No | 4063 | 67.0 | 3066 | 67.9 | 7129 | 67.4 | |
| Health checkup behavior | |||||||
| No checkups | 1851 | 30.5 | 1633 | 36.2 | 3484 | 32.9 | <0.001 |
| Checkups | 4217 | 69.5 | 2883 | 63.8 | 7100 | 67.1 | |
| Lifestyle awareness | |||||||
| Harsh | 3830 | 63.1 | 2683 | 59.4 | 6513 | 61.5 | <0.001 |
| Regular/comfortable | 2238 | 36.9 | 1833 | 40.6 | 4071 | 38.5 | |
| Total | 6068 | (100.0) | 4516 | (100.0) | 10,584 | (100.0) |
| Stress Group | 1st | 2nd | 3rd | 4th | 5th | 6th | 7th | 8th | 9th | 10th |
| No worries/stress group | Lower back pain | Stiff shoulders | Joint pain in hands and feet | Cough/phlegm | Blocked nose/nasal discharge | Numbness of limbs | Itchy eyes | Tinnitus | Frequent urination | Difficulty hearing |
| Number (%) | 405 (7.4) | 309 (5.7) | 213 (3.9) | 141 (2.6) | 131 (2.4) | 122 (2.2) | 121 (2.2) | 108 (2.0) | 107 (2.0) | 106 (1.9) |
| 1st | 2nd | 3rd | 4th | 5th | 6th | 7th | 8th | 9th | 10th | |
| Worries/stress group | Lower back pain | Stiff shoulders | Feeling listless | Joint pain in hands and feet | Blurred vision | Headache | Cough/phlegm | Numbness of limbs | Itching | Blocked nose/ nasal discharge |
| Number (%) | 983 (19.2) | 934 (18.3) | 499 (9.8) | 479 (9.4) | 406 (7.9) | 368 (7.2) | 363 (7.1) | 354 (6.9) | 338 (6.6) | 336 (6.6) |
| Stress Group | 1st | 2nd | 3rd | 4th | 5th | 6th | 7th | 8th | 9th | 10th |
| No worries/stress group | High blood pressure | Dyslipidemia | Diabetes | Eye disease | Dental disease | Lumbago | Stiff shoulders | Gastroduodenal disease | Angina/cardiac infarction | Prostatic hyperplasia |
| Number (%) | 834 (15.3) | 335 (6.1) | 325 (5.9) | 281 (5.1) | 262 (4.8) | 250 (4.6) | 125 (2.3) | 107 (2.0) | 93 (1.7) | 87 (1.6) |
| 1st | 2nd | 3rd | 4th | 5th | 6th | 7th | 8th | 9th | 10th | |
| Worries/stress group | High blood pressure | Dyslipidemia | Lumbago | Diabetes | Dental disease | Eye disease | Stiff shoulders | Joint disease | Depression, etc. | Other skin disease |
| Number (%) | 776 (15.2) | 383 (7.5) | 382 (7.5) | 354 (6.9) | 340 (6.7) | 335 (6.6) | 243 (4.8) | 180 (3.5) | 167 (3.3) | 144 (2.8) |
| Survey Attributes | Yes | (%) | No | (%) | Total | (%) | Unadjusted ORs | p Value (χ2 Test) |
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Male | 2257 | (44.3) | 2835 | (55.7) | 5092 | (100.0) | 0.733 | <0.001 |
| Female | 2858 | (52.0) | 2634 | (48.0) | 5492 | (100.0) | ||
| Self-rated health | ||||||||
| Poor | 1199 | (81.7) | 269 | (18.3) | 1468 | (100.0) | 5.918 | <0.001 |
| Regular/good | 3916 | (43.0) | 5200 | (57.0) | 9116 | (100.0) | ||
| Presence of subjective symptoms | ||||||||
| Yes | 2516 | (68.9) | 1137 | (31.1) | 3653 | (100.0) | 3.688 | <0.001 |
| No | 2599 | (37.5) | 4332 | (62.5) | 6931 | (100.0) | ||
| Presence of regular hospital visits | ||||||||
| Yes | 2611 | (54.0) | 2224 | (46.0) | 4835 | (100.0) | 1.522 | <0.001 |
| No | 2500 | (43.5) | 3242 | (56.5) | 5742 | (100.0) | ||
| Presence of regular clinic visits for dental disease | ||||||||
| Yes | 340 | (56.5) | 262 | (43.5) | 602 | (100.0) | 1.121 | 0.192 |
| No | 2271 | (53.6) | 1962 | (46.4) | 4233 | (100.0) | ||
| Symptoms: swollen/bleeding gums | ||||||||
| Yes | 192 | (78.7) | 52 | (21.3) | 244 | (100.0) | 1.724 | <0.001 |
| No | 2324 | (68.2) | 1085 | (31.8) | 3409 | (100.0) | ||
| Symptoms: difficulty chewing | ||||||||
| Yes | 151 | (73.7) | 54 | (26.3) | 205 | (100.0) | 1.281 | 0.127 |
| No | 2365 | (68.6) | 1083 | (31.4) | 3448 | (100.0) | ||
| Symptoms: tooth pain | ||||||||
| Yes | 2366 | (68.7) | 1076 | (31.3) | 3442 | (100.0) | 0.894 | 0.474 |
| No | 150 | (71.1) | 61 | (28.9) | 211 | (100.0) | ||
| Lifestyle awareness | ||||||||
| Harsh | 3459 | (53.1) | 3054 | (46.9) | 6513 | (100.0) | 1.652 | <0.001 |
| Regular/comfortable | 1656 | (40.7) | 2415 | (59.3) | 4071 | (100.0) | ||
| Smoking | ||||||||
| Yes | 1134 | (47.8) | 1236 | (52.2) | 2370 | (100.0) | 0.976 | 0.595 |
| No | 3981 | (48.5) | 4233 | (51.5) | 8214 | (100.0) | ||
| Drinking alcohol | ||||||||
| Yes | 1580 | (45.7) | 1875 | (54.3) | 3455 | (100.0) | 0.857 | <0.001 |
| No | 3535 | (49.6) | 3594 | (50.4) | 7129 | (100.0) | ||
| Health checkup behavior | ||||||||
| No checkups | 3374 | (47.5) | 3726 | (52.5) | 7100 | (100.0) | 0.907 | 0.017 |
| Checkups | 1741 | (50.0) | 1743 | (50.0) | 3484 | (100.0) |
| Selected Explanatory Variable | Partial Regression Coefficient | Wald | p Value | Judgement | Odds Ratio | Lower Limit | Upper Limit |
|---|---|---|---|---|---|---|---|
| Self-rated health (1, poor/0, wrt: regular, good) | 1.36 | 197.3 | <0.001 | ** | 3.91 | 3.23 | 4.73 |
| Lifestyle awareness (1, harsh/0, wrt: regular, comfortable) | 0.67 | 76.1 | <0.001 | ** | 1.96 | 1.68 | 2.28 |
| Symptoms: swollen/bleeding gums (1, yes/0, wrt: no) | 0.54 | 8.4 | 0.004 | ** | 1.71 | 1.19 | 2.48 |
| Symptoms: difficulty chewing (1, yes/0, wrt: no) | 0.43 | 4.8 | 0.028 | * | 1.54 | 1.05 | 2.29 |
| Health checkup behavior (1, no checkups/0, wrt: checkups) | 0.39 | 17.2 | <0.001 | ** | 1.48 | 1.23 | 1.79 |
| Age (1, elderly group/0, wrt: middle-aged group) | −0.67 | 73.0 | <0.001 | ** | 0.51 | 0.44 | 0.60 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Komatsuzaki, A.; Ono, S. Study of the Effects of Recognition of Stress on Symptoms and Regular Hospital Visits: An Analysis from Japanese National Statistics. Healthcare 2020, 8, 274. https://doi.org/10.3390/healthcare8030274
Komatsuzaki A, Ono S. Study of the Effects of Recognition of Stress on Symptoms and Regular Hospital Visits: An Analysis from Japanese National Statistics. Healthcare. 2020; 8(3):274. https://doi.org/10.3390/healthcare8030274
Chicago/Turabian StyleKomatsuzaki, Akira, and Sachie Ono. 2020. "Study of the Effects of Recognition of Stress on Symptoms and Regular Hospital Visits: An Analysis from Japanese National Statistics" Healthcare 8, no. 3: 274. https://doi.org/10.3390/healthcare8030274
APA StyleKomatsuzaki, A., & Ono, S. (2020). Study of the Effects of Recognition of Stress on Symptoms and Regular Hospital Visits: An Analysis from Japanese National Statistics. Healthcare, 8(3), 274. https://doi.org/10.3390/healthcare8030274





