Impact of Standardized Prenatal Clinical Training for Traditional Birth Attendants in Rural Guatemala
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Alkema, L.; Chou, D.; Hogan, D.; Zhang, S.; Moller, A.B.; Gemmill, A.; Fat, D.M.; Boerma, T.; Temmerman, M.; Mathers, C.; et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: A systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet 2016, 387, 462–474. [Google Scholar] [CrossRef]
- Zureick-Brown, S.; Newby, H.; Chou, D.; Mizoguchi, N.; Say, L.; Suzuki, E.; Wilmoth, J. Understanding Global Trends in Maternal Mortality. Int. Perspect. Sex Reprod. Health 2013, 39, 32–41. [Google Scholar] [CrossRef] [PubMed]
- MSPAS. Estudio Nacional de Mortalidad Materna 2011. Guatemala City. 2011. Available online: http://www.mspas.gob.gt/index.php/component/jdownloads/send/94-muerte-materna/805-estudio-nacional-de-mortalidad-materna-2011?option=com_jdownloads (accessed on 28 September 2016).
- Walton, A.; Kestler, E.; Dettinger, J.C.; Zelek, S.; Holme, F.; Walker, D. Impact of a low-technology simulation-based obstetric and newborn care training scheme on non-emergency delivery practices in Guatemala. Int. J. Gynaecol. Obstet. 2016, 132, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Salud Publica y Asistencia Social. Encuesta Nacional de Salud Materno Infantil: Informe Interno Priliminario; Ministerio de Salud Publica y Asistencia Social: Guatemala City, Guatemala, 2017. [Google Scholar]
- Bailey, P.E.; Szaszdi, J.A.; Glover, L. Obstetric complications: Does training traditional birth attendants make a difference. Rev. Panam. Salud Publica 2002, 11, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Walsh, L. Beliefs and rituals in traditional birth attendant practice in Guatemala. J. Transcult. Nurs. 2006, 17, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Mahler, H. The safe motherhood initiative: A call to action. Lancet 1987, 1, 668–670. [Google Scholar] [CrossRef]
- Byrne, A.; Morgan, A. How the integration of traditional birth attendants with formal health systems can increase skilled birth attendance. Int. J. Gynaecol. Obstet. 2011, 115, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Wilson, A.; Gallos, I.D.; Plana, N.; Lissauer, D.; Khan, K.S.; Zamora, J.; MacArthur, C.; Coomarasamy, A. Effectiveness of strategies incorporating training and support of traditional birth attendants on perinatal and maternal mortality: Meta-analysis. BMJ 2011, 343. [Google Scholar] [CrossRef] [PubMed]
- Sakala, C.; Newburn, M. Meeting needs of childbearing women and newborn infants through strengthened midwifery. Lancet 2014, 384, e39–e40. [Google Scholar] [CrossRef]
- Munabi-Babigumira, S.; Glenton, C.; Lewin, S.; Fretheim, A.; Nabudere, H. Factors that influence the provision of intrapartum and postnatal care by skilled birth attendants in low- and middle-income countries: A qualitative evidence synthesis. Cochrane Database Syst. Rev. 2017, 11, Cd011558. [Google Scholar] [CrossRef] [PubMed]
- Carlough, M.; McCall, M. Skilled birth attendance: What does it mean and how can it be measured? A clinical skills assessment of maternal and child health workers in Nepal. Int. J. Gynaecol. Obstet. 2005, 89, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Ayiasi, R.M.; Criel, B.; Orach, C.G.; Nabiwemba, E.; Kolsteren, P. Primary healthcare worker knowledge related to prenatal and immediate newborn care: A cross sectional study in Masindi, Uganda. BMC Health Serv. Res. 2014, 14, 65. [Google Scholar] [CrossRef] [PubMed]
- WHO; ICM; FIGO. Making Pregnancy Safer: The Critical Role of the Skilled Birth Attendant Geneva; World Health Organization: New York, NY, USA, 2004. [Google Scholar]
- Ministry of Health and Public Assistance. Training Manual for Traditional Birth Attendants in Neonatal Maternal Care; Program, N.R.H., Ed.; Ministry of Health and Public Assistance: Guatemala City, Guatemala, 2016. [Google Scholar]
- Hernandez, S.; Oliveira, J.B.; Shirazian, T. How a training program is transforming the role of traditional birth attendants from cultural practitioners to unique health-care providers: A community case study in rural Guatemala. Front. Public Health 2017, 5. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, S.; Oliveira, J.; Cuc, J.C.; Shirazian, T. Prenatal Skills Pilot Study of Graduates from a Traditional Birth Attendant Training Program in Rural Guatemala; American College of Obstetrics and Gynecology: Austin, TX, USA, 2018. [Google Scholar]
- McCord, C.; Premkumar, R.; Arole, S.; Arole, R. Efficient and effective emergency obstetric care in a rural Indian community where most deliveries are at home. Int. J. Gynaecol. Obstet. 2001, 75, 297–307. [Google Scholar] [CrossRef]
- Jokhio, A.H.; Winter, H.R.; Cheng, K.K. An Intervention involving traditional birth attendants and perinatal and maternal mortality in Pakistan. N. Engl. J. Med. 2005, 352, 2091–2099. [Google Scholar] [CrossRef] [PubMed]
- Spector, J.M.; Agrawal, P.; Kodkany, B.; Lipsitz, S.; Lashoher, A.; Dziekan, G.; Bahl, R.; Merialdi, M.; Mathai, M.; Lemer, C.; et al. Improving quality of care for maternal and newborn health: Prospective pilot study of the WHO safe childbirth checklist program. PLoS ONE 2012, 7, e35151. [Google Scholar] [CrossRef] [PubMed]
- Patabendige, M.; Senanayake, H. Implementation of the WHO safe childbirth checklist program at a tertiary care setting in Sri Lanka: A developing country experience. BMC Pregnancy Childbirth 2015, 15, 12. [Google Scholar] [CrossRef] [PubMed]
- True, B.A.; Cochrane, C.C.; Sleutel, M.R.; Newcomb, P.; Tullar, P.E.; Sammons, J.H., Jr. Developing and Testing a Vaginal Delivery Safety Checklist. J. Obstet. Gynecol. Neonatal. Nurs. 2016, 45, 239–249. [Google Scholar] [CrossRef] [PubMed]
- Individualized, Supportive Care Key to Positive Childbirth Experience, Says WHO: World Health Organization 2018. Available online: http://www.who.int/mediacentre/news/releases/2018/positive-childbirth-experience/en/ (accessed on 16 February 2018).
- Stollak, I.; Valdez, M.; Rivas, K.; Perry, H. Casas Maternas in the rural highlands of Guatemala: A Mixed-methods case study of the introduction and utilization of birthing facilities by an indigenous population. Glob. Health Sci. Pract. 2016, 4, 114–131. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Average | Range |
|---|---|---|
| Age | 40 | 22–54 |
| Level of Education | 2nd grade | No formal education-8th grade (one outlier with one participant pursuing a technical degree in nutrition) |
| Marital Status | Married | 1 single, 1 widowed, 11 married |
| Years of Experience | 9 | 0–27 |
| Dominant Language | Spanish, Tz’tujil, Kaqcuichel |
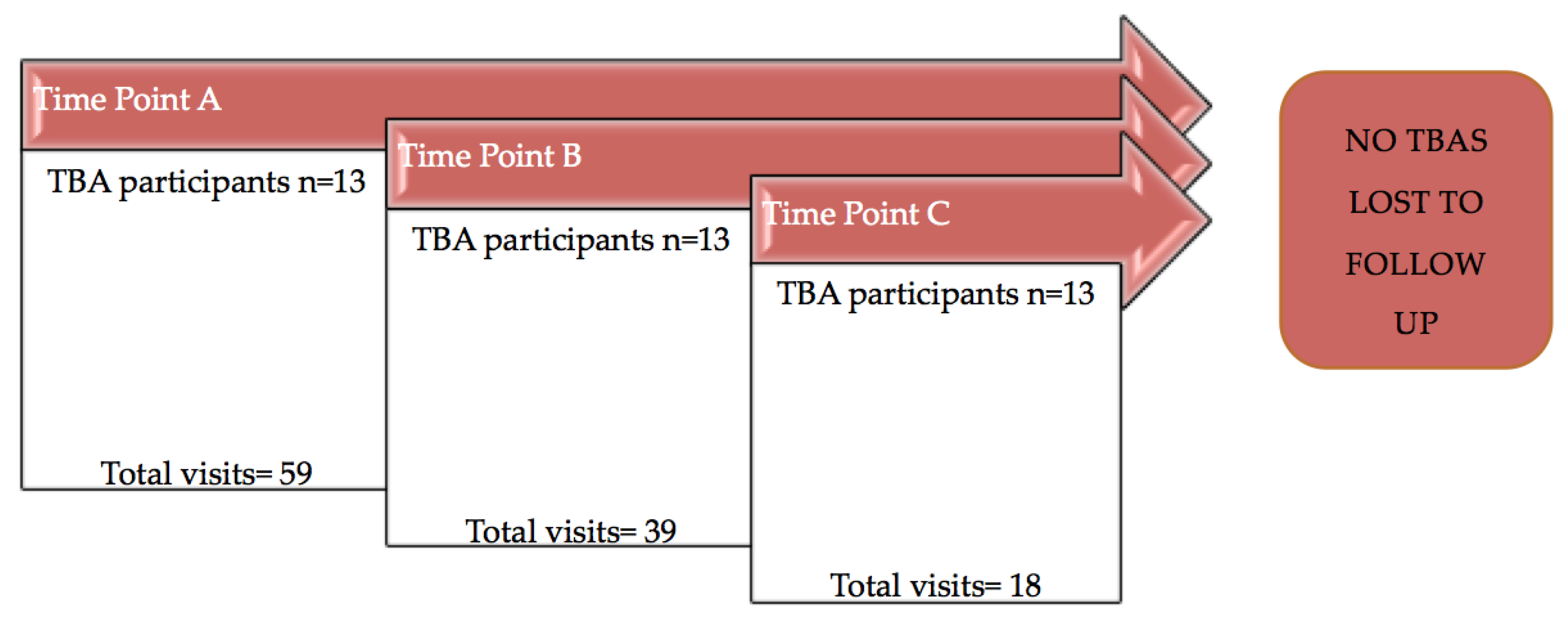
| Study Time Point | Dates of Data Collection | Total Weeks of Clinical Training | Total Weeks of Knowledge-Based Learning |
|---|---|---|---|
| Time Point A 1 | March 22–April 7, 2017 | 0 | 0 |
| Time Point B 2 | June 30–August 16, 2017 | 14 | 14 |
| Time Point C 3 | November 7–December 12, 2017 | 38 | 14 |
| Variable | Definition | Reason for Referral |
|---|---|---|
| History | ||
| Accurately calculates EDD | Using Naegele’s rule or pregnancy wheel. | If LMP unknown, referral for dating US. |
| Accurately calculates GA | Only if the mother knows LMP. | If LMP unknown, referral for dating US. |
| Age | Asks mother for an identification card if age is not known. | Referral recommended if AMA or less than 16 years old. |
| # of previous pregnancies | All pregnancies, including miscarriages. | |
| # of living children | All children; follows up if there is a discrepancy between total pregnancies and living children. | |
| Problems with previous pregnancies | Asks about prolonged labor, hemorrhage, problems with blood pressure, severe headache, fever during or after labor, infection during or after labor, prior C-sections. | Referral recommended if mother reports any prior problem. If C-section less than two years from current pregnancy recommends hospital birth. |
| Past medical history | Assesses any health conditions outside of pregnancy. | |
| Current medications | Assesses both OTC medications and street supplements. | |
| Documents history | Variables of importance are name, age, EDD, and prior issues of importance in order to report to the MOH. Not applicable for illiterate TBA. | |
| Clinical skills | ||
| Washes hands | Uses soap and water or antiseptic solution. | |
| Measures blood pressure | Mother seated or supine, arm below the heart, places cuff 1–2 finger breadths above the elbow, places stethoscope in the area of the brachial artery under the cuff. | Refers if blood pressure greater than 140/90, or in “red zone” if illiterate TBA. |
| Measures heart rate | Locates radial pulse and measures for 60 s. | |
| Measures fundal height | Can use a measuring tape or hand measurements if TBA is illiterate. | Refers if there is a difference greater than 4 cm from fundal height compared to GA. |
| Listens to fetal heart rate | Can find fetal heart rate and distinguish from maternal heart rate and placental vessels. | Refers if fetal distress (FHR > 160 bpm, <100 bpm) persists throughout the visit. |
| Finds the position of fetus | Uses Leopold’s maneuvers. | If the fetal position is oblique, transverse, or breech, in late pregnancy, discusses with mother the dangers of home birth. |
| Documents all findings | Variables of importance are blood pressure findings to track trends over pregnancy, not applicable if illiterate. | |
| Counseling | ||
| Discusses severe headaches | Explains to mom the risk of a severe headache and associated changes in vision. | Discusses with mother to report to the health post, local hospital, or private clinic. |
| Discusses severe abdominal pains | Demonstrates pain in the epigastric region. | Discusses with mother to report to the health post, local hospital, or private clinic. |
| Discusses vaginal bleeding | Explains the risk of spotting or bleeding at any point during the pregnancy. | Discusses with mother to report to the health post, local hospital, or private clinic. |
| Discusses fever | Explains chills and night sweats as symptoms of a fever. | Discusses with mother to report to the health post, local hospital, or private clinic. |
| Discusses location of birth | Discusses with mother and partner (if present) about the risks and benefits of both a home birth and a hospital birth). | |
| Discusses emergency plan | Discusses with mother and partner (if present) where to report and how to get there if an emergency arises during labor and delivery. | |
| Distributes prenatal vitamins | Hands a 30 day supply to mother. | |
| Counsels on the importance of prenatal vitamins | Explains the maternal and fetal benefit of prenatal vitamins to mother. | |
| Counsels on Td vaccine | Explains the vaccine schedule (1st shot, 2nd shot 2 months later, 3rd shot months later) to mother and the importance of vaccination especially if a home birth is planned. | Refers to either health post or local hospital to received Td vaccine. |
| Time Point A 2 | Time Point B 3 | Time Point C 4 | p-value 5 | |
|---|---|---|---|---|
| Percentage of correctly performed prenatal clinical skills | 25.8 (19.6) | 62.3 (16.3) | 71 (12.5) | Between A and B, 0.0001 |
| Between B and C, 0.034 |
| Prenatal Skills | Time Point A 2 | Time Point B 3 | Time Point C 4 | p-value 5 |
|---|---|---|---|---|
| History (overall) | 26.3% | 58.8% | 87.1% | Between A and B, 0.005 |
| Between B and C, <0.0001 | ||||
| Accurately calculates EDD | 52.0% | 82.0% | 90.0% | - |
| Accurately calculates GA | 7.5% | 68.0% | 90.0% | - |
| Age | 36.0% | 64.0% | 92.0% | - |
| # of previous pregnancies | 43.5% | 64.0% | 100.0% | - |
| # of living children | 37.0% | 64.0% | 100.0% | - |
| Problems with previous pregnancies | 35.5% | 50.0% | 100.0% | - |
| Past medical history | 10.0% | 52.0% | 70.0% | - |
| Current medications | 17.5% | 44.0% | 78.5% | - |
| Documents history | 8.5% | 100.0% | 100.0% | - |
| Clinical skills (overall) | 9.7% | 92.4% | 81.4% | Between A and B, ≤0.0001 |
| Between B and C, 0.19 | ||||
| Washes hands | 0.0% | 78.0% | 45.0% | - |
| Measures blood pressure | 0.0% | 100.0% | 93.0% | - |
| Measures heart rate | 0.0% | 94.0% | 100.0% | - |
| Measures fundal height | 0.0% | 88.0% | 93.0% | - |
| Listens to fetal heart rate | 0.0% | 100.0% | 100.0% | - |
| Finds position of fetus | 64.5% | 94.0% | 100.0% | - |
| Documents all findings | 0% | 100.0% | 87.0% | - |
| Counseling (overall) | 27.7% | 86.2% | 72.0% | Between A and B, ≤0.0001 |
| Between B and C, 0.09 | ||||
| Discusses severe headache | 40.5% | 89.0% | 94.0% | - |
| Discusses severe abdominal pain | 28.0% | 89.0% | 94.0% | - |
| Discusses vaginal bleeding | 34.0% | 89.0% | 89.0% | - |
| Discusses fever | 35.0% | 89.0% | 83.0% | - |
| Discusses location of birth | 41.0% | 86.0% | 83.0% | - |
| Discusses emergency plan | 43.5% | 86.0% | 84.0% | - |
| Distributes prenatal vitamins | 0.0% | 89.0% | 78.0% | - |
| Counsels on importance of prenatal vitamins | 0.0% | 85.0% | 65.0% | - |
| Counsels on Td vaccine | 29.5% | 89.0% | 50.0% | - |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernandez, S.; Oliveira, J.; Jones, L.; Chumil, J.; Shirazian, T. Impact of Standardized Prenatal Clinical Training for Traditional Birth Attendants in Rural Guatemala. Healthcare 2018, 6, 60. https://doi.org/10.3390/healthcare6020060
Hernandez S, Oliveira J, Jones L, Chumil J, Shirazian T. Impact of Standardized Prenatal Clinical Training for Traditional Birth Attendants in Rural Guatemala. Healthcare. 2018; 6(2):60. https://doi.org/10.3390/healthcare6020060
Chicago/Turabian StyleHernandez, Sasha, Jessica Oliveira, Leah Jones, Juan Chumil, and Taraneh Shirazian. 2018. "Impact of Standardized Prenatal Clinical Training for Traditional Birth Attendants in Rural Guatemala" Healthcare 6, no. 2: 60. https://doi.org/10.3390/healthcare6020060
APA StyleHernandez, S., Oliveira, J., Jones, L., Chumil, J., & Shirazian, T. (2018). Impact of Standardized Prenatal Clinical Training for Traditional Birth Attendants in Rural Guatemala. Healthcare, 6(2), 60. https://doi.org/10.3390/healthcare6020060




