Self-Management of Hip Osteoarthritis Five Years After a Cycling and Education Treatment Pathway
Abstract
:1. Introduction
The Cycling against Hip Pain (CHAIN) Programme
2. Materials and Methods
2.1. Ethical Considerations
2.2. Data Collection
2.3. Data Analysis
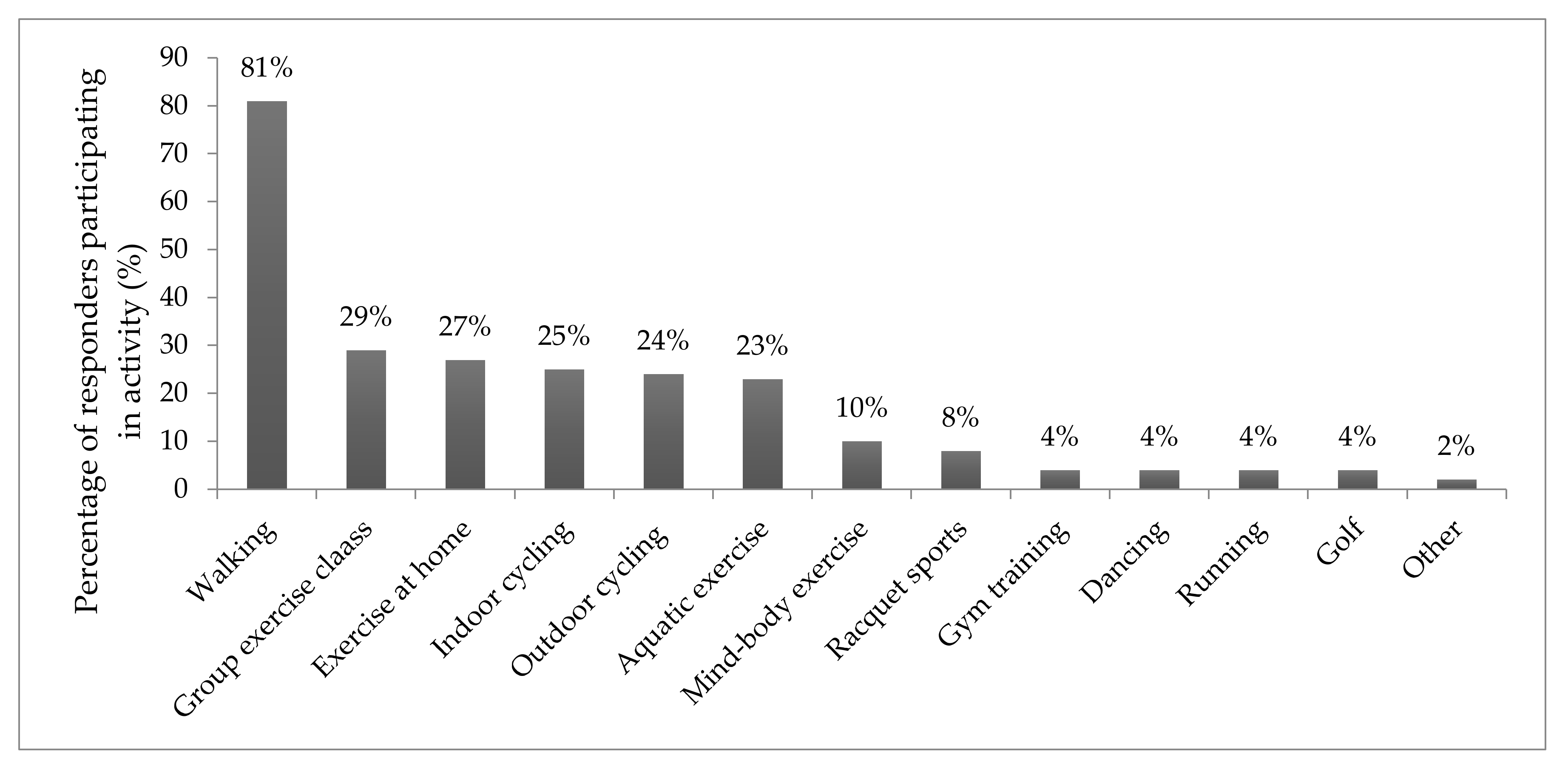
3. Results
Treatment for Hip Pain
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Cross, M.; Smith, E.; Hoy, D.; Nolte, S.; Ackerman, I.; Fransen, M.; Bridgett, L.; Williams, S.; Guillemin, F.; Hill, C.L.; et al. The global burden of hip and knee osteoarthritis: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 2014, 73, 1323–1330. [Google Scholar] [CrossRef] [PubMed]
- OARSI Research Society International. Osteoarthritis: A Serious Disease; OARSI Research Society International: 2016. Available online: https://www.oarsi.org/education/oarsi-resources/oarsi-white-paper-oa-serious-disease (accessed on 11 February 2020).
- Versus Arthritis. State of Musculoskeletal Health 2018. Versus Arthritis. 2018. Available online: https://www.versusarthritis.org/about-arthritis/data-and-statistics/state-of-musculoskeletal-health-2019/ (accessed on 22 January 2020).
- Bijlsma, J.W.; Berenbaum, F.; Lafeber, F.P. Osteoarthritis: An update with relevance for clinical practice. Lancet 2011, 377, 2115–2126. [Google Scholar] [CrossRef]
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef]
- Ethgen, O.; Bruyere, O.; Richy, F.; Dardennes, C.; Reginster, J.Y. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J. Bone Joint Surg. Am. 2004, 86, 963–974. [Google Scholar] [CrossRef] [PubMed]
- Beswick, A.D.; Wylde, V.; Gooberman-Hill, R.; Blom, A.; Dieppe, P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open 2012, 2, e000435. [Google Scholar] [CrossRef]
- Konopka, J.F.; Lee, Y.Y.; Su, E.P.; McLawhorn, A.S. Quality-Adjusted Life Years After Hip and Knee Arthroplasty: Health-Related Quality of Life After 12,782 Joint Replacements. JB JS Open Access 2018, 3, e0007. [Google Scholar] [CrossRef]
- Chang, R.W.; Pellisier, J.M.; Hazen, G.B. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA 1996, 275, 858–865. [Google Scholar] [CrossRef]
- Nutt, J.L.P.K.; Kellett, C.F. (ii) Complications of total hip arthroplasty. Orthop. Trauma 2013, 22, 272–276. [Google Scholar] [CrossRef]
- Chu, C.R.; Williams, A.A.; Coyle, C.H.; Bowers, M.E. Early diagnosis to enable early treatment of pre-osteoarthritis. Arthritis Res. Ther. 2012, 14, 212. [Google Scholar] [CrossRef] [Green Version]
- Zhang, W.; Moskowitz, R.W.; Nuki, G.; Abramson, S.; Altman, R.D.; Arden, N.; Bierma-Zeinstra, S.; Brandt, K.D.; Croft, P.; Doherty, M.; et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthr. Cartil. 2008, 16, 137–162. [Google Scholar] [CrossRef] [Green Version]
- National Institute for Health and Care Excellence (NICE). Osteoarthritis: Care and Management. Available online: https://www.nice.org.uk/guidance/CG177 (accessed on 20 June 2019).
- Wainwright, T.W.; Immins, T.; Middleton, R.G. A cycling and education programme for the treatment of hip osteoarthritis: A quality improvement study. Int. J. Orthop. Trauma Nurs. 2016, 23, 14–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wainwright, T.W.; Immins, T.; Middleton, R.G. Hip osteoarthritis: Patients with complex comorbidities can make exceptional improvements following intensive exercise and education. BMJ Case Rep. 2015, 2015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fransen, M.; McConnell, S.; Harmer, A.R.; Van der Esch, M.; Simic, M.; Bennell, K.L. Exercise for osteoarthritis of the knee: A Cochrane systematic review. Br. J. Sports Med. 2015, 49, 1554–1557. [Google Scholar] [CrossRef] [PubMed]
- Skou, S.T.; Roos, E.M. Good Life with osteoArthritis in Denmark (GLA:D): Evidence-based education and supervised neuromuscular exercise delivered by certified physiotherapists nationwide. BMC Musculoskelet Disord 2017, 18, 72. [Google Scholar] [CrossRef] [Green Version]
- Hurley, M.V.; Walsh, N.E.; Mitchell, H.L.; Pimm, T.J.; Patel, A.; Williamson, E.; Jones, R.H.; Dieppe, P.A.; Reeves, B.C. Clinical effectiveness of a rehabilitation program integrating exercise, self-management, and active coping strategies for chronic knee pain: A cluster randomized trial. Arthritis Rheum. 2007, 57, 1211–1219. [Google Scholar] [CrossRef]
- Bennell, K.L.; Egerton, T.; Martin, J.; Abbott, J.H.; Metcalf, B.; McManus, F.; Sims, K.; Pua, Y.-H.; Wrigley, T.V.; Forbes, A.; et al. Effect of physical therapy on pain and function in patients with hip osteoarthritis: A randomized clinical trial. JAMA 2014, 311, 1987–1997. [Google Scholar] [CrossRef]
- Jessep, S.A.; Walsh, N.E.; Ratcliffe, J.; Hurley, M.V. Long-term clinical benefits and costs of an integrated rehabilitation programme compared with outpatient physiotherapy for chronic knee pain. Physiotherapy 2009, 95, 94–102. [Google Scholar] [CrossRef]
- National Health Research Authority. HRA Decision Tool. Available online: http://www.hra-decisiontools.org.uk/ethics/ (accessed on 21 June 2019).
- World Medical Association. WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 21 June 2019).
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S.; Altman, D.G.; Blettner, M.; Boffetta, P.; et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [Green Version]
- Strobe-Statement. Checklist of Items that Should be Included in Reports of Cross-Sectional Studies. Available online: https://www.strobe-statement.org/fileadmin/Strobe/uploads/checklists/STROBE_checklist_v4_cross-sectional.pdf (accessed on 9 October 2019).
- Kelley, K.; Clark, B.; Brown, V.; Sitzia, J. Good practice in the conduct and reporting of survey research. Int. J. Qual. Health Care 2003, 15, 261–266. [Google Scholar] [CrossRef] [Green Version]
- Boyatzis. Transforming Qualitative Information Thematic Analysis and Code Development; Sage: Thousand Oaks, CA, USA, 1998. [Google Scholar]
- Bannuru, R.R.; Osani, M.C.; Vaysbrot, E.E.; Arden, N.K.; Bennell, K.; Bierma-Zeinstra, S.M.A.; Kraus, V.B.; Lohmander, L.S.; Abbott, J.H.; Bhandari, M.; et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 2019. [Google Scholar] [CrossRef] [Green Version]
- Mathieu, S.; Couderc, M.; Tournadre, A.; Soubrier, M. Cardiovascular profile in osteoarthritis: A meta-analysis of cardiovascular events and risk factors. Joint Bone Spine 2019, 86, 679–684. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D. Physical activity is medicine for older adults. Postgrad. Med. J. 2014, 90, 26–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abbott, J.H.; Wilson, R.; Pinto, D.; Chapple, C.M.; Wright, A.A.; MOA Trial Team. Incremental clinical effectiveness and cost effectiveness of providing supervised physiotherapy in addition to usual medical care in patients with osteoarthritis of the hip or knee: 2-year results of the MOA randomised controlled trial. Osteoarthr. Cartil. 2019, 27, 424–434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hurley, M.; Dickson, K.; Hallett, R.; Grant, R.; Hauari, H.; Walsh, N.; Stansfield, C.; Oliver, S. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: A mixed methods review. Cochrane Database Syst. Rev. 2018, 4, CD010842. [Google Scholar] [CrossRef]
- Garver, M.J.; Focht, B.C.; Taylor, S.J. Integrating lifestyle approaches into osteoarthritis care. J. Multidiscip. Healthc. 2015, 8, 409–418. [Google Scholar] [CrossRef] [Green Version]
- Fincham, J.E. Response rates and responsiveness for surveys, standards, and the Journal. Am. J. Pharm. Educ. 2008, 72, 43. [Google Scholar] [CrossRef] [Green Version]
| Characteristic | Frequency (%) | |
|---|---|---|
| Gender n (%) | Male | 38 (46%) |
| Female | 45 (54%) | |
| Primary diagnosis n (%) | No diagnosis | 10 (13%) |
| Osteoarthritis | 64 (80%) | |
| Rheumatoid arthritis | 1 (1%) | |
| Post Traumatic | 1 (1%) | |
| Other | 4 (5%) | |
| Not stated | 3 (4%) | |
| Body Mass Index (BMI) n (%) | <18.5 (underweight) 18.5–24.9 (normal) | 1 (1%) 23(28%) |
| 25.0–29.9 (overweight) | 26 (31%) | |
| 30.0 and over (obese) | 20 (24%) | |
| Not stated | 13 (16%) | |
| Age mean (SD) | 62.66 (8.74) | |
| Baseline Oxford Hip score mean (SD) | 33.51 (7.81) |
| Question | Answer | Frequency (%) |
|---|---|---|
| General practitioner (GP) visit for hip pain | Yes No | 46 (55%) 37 (45%) |
| Treatment to affected hip | No treatment Total hip replacement Unilateral Bilateral Physiotherapy Intra-articular injection | 37 (45%) 36 (43%) 34 (94%) 2 (6%) 7 (8%) 3 (4%) |
| Hospital | Local NHS hospital Local private hospital Elsewhere | 27 (75%) 7 (19%) 2 (6%) |
| Year of hip replacement | 2014 2015 2016 2017 2018 2019 | 5 (14%) 8 (22%) 6 (17%) 8 (22%) 7 (19%) 2 (6%) |
| Treatment to non-affected hip | Total hip replacement Intra-articular injection Pain killers No treatment | 1 (1%) 1 (1%) 2 (2%) 79 (95%) |
| Question | Answer | Frequency (%) |
|---|---|---|
| Did undertaking the CHAIN programme increase your knowledge of self-managing your hip pain? | Yes A little No Did not answer | 68 (82%) 12 (14%) 2 (2%) 1 (1%) |
| After the programme, did you feel that you were able to self-manage your hip pain? | Yes A little No Did not answer | 54 (65%) 23 (28%) 5 (6%) 1 (1%) |
| Since completing CHAIN, have you purchased a bike? | Yes Indoor Outdoor No Already owned a bike | 24 (29%) 17 (71%) 7 (29%) 20 (24%) 39 (47%) |
| Since completing CHAIN, have you joined a gym or leisure centre? | Yes Already a member No Did not answer | 25 (30%) 10 (12%) 46 (55%) 2 (2%) |
| Are you still in contact with anyone you were on the course with? | Yes No | 4 (5%) 79 (95%) |
| Would you recommend the course to a friend? | Yes Maybe No Did not answer | 68 (82%) 7 (8%) 2 (2%) 6 (7%) |
| Would you be interested in completing the CHAIN programme again? | Yes Maybe No Did not answer | 33 (40%) 16 (19%) 27 (33%) 7 (8%) |
| Theme | Frequency (%) |
|---|---|
| Increased participation in physical activity | 20 (25) |
| Physical benefits | 14 (18) |
| Knowledge benefits | 14 (18) |
| Constraints | 11 (14) |
| Limited effects | 8 (10) |
| Suggestions for improvement | 7 (9) |
| Social benefits | 5 (6) |
| Total | 76 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wainwright, T.W.; Burgess, L.C.; Immins, T.; Middleton, R.G. Self-Management of Hip Osteoarthritis Five Years After a Cycling and Education Treatment Pathway. Healthcare 2020, 8, 37. https://doi.org/10.3390/healthcare8010037
Wainwright TW, Burgess LC, Immins T, Middleton RG. Self-Management of Hip Osteoarthritis Five Years After a Cycling and Education Treatment Pathway. Healthcare. 2020; 8(1):37. https://doi.org/10.3390/healthcare8010037
Chicago/Turabian StyleWainwright, Thomas W., Louise C. Burgess, Tikki Immins, and Robert G. Middleton. 2020. "Self-Management of Hip Osteoarthritis Five Years After a Cycling and Education Treatment Pathway" Healthcare 8, no. 1: 37. https://doi.org/10.3390/healthcare8010037
APA StyleWainwright, T. W., Burgess, L. C., Immins, T., & Middleton, R. G. (2020). Self-Management of Hip Osteoarthritis Five Years After a Cycling and Education Treatment Pathway. Healthcare, 8(1), 37. https://doi.org/10.3390/healthcare8010037






