Does the “Morning Morality Effect” Apply to Prehospital Anaesthesiologists? An Investigation into Diurnal Changes in Ethical Behaviour
Abstract
:1. Introduction
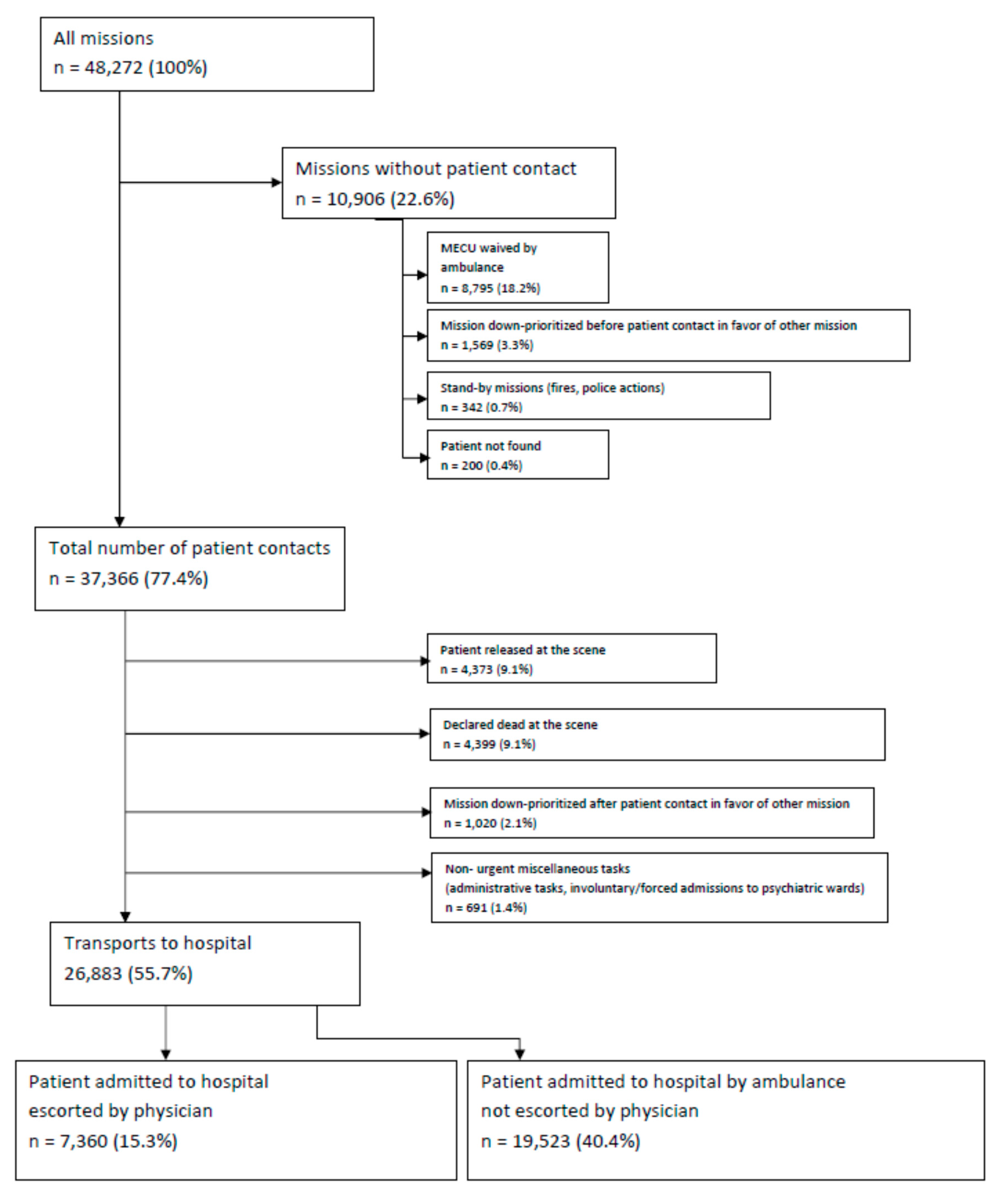
2. Methods
2.1. Study Setting and Population
2.2. Study Design
2.3. Statistical Analyses
2.4. Legislative Approval of the Study
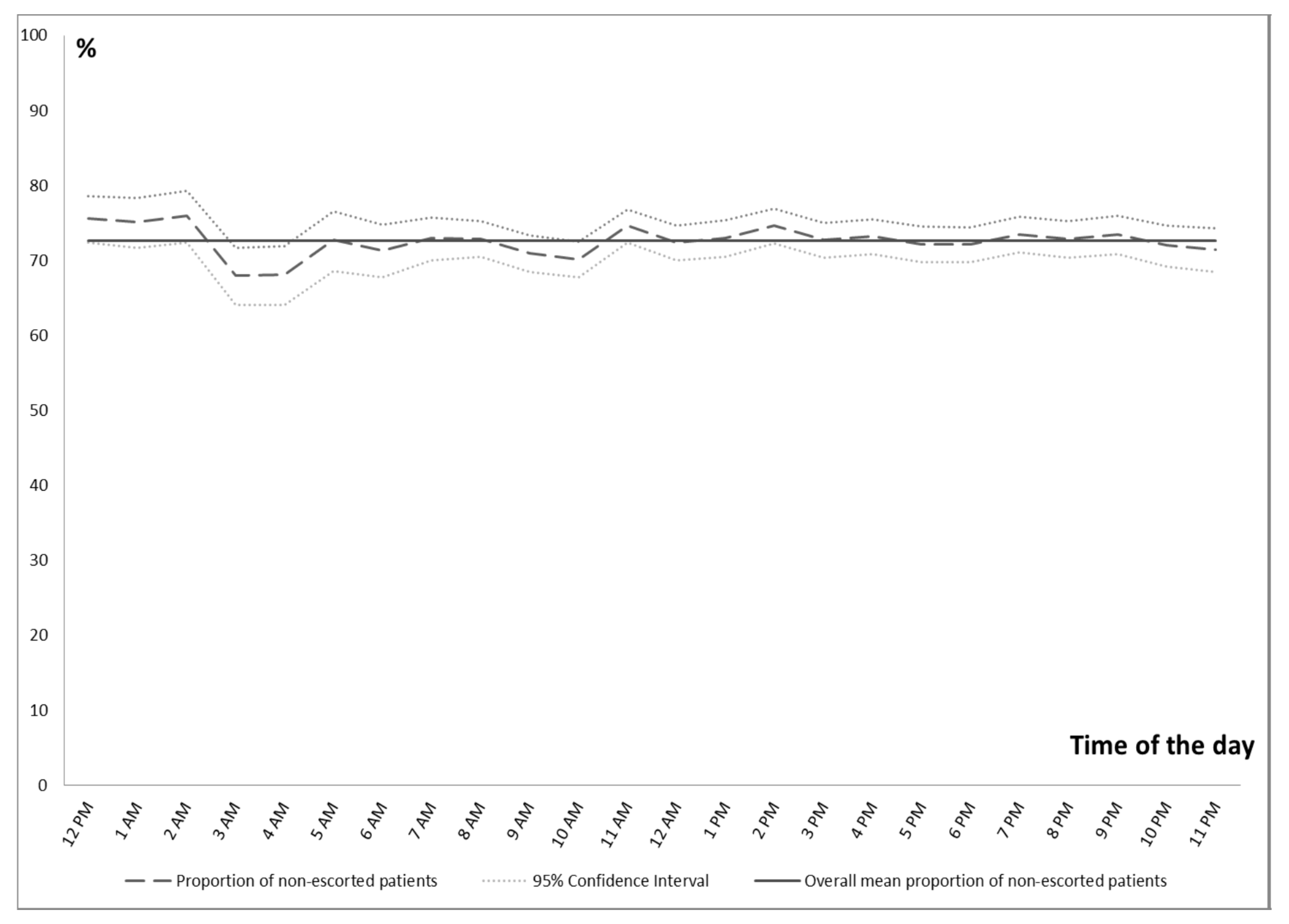
3. Results
4. Discussion
4.1. Strengths of the Study
4.2. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kouchaki, M.; Smith, I.H. The morning morality effect: The influence of time of day on unethical behavior. Psychol. Sci. 2014, 25, 95–102. [Google Scholar] [CrossRef]
- Danziger, S.; Levav, J.; Avnaim-Pesso, L. Extraneous factors in judicial decisions. Proc. Natl. Acad. Sci. USA 2011, 108, 6889–6892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haidt, J. The emotional dog and its rational tail: A social intuitionist approach to moral judgment. Psychol. Rev. 2001, 108, 814–834. [Google Scholar] [CrossRef] [PubMed]
- Schnall, S.; Haidt, J.; Clore, G.L.; Jordan, A.H. Disgust as embodied moral judgment. Personal. Soc. Psychol. Bull. 2008, 34, 1096–1109. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.R.; Eastman, C.I. Shift work: Health, performance and safety problems, traditional countermeasures, and innovative management strategies to reduce circadian misalignment. Nat. Sci. Sleep 2012, 4, 111–132. [Google Scholar]
- Andersen, M.S.; Johnsen, S.P.; Sorensen, J.N.; Jepsen, S.B.; Hansen, J.B.; Christensen, E.F. Implementing a nationwide criteria-based emergency medical dispatch system: A register-based follow-up study. Scand. J. Trauma Resusc. Emerg. Med. 2013, 21, 53. [Google Scholar] [CrossRef] [Green Version]
- Mikkelsen, S.; de Muckadell, C.S.; Binderup, L.G.; Lossius, H.M.; Toft, P.; Lassen, A.T. Termination of prehospital resuscitative efforts: A study of documentation on ethical considerations at the scene. Scand. J. Trauma Resusc. Emerg. Med. 2017, 25, 35. [Google Scholar] [CrossRef] [Green Version]
- Mikkelsen, S.; Lossius, H.M.; Toft, P.; Lassen, A.T. Characteristics and prognoses of patients treated by an anaesthesiologist-manned prehospital emergency care unit. A retrospective cohort study. BMJ Open 2017, 7, e014383. [Google Scholar] [CrossRef]
- Raatiniemi, L.; Mikkelsen, K.; Fredriksen, K.; Wisborg, T. Do pre-hospital anaesthesiologists reliably predict mortality using the NACA severity score? A retrospective cohort study. Acta Anaesthesiol. Scand. 2013, 57, 1253–1259. [Google Scholar] [CrossRef]
- WHO. International Statistical Classification of Diseases and Related Health Problems 10th Revision. Available online: http://apps.who.int/classifications/icd10/browse/2016/en (accessed on 20 January 2020).
- Hippocrates of Cos (1923). The Oath. In Loeb Classical Library; Loeb Classic Library 147; Harvard University Press: Cambridge, MA, USA, 2018; pp. 298–299. Available online: https://www.loebclassics.com/view/hippocrates_cos-oath/1923/pb_LCL147.301.xml (accessed on 4 September 2019).
- Imran, M.; Samad, S.; Maaz, M.; Qadeer, A.; Najmi, A.K.; Aqil, M. Hippocratic oath and conversion of ethico-regulatory aspects onto doctors as a physician, private individual and a clinical investigator. J. Midlife Health 2013, 4, 203–209. [Google Scholar] [CrossRef]
- Hurwitz, B.; Vass, A. What’s a good doctor, and how can you make one? BMJ 2002, 325, 667–668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chapman, E.N.; Kaatz, A.; Carnes, M. Physicians and implicit bias: How doctors may unwittingly perpetuate health care disparities. J. Gen. Intern. Med. 2013, 28, 1504–1510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- FitzGerald, C.; Hurst, S. Implicit bias in healthcare professionals: A systematic review. BMC Med. Ethics 2017, 18, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robertson, C.; Rose, S.; Kesselheim, A.S. Effect of financial relationships on the behaviors of health care professionals: A Review of the Evidence. J. Law Med. Ethics 2012, 40, 452–466. [Google Scholar] [CrossRef]
- Sah, S. Conflicts of interest and your physician: Psychological processes that cause unexpected changes in behavior. J. Law Med. Ethics 2012, 40, 482–487. [Google Scholar] [CrossRef]
- Kochan, C.A.; Budd, J.M. The persistence of fraud in the literature: The Darsee case. J. Am. Soc. Inf. Sci. 1992, 43, 488–493. [Google Scholar] [CrossRef]
- White, P.F.; Rosow, C.E.; Shafer, S.L. Editorial Board of Anesthesia & Analgesia. The Scott Reuben saga: One last retraction. Anesth. Analg. 2011, 112, 512–515. [Google Scholar]
- Significant Indication of Fraud in Penkowas Early Research. News, University of Copenhagen. Available online: http://news.ku.dk/all_news/2012/2012.8/indications_of_fraud_in_penkowas_early_research/ (accessed on 4 September 2019).
- Chretien, K.C.; Tuck, M.G. Online professionalism: A synthetic review. Int. Rev. Psychiatry 2015, 27, 106–117. [Google Scholar] [CrossRef]
- Askitopoulou, H.; Vgontzas, A.N. The relevance of the Hippocratic Oath to the ethical and moral values of contemporary medicine. Part I: The Hippocratic Oath from antiquity to modern times. Eur. Spine J. 2018, 27, 1481–1490. [Google Scholar] [CrossRef]
- Askitopoulou, H.; Vgontzas, A.N. The relevance of the Hippocratic Oath to the ethical and moral values of contemporary medicine. Part II: Interpretation of the Hippocratic Oath-today’s perspective. Eur Spine J. 2018, 27, 1491–1500. [Google Scholar] [CrossRef]
- Gillon, R. Medical ethics: Four principles plus attention to scope. BMJ 1994, 309, 184–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, R. All doctors are problem doctors. BMJ 1997, 314, 841–842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ebrahimian, A.; Seyedin, H.; Jamshidi-Orak, R.; Masoumi, G. Exploring factors affecting emergency medical services staffs’ decision about transporting medical patients to medical facilities. Emerg. Med. Int. 2014, 2014, 215329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brandling, J.; Kirby, K.; Black, S.; Voss, S.; Benger, J. Emergency medical service provider decision-making in out of hospital cardiac arrest: An exploratory study. BMC Emerg. Med. 2017, 17, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Montassier, E.; Labady, J.; Andre, A.; Potel, G.; Berthier, F.; Jenvrin, J.; Penverne, Y. The effect of work shift configurations on emergency medical dispatch center response. Prehosp. Emerg. Care 2015, 19, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Kelz, R.; Freeman, K.M.; Hosokawa, P.W.; Asch, D.A.; Spitz, F.R.; Moskowitz, M.; Henderson, W.G.; Mitchell, M.E.; Itani, K.M.F. Time of day is associated with postoperative morbidity: An analysis of the national surgical quality improvement program data. Ann. Surg. 2008, 247, 544–552. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, G.; Chen, Q.; Li, L. Depletion, moral identity, and unethical behavior: Why people behave unethically after self-control exertion. Conscious. Cogn. 2017, 56, 188–198. [Google Scholar] [CrossRef]
- Baumeister, R.F.; Bratslavsky, E.; Muraven, M.; Tice, D.M. Ego depletion: Is the active self a limited resource? J. Personal. Soc. Psychol. 1998, 74, 1252–1265. [Google Scholar] [CrossRef]
- Muraven, M.; Baumeister, R.F. Self-regulation and depletion of limited resources: Does self-control resemble a muscle? Psychol. Bull. 2000, 126, 247–259. [Google Scholar] [CrossRef]
- Mead, N.L.; Baumeister, R.F.; Gino, F.; Schweitzer, M.E.; Ariely, D. Too tired to tell the truth: Self-control resource depletion and dishonesty. J. Exp. Soc. Psychol. 2009, 45, 594–597. [Google Scholar] [CrossRef] [Green Version]
- Truglio-Londrigan, M.; Slyer, J.T.; Singleton, J.K.; Worral, P. A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. JBI Libr. Syst. Rev. 2012, 10, 4633–4646. [Google Scholar] [CrossRef] [PubMed]
- Surowiecki, J. The Wisdom of Crowds; First Anchor Books: New York, NY, USA, 2005; ISBN 978-0-385-72170-6. [Google Scholar]
- Lee, M.D.; Steyvers, M.; Miller, B. A cognitive model for aggregating people’s rankings. PLoS ONE 2014, 9, e96431. [Google Scholar] [CrossRef] [PubMed]
- Akerstedt, T.; Wright, K. Sleep loss and fatigue in shift work and shift work disorder. Sleep Med. Clin. 2009, 4, 257–271. [Google Scholar] [CrossRef] [Green Version]
- Barger, L.K.; Lockley, S.W.; Rajaratnam, S.M.; Landrigan, C.P. Neurobehavioural, health, and safety consequences associated with shift work in safety-sensitive professions. Curr. Neurol. Neurosci. Rep. 2009, 9, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Holden, J.D. Hawthorne effects and research into professional practice. J. Eval. Clin. Pract. 2001, 7, 65–70. [Google Scholar] [CrossRef]
- Gunia, B.C.; Barnes, C.M.; Sah, S. The morality of larks and owls: Unethical behavior depends on chronotype as well as time of day. Psychol. Sci. 2014, 25, 2272–2274. [Google Scholar] [CrossRef]
- Christensen, E.F.; Bendtsen, M.D.; Larsen, T.M.; Jensen, F.B.; Lindskou, T.A.; Holdgaard, H.O.; Hansen, P.A.; Johnsen, S.P.; Christiansen, C.F. Trends in diagnostic patterns and mortality in emergency ambulance service patients in 2007–2014: A population-based cohort study from the North Denmark Region. BMJ Open 2017, 7, e014508. [Google Scholar] [CrossRef]
- Boivin, D.B.; Boudreau, P. Impacts of shift work on sleep and circadian rhythms. Pathol. Biol. (Paris) 2014, 62, 292–301. [Google Scholar] [CrossRef]
| Year | Transported to Hospital with Escort n (%(95%CI)) | Transported to Hospital without Escort n (%(95%CI)) | Total no. of Patients Transported to Hospital |
|---|---|---|---|
| 2007 (4th quarter) | 229 (27.9 (24.8–31.1)) | 593 (72.1 (68.9–75.2)) | 822 |
| 2008 | 725 (22.9 (21.5–24.4)) | 2439 (77.1 (75.6–78.5)) | 3164 |
| 2009 | 683 (22.0 (20.6–23.5)) | 2416 (78.0 (76.5–79.4)) | 3099 |
| 2010 | 619 (22.3 (20.8–23.9)) | 2151 (76.7 (76.1–79.2)) | 2770 |
| 2011 | 639 (24.0 (22.4–25.7)) | 2021 (76.0 (74.3–77.6)) | 2660 |
| 2012 | 596 (23.2 (21.6–24.9)) | 1974 (76.8 (75.1–78.4)) | 2570 |
| 2013 | 598 (25.5 (23.7–27.3)) | 1750 (74.5 (72.7–76.3)) | 2348 |
| 2014 | 685 (29.5 (27.7–31.4)) | 1635 (70.5 (68.6–72.3)) | 2320 |
| 2015 | 664 (34.6 (32.4–36.7)) | 1257 (65.4 (63.3–67.6)) | 1921 |
| 2016 | 628 (34.9 (32.7–37.1)) | 1173 (65.1 (62.9–67.3)) | 1801 |
| 2017 | 610 (38.3 (35.9–40.7)) | 983 (61.7 (59.3–64.1)) | 1593 |
| 2018 | 684 (37.7 (35.5–40.0)) | 1131 (62.3 (60.0–64.5)) | 1815 |
| Day | Evening | Night | p–Value | |
|---|---|---|---|---|
| Escorted by physician | 3077 | 2811 | 1468 | 1.00 |
| Unescorted by physician | 8164 | 7443 | 3900 |
| Time Interval | Total Number of Patients Admitted to Hospital | Patients Admitted to Hospital without Physician Escort (n (% (95%CI)) |
|---|---|---|
| 12:00 a.m.–0:59 a.m. | 806 | 609 (75.5 (72.4–78.5)) |
| 1:00 a.m.–1:59 a.m. | 661 | 496 (75.0 (71.6–78.3)) |
| 2:00 a.m.–2:59 a.m. | 612 | 465 (75.9 (72.4–79.3)) |
| 3:00 a.m.–3:59 a.m. | 583 | 396 (67.9 (64.0–71.7)) |
| 4:00 a.m.–4:59 a.m. | 551 | 375 (68.1 (64.0–71.9)) |
| 5:00 a.m.–5:59 a.m. | 501 | 364 (72.7 (68.5–76.5)) |
| 6:00 a.m.–6:59 a.m. | 672 | 479 (71.3 (67.7–74.7)) |
| 7:00 a.m.–7:59 a.m. | 982 | 716 (72.9 (70.0–75.7)) |
| 8:00 a.m.–8:59 a.m. | 1345 | 980 (72.9 (70.4–75.2)) |
| 9:00 a.m.–9:59 a.m. | 1370 | 971 (70.9 (68.4–73.3)) |
| 10:00 a.m.–10:59 a.m. | 1439 | 1009 (70.1 (67.7–72.5)) |
| 11:00 a.m.–11:59 a.m. | 1450 | 1082 (74.6 (72.3–76.8)) |
| 12:00 p.m.–0:59 p.m. | 1473 | 1066 (72.4 (70.0–74.6)) |
| 1:00 p.m.–1:59 p.m. | 1358 | 991 (73.0 (70.5–75.3)) |
| 2:00 p.m.–2:59 p.m. | 1360 | 1014 (74.6 (72.2–76.9)) |
| 3:00 p.m.–3:59 p.m. | 1446 | 1051 (72.7 (70.3–75.0)) |
| 4:00 p.m.–4:59 p.m. | 1459 | 1067 (73.1 (70.8–75.4)) |
| 5:00 p.m.–5:59 p.m. | 1381 | 996 (72.1 (69.7–74.5)) |
| 6:00 p.m.–6:59 p.m. | 1469 | 1059 (72.1 (69.7–74.4)) |
| 7:00 p.m.–7:59 p.m. | 1351 | 992 (73.4 (71.0–75.8)) |
| 8:00 p.m.–8:59 p.m. | 1327 | 966 (72.8 (70.3–75.2)) |
| 9:00 p.m.–9:59 p.m. | 1197 | 879 (73.4 (70.8–75.9)) |
| 10:00 p.m.–10:59 p.m. | 1127 | 811 (72.0 (69.2–74.6)) |
| 11:00 p.m.–11:59 p.m. | 943 | 673 (71.4 (68.4–74.2)) |
| Total | 26,863 | 19,507 (72.6 (72.1–73.1)) |
| Characteristics | Odds Ratio | 95% CI | p-Value |
|---|---|---|---|
| Day of week | |||
| Sat.–Sun. | 1 (Reference) | ||
| Mon.–Fri. | 1.02 | 0.96–1.08 | 0.61 |
| Time of day | |||
| 08:00 a.m.–15:59 p.m. | 1 (Reference) | ||
| 16:00 p.m.–23:59 p.m. | 1.00 | 0.94–1.06 | 0.94 |
| 00:00 a.m.–07:59 a.m. | 1.00 | 0.93–1.08 | 0.99 |
| ICD-10 Chapter | Diagnosis Group | Patients (Total) | Patients Escorted to Hospital by Physician (Proportion of Subgroup) | Patients not Escorted to Hospital by Physician (Proportion of Subgroup) | ||
|---|---|---|---|---|---|---|
| (n) | (% (95% CI)) | (n) | (% (95% CI)) | |||
| Chapter I | Certain infectious and parasitic diseases (A00–B99) | 284 | 147 | 51.8 (45.8–57.7) | 137 | 48.2 (42.3–54.2) |
| Chapter II | Neoplasms (C00–D48) | |||||
| Chapter III | Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism (D50–D89) | |||||
| Chapter IV | Endocrine, nutritional and metabolic diseases (E00–E90) | 413 | 61 | 14.8 (11.5–18.6) | 352 | 85.2 (81.4–88.5) |
| Chapter V | Mental and behavioural disorders (F00–F99) | 533 | 74 | 13.9 (11.1–17.1) | 459 | 86.1 (82.9–88.9) |
| Chapter VI | Diseases of the nervous system (G00–G99) | 658 | 168 | 25.5 (22.2–29.0) | 490 | 74.5 (71.0–77.7) |
| Chapter VII | Diseases of the eye and adnexa (H00–H59) | |||||
| Chapter VIII | Diseases of the ear and mastoid process (H60–H95) | |||||
| Chapter IX | Diseases of the circulatory system (I00–I99) | 5245 | 2252 | 42.9 (41.6–44.3) | 2993 | 57.1 (55.7–58.4) |
| Chapter X | Diseases of the respiratory system (J00–J99) | 3129 | 997 | 31.9 (30.2–33.5) | 2132 | 68.1 (66.5–69.8) |
| Chapter XI | Diseases of the digestive system (K00–K93) | 354 | 92 | 26.0 (21.5–30.9) | 262 | 74.0 (69.1–78.5) |
| Chapter XII | Diseases of the skin and subcutaneous tissue (L00–L99) | |||||
| Chapter XIII | Diseases of the musculoskeletal system and connective tissue (M00–M99) | 133 | 2 | 1.5 (0.2–5.3) | 131 | 98.5 (94.7–99.8) |
| Chapter XIV | Diseases of the genitourinary system (N00–N99) | 83 | 11 | 13.3 (6.8–22.5) | 72 | 86.7 (77.5–93.2) |
| Chapter XV | Pregnancy, childbirth and the puerperium (O00–O99) | 91 | 34 | 37.4 (27.4–48.1) | 57 | 62.6 (31.9–72.6) |
| Chapter XVI | Certain conditions originating in the perinatal period (P00–P96) | 11 | 2 | 18.1 (2.3–51.8) | 9 | 81.8 (48.2–97.7) |
| Chapter XVII | Congenital malformations, deformations and chromosomal abnormalities (Q00–Q99) | |||||
| Chapter XVIII | Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R00–R99) | 4937 | 978 | 19.8 (18.7–20.9) | 3959 | 80.2 (79.1–81.3) |
| Chapter XIX | Injury, poisoning and certain other consequences of external causes (S00–T98) | 4042 | 1397 | 34.6 (33.1–36.1) | 2645 | 65.4 (63.9–66.9) |
| Chapter XX | External causes of morbidity and mortality (V01–Y98) | |||||
| Chapter XXI | Factors influencing health status and contact with health services (Z00–Z99) | 6851 | 1122 | 16.4 (15.5–17.3) | 5729 | 83.6 (82.7–84.5) |
| Chapter XXII | Codes for special purposes (U00–U85) | |||||
| Missing | 109 | 20 | 18.3 (11.6–26.9) | 89 | 81.7 (73.1–88.4) | |
| Total | 26,883 | 7360 | 27.4 (26.9–27.9) | 19,523 | 72.3 (72.1–73.2) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brøchner, A.C.; Binderup, L.G.; Schaffalitzky de Muckadell, C.; Mikkelsen, S. Does the “Morning Morality Effect” Apply to Prehospital Anaesthesiologists? An Investigation into Diurnal Changes in Ethical Behaviour. Healthcare 2020, 8, 101. https://doi.org/10.3390/healthcare8020101
Brøchner AC, Binderup LG, Schaffalitzky de Muckadell C, Mikkelsen S. Does the “Morning Morality Effect” Apply to Prehospital Anaesthesiologists? An Investigation into Diurnal Changes in Ethical Behaviour. Healthcare. 2020; 8(2):101. https://doi.org/10.3390/healthcare8020101
Chicago/Turabian StyleBrøchner, Anne Craveiro, Lars Grassmé Binderup, Caroline Schaffalitzky de Muckadell, and Søren Mikkelsen. 2020. "Does the “Morning Morality Effect” Apply to Prehospital Anaesthesiologists? An Investigation into Diurnal Changes in Ethical Behaviour" Healthcare 8, no. 2: 101. https://doi.org/10.3390/healthcare8020101
APA StyleBrøchner, A. C., Binderup, L. G., Schaffalitzky de Muckadell, C., & Mikkelsen, S. (2020). Does the “Morning Morality Effect” Apply to Prehospital Anaesthesiologists? An Investigation into Diurnal Changes in Ethical Behaviour. Healthcare, 8(2), 101. https://doi.org/10.3390/healthcare8020101






