Rural Resident Experience on National Basic Public Health Services: A Cross-Sectional Survey in 10 Western Provinces of China
Abstract
1. Introduction
2. Materials and Methods
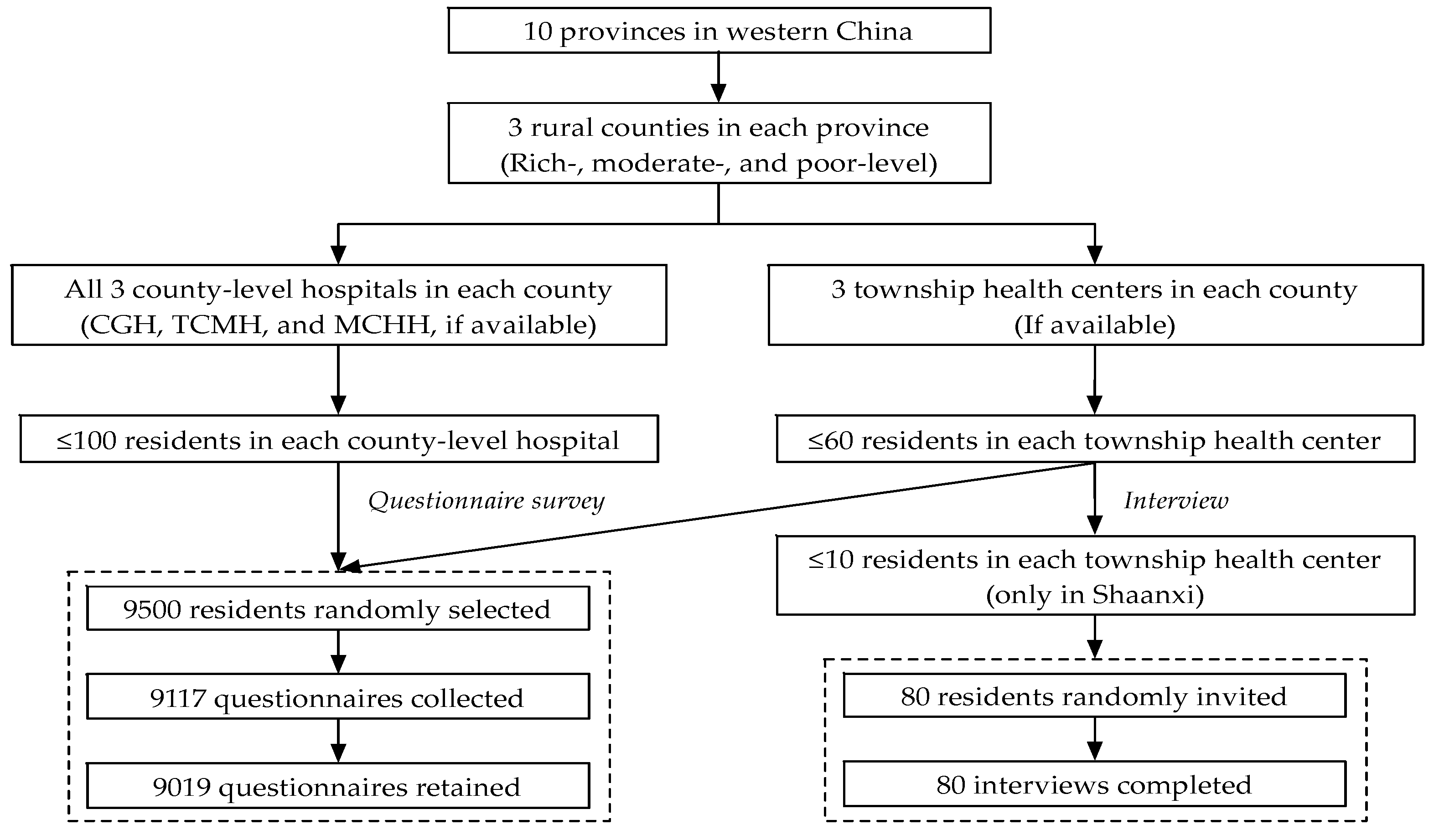
2.1. Study Design and Participants
2.2. Data Collection and Variables Measurement
2.3. Statistical Methods
2.4. Charactersitics of Participants
2.5. Ethics
3. Results
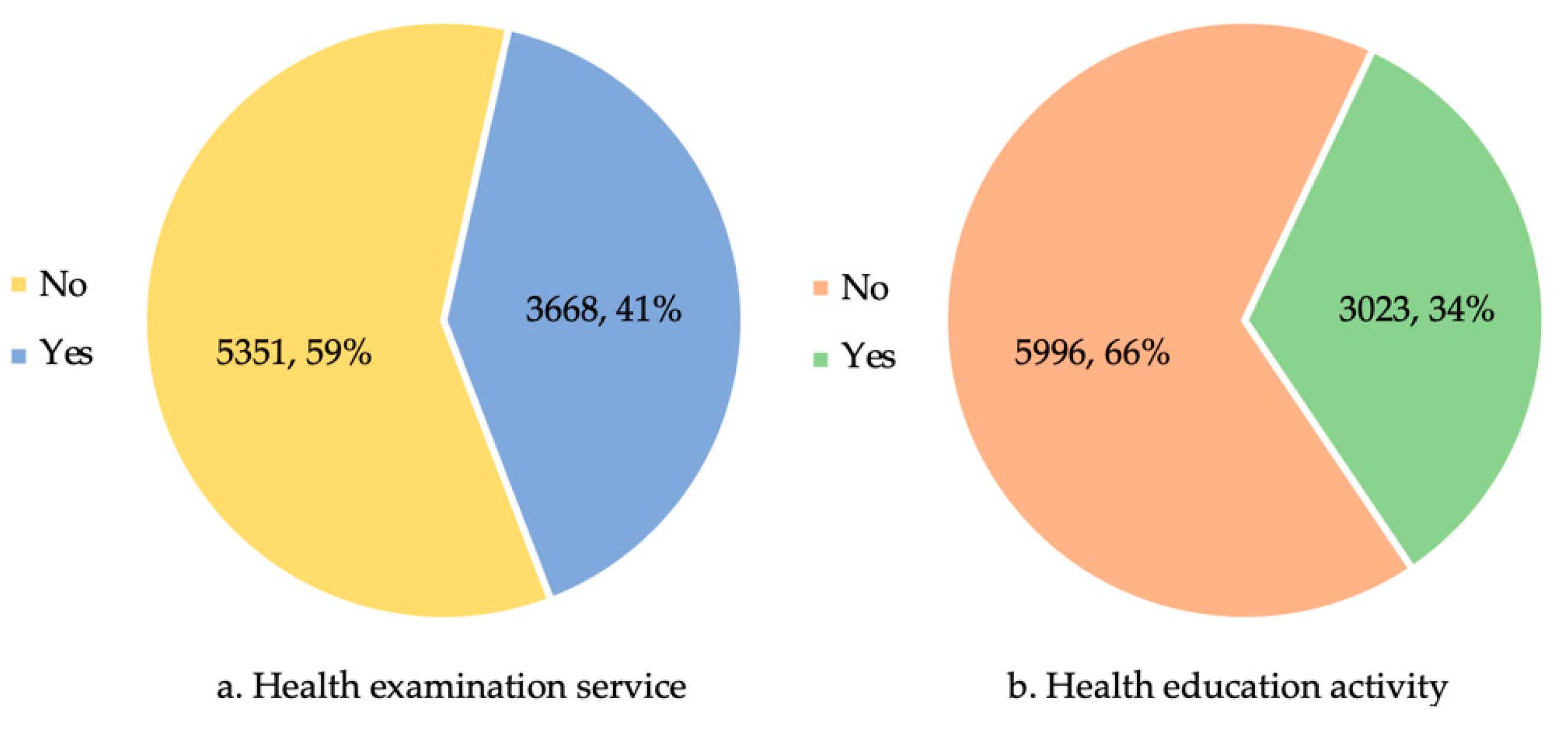
3.1. Resident Experience on Rural Basic Public Health Services
3.2. Influencing Factors of Residents’ Overall Satisfaction with Rural Basic Public Health Services
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization; The United Nations Children’s Fund. A Vision for Primary Health Care in the 21st Century: Towards Universal Health Coverage and the Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Chen, Z. Launch of the health-care reform plan in China. Lancet 2009, 373, 1322–1324. [Google Scholar] [CrossRef]
- The World Bank; World Health Organization. Healthy China: Deepening Health Reform in China; International Bank for Reconstruction and Development; The World Bank and World Health Organization: Washington, DC, USA, 2019. [Google Scholar]
- Yip, W.C.-M.; Hsiao, W.C.; Chen, W.; Hu, S.; Ma, J.; Maynard, A. Early appraisal of China’s huge and complex health-care reforms. Lancet 2012, 379, 833–842. [Google Scholar] [CrossRef]
- Yip, W.; Fu, H.; Chen, A.T.; Zhai, T.; Jian, W.; Xu, R.; Pan, J.; Hu, M.; Zhou, Z.; Chen, Q.; et al. 10 years of health-care reform in China: Progress and gaps in Universal Health Coverage. Lancet 2019, 394, 1192–1204. [Google Scholar] [CrossRef]
- Yuan, B.; Balabanova, D.; Gao, J.; Tang, S.; Guo, Y. Strengthening public health services to achieve universal health coverage in China. BMJ 2019, 365, l2358. [Google Scholar] [CrossRef] [PubMed]
- National Health Commission of China; Ministry of Finance of China; National Administration of Traditional Chinese Medicine of China. Notice on Implementing the Basic Public Health Service Project in 2019. Available online: http://www.gov.cn/xinwen/2019-09/05/content_5427467.htm (accessed on 11 November 2019).
- Li, X.; Lu, J.; Hu, S.; Cheng, K.; De Maeseneer, J.; Meng, Q.; Mossialos, E.; Xu, D.R.; Yip, W.; Zhang, H.; et al. The primary health-care system in China. Lancet 2017, 390, 2584–2594. [Google Scholar] [CrossRef]
- Yang, L.; Sun, L.; Wen, L.; Zhang, H.; Li, C.; Hanson, K.; Fang, H. Financing strategies to improve essential public health equalization and its effects in China. Int. J. Equity Health 2016, 15, 194. [Google Scholar] [CrossRef]
- Zhou, H.; Zhang, W.; Zhang, S.; Wang, F.; Zhong, Y.; Gu, L.; Qu, Z.; Liang, X.; Sa, Z.; Wang, X.; et al. Health providers’ perspectives on delivering public health services under the contract service policy in rural China: Evidence from Xinjian County. BMC Health Serv. Res. 2015, 15, 75. [Google Scholar] [CrossRef]
- Zhang, J.; Lin, S.; Liang, D.; Qian, Y.; Zhang, D.; Hou, Z. Public Health Services Utilization and Its Determinants among Internal Migrants in China: Evidence from a Nationally Representative Survey. Int. J. Environ. Res. Public Health 2017, 14, 1002. [Google Scholar] [CrossRef]
- Wang, L.; Wang, Z.; Ma, Q.; Fang, G.; Yang, J. The development and reform of public health in China from 1949 to 2019. Glob. Health 2019, 15, 45. [Google Scholar] [CrossRef]
- Wang, Z.; Ao, Q.; Luo, Y.; Wang, Q.; Lu, Z.; Liu, J. Estimating the costs of the national basic public health services in Zhuhai, China, through activity-based costing: A cross-sectional study. BMJ Open 2019, 9, e024831. [Google Scholar] [CrossRef]
- Yin, D.; Wong, S.T.; Chen, W.; Xin, Q.; Wang, L.; Cui, M.; Yin, T.; Li, R.; Zheng, X.; Yang, H.; et al. A model to estimate the cost of the National Essential Public Health Services Package in Beijing, China. BMC Health Serv. Res. 2015, 15, 222. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Kong, Y.; Sun, J.; Zhang, Y.; Yuan, L.; Wang, J. What are the challenges faced by village doctors in provision of basic public health services in Shandong, China? A qualitative study. Int. J. Environ. Res. Public Health 2019, 16, 2519. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chen, M.; Shi, X.-Q. Challenges of Basic Public Health Services Provided by Village Doctors in Guizhou, China. Asia Pac. J. Public Health 2015, 27, 69S–76S. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Lei, T.; Xie, Z.; Zhang, T. Determinants of basic public health services provision by village doctors in China: Using non-communicable diseases management as an example. BMC Health Serv. Res. 2015, 16, 42. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Smith, H.J.; Fei, Y.; Xu, B.; Nie, S.; Yan, W.; Diwan, V.K.; Sauerborn, R.; Dong, H. Factors influencing the provision of public health services by village doctors in Hubei and Jiangxi provinces, China. Bull. World Health Organ. 2013, 91, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Liang, S.; Deng, H.; Liu, S.; Wang, G.; Li, L.; Wang, M.; Pu, J.; Xing, W.; Luo, X.; Ehiri, J.; et al. Competency building for lay health workers is an intangible force driving basic public health services in Southwest China. BMC Health Serv. Res. 2019, 19, 596. [Google Scholar] [CrossRef]
- Zhao, Y.; Cui, S.; Yang, J.; Wang, W.; Guo, A.; Liu, Y.; Liang, W. Basic public health services delivered in an urban community: A qualitative study. Public Health 2011, 125, 37–45. [Google Scholar] [CrossRef]
- Liu, J.; Mao, Y. Patient Satisfaction with Rural Medical Services: A Cross-Sectional Survey in 11 Western Provinces in China. Int. J. Environ. Res. Public Health 2019, 16, 3968. [Google Scholar] [CrossRef]
- Stewart, D.W.; Shamdasani, P.N. Focus Groups: Theory and Practice; SAGA Publications: Thousand Oaks, CA, USA, 2015. [Google Scholar]
- OECD/EU. Health at a Glance: Europe 2018: State of Health in the EU Cycle; OECD Publishing: Paris, France, 2018. [Google Scholar]
- Great Britain: Department of Health. Healthy Lives, Healthy People: Our Strategy for Public Health in England; Stationery Office (Great Britain): Norwich, UK, 2010; ISBN 978-0-10-179852-5. [Google Scholar]
- Stephen, G.; Jan, Y.; Padmanabhan, B. Essential Public Health: Theory and Practice; Cambridge University Press: Cambridge, UK, 2012. [Google Scholar]
- Mckinlay, J.; Marceau, L. US public health and the 21st century: Diabetes mellitus. Lancet 2000, 356, 757–761. [Google Scholar] [CrossRef]
- Harrison, G. Essential Public Health Functions: A Three-Country Study in the Western Pacific Region; World Health Organization: Geneva, Switzerland, 2003; ISBN 978-92-9061-082-3. [Google Scholar]
- Liu, J.; Zhu, B.; Zhang, N.; He, R.; Mao, Y. Are Medical Graduates’ Job Choices for Rural Practice Consistent with their Initial Intentions? A Cross-Sectional Survey in Western China. Int. J. Environ. Res. Public Health 2019, 16, 3381. [Google Scholar] [CrossRef]
- Liu, J.; Zhu, B.; Mao, Y. Association between rural clinical clerkship and medical students’ intentions to choose rural medical work after graduation: A cross-sectional study in western China. PLoS ONE 2018, 13, e0195266. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Zhu, B.; Wu, J.; Mao, Y. Job satisfaction, work stress, and turnover intentions among rural health workers: A cross-sectional study in 11 western provinces of China. BMC Fam. Pract. 2019, 20, 9. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Mao, Y. Does previous job mobility behaviour have an effect on current turnover intentions of rural nurses? A cross-sectional survey in western China. Lancet 2019, 394, S49. [Google Scholar] [CrossRef]
- Liu, J.; Zhang, K.; Mao, Y. Attitude towards working in rural areas: A cross-sectional survey of rural-oriented tuition-waived medical students in Shaanxi, China. BMC Med. Educ. 2018, 18, 91. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Wang, H.; Wang, D.; Yuan, B. Job satisfaction of the primary healthcare providers with expanded roles in the context of health service integration in rural China: A cross-sectional mixed methods study. Hum. Resour. Health 2019, 17, 70. [Google Scholar] [CrossRef] [PubMed]
- Macharia, P.M.; Ouma, P.O.; Gogo, E.G.; Snow, R.W.; Noor, A.M. Spatial accessibility to basic public health services in South Sudan. Geospat. Health 2017, 12, 510. [Google Scholar] [CrossRef] [PubMed]
- Wei, X. Research on residents’ sense of gain and will of involvement in essential public health service. J. Panzhihua Univ. 2019, 36, 30–33. [Google Scholar]
- Liu, J.; Wu, Q.; Liu, H.; Zheng, T.; Tan, X.; Chen, M. Study on the influencing factors of the satisfaction of patients with hypertension to the village clinics under the background of rural basic public health services. Med. Soc. 2019, 32, 61–63. [Google Scholar]
- Xu, X.; Yang, Q.; Qiu, Y.; Zhao, Y.; Wang, W.; Ye, C.; Shang, X. Investigation of residents’ sensitivity to basic public health service project in Zhejiang province. Chin. J. Public Health Manag. 2018, 34, 765–768. [Google Scholar]
- Deng, L.; Yang, Y.; Chen, Y.; Cui, W.; Zhang, X. Analysis on awareness rate and satisfaction of resident’s basic public health service in 6 prefectures (cities) of Yunnan Province. Soft Sci. Health 2018, 32, 54–58. [Google Scholar]
- Qiu, F.; Li, W.; Yu, T.; Yan, Z.; Zheng, N. The investigation and analysis of residents’ awareness rate and satisfaction on basic public health service in Fuzhou. J. Community Med. 2017, 15, 10–12. [Google Scholar]
- Liu, H.; Ding, G. Analysis on residents’ knowledge and satisfaction of equalization policies on basic public health services in five districts of Gansu. Chongqing Med. 2016, 45, 1539–1541. [Google Scholar]
- Zhou, J.; Shi, J.; Yang, S.; Zhou, F.; Ye, L.; Liang, B.; Jiang, S. The utilization and satisfaction of basic public health services in patients with non-infectious diseases in Nanning. J. Community Med. 2015, 13, 56–59. [Google Scholar]
- Shang, X.; Wang, W.; Qiu, Y.; He, F.; Xu, X.; Lin, J. Residents satisfaction with basic public health service project in Zhejiang. Chin. J. Public Health Manag. 2015, 31, 912–914. [Google Scholar]
- Huang, W.; Zhou, J.; Yang, S.; Zhou, F.; Huang, J. Satisfaction with basic public health service among residents in Nanning in 2013. J. Community Med. 2015, 13, 13–15. [Google Scholar]
- He, S.; Feng, D.; Feng, Z. Investigation on utilization of primary public health services and satisfactory degree among elders in rural areas of China based on the goal of equalization. Med. Soc. 2012, 25, 49–51. [Google Scholar]
- Xu, S.; Gu, X.; Shi, S.; Chen, G.; Chen, R. Comparative research on awareness rate of basic public health services and satisfactory degree among urban and rural residents on goal of equalization. Anhui Med. J. 2017, 38, 1216–1219. [Google Scholar]
- Zhang, X.; Zhai, M.; Ge, W.; Liu, S.; Zhang, S.; Dang, R. Investigation on knowledge and utilization of basic public health services and satisfactory degree among rural residents based on the goal of equalization. J. Jining Med. Univ. 2015, 38, 271–274, 277. [Google Scholar]
- Ji, Y.; Ma, R.; Yu, X.; Jiang, J. The survey and analysis of satisfaction degree of residents’ basic public health service in some place of Anhui. J. Baotou Med. Coll. 2019, 35, 98–99, 108. [Google Scholar]
- Hao, A.; Li, C.; Pan, B. Guangdong residents’ awareness and satisfaction with China’s national essential public health services: A telephone-based survey. Chin. Gen. Pract. 2019, 22, 407–412. [Google Scholar]
- Gebreyesus, A. Determinants of client satisfaction with family planning services in public health facilities of Jigjiga town, Eastern Ethiopia. BMC Health Serv. Res. 2019, 19, 618. [Google Scholar] [CrossRef] [PubMed]
- Gitobu, C.M.; Gichangi, P.B.; Mwanda, W.O. Satisfaction with Delivery Services Offered under the Free Maternal Healthcare Policy in Kenyan Public Health Facilities. J. Environ. Public Health 2018, 2018, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Xiao, Y.; Zhao, K.; Liu, A. Implementation progress and effect of national essential public health services program in China. Chin. J. Public Health 2019, 35, 657–664. [Google Scholar]
- Liu, J.; Zhu, B.; Zhang, N.; He, R.; Mao, Y. Are medical graduates’ initial intentions consistent with whether they ultimately opt for rural practice after graduation? A cross-sectional survey in western China. Lancet 2018, 392, S18. [Google Scholar] [CrossRef]
| Characteristics | N | % |
|---|---|---|
| Gender (n = 8949) | ||
| Female | 5061 | 56.55 |
| Male | 3888 | 43.45 |
| Age (n = 8632) | ||
| ≤35 years | 3658 | 42.38 |
| 36–45 years | 1795 | 20.79 |
| ≥46 years | 3179 | 36.83 |
| Education (n = 8980) | ||
| Illiteracy | 1336 | 14.88 |
| Primary school | 2036 | 22.67 |
| Junior high school | 2770 | 30.85 |
| Senior high school and above | 2838 | 31.6 |
| Occupation (n = 8984) | ||
| Farmer | 4223 | 47.01 |
| Nonfarmer | 3603 | 40.1 |
| Other | 1158 | 12.89 |
| Monthly income (n = 8956) | ||
| No regular income | 2796 | 31.22 |
| ≤2000 Yuan | 3754 | 41.92 |
| ≥2001 Yuan | 2406 | 26.86 |
| Health status (n = 9019) | ||
| Relatively bad | 2371 | 26.29 |
| Good | 6648 | 73.71 |
| Indicators | Likert 5-point Scale of Resident Satisfaction, N (%) | Satisfaction Score | Spearman Correlation 1 | |||||
|---|---|---|---|---|---|---|---|---|
| Strongly Dissatisfied | Dissatisfied | Neither Dissatisfied nor Satisfied | Satisfied | Strongly Satisfied | Mean ± S.D. 2 | Coeffi. 3 | p-Value | |
| Health education | 198 (2.20) | 1314 (14.63) | 3288 (36.61) | 3103 (34.55) | 1078 (12.00) | 3.40 ± 0.951 | 0.537 | <0.001 |
| Immunization and health man. 4 for children | 135 (1.50) | 997 (11.10) | 2848 (31.69) | 3698 (41.15) | 1308 (14.56) | 3.56 ± 0.922 | 0.521 | <0.001 |
| Maternal health man. 4 | 113 (1.26) | 1223 (13.61) | 2990 (33.29) | 3398 (37.83) | 1259 (14.02) | 3.50 ± 0.937 | 0.579 | <0.001 |
| Elderly health man. 4 | 135 (1.50) | 1557 (17.30) | 3026 (33.63) | 3109 (34.55) | 1172 (13.02) | 3.40 ± 0.968 | 0.577 | <0.001 |
| Health man. 4 for residents with chronic diseases | 153 (1.70) | 1729 (19.23) | 2890 (32.15) | 2979 (33.14) | 1239 (13.78) | 3.38 ± 0.999 | 0.591 | <0.001 |
| Reporting and handling of infectious diseases | 132 (1.47) | 1540 (17.13) | 2955 (32.87) | 3129 (34.81) | 1233 (13.72) | 3.42 ± 0.974 | 0.592 | <0.001 |
| PHC worker’s attitude | 132 (1.47) | 764 (8.49) | 2817 (31.29) | 3759 (41.75) | 1532 (17.01) | 3.64 ± 0.910 | 0.710 | <0.001 |
| Overall satisfaction | 124 (1.37) | 813 (9.01) | 2950 (32.71) | 3666 (40.65) | 1466 (16.25) | 3.61 ± 0.908 | N/A | |
| Characteristics | Mean ± S.D. 1 | One-Way ANOVA |
|---|---|---|
| F-Value (p-Value) | ||
| Gender | 1.092 (0.296) | |
| Female | 3.62 ± 0.888 | |
| Male | 3.60 ± 0.932 | |
| Age | 15.717 (<0.001) | |
| ≤35 years | 3.55 ± 0.931 | |
| 36–45 years | 3.64 ± 0.930 | |
| ≥46 years | 3.67 ± 0.864 | |
| Education | 2.860 (0.035) | |
| Illiteracy | 3.64 ± 0.923 | |
| Primary school | 3.65 ± 0.881 | |
| Junior high school | 3.59 ± 0.898 | |
| ≥ Senior high school | 3.59 ± 0.930 | |
| Occupation | 23.263 (<0.001) | |
| Farmer | 3.67 ± 0.874 | |
| Nonfarmer | 3.60 ± 0.943 | |
| Other | 3.47 ± 0.902 | |
| Monthly income | 9.711 (<0.001) | |
| No regular income | 3.55 ± 0.905 | |
| ≤2000 Yuan | 3.64 ± 0.909 | |
| ≥2001 Yuan | 3.64 ± 0.902 | |
| Health status | 43.336 (<0.001) | |
| Relatively bad | 3.72 ± 0.925 | |
| Good | 3.58 ± 0.899 |
| Variables | Multiple Linear Regression | Binary Logistic Regression | ||||||
|---|---|---|---|---|---|---|---|---|
| B (95% CI 1) | S.E. 2 | t-Value | p-Value | B | S.E. 2 | OR 3 (95% CI 1) | p-Value | |
| Satisfaction with health education | 0.074 (0.056, 0.092) | 0.009 | 8.160 | <0.001 | 0.323 | 0.045 | 1.38 (1.26, 1.51) | <0.001 |
| Satisfaction with immunization and health man. 4 for children | 0.043 (0.024, 0.061) | 0.009 | 4.498 | <0.001 | 0.170 | 0.046 | 1.19 (1.08, 1.30) | <0.001 |
| Satisfaction with maternal health man. 4 | 0.074 (0.054, 0.094) | 0.010 | 7.346 | <0.001 | 0.283 | 0.048 | 1.33 (1.21, 1.46) | <0.001 |
| Satisfaction with elderly health man. 4 | 0.073 (0.054, 0.092) | 0.010 | 7.438 | <0.001 | 0.288 | 0.046 | 1.33 (1.22, 1.46) | <0.001 |
| Satisfaction with health man. 4 for residents with chronic diseases | 0.099 (0.080, 0.117) | 0.009 | 10.412 | <0.001 | 0.311 | 0.044 | 1.37 (1.25, 1.49) | <0.001 |
| Satisfaction with reporting and handling of infectious diseases | 0.128 (0.109, 0.147) | 0.010 | 13.122 | <0.001 | 0.397 | 0.046 | 1.49 (1.36, 1.63) | <0.001 |
| Satisfaction with PHC worker’s attitude | 0.425 (0.407, 0.443) | 0.009 | 46.171 | <0.001 | 1.527 | 0.050 | 4.61 (4.17, 5.08) | <0.001 |
| Age (36–45 years) | 0.007 (−0.027, 0.040) | 0.017 | 0.386 | 0.700 | 0.074 | 0.085 | 1.08 (0.91, 1.27) | 0.382 |
| Age (≥46 years) | 0.037 (0.005, 0.069) | 0.016 | 2.281 | 0.023 | 0.281 | 0.079 | 1.33 (1.14, 1.55) | <0.001 |
| Education (Primary school) | 0.012 (−0.031, 0.054) | 0.022 | 0.542 | 0.588 | 0.119 | 0.106 | 1.13 (0.91, 1.39) | 0.265 |
| Education (Junior high school) | −0.008 (−0.051, 0.035) | 0.022 | −0.365 | 0.715 | −0.091 | 0.107 | 0.91 (0.74, 1.13) | 0.395 |
| Education (≥ Senior high school) | 0.002 (−0.046, 0.050) | 0.024 | 0.078 | 0.938 | 0.033 | 0.120 | 1.03 (0.82, 1.31) | 0.782 |
| Occupation (Nonfarmer) | −0.017 (−0.051, 0.018) | 0.018 | −0.954 | 0.340 | −0.103 | 0.086 | 0.90 (0.76, 1.07) | 0.227 |
| Occupation (Other) | −0.037 (−0.078, 0.004) | 0.021 | −1.766 | 0.077 | −0.021 | 0.102 | 0.98 (0.80, 1.20) | 0.839 |
| Income (≤2000 Yuan) | 0.010 (−0.021, 0.040) | 0.016 | 0.640 | 0.522 | 0.116 | 0.076 | 1.12 (0.97, 1.30) | 0.129 |
| Income (≥2001 Yuan) | 0.040 (0.003, 0.078) | 0.019 | 2.112 | 0.035 | 0.181 | 0.094 | 1.20 (0.99, 1.44) | 0.055 |
| Health status (Relatively bad) | 0.007 (−0.021, 0.036) | 0.015 | 0.509 | 0.611 | 0.037 | 0.073 | 1.04 (0.90, 1.20) | 0.614 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.; Mao, Y. Rural Resident Experience on National Basic Public Health Services: A Cross-Sectional Survey in 10 Western Provinces of China. Healthcare 2019, 7, 160. https://doi.org/10.3390/healthcare7040160
Liu J, Mao Y. Rural Resident Experience on National Basic Public Health Services: A Cross-Sectional Survey in 10 Western Provinces of China. Healthcare. 2019; 7(4):160. https://doi.org/10.3390/healthcare7040160
Chicago/Turabian StyleLiu, Jinlin, and Ying Mao. 2019. "Rural Resident Experience on National Basic Public Health Services: A Cross-Sectional Survey in 10 Western Provinces of China" Healthcare 7, no. 4: 160. https://doi.org/10.3390/healthcare7040160
APA StyleLiu, J., & Mao, Y. (2019). Rural Resident Experience on National Basic Public Health Services: A Cross-Sectional Survey in 10 Western Provinces of China. Healthcare, 7(4), 160. https://doi.org/10.3390/healthcare7040160





