Adjusting Daily Inpatient Bed Allocation to Smooth Emergency Department Occupancy Variation
Abstract
1. Introduction
2. Materials and Methods
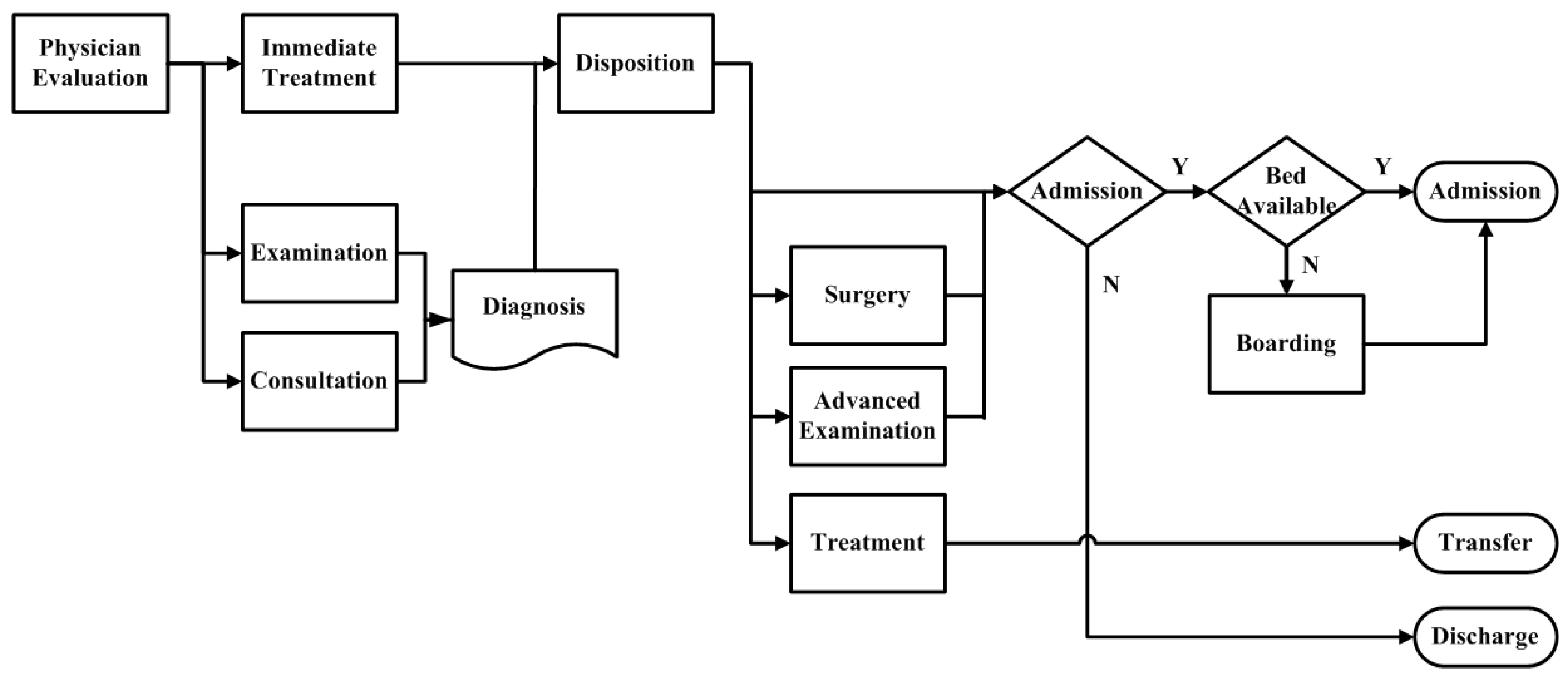
2.1. Model Development
- Proportion of patients held >24 h. This is the percentage of patients who stay in the ED for more than 24 h with no physician admission disposition.
- Proportion of patients held >48 h. This indicates the percentage of patients who stay in the ED for more than 48 h with no physician admission disposition.
- Proportion of admitted patients held >24 h. This represents the percentage of patients who get admitted to the hospital and wait for more than 24 h with no available bed assigned.
- Proportion of admitted patients held >48 h. This is the percentage of patients who get admitted to the hospital and wait for more than 24 h with no available bed assigned.
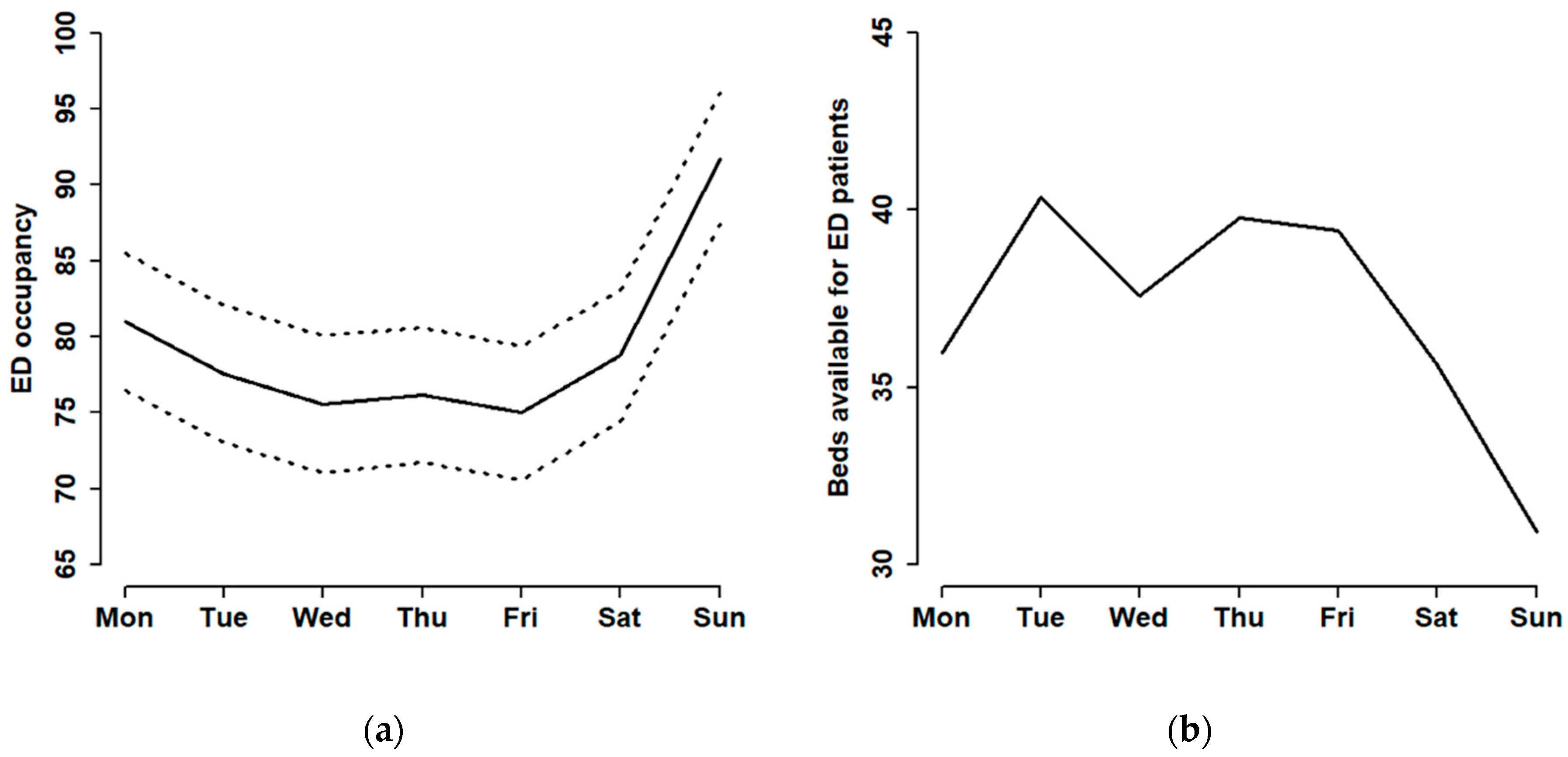
2.2. Current ED Operations
2.3. Analysis of the Strategy
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Derlet, R.W. Overcrowding in emergency departments: Increased demand and decreased capacity. Ann. Emerg. Med. 2002, 39, 430–432. [Google Scholar] [CrossRef]
- Drummond, A.J. No room at the inn: Overcrowding in Ontario’s emergency departments. Can. J. Emerg. Med. 2002, 4, 91–97. [Google Scholar] [CrossRef]
- Di Somma, S.; Paladino, L.; Vaughan, L.; Lalle, I.; Magrini, L.; Magnanti, M. Overcrowding in emergency department: An international issue. Intern. Emerg. Med. 2015, 10, 171–175. [Google Scholar] [CrossRef]
- Pines, J.M.; Griffey, R.T. What We have learned from a decade of ED crowding research. Acad. Emerg. Med. 2015, 22, 985–987. [Google Scholar] [CrossRef]
- Chang, A.M.; Cohen, D.J.; Lin, A.; Augustine, J.; Handel, D.A.; Howell, E.; Kim, H.; Pines, J.M.; Schuur, J.D.; McConnell, K.J. Hospital strategies for reducing emergency department crowding: A mixed-methods study. Ann. Emerg. Med. 2018, 71, 497–505. [Google Scholar] [CrossRef]
- Salehi, L.; Phalpher, P.; Valani, R.; Meaney, C.; Amin, Q.; Ferrari, K.; Mercuri, M. Emergency department boarding: A descriptive analysis and measurement of impact on outcomes. Can. J. Emerg. Med. 2018, 20, 929–937. [Google Scholar] [CrossRef]
- Affleck, A.; Parks, P.; Drummond, A.; Rowe, B.H.; Ovens, H.J. Emergency department overcrowding and access block. Can. J. Emerg. Med. 2013, 15, 359–370. [Google Scholar] [CrossRef]
- Asplin, B.R.; Magid, D.J.; Rhodes, K.V.; Solberg, L.I.; Lurie, N.; Camargo, C.A., Jr. A conceptual model of emergency department crowding. Ann. Emerg. Med. 2003, 42, 173–180. [Google Scholar] [CrossRef]
- Sprivulis, P.C.; Da Silva, J.; Jacobs, I.G.; Jelinek, G.A.; Frazer, A.R.L. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med. J. Aust. 2006, 184, 208–212. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. Hospital Volume Statistics; Ministry of Health and Welfare: Taiwan, China, 2017.
- Executive Yuan. The Republic of China Yearbook 2011; Government Information Office: Taiwan, China, 2011.
- Ministry of Health and Welfare. National Health Insurance Medical Quality Information Open Web; Ministry of Health and Welfare: Taiwan, China, 2018.
- Considine, J.; Kropman, M.; Kelly, E.; Winter, C. Effect of emergency department fast track on emergency department length of stay: A case–control study. Emerg. Med. J. 2008, 25, 815–819. [Google Scholar] [CrossRef]
- Australasian College for Emergency Medicine. Emergency Department Overcrowding Position Statement; Australasian College for Emergency Medicine: Melbourne, Australia, 2011. [Google Scholar]
- Asplin, B.R.; Magid, D.J. If you want to fix crowding, start by fixing your hospital. Ann. Emerg. Med. 2007, 49, 273–274. [Google Scholar] [CrossRef]
- Dawson, H.; Weerasooriya, J.; Webster, G. Hospital admissions via the emergency department: Implications for planning and patient flow. Healthc. Q. 2008, 11, 20–22. [Google Scholar] [CrossRef][Green Version]
- Forero, R.; McCarthy, S.; Hillman, K. Access block and emergency department overcrowding. Crit. Care 2011, 15, 216. [Google Scholar] [CrossRef]
- Pines, J.M.; Hilton, J.A.; Weber, E.J.; Alkemade, A.J.; Al Shabanah, H.; Anderson, P.D.; Bernhard, M.; Bertini, A.; Gries, A.; Ferrandiz, S. International perspectives on emergency department crowding. Acad. Emerg. Med. 2011, 18, 1358–1370. [Google Scholar] [CrossRef]
- Imperato, J.; Morris, D.S.; Binder, D.; Fischer, C.; Patrick, J.; Sanchez, L.D.; Setnik, G. Physician in triage improves emergency department patient throughput. Intern. Emerg. Med. 2012, 7, 457–462. [Google Scholar] [CrossRef]
- Duguay, C.; Chetouane, F. Modeling and improving emergency department systems using discrete event simulation. Simulation 2007, 83, 311–320. [Google Scholar] [CrossRef]
- Arya, R.; Wei, G.; McCoy, J.V.; Crane, J.; Ohman-Strickland, P.; Eisenstein, R.M. Decreasing length of stay in the emergency department with a split emergency severity index 3 patient flow model. Acad. Emerg. Med. 2013, 20, 1171–1179. [Google Scholar] [CrossRef]
- Rogg, J.G.; White, B.A.; Biddinger, P.D.; Chang, Y.; Brown, D.F.M. A long-term analysis of physician triage screening in the emergency department. Acad. Emerg. Med. 2013, 20, 374–380. [Google Scholar] [CrossRef]
- Russ, S.; Jones, I.; Aronsky, D.; Dittus, R.S.; Slovis, C.M. Placing physician orders at triage: The effect on length of stay. Ann. Emerg. Med. 2010, 56, 27–33. [Google Scholar] [CrossRef]
- Ng, D.; Vail, G.; Thomas, S.; Schmidt, N. Applying the Lean principles of the Toyota Production System to reduce wait times in the emergency department. Can. J. Emerg. Med. 2010, 12, 50–57. [Google Scholar] [CrossRef]
- Khare, R.K.; Powell, E.S.; Reinhardt, G.; Lucenti, M. Adding more beds to the emergency department or reducing admitted patient boarding times: Which has a more significant influence on emergency department congestion? Ann. Emerg. Med. 2009, 53, 575–585. [Google Scholar] [CrossRef]
- Chen, W.; Guo, H.; Tsui, K.-L. A new medical staff allocation via simulation optimisation for an emergency department in Hong Kong. Int. J. Prod. Res. 2019, 1–20. [Google Scholar] [CrossRef]
- Moskop, J.C.; Sklar, D.P.; Geiderman, J.M.; Schears, R.M.; Bookman, K.J. Emergency department crowding, part 2—Barriers to reform and strategies to overcome them. Ann. Emerg. Med. 2009, 53, 612–617. [Google Scholar] [CrossRef]
- Rathlev, N.K.; Chessare, J.; Olshaker, J.; Obendorfer, D.; Mehta, S.D.; Rothenhaus, T.; Crespo, S.; Magauran, B.; Davidson, K.; Shemin, R. Time series analysis of variables associated with daily mean emergency department length of stay. Ann. Emerg. Med. 2007, 49, 265–271. [Google Scholar] [CrossRef]
- Dunn, R. Reduced access block causes shorter emergency department waiting times: An historical control observational study. Emerg. Med. 2003, 15, 232–238. [Google Scholar] [CrossRef]
- Forster, A.J.; Stiell, I.; Wells, G.; Lee, A.J.; Van Walraven, C. The effect of hospital occupancy on emergency department length of stay and patient disposition. Acad. Emerg. Med. 2003, 10, 127–133. [Google Scholar] [CrossRef]
- Jun, J.B.; Jacobson, S.H.; Swisher, J.R. Application of discrete-event simulation in health care clinics: A survey. J. Oper. Res. Soc. 1999, 50, 109–123. [Google Scholar] [CrossRef]
- Yurtkuran, A.; Emel, E. Simulation based decision-making for hospital pharmacy management. In Proceedings of the 2008 Winter Simulation Conference, Miami, FL, USA, 7–10 December 2008; pp. 1539–1546. [Google Scholar]
- Oakley, D.; Onggo, B.S.; Worthington, D. Symbiotic simulation for the operational management of inpatient beds: Model development and validation using Δ-method. Health Care Manag. Sci. 2020, 23, 153–169. [Google Scholar] [CrossRef]
- Devapriya, P.; Strömblad, C.T.B.; Bailey, M.D.; Frazier, S.; Bulger, J.; Kemberling, S.T.; Wood, K.E. StratBAM: A discrete-event simulation model to support strategic hospital bed capacity decisions. J. Med. Syst. 2015, 39, 130. [Google Scholar] [CrossRef]
- Bair, A.E.; Song, W.T.; Chen, Y.-C.; Morris, B.A. The impact of inpatient boarding on ED efficiency: A discrete-event simulation study. J. Med. Syst. 2010, 34, 919–929. [Google Scholar] [CrossRef]
- Hoot, N.R.; LeBlanc, L.J.; Jones, I.; Levin, S.R.; Zhou, C.; Gadd, C.S.; Aronsky, D. Forecasting emergency department crowding: A discrete event simulation. Ann. Emerg. Med. 2008, 52, 116–125. [Google Scholar] [CrossRef]
- Zhu, Z.; Hoon Hen, B.; Liang Teow, K. Estimating ICU bed capacity using discrete event simulation. Int. J. Health Care Qual. Assur. 2012, 25, 134–144. [Google Scholar] [CrossRef]
- Hilmola, O.-P.; Henttu, V. Transportation costs do matter: Simulation study from hospital investment decision. J. Model. Manag. 2016, 11, 560–584. [Google Scholar] [CrossRef]
- Barjis, J.; Verbraeck, A.; Shim, S.J.; Kumar, A. Simulation for emergency care process reengineering in hospitals. Bus. Process Manag. J. 2010, 16, 795–805. [Google Scholar]
- Isfahani, M.N.; Davari, F.; Azizkhani, R.; Rezvani, M. Decreased emergency department overcrowding by discharge lounge: A computer simulation study. Int. J. Prev. Med. 2020, 11, 13. [Google Scholar]
- Gul, M.; Guneri, A.F. A comprehensive review of emergency department simulation applications for normal and disaster conditions. Comput. Ind. Eng. 2015, 83, 327–344. [Google Scholar] [CrossRef]
- Moreno-Carrillo, A.; Arenas, L.M.Á.; Fonseca, J.A.; Caicedo, C.A.; Tovar, S.V.; Muñoz-Velandia, O.M. Application of queuing theory to optimize the triage process in a tertiary emergency care (“ER”) department. J. Emerg. Trauma Shock 2019, 12, 268–273. [Google Scholar]
- Zhang, A.; Zhu, X.; Lu, Q.; Zhang, R. Impact of prioritization on the outpatient queuing system in the emergency department with limited medical resources. Symmetry 2019, 11, 796. [Google Scholar] [CrossRef]
- Bandi, C.; Trichakis, N.; Vayanos, P. Robust multiclass queuing theory for wait time estimation in resource allocation systems. Manag. Sci. 2019, 65, 152–187. [Google Scholar] [CrossRef]

| Scenario | Weekdays | Weekends (Adjusted to Maintain the Same Total Number on a Weekly Basis) |
|---|---|---|
| S1 | 32.49 (average) | 28.07 |
| S2 | 30.93 (−5%) | 31.97 |
| S3 | 29.37 (−10%) | 35.87 |
| S4 | 27.80 (−15%) | 39.78 |
| S5 | 26.24 (−20%) | 43.68 |
| S6 | 23.12 (−30%) | 51.48 |
| Scenario | Mean | Std a | Smoothing Effects b |
|---|---|---|---|
| Original | 79.40 | 5.82 | baseline |
| S1 (average) | 78.77 | 5.26 | 9.62% |
| S2 (−5%) | 78.23 | 5.12 | 12.03% |
| S3 (−10%) | 84.91 | 4.16 | 28.52% |
| S4 (−15%) | 88.26 | 3.42 | 41.24% |
| S5 (−20%) | 77.42 | 3.71 | 36.25% |
| S6 (−30%) | 83.33 | 5.14 | 11.68% |
| Strategy | ED Patients Held >24 h | ED Patients Held >48 h | Admitted ED Patients Held >24 h | Admitted ED Patients Held >48 h |
|---|---|---|---|---|
| Original | 8.44 | 4.86 | 30.12 | 17.32 |
| S1 (average) | 8.63 | 4.83 | 30.79 | 17.22 |
| S2 (−5%) | 8.58 | 4.79 | 30.60 | 17.08 |
| S3 (−10%) | 10.12 | 6.00 | 36.11 | 21.43 |
| S4 (−15%) | 10.40 | 6.18 | 37.15 | 22.07 |
| S5 (−20%) | 8.80 | 4.90 | 31.37 | 17.58 |
| S6 (−30%) | 10.07 | 5.41 | 35.90 | 19.31 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, J.C.-H.; Weng, S.-J.; Liu, S.-C.; Tsai, Y.-T.; Gotcher, D.F.; Chen, C.-H.; Chou, C.-A.; Kim, S.-H. Adjusting Daily Inpatient Bed Allocation to Smooth Emergency Department Occupancy Variation. Healthcare 2020, 8, 78. https://doi.org/10.3390/healthcare8020078
Tsai JC-H, Weng S-J, Liu S-C, Tsai Y-T, Gotcher DF, Chen C-H, Chou C-A, Kim S-H. Adjusting Daily Inpatient Bed Allocation to Smooth Emergency Department Occupancy Variation. Healthcare. 2020; 8(2):78. https://doi.org/10.3390/healthcare8020078
Chicago/Turabian StyleTsai, Jeffrey Che-Hung, Shao-Jen Weng, Shih-Chia Liu, Yao-Te Tsai, Donald F. Gotcher, Chih-Hao Chen, Chun-An Chou, and Seung-Hwan Kim. 2020. "Adjusting Daily Inpatient Bed Allocation to Smooth Emergency Department Occupancy Variation" Healthcare 8, no. 2: 78. https://doi.org/10.3390/healthcare8020078
APA StyleTsai, J. C.-H., Weng, S.-J., Liu, S.-C., Tsai, Y.-T., Gotcher, D. F., Chen, C.-H., Chou, C.-A., & Kim, S.-H. (2020). Adjusting Daily Inpatient Bed Allocation to Smooth Emergency Department Occupancy Variation. Healthcare, 8(2), 78. https://doi.org/10.3390/healthcare8020078





