Opportunities for Quality Improvement Programs (QIPs) in the Nutrition Support of Patients with Cancer
Abstract
1. Introduction
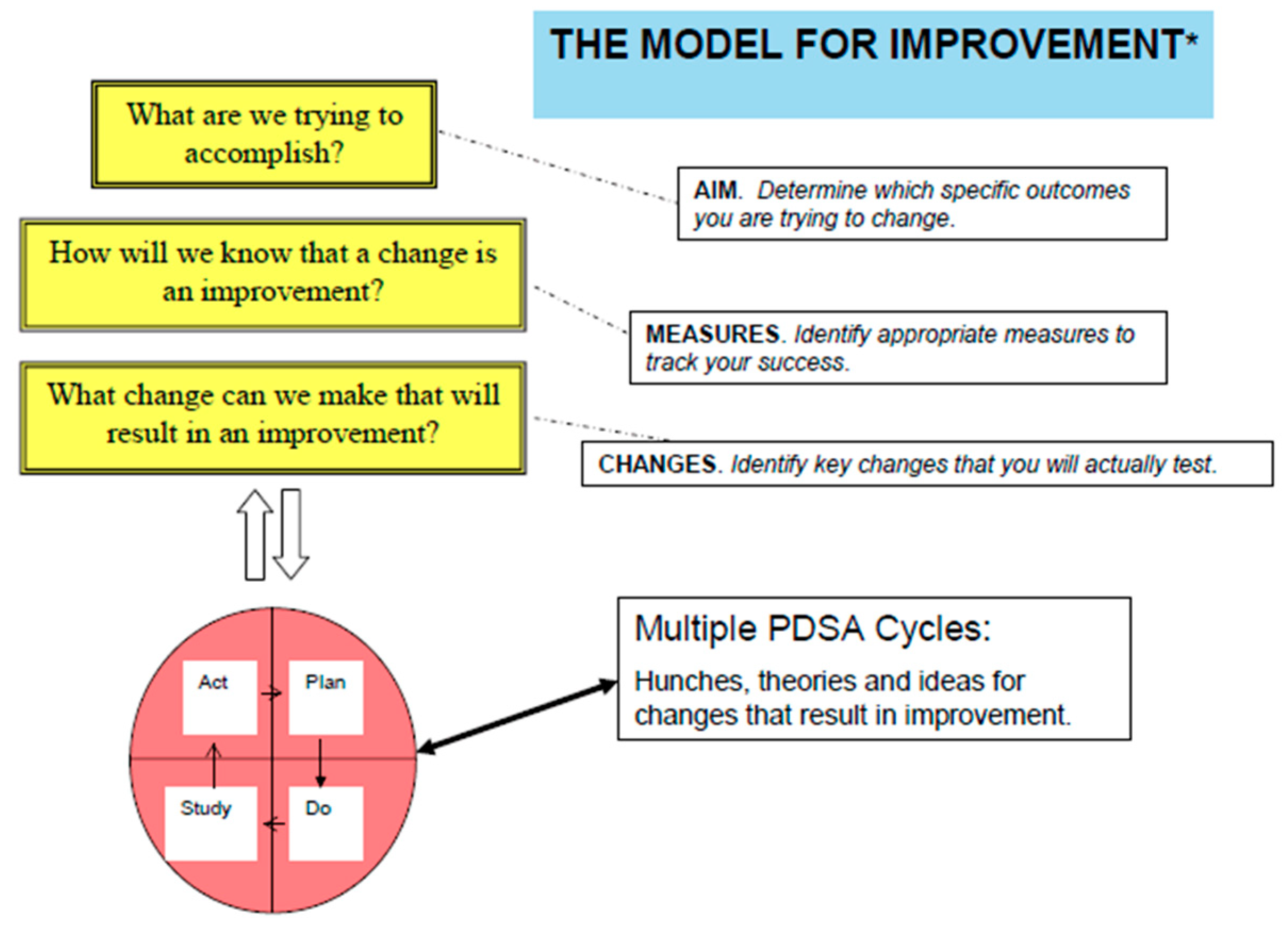
2. The Healthcare Quality Improvement Process
- Establishes improvement goals
- Identifies possible strategies
- Chooses specific interventions to implement
- Prepares a written action plan.
3. Quality Frameworks for Nutrition in Cancer Care
3.1. International Nutrition-Specific Oncology Care Guidelines
3.2. U.S. Nutrition-Specific Oncology Care Standards and Guidelines
3.3. Nutrition in U.S. General Oncology Care Standards and Guidelines
3.4. Nutrition in U.S. Cancer Care Quality Measures, Initiatives, and Data Sources
4. Review of Malnutrition and Nutrition-Focused QIPs in Cancer Care
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Walsh, D.; Szafranski, M.; Aktas, A.; Kadakia, K.C. Malnutrition in cancer care: Time to address the elephant in the room. J. Oncol. Pract. 2019, 15, 357–359. [Google Scholar] [CrossRef] [PubMed]
- Von Haehling, S.; Anker, S.D. Cachexia as a major underestimated and unmet medical need: Facts and numbers. J. Cachexia Sarcopenia Muscle 2010, 1, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Muscaritoli, M.; Lucia, S.; Farcomeni, A.; Lorusso, V.; Saracino, V.; Barone, C.; Plastino, F.; Gori, S.; Magarotto, R.; Carteni, G.; et al. Prevalence of malnutrition in patients at first medical oncology visit: The PreMiO study. Oncotarget 2017, 8, 79884–79896. [Google Scholar] [CrossRef] [PubMed]
- Caillet, P.; Liuu, E.; Raynaud Simon, A.; Bonnefoy, M.; Guerin, O.; Berrut, G.; Lesourd, B.; Jeandel, C.; Ferry, M.; Rolland, Y.; et al. Association between cachexia, chemotherapy and outcomes in older cancer patients: A systematic review. Clin. Nutr. Edinb. Scotl. 2017, 36, 1473–1482. [Google Scholar] [CrossRef]
- Dewys, W.D.; Begg, C.; Lavin, P.T.; Band, P.R.; Bennett, J.M.; Bertino, J.R.; Cohen, M.H.; Douglass, H.O.; Engstrom, P.F.; Ezdinli, E.Z.; et al. Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am. J. Med. 1980, 69, 491–497. [Google Scholar] [CrossRef]
- Martin, L.; Senesse, P.; Gioulbasanis, I.; Antoun, S.; Bozzetti, F.; Deans, C.; Strasser, F.; Thoresen, L.; Jagoe, R.T.; Chasen, M.; et al. Diagnostic criteria for the classification of cancer-associated weight loss. J. Clin. Oncol. 2015, 33, 90–99. [Google Scholar] [CrossRef]
- Wong, H.C.Y.; Lam, K.Y.; Chong, C.C.N.; Chan, A.W.H.; Chan, S.L. Impact of weight loss during chemotherapy in Chinese patients with unresectable pancreatic cancer. Nutr. Cancer 2019, 71, 954–970. [Google Scholar] [CrossRef]
- Takayoshi, K.; Uchino, K.; Nakano, M.; Ikejiri, K.; Baba, E. Weight loss during initial chemotherapy predicts survival in patients with advanced gastric cancer. Nutr. Cancer 2017, 69, 408–415. [Google Scholar] [CrossRef]
- Thompson, K.L.; Elliott, L.; Fuchs-Tarlovsky, V.; Levin, R.M.; Voss, A.C.; Piemonte, T. Oncology evidence-based nutrition practice guideline for adults. J. Acad. Nutr. Diet. 2017, 117, 297–310. [Google Scholar] [CrossRef]
- Trujillo, E.B.; Dixon, S.W.; Claghorn, K.; Levin, R.M.; Mills, J.B.; Spees, C.K. Closing the gap in nutrition care at outpatient cancer centers: Ongoing initiatives of the Oncology Nutrition Dietetic Practice Group. J. Acad. Nutr. Diet. 2018, 118, 749–760. [Google Scholar] [CrossRef]
- Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Fearon, K.; Hutterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN guidelines on nutrition in cancer patients. Clin. Nutr. Edinb. Scotl. 2017, 36, 11–48. [Google Scholar] [CrossRef] [PubMed]
- Trujillo, E.B.; Claghorn, K.; Dixon, S.W.; Hill, E.B.; Braun, A.; Lipinski, E.; Platek, M.E.; Vergo, M.T.; Spees, C. Inadequate nutrition coverage in outpatient cancer centers: Results of a national survey. J. Oncol. 2019, 2019, 7462940. [Google Scholar] [CrossRef] [PubMed]
- Centers for Medicare & Medicaid Services Oncology Care Model. Available online: https://innovation.cms.gov/innovation-models/oncology-care (accessed on 1 June 2020).
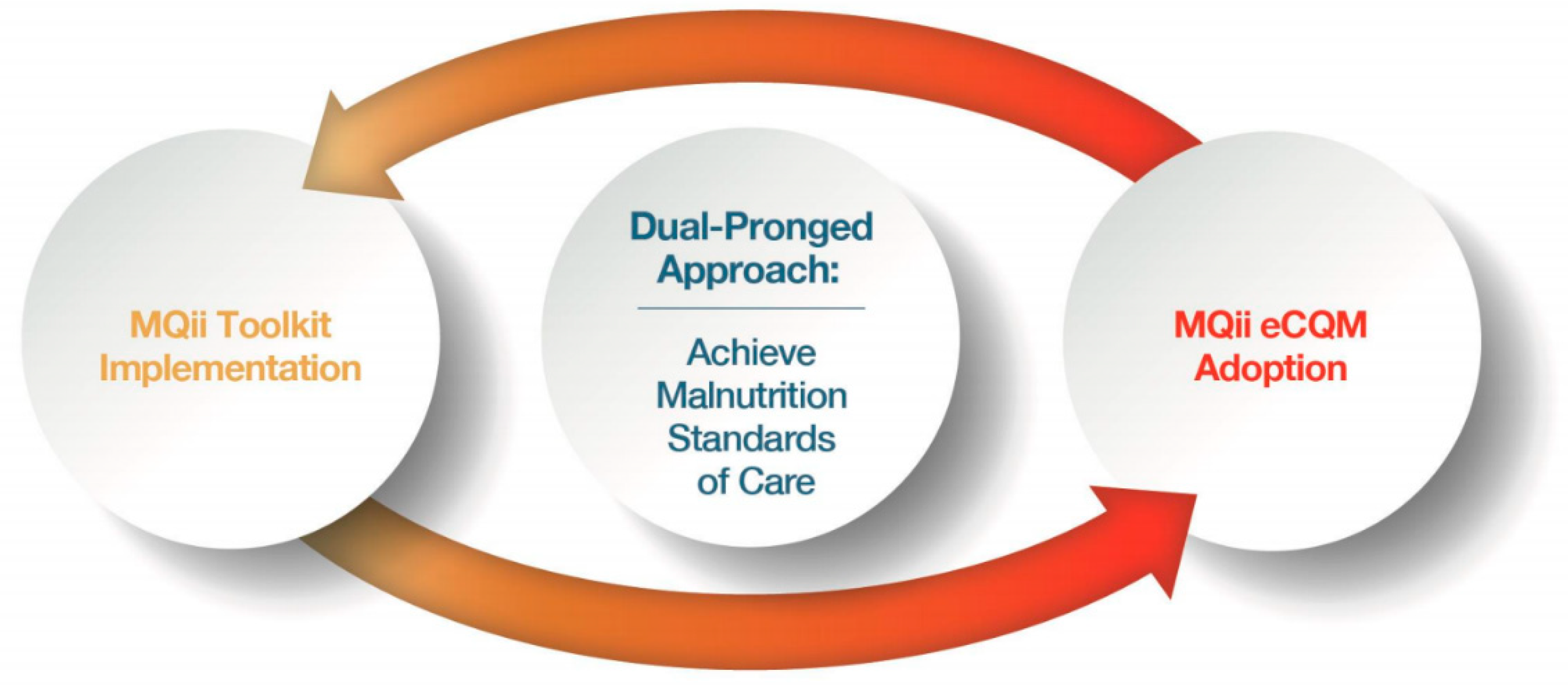
- McCauley, S.M.; Barrocas, A.; Malone, A. Hospital nutrition care betters patient clinical outcomes and reduces costs: The Malnutrition Quality Improvement Initiative story. J. Acad. Nutr. Diet. 2019, 119, S11–S14. [Google Scholar] [CrossRef] [PubMed]
- Agency for Healthcare Research and Quality Practice Facilitation Handbook, Module Approaches to Quality Improvement. Available online: https://www.ahrq.gov/ncepcr/tools/pf-handbook/mod4.html (accessed on 1 June 2020).
- Langley, G.; Nolan, T.; Provost, L.; Norman, C.; Moen, R.; Nolan, K. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance; Jossey-Bass: San Francisco, CA, USA, 1996. [Google Scholar]
- Deming, W.E. The New Economics for Industry, Government, Education; Massachusetts Institute of Technology: Cambridge, MA, USA, 1994. [Google Scholar]
- Malnutrition Quality Improvement Initiative (MQii). Available online: http://malnutritionquality.org/ (accessed on 1 June 2020).
- Electronic Clinical Quality Measures (eCQMs). Available online: https://www.eatrightpro.org/practice/quality-management/quality-improvement/malnutrition-quality-improvement-initiative (accessed on 1 June 2020).
- McCauley, S.M.; Mitchell, K.; Heap, A. The Malnutrition Quality Improvement Initiative: A multiyear partnership transforms care. J. Acad. Nutr. Diet. 2019, 119, S18–S24. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.H.; Yang, T.; Ma, X.D.; Qi, Y.X.; Lin, Y.Y.; Chen, X.Z.; Duan, Y.Q.; Sun, D.L. Heterogeneity of nutrition care procedures in nutrition guidelines for cancer patients. Clin. Nutr. 2020, 39, 1692–1704. [Google Scholar] [CrossRef]
- Evidence-Based Practice Guidelines for the Nutritional Management of Adult Patients with Head and Neck Cancer Clinical Guidelines Wiki. Available online: https://wiki.cancer.org.au/australia/COSA:Head_and_neck_cancer_nutrition_guidelines (accessed on 1 June 2020).
- August, D.A.; Huhmann, M.B.; American Society for Parenteral and Enteral Nutrition (ASPEN) Board of Directors. ASPEN. clinical guidelines: Nutrition support therapy during adult anticancer treatment and in hematopoietic cell transplantation. J. Parenter. Enteral Nutr. 2009, 33, 472–500. [Google Scholar] [CrossRef]
- Macris, P.C.; Schilling, K.; Palko, R. Academy of Nutrition and Dietetics: Revised 2017 standards of practice and standards of professional performance for registered dietitian nutritionists (competent, proficient, and expert) in oncology nutrition. J. Acad. Nutr. Diet. 2018, 118, 736–748. [Google Scholar] [CrossRef]
- Huhmann, M.B.; August, D.A. Review of American Society for Parenteral and Enteral Nutrition (ASPEN) Clinical Guidelines for Nutrition Support in Cancer Patients: Nutrition screening and assessment. Nutr. Clin. Pract. 2008, 23, 182–188. [Google Scholar] [CrossRef]
- Huhmann, M.B.; August, D.A. Nutrition support in surgical oncology. Nutr. Clin. Pract. 2009, 24, 520–526. [Google Scholar] [CrossRef]
- Optimal Resources for Cancer Care. Available online: https://www.facs.org/-/media/files/quality-programs/cancer/coc/optimal_resources_for_cancer_care_2020_standards.ashx (accessed on 14 July 2020).
- Nelson, G.; Bakkum-Gamez, J.; Kalogera, E.; Glaser, G.; Altman, A.; Meyer, L.A.; Taylor, J.S.; Iniesta, M.; Lasala, J.; Mena, G.; et al. Guidelines for perioperative care in gynecologic/oncology: Enhanced Recovery After Surgery (ERAS®) Society recommendations—2019 update. Int. J. Gynecol. Cancer 2019, 29, 651–668. [Google Scholar] [CrossRef]
- Dort, J.C.; Farwell, D.G.; Findlay, M.; Huber, G.F.; Kerr, P.; Shea-Budgell, M.A.; Simon, C.; Uppington, J.; Zygun, D.; Ljungqvist, O.; et al. Optimal perioperative care in major head and neck cancer with free flap reconstruction: A consensus review and recommendations form the Enhanced Recovery After Surgery Society. JAMA Otolaryngol. Head Neck Surg. 2017, 143, 292–303. [Google Scholar] [CrossRef] [PubMed]
- Yannick, C.; Valerio, M.; Persson, B.; Jichlinski, P.; Ljungqvist, O.; Hubner, M.; Kassouf, W.; Muller, S.; Galdini, G.; Carli, F.; et al. Guidelines for perioperative care after radical cystectomy for bladder cancer: Enhanced Recovery After Surgery (ERAS®) society recommendations. Clin. Nutr. 2013, 32, 879–887. [Google Scholar] [CrossRef]
- Nutrition in Cancer Care PDQ®. Available online: https://www.cancer.gov/about-cancer/treatment/side-effects/appetite-loss/nutrition-hp-pdq#_AboutThis_1 (accessed on 14 July 2020).
- National Comprehensive Cancer Network (NCCN) Guidelines. Available online: https://www.nccn.org/professionals/physician_gls/default.aspx (accessed on 1 June 2020).
- Guidelines, Tools & Resources. Available online: https://www.asco.org/research-guidelines/quality-guidelines/guidelines (accessed on 1 June 2020).
- QOPI® 2020 Reporting Tracks. Available online: https://practice.asco.org/sites/default/files/drupalfiles/QOPI-2020-Round-2-Reporting-Tracks-Public-Posting.pdf (accessed on 14 July 2020).
- CoC Quality of Care Measures. Available online: https://www.facs.org/quality-programs/cancer/ncdb/qualitymeasurescocweb (accessed on 14 July 2020).
- Cancer Measures. Available online: http://www.qualityforum.org/Projects/c-d/Cancer/Cancer.aspx (accessed on 14 July 2020).
- Quality Resources and Improvement Activities. Available online: https://www.ons.org/make-difference/quality-improvement/quality-improvement-registry (accessed on 14 July 2020).
- Quality Programs. Available online: https://practice.asco.org/quality-improvement/quality-programs (accessed on 14 July 2020).
- National Cancer Database. Available online: https://www.facs.org/quality-programs/cancer/ncdb (accessed on 14 July 2020).
- Brown, T.J.; Wolfe, H.R.; Hardy, S.; Bhulani, N.; Hong, C.; Khosama, L.; Cheedella, N.; Hobbs, S.; Froehlich, T.W.; Kamal, A.; et al. Development of a nutrition-focused quality improvement program for new patients with cancer seen at the UTSW Simmons Comprehensive Cancer Center (SCCC) outpatient gastrointestinal (GI) oncology clinic. J. Clin. Oncol. 2018, 36, 143. [Google Scholar] [CrossRef]
- Levonyak, N.; Hodges, M.P.; Broome, N.; Beg, M.S.; Kainthla, R.; Sanjeevaiah, A.; Sadeghi, N.; Pandey, N.; Mhoon, V.; Cox, J.V.; et al. A nutrition-focused quality improvement program to improve rate of documented nutrition plan at a safety-net hospital gastrointestinal (GI) oncology clinic. J. Clin. Oncol. 2019, 37, 289. [Google Scholar] [CrossRef]
- Kiss, N.; Gilliand, S.; Quinn, P.; Atkins, L.; Black, J.; Frowen, J. Evaluating the effectiveness of a nutrition assistant role in a head and neck cancer clinic. Nutr. Diet. 2019, 76, 21–27. [Google Scholar] [CrossRef]
- Pranoy, S.; Reynolds, M.; Lim, S. Evaluation of nutritional deficiencies in a new gastroenterology-led South Wales neuroendocrine tumour (NET) service. Neuroendocrinology 2019, 108, S87. [Google Scholar]
- Jacquelin-Ravel, N.; Pugliesi-Rinaldi, A.; Joly, C.; Ho, S.; Mareschal, J.; Dietrich, P.Y.; Dulguerov, P.; Miralbell, R.; Pichard, C. Onconut: Nutritional care optimization for cancer patients. Clin. Nutr. 2014, 33, S4. [Google Scholar] [CrossRef]
- Hill, A.; Kiss, N. Evaluation of an evidence-based nutrition care pathway for lung cancer patients undergoing radiotherapy. J. Thorac. Oncol. 2012, 7, S172. [Google Scholar]
- Loeliger, J.; Hodgson, B. Nutrition assistants and malnutrition in a cancer setting: Exploring an integrated model of care. Asia Pac. J. Clin. Oncol. 2010, 3, S137. [Google Scholar]
- Tappenden, K.A.; Quatrara, B.; Parkhurst, M.L.; Malone, A.M.; Fanjiang, G.; Ziegler, T.R. Critical role of nutrition in improving quality of care: An interdisciplinary call to action to address adult hospital malnutrition. JPEN J. Parenter. Enteral Nutr. 2013, 37, 482–497. [Google Scholar] [CrossRef]
- Pedrazzoli, P.; Caccialanza, R.; Cotogni, P.; Esposti, L.D.; Perrone, V.; Sangiorgi, D.; DiCostanzo, F.; Gavazzi, C.; Santoro, A.; Pinto, C. The advantages of clinical nutrition use in oncologic patients in Italy: Real world insights. Healthcare 2020, 8, 125. [Google Scholar] [CrossRef] [PubMed]
- Ravasco, P. Nutrition in cancer patients. J. Clin. Med. 2019, 8, 1211. [Google Scholar] [CrossRef]
- Pratt, K.J.; Hernandez, B.; Blancato, R.; Blankenship, J.; Mitchell, K. Impact of an interdisciplinary malnutrition quality improvement project at a large metropolitan hospital. BMJ Open Qual. 2020, 9, e000735. [Google Scholar] [CrossRef] [PubMed]
- Taurchini, M.; Del Naja, C.; Tancredi, A. Enhanced Recovery After Surgery: A patient centered process. J. Vis. Surg. 2018, 4, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Boitano, T.K.L.; Smith, H.J.; Rushton, T.; Johnston, M.C.; Lawson, P.; Leath, C.A.; Xhaja, A.; Guthrie, M.P.; Straughn, J.M. Impact of Enhanced Recovery After Surgery (ERAS®) protocol on gastrointestinal function in gynecologic oncology patients undergoing laparotomy. Gynecol. Oncol. 2018, 151, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Bisch, S.P.; Wells, T.; Garmlich, L.; Faris, P.; Wang, X.; Tran, D.T.; Thanh, N.X.; Glaze, S.; Chu, P.; Ghatage, P.; et al. Enhanced Recovery After Surgery (ERAS®) in gynecologic oncology: System-wide implementation and audit leads to improved value and patient outcomes. Gynecol. Oncol. 2018, 141, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Pisarska, M.; Torbicz, G.; Gajewska, N.; Rubinkiewicz, M.; Wierdak, M.; Major, P.; Budzynski, A.; Ljungqvist, O.; Pedziwiatr, M. Compliance with ERAS® protocol and 3-year survival after laparoscopic surgery for non-metastatic colorectal cancer. World J. Surg. 2019, 43, 2552–2560. [Google Scholar] [CrossRef]
- Include MNT into Care Design and Payment for Future Oncology Model. Available online: https://www.eatrightpro.org/news-center/on-the-pulse-of-public-policy/regulatory-comments/include-mnt-into-care-design-and-payment-for-future-oncology-model (accessed on 1 June 2020).
- Food and Nutrition Board; Health and Medicine Division; National Academies of Sciences, Engineering, and Medicine. Examining Access to Nutrition Care in Outpatient Cancer Centers: Proceedings of a Workshop; National Academies Press: Washington, DC, USA, 2016. Available online: https://www.ncbi.nlm.nih.gov/books/NBK379326/ (accessed on 1 June 2020).
- Adams, K.M.; Kohlmeier, M.; Powell, M.; Zeisel, S.H. Nutrition in medicine: Nutrition education for medical students and residents. Nutr. Clin. Pract. 2010, 25, 471–480. [Google Scholar] [CrossRef]
- Crowley, J.; Ball, L.; Hiddink, G.J. Nutrition in medical education: A systematic review. Lancet Planet. Health 2019, 3, e379. [Google Scholar] [CrossRef]
- The Malnutrition Quality Collaborative. National Blueprint: Achieving Quality Malnutrition Care for Older Adults; Avalere Health and Defeat Malnutrition Today: Washington, DC, USA, 2020; Available online: https://www.defeatmalnutrition.today/sites/default/files/National_Blueprint_MAY2020_Update_OnlinePDF_FINAL.pdf (accessed on 14 July 2020).
- Muscaritoli, M.; Arends, J.; Aapro, M. From guidelines to clinical practice: A roadmap for oncologists for nutrition therapy for cancer patients. Ther. Adv. Med. Oncol. 2019, 11. [Google Scholar] [CrossRef]
- Rauh, S.; Antonuzzo, A.; Bossi, P.; Eckert, R.; Fallon, M.; Frobe, A.; Gonella, S.; Giusti, R.; Lakatos, G.; Santini, D.; et al. Nutrition in patients with cancer: A new area for medical oncologists? A practising oncologist’s interdisciplinary position paper. ESMO Open 2018, 3, e000345. [Google Scholar] [CrossRef] [PubMed]
- eCQMs Frequently Asked Questions. Available online: https://www.eatrightpro.org/practice/quality-management/quality-improvement/ecqms-frequently-asked-questions (accessed on 1 June 2020).
- Mullin, G.E.; Fan, L.; Sulo, S.; Partridge, J. The association between oral nutrition supplements and 30-day hospital readmissions of malnourished patients at a US academic medical center. J. Acad. Nutr. Diet. 2019, 119, 1168–1174. [Google Scholar] [CrossRef] [PubMed]
- Arensberg, M.B.; Sulo, S.; Drawert, S. United States value-based payment programs provide framework for developing nutrition-focused quality improvement programs (QIPs) to address malnutrition in outpatient cancer care. J. Clin. Nutr. Food Sci. 2020. accepted. [Google Scholar]
| Organization and Developer | Title and Target Audience | Methodology and Scope |
|---|---|---|
| Academy of Nutrition and Dietetics (the Academy) Oncology Workgroup | Oncology Evidence-Based Nutrition Practice Guideline for Adults [9] Registered Dietitian Nutritionists (RDNs) |
|
| Academy Oncology Nutrition Dietetic Practice Group, with guidance from Academy Quality Management Committee | Academy of Nutrition and Dietetics: Revised 2017 Standards of Practice and Standards of Professional Performance for Registered Dietitian Nutritionists (Competent, Proficient, and Expert) in Oncology Nutrition [24] RDNs |
|
| American Society for Parenteral and Enteral Nutrition (ASPEN) ASPEN Members | Review of American Society for Parenteral and Enteral Nutrition (ASPEN) Clinical Guidelines for Nutrition Support in Cancer Patients: Nutrition Screening and Assessment [25] Multidisciplinary teams |
|
| ASPEN ASPEN Members | Nutrition Support in Surgical Oncology [26] Multidisciplinary teams |
|
| ASPEN ASPEN Members and Board of Directors | ASPEN Clinical Guidelines: Nutrition Support Therapy During Adult Anticancer Treatment and in Hematopoietic Cell Transplantation [23] Multidisciplinary teams |
|
| Organization | Reference | Methodology and Scope |
|---|---|---|
| American College of Surgeons (ACS) ACS Multidisciplinary Commission on Cancer | Commission on Cancer. Optimal Resources for Cancer Care (2020 Standards) [27] Accredited U.S. cancer programs |
|
| Enhanced Recovery After Surgery (ERAS®) Society Joint efforts of the ERAS® Society and authors from the international ERAS® Gynecology chapters | Guidelines for Perioperative Care in Gynecologic/Oncology: Enhanced Recovery After Surgery (ERAS®) Society Recommendations-2019 Update [28] Surgical teams |
|
| ERAS® Society Endorsed by ERAS® Society and international panel of experts in major head/neck cancer surgery and enhanced recovery after surgery | Optimal Perioperative Care in Major Head and Neck Cancer Surgery with Free Flap Reconstruction, a Consensus Review and Recommendations from the Enhanced Recovery After Surgery Society [29] Surgical teams |
|
| ERAS® Society ERAS® Society working group | Guidelines for Perioperative Care after Radical Cystectomy for Bladder Cancer: Enhanced Recovery After Surgery (ERAS®) Society recommendations [30] Surgical teams |
|
| National Cancer Institute PDQ® Supportive and Palliative Care Editorial Board | PDQ® Nutrition in Cancer Care [31] Clinicians |
|
| Type of NCCN Guideline (N) | Number (%) of NCCN Guidelines with Nutrition Mentions | NCCN Guidelines with Specific Nutrition Section |
|---|---|---|
| Diagnosis-specific guidelines (53) | 19 (36%) 1–10 nutrition mentions 3 (6%) 11–25 nutrition mentions 3 (6%) >25 nutrition mentions | Head and neck cancer |
| Population-specific guidelines (2) | 1 (50%) 1–10 nutrition mentions 1 (50%) >25 nutrition mentions | Older adult oncology |
| Supportive care guidelines (12) | 6 (50%) 1–10 nutrition mentions 3 (25%) >25 nutrition mentions | Cancer-related fatigue Survivorship |
| Patient-directed guidelines (39) | 9 (23%) 1–10 nutrition mention 2 (5%) 11–25 nutrition mentions | Nasopharyngeal cancer Oral cancers Stomach cancer |
| String | Terms |
|---|---|
| Cancer | Cancer, neoplasm, tumor, oncology, carcinoma, sarcoma |
| Nutrition | Food, diet, nutrition |
| Care | Assessment, care plan, plan, counsel, council, diagnosis, consult, discharge education, education, evaluation, index, intervention, monitoring, oral nutrition supplement (ONS), screening, therapy, treatment |
| Efficacy | Efficacy, effectiveness, efficient, efficiency, effectiveness, effectivity |
| Quality | Improvement of quality, improvement of care, improvement of treatment, improvement of therapy |
| Publication Type and Cancer Diagnosis | Title | Methodology | Conclusions |
|---|---|---|---|
| Article Head and neck cancer | Evaluating the effectiveness of a nutrition assistant role in a head and neck cancer clinic [42] |
|
|
| Conference abstract Neuroendocrine tumor (NET) | Evaluation of nutritional deficiencies in a new gastroenterology-led South Wales neuroendocrine tumor (NET) service [43] |
|
|
| Conference abstract Gastrointestinal (GI) cancer | A nutrition-focused quality improvement program to improve rate of documented nutrition plan at a safety-net hospital gastrointestinal (GI) oncology clinic [41] |
|
|
| Conference abstract Gastrointestinal (GI) cancer | Development of a nutrition-focused quality improvement program for new patients with cancer seen at the UTSW Simmons Comprehensive Cancer Center (SCCC) outpatient gastrointestinal (GI) oncology clinic [40] |
|
|
| Conference abstract Not specified | Onconut®: Nutritional care optimization for cancer patients [44] |
|
|
| Conference abstract Lung cancer | Evaluation of an evidence-based nutrition care pathway for lung cancer patients undergoing radiotherapy [45] |
|
|
| Conference abstract Not specified | Nutrition assistants and malnutrition in a cancer setting: Exploring an integrated model of care [46] |
|
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arensberg, M.B.; Richards, J.; Benjamin, J.; Kerr, K.; Hegazi, R. Opportunities for Quality Improvement Programs (QIPs) in the Nutrition Support of Patients with Cancer. Healthcare 2020, 8, 227. https://doi.org/10.3390/healthcare8030227
Arensberg MB, Richards J, Benjamin J, Kerr K, Hegazi R. Opportunities for Quality Improvement Programs (QIPs) in the Nutrition Support of Patients with Cancer. Healthcare. 2020; 8(3):227. https://doi.org/10.3390/healthcare8030227
Chicago/Turabian StyleArensberg, Mary Beth, Julie Richards, Jyoti Benjamin, Kirk Kerr, and Refaat Hegazi. 2020. "Opportunities for Quality Improvement Programs (QIPs) in the Nutrition Support of Patients with Cancer" Healthcare 8, no. 3: 227. https://doi.org/10.3390/healthcare8030227
APA StyleArensberg, M. B., Richards, J., Benjamin, J., Kerr, K., & Hegazi, R. (2020). Opportunities for Quality Improvement Programs (QIPs) in the Nutrition Support of Patients with Cancer. Healthcare, 8(3), 227. https://doi.org/10.3390/healthcare8030227






