Factors Influencing Global Variations in COVID-19 Cases and Fatalities; A Review
Abstract
1. Introduction
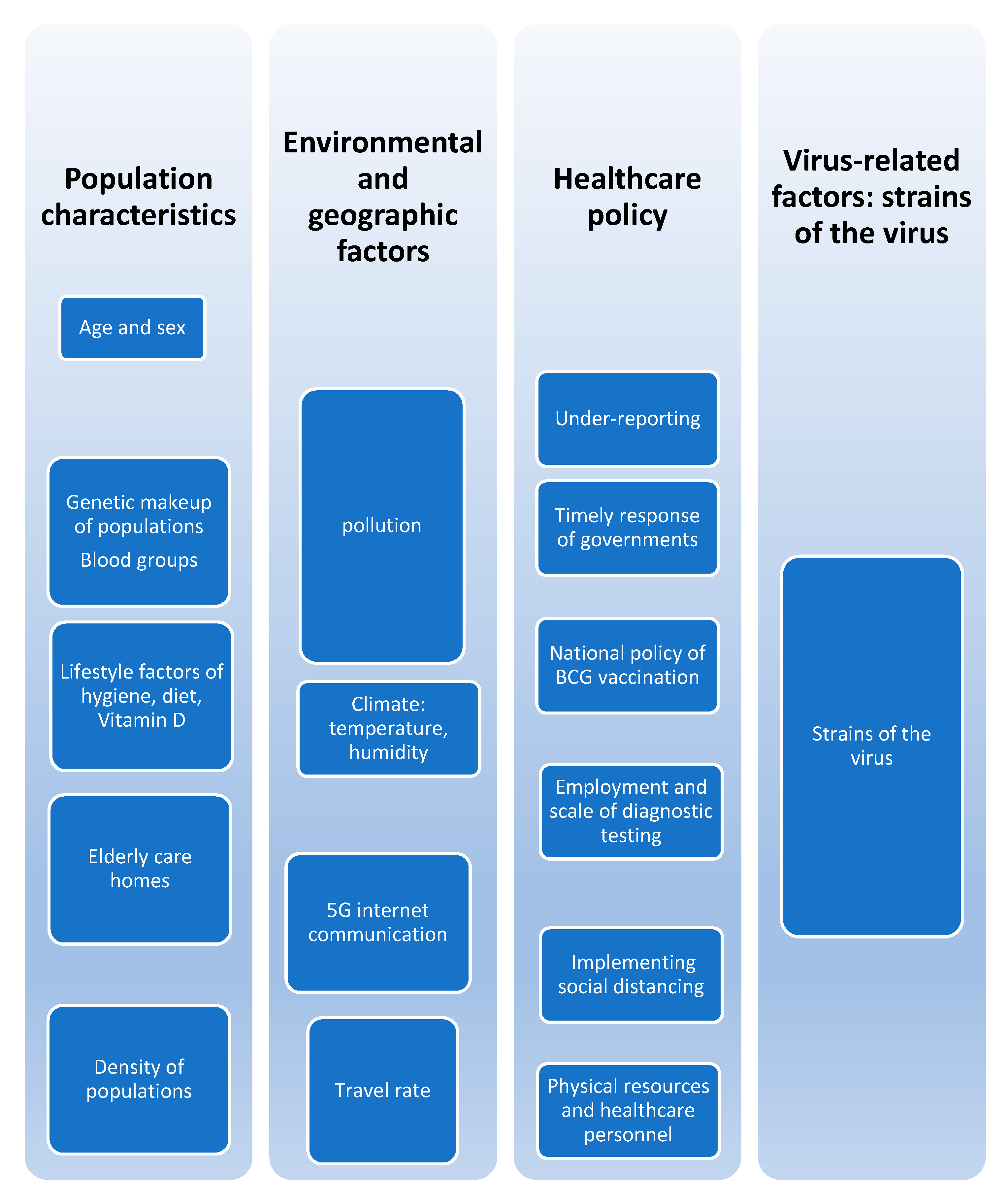
2. Potential Factors Influencing COVID-19 Case and Death Rates
2.1. Population Characteristics
2.1.1. Age and Sex
2.1.2. Genetic and Racial Characteristics
2.1.3. Social Life Style Factors
2.1.4. Elderly Home Facilities
2.1.5. Density of Population
2.2. Healthcare Policy
2.2.1. Bacille Calmette-Guérin (BCG) Vaccination
2.2.2. Screening, Testing, and Under-Reporting
2.2.3. Insufficient Physical and Human Health Resources
2.3. Environmental Factors
2.4. Virus Factors
Author Contributions
Funding
Conflicts of Interest
References
- Najla, D.O.; Hamzah, B.; Shaden, A.-H.S.B.; Abdalla, A.-H.O.A. COVID-19: Present and Future Challenges for Dental Practice. Int. J. Environ. Res. Public Health 2020, 17, 3151. [Google Scholar]
- Li, L.Y.; Wu, W.; Chen, S.; Gu, J.W.; Li, X.L.; Song, H.J.; Feng, D.; Gang, W.; Chang, Q.Z.; Xiao, Y.W.; et al. Digestive system involvement of novel coronavirus infection: Prevention and control infection from a gastroenterology perspective. J. Dig. Dis. 2020, 21, 199–204. [Google Scholar] [CrossRef]
- Nouri-Vaskeh, M.; Alizadeh, L. Fecal transmission in COVID-19: A potential shedding route. J. Med. Virol. 2020. [Google Scholar] [CrossRef] [PubMed]
- World Economic Forum. Available online: https://www.weforum.org/agenda/2020/03/coronavirus-covid-19-cost-economy-2020-un-trade-economics-pandemic/2020 (accessed on 15 June 2020).
- Amariles, P.; Granados, J.; Ceballos, M.; Montoya, C.J. COVID-19 in Colombia endpoints. Are we different, like Europe? Res. Soc. Adm. Pharm. 2020. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Morales, A.J.; Cardona-Ospina, J.A.; Gutiérrez-Ocampo, E.; Villamizar-Peña, R.; Holguin-Rivera, Y.; Escalera-Antezana, J.P.; Alvarado-Arnez, L.E.; Bonilla-Aldana, D.K.; Franco-Paredes, C.; Henao-Martinez, A.F.; et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med. Infect. Dis. 2020, 34, 101623. [Google Scholar] [CrossRef] [PubMed]
- Velavan, T.P.; Meyer, C.G. The COVID-19 epidemic. Trop. Med. Int. Health 2020, 25, 278–280. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Onder, G.; Rezza, G.; Brusaferro, S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. J. Am. Med. Assoc. 2020. [Google Scholar] [CrossRef] [PubMed]
- Roved, J.; Westerdahl, H.; Hasselquist, D. Sex differences in immune responses: Hormonal effects, antagonistic selection, and evolutionary consequences. Horm. Behav. 2017, 88, 95–105. [Google Scholar] [CrossRef]
- Conti, P.; Younes, A. Coronavirus COV-19/SARS-CoV-2 affects women less than men: Clinical response to viral infection. J. Biol. Regul. Homeost. Agents 2020, 34. [Google Scholar] [CrossRef]
- Gudbjartsson, D.F.; Helgason, A.; Jonsson, H.; Magnusson, O.T.; Melsted, P.; Norddahl, G.L.; Saemundsdottir, J.; Sigurdsson, A.; Sulem, P.; Agustsdottir, A.B.; et al. Spread of SARS-CoV-2 in the Icelandic Population. N. Engl. J. Med. 2020, 382, 2302–2315. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.D. Antihypertensive drugs and risk of COVID-19? Lancet Respir. Med. 2020, 8, e28. [Google Scholar] [CrossRef]
- Zietz, M.; Tatonetti, N.P. Testing the association between blood type and COVID-19 infection, intubation, and death. MedRxiv 2020. [Google Scholar] [CrossRef]
- Lindesmith, L.; Moe, C.; Marionneau, S.; Ruvoen, N.; Jiang, X.; Lindblad, L.; Stewart, P.; LePendu, J.; Baric, R. Human susceptibility and resistance to Norwalk virus infection. Nat. Med. 2003, 9, 548–553. [Google Scholar] [CrossRef]
- Batool, Z.; Durrani, S.H.; Tariq, S. Association of Abo and Rh Blood Group Types to Hepatitis B, Hepatitis C, HIV And Syphilis Infection, a Five Year’ Experience in Healthy Blood Donors in a Tertiary Care Hospital. J. Ayub. Med. Coll. Abbottabad 2017, 29, 90–92. [Google Scholar]
- Cheng, Y.; Cheng, G.; Chui, C.H.; Lau, F.Y.; Chan, P.K.S.; Ng, M.H.L.; Sung, J.J.Y.; Wong, R.S.M. ABO blood group and susceptibility to severe acute respiratory syndrome. J. Am. Med. Assoc. 2005, 293, 1450–1451. [Google Scholar] [CrossRef]
- Zhao, J.; Yang, Y.; Huang, H.-P.; Li, D.; Gu, D.-F.; Lu, X.-F.; Zhang, Z.; Liu, L.; Liu, T.; Liu, Y.K.; et al. Relationship between the ABO Blood Group and the COVID-19 Susceptibility. MedRxiv 2020. [Google Scholar] [CrossRef]
- Guillon, P.; Clément, M.; Sébille, V.; Rivain, J.G.; Chou, C.F.; Ruvoën-Clouet, N.; Pendu, J.L. Inhibition of the interaction between the SARS-CoV Spike protein and its cellular receptor by anti-histo-blood group antibodies. Glycobiology 2008, 18, 1085–1093. [Google Scholar] [CrossRef]
- Dyer, O. Covid-19: Black people and other minorities are hardest hit in US. BMJ 2020, 369, m1483. [Google Scholar] [CrossRef]
- Millett, G.A.; Jones, A.T.; Benkeser, D.; Baral, S.; Mercer, L.; Beyrer, C.; Honermann, B.; Lankiewicz, E.; Mena, L.; Crowley, J.S.; et al. Assessing Differential Impacts of COVID-19 on Black Communities. Ann. Epidemiol. 2020, 47, 37–44. [Google Scholar] [CrossRef]
- Bentrem, F.W. COVID-19 Death Rate: Is it in our DNA? Preprint 2020. [Google Scholar] [CrossRef]
- Antonio, C.; Vicent, M.; Armando, A.d.S. Coronavirus, Population Genetics, and Humanities. Mirabilia 2020, 30, 2–15. [Google Scholar]
- van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef]
- Elsayed, S.; Abu-Hammad, O.; Alolayan, A.; Althagafi, N.; Ayed, Y.; Dar-Odeh, N. Getting to Know SARS-CoV-2: Towards a Better Understanding of the Factors Influencing Transmission. Pesqui. Bras. Odontopediatr. Clin. Integr. 2020, 20, 0122. [Google Scholar]
- Lin, C.M.; Wu, F.M.; Kim, H.K.; Doyle, M.P.; Michaels, B.S.; Williams, L.K. A Comparison of Hand Washing Techniques to Remove Escherichia coli and Caliciviruses under Natural or Artificial Fingernails. J. Food Prot. 2003, 66, 2296–2301. [Google Scholar] [CrossRef] [PubMed]
- Berardi, A.; Perinelli, D.R.; Merchant, H.A.; Bisharat, L.; Basheti, I.A.; Bonacucina, G.; Cespi, M.; Palmieri, G.F. Hand sanitisers amid CoViD-19: A critical review of alcohol-based products on the market and formulation approaches to respond to increasing demand. Int. J. Pharm. 2020, 584, 119431. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, A.; Grubaugh, N.D. Why does Japan have so few cases of COVID19? EMBO Mol. Med. 2020, 12, e12481. [Google Scholar] [CrossRef] [PubMed]
- Andersen, C.J.; Murphy, K.E.; Fernandez, M.L. Impact of Obesity and Metabolic Syndrome on Immunity. Adv. Nutr. 2016, 7, 66–75. [Google Scholar] [CrossRef]
- Honce, R.; Schultz-Cherry, S. Impact of obesity on influenza A virus pathogenesis, immune response, and evolution. Front Immunol. 2019, 10, 1071. [Google Scholar] [CrossRef]
- Dhama, K.; Sharun, K.; Tiwari, R.; Dadar, M.; Malik, Y.S.; Singh, K.P.; Chaicumpa, W. COVID-19, an emerging coronavirus infection: Advances and prospects in designing and developing vaccines, immunotherapeutics, and therapeutics. Hum. Vaccines Immunother. 2020, 16, 1232–1238. [Google Scholar] [CrossRef]
- Rhodes, J.M.; Subramanian, S.; Laird, E.; Griffin, G.; Kenny, R.A. Perspective: Vitamin D deficiency and COVID-19 severity—Plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2, and thrombosis (R1). J. Intern. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Yang, J.; Chen, J.; Luo, Q.; Zhang, Q.; Zhang, H. Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system. Mol. Med. Rep. 2017, 16, 7432–7438. [Google Scholar] [CrossRef]
- Scott, D.; Blizzard, L.; Fell, J.; Ding, C.; Winzenberg, T.; Jones, G. A prospective study of the associations between 25-hydroxy-vitamin D, sarcopenia progression and physical activity in older adults. Clin. Endocrinol. 2010, 73, 581–587. [Google Scholar] [CrossRef] [PubMed]
- McMichael, T.M.; Currie, D.W.; Clark, S.; Pogosjans, S.; Kay, M.; Schwartz, N.G.; Lewis, J.; Baer, A.; Kawakami, V.; Luko, M.D.; et al. Epidemiology of Covid-19 in a Long-Term Care Facility in King County, Washington. N. Engl. J. Med. 2020, 382, 2005–2011. [Google Scholar] [CrossRef]
- McConnell, D. Balancing the duty to treat with the duty to family in the context of the COVID-19 pandemic. J. Med. Ethics 2020, 46, 360–363. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, L.A.J.; Netea, M.G. BCG-induced trained immunity: Can it offer protection against COVID-19? Nat. Rev. Immunol. 2020, 20, 335–337. [Google Scholar] [CrossRef]
- World Health Organization [WHO]. 2020. Available online: https://www.who.int/news-room/commentaries/detail/bacille-calmette-gu%C3%A9rin-(bcg)-vaccination-and-covid-19 (accessed on 15 June 2020).
- Vrieze, J. Can a century-old TB vaccine steel the immune system against the new coronavirus? Science 2020. [Google Scholar] [CrossRef]
- Paital, B.; Das, K.; Parida, S.K. Inter nation social lockdown versus medical care against COVID-19, a mild environmental insight with special reference to India. Sci. Total Environ. 2020, 728, 138914. [Google Scholar] [CrossRef]
- Mahato, S.; Pal, S.; Ghosh, K.G. Effect of lockdown amid COVID-19 pandemic on air quality of the megacity Delhi, India. Sci. Total Environ. 2020, 730, 139086. [Google Scholar] [CrossRef]
- Riccioni, L.; Bertolini, G.; Giannini, A.; Vergano, M.; Gristina, G.; Livigni, S.; Mistraletti, G.; Flavia Petrini Gruppo di Lavoro Siaarti-Società Italiana di Anestesia Analgesia Rianimazione E Terapia Intensiva. Clinical ethics recommendations for the allocation of intensive care treatments, in exceptional, resource-limited circumstances. Recenti Prog. Med. 2020, 111, 207–211. [Google Scholar] [CrossRef]
- Jackson, D.; Anders, R.; Padula, W.V.; Daly, J.; Davidson, P.M. Vulnerability of nurse and physicians with COVID-19: Monitoring and surveillance needed. J. Clin. Nurs. 2020. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Zhang, J.; Meadows, M.E.; Liu, Y.; Hua, T.; Fu, B. A systematic approach is needed to contain COVID-19 globally. Sci. Bull. 2020, 65, 876–878. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Tang, K.; Feng, K.; Lv, W. High Temperature and High Humidity Reduce the Transmission of COVID-19. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Moriyama, M.; Hugentobler, W.J.; Iwasaki, A. Seasonality of Respiratory Viral Infections. Annu. Rev. Virol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Brandt, E.B.; Beck, A.F.; Mersha, T.B. Air pollution, racial disparities and COVID-19 mortality. J. Allergy Clin. Immunol. 2020, 146, 61–63. [Google Scholar] [CrossRef]
- Zhu, Y.; Xie, J.; Huang, F.; Cao, L. Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Sci. Total Environ. 2020, 727, 138704. [Google Scholar] [CrossRef]
- De Wit, E.; Van Doremalen, N.; Falzarano, D.; Munster, V.J. SARS and MERS: Recent insights into emerging coronaviruses. Nat. Rev. Microbiol. 2016, 14, 523–534. [Google Scholar] [CrossRef]
| Country | Total Cases | Total Deaths | Cases/M | Deaths/M | Total Tests | Tests/M | Population | |
|---|---|---|---|---|---|---|---|---|
| 1 | USA | 3,159,414 | 134,867 | 9544 | 407 | 39,482,200 | 119,265 | 331,044,624 |
| 2 | Brazil | 1,716,196 | 68,055 | 8073 | 320 | 4,468,829 | 21,021 | 212,591,154 |
| 3 | India | 769,257 | 21,161 | 557 | 15 | 10,740,832 | 7782 | 1,380,270,828 |
| 4 | Russia | 707,301 | 10,843 | 4847 | 74 | 22,079,294 | 151,294 | 145,935,982 |
| 5 | Peru | 312,911 | 11,133 | 9488 | 338 | 1,842,316 | 55,862 | 32,979,917 |
| 6 | Chile | 303,083 | 6573 | 15,852 | 344 | 1,220,790 | 63,850 | 19,119,526 |
| 7 | Spain | 299,593 | 28,396 | 6408 | 607 | 5,734,599 | 122,652 | 46,755,218 |
| 8 | UK | 286,979 | 44,517 | 4227 | 656 | 11,041,203 | 162,625 | 67,893,830 |
| 9 | Mexico | 275,003 | 32,796 | 2132 | 254 | 684,804 | 5310 | 128,958,893 |
| 10 | Iran | 248,379 | 12,084 | 2956 | 144 | 1,872,391 | 22,287 | 84,012,442 |
| 11 | Italy | 242,149 | 34,914 | 4005 | 577 | 5,754,116 | 95,173 | 60,459,584 |
| 12 | Pakistan | 240,848 | 4983 | 1090 | 23 | 1,491,437 | 6750 | 220,955,441 |
| 13 | South Africa | 224,665 | 3602 | 3787 | 61 | 1,944,399 | 32,777 | 59,322,322 |
| 14 | Saudi Arabia | 220,144 | 2059 | 6322 | 59 | 2,071,823 | 59,496 | 34,822,930 |
| 15 | Turkey | 208,938 | 5282 | 2477 | 63 | 3,782,520 | 44,840 | 84,356,463 |
| 16 | Germany | 198,765 | 9115 | 2372 | 109 | 6,376,054 | 76,096 | 83,790,088 |
| Model | Unstandardized Coefficients | Standardized Coefficients | t | Sig. | 95.0% Confidence Interval for B | ||
|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Lower Bound | Upper Bound | |||
| (Constant) | 955.097 | 260.348 | 3.669 | 0.000 | 441.536 | 1468.657 | |
| Tests/M | 0.023 | 0.003 | 0.426 | 6.470 | 0.000 | 0.016 | 0.030 |
| R | R Square | Adjusted R Square | Std. Error of the Estimate | Durbin-Watson |
|---|---|---|---|---|
| 0.426 | 0.181 | 0.177 | 3057.12969 | 2.160 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abu-Hammad, O.; Alnazzawi, A.; Borzangy, S.S.; Abu-Hammad, A.; Fayad, M.; Saadaledin, S.; Abu-Hammad, S.; Dar-Odeh, N. Factors Influencing Global Variations in COVID-19 Cases and Fatalities; A Review. Healthcare 2020, 8, 216. https://doi.org/10.3390/healthcare8030216
Abu-Hammad O, Alnazzawi A, Borzangy SS, Abu-Hammad A, Fayad M, Saadaledin S, Abu-Hammad S, Dar-Odeh N. Factors Influencing Global Variations in COVID-19 Cases and Fatalities; A Review. Healthcare. 2020; 8(3):216. https://doi.org/10.3390/healthcare8030216
Chicago/Turabian StyleAbu-Hammad, Osama, Ahmad Alnazzawi, Sary S. Borzangy, Abdalla Abu-Hammad, Mostafa Fayad, Selma Saadaledin, Shaden Abu-Hammad, and Najla Dar-Odeh. 2020. "Factors Influencing Global Variations in COVID-19 Cases and Fatalities; A Review" Healthcare 8, no. 3: 216. https://doi.org/10.3390/healthcare8030216
APA StyleAbu-Hammad, O., Alnazzawi, A., Borzangy, S. S., Abu-Hammad, A., Fayad, M., Saadaledin, S., Abu-Hammad, S., & Dar-Odeh, N. (2020). Factors Influencing Global Variations in COVID-19 Cases and Fatalities; A Review. Healthcare, 8(3), 216. https://doi.org/10.3390/healthcare8030216







