The BASE-Program—A Multidimensional Approach for Health Promotion in Companies
Abstract
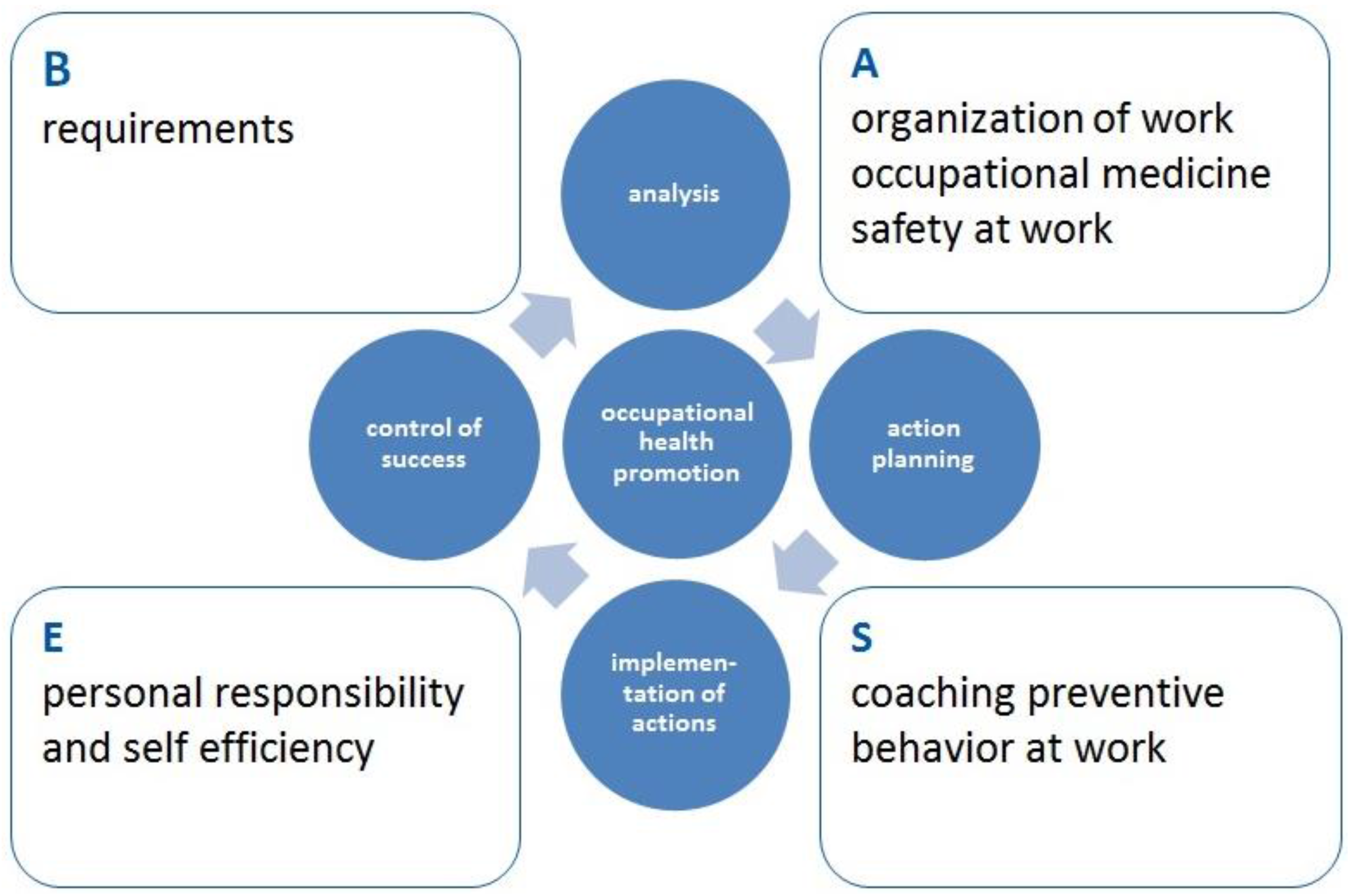
:1. Introduction
- The program ties in with the companies’ structures of the working conditions;
- The program considers the companies’ organizational and social environment;
- The program integrates the employees in the assessment of working health risks (participatory approach).
- Daily activities are analysed within the initial assessment of requirements by observation of the workplace and/or video analyses. This helps to create functional load/exposure profiles and identify recurring movements of high load factor.
- Based on the results of these analyses, adequate movement tasks are generated to train the coping with the usual demands of work. The introduction of a first-hand experience in behaviour change involves the movement experiences (titled the “AHA”-experience). This AHA experience is comprised of three components: (1) body awareness; (2) recognition of dysfunctional movements; and (3) understanding positive and negative behaviour in day-to-day working tasks. This serves as the initial step in preparing for the necessary change in automated movement behaviour.
- The movement experiences are reflected on and internalized by discussion targeting the adaption of ergonomic motor execution to suit individual physical working conditions.
- An explanation is provided about why the changed motor execution leads to reduced stresses and strains and how it can be implemented in day-to-day work. These considerations are made together by the exercise instructors and the employees.
- The employees get the opportunity to put the new movement perceptions into practice by repeated solving of different movement tasks which they may encounter at work.
- The principles of ergonomic motor behaviour are tested and reflected in different labour situations to facilitate a transfer to different actions in day-to-day work.
- Implementation of the BASE concept (stage one)
- Evaluation of the outcome effects of the interventions (stage two)
- Lasting effects and enhancing of health promotion (stage three)
2. Experimental Section
2.1. Application Fields and Goals
2.2. Participants
2.2.1. Application Field 1
2.2.2. Application Field 2
2.2.3. Application Field 3
2.3. Ethical Statements
2.4. Materials and Methods
2.4.1. Questionnaires
2.4.2. Observation of the Workplace
2.4.3. Physical Examinations
2.4.4. Cognitive Representation of Movement Coordination/Changes in Cognitive Structures
2.5. Statistical Analysis
3. Results
3.1. Application Field No. 1—BASE in an International Logistic Company
3.1.1. Implementation of the BASE Concept (Stage One)
- The organization of the work place, i.e., working height, distance from the object to be lifted and foot and body positions needed to be improved.
- During the lifting process, most of the employees had straight legs with low knee angles which led to stresses on the lower spine.
- Most workers lifted boxes with a thoracic spine hyper lordosis.
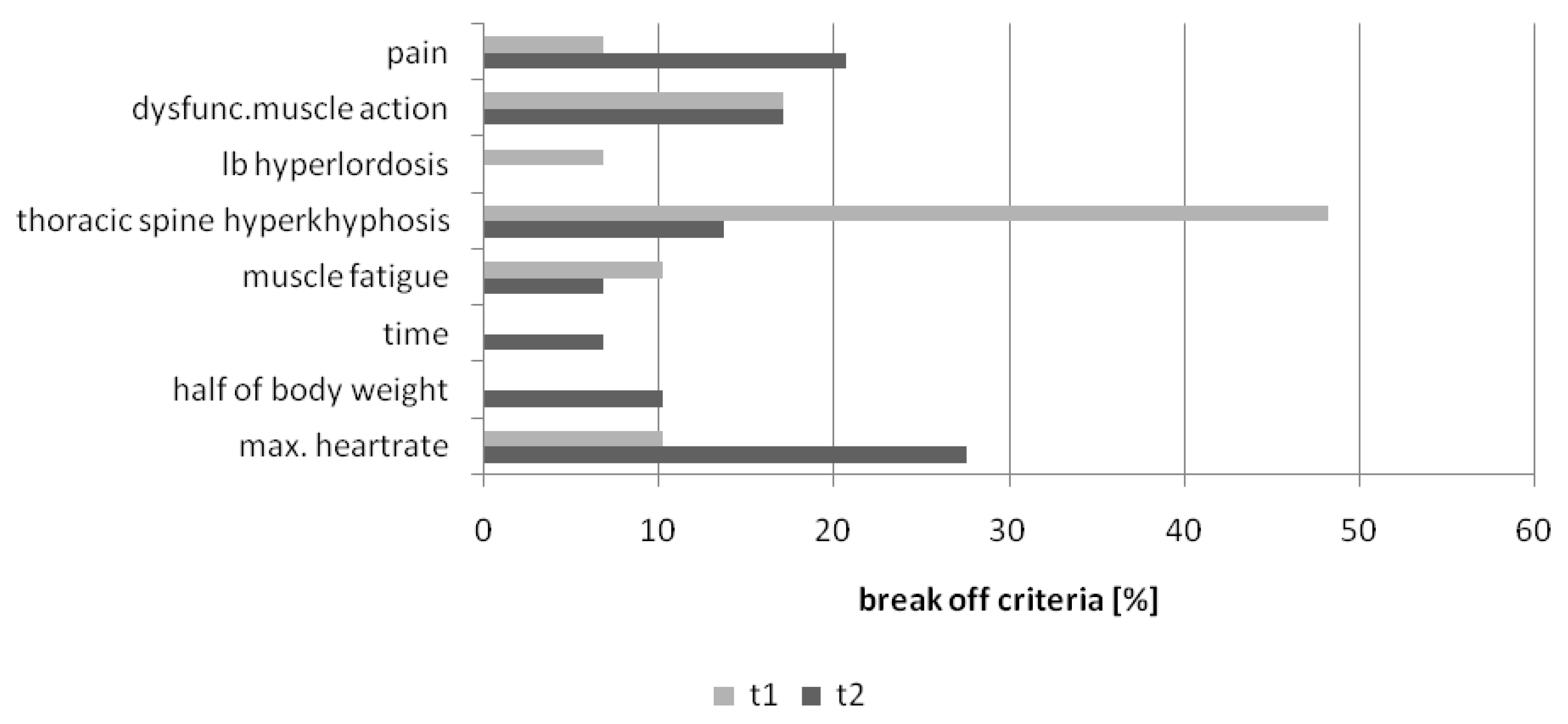
3.1.2. Evaluation of Outcome Effects after the Workplace Intervention (Stage Two)
3.1.3. Learning and Lasting Effects of Workers’ Knowledge and Behaviour with Regard to Ergonomic Box Lifting (Stage Three)
3.2. Application Field No. 2—BASE in an International Industrial Company
3.2.1. Implementation of the BASE Concept (Stage One)
- Exercises for movement and body awareness inside the working process,
- Reflections of one’s own movement and working behaviour,
- Instructions for movement optimization,
- Instructions for independently executing compensatory exercises, and
- Monitoring of personal health promotion.
- Workplace organization
- Positioning in front of loads
- Optimal way of grabbing
- Ergonomic screwing operations
- Ergonomic turning and rotational movements
- Compensatory exercises for strained muscle groups for home workouts
3.2.2. Evaluation of Outcome Effects after the Workplace Intervention (Stage Two)
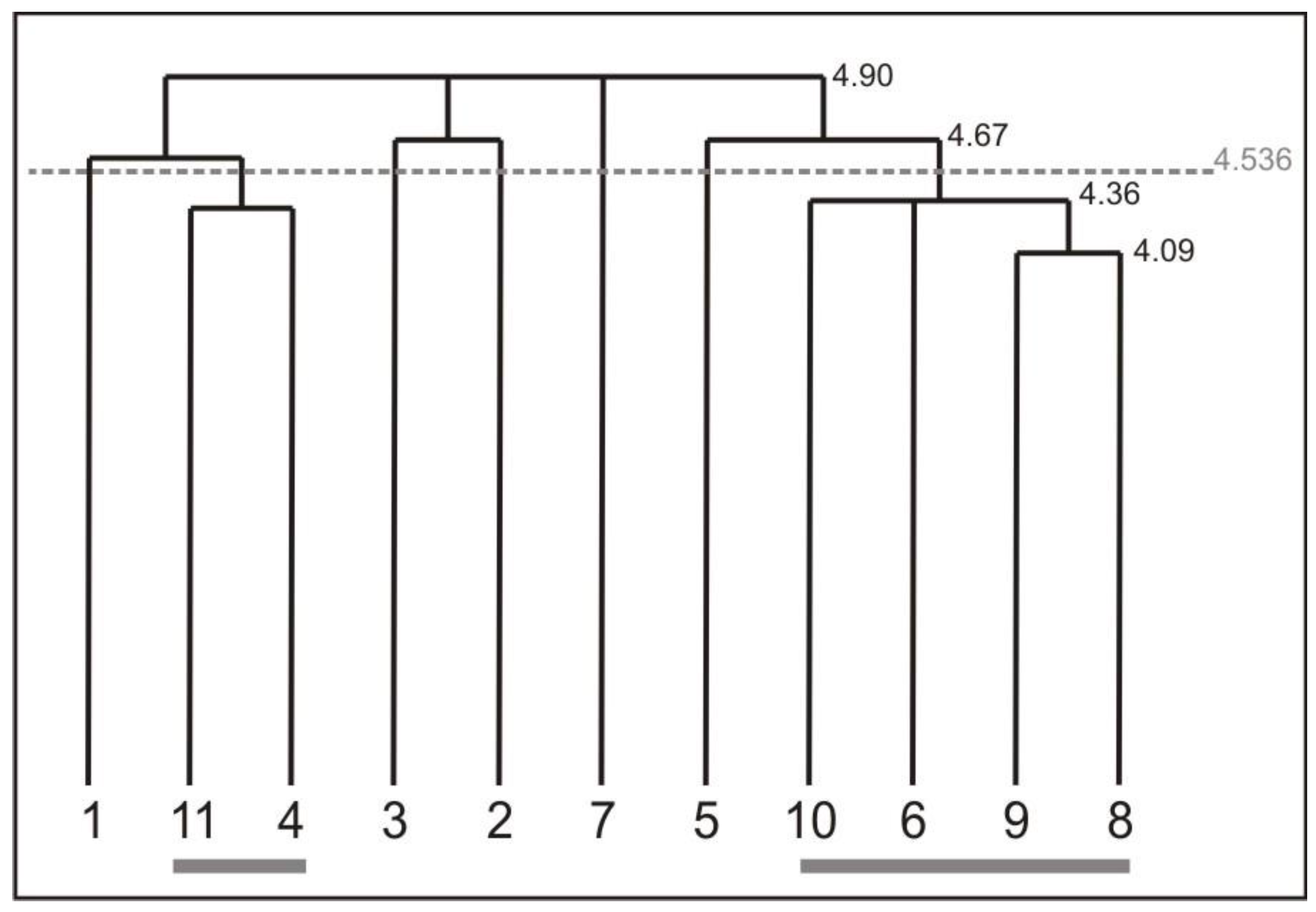
3.2.3. Learning and Lasting Effects of Workers’ Cognitive Representation and Behaviour of an Ergonomic Screwing Action (Stage Three)
3.3. Application Field No. 3—BASE in Office Workers in a Management Department
3.3.1. Implementation of the BASE Concept (Stage One)
3.3.2. Evaluation of Outcome Effects after the Workplace Intervention (Stage Two)
- Exercises to be aware of discomfort body positions
- Working height and sitting position
- Workplace and work organisation
- Dynamic sitting
- Detail seeing and the consequences of the head position to reduce neck pain
- Shoulder flexibility
- Ergonomic mouse handling
- Motivation for additional physical activity
3.3.3. Motivation and Satisfaction with Additional Exercises (Stage Three)
4. Discussion
4.1. Implementation of the BASE-Program in the Three Application Fields (Stage One)
4.2. Evaluation of the Outcome Effects of the Interventions (Stage Two)
4.2.1. Application Field 1 Logistic Workers
4.2.2. Application Field 2 Cellular Manufacturing
4.2.3. Application Field 3 Office Workers
4.3. Lasting Effects and Enhancing Health Promotion (Stage Three)
4.3.1. Application Field 1 Logistic Workers
4.3.2. Application Field 2 Cellular Manufacturing
4.3.3. Application Field 3 Office Workers
5. Limitations
6. Conclusions
- The employees should be involved actively in the program to express and comment on their needs and to clarify questions of understanding.
- Further instruments are needed (e.g., multipliers, posters, flyer, homework materials), to establish steady functional memory structures within each employee.
- Just the exercise program for the home workout is not sufficient for an obligatory performance of the exercises. In this case, a link to company sports or other prevention courses should be considered.
- The intervention programs should be tailored and individualized.
- Referring to change automatized movements or habits, the interventions should include more practice and transfer units within different working conditions and situations.
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Wollesen, B.; Menzel, J.; Drögemüller, R.; Hartwig, C.; Mattes, K. The effects of a workplace health promotion program in small and middle-sized companies: A pre-post analysis. J. Public Health 2016. [Google Scholar] [CrossRef]
- Ulich, E. Wandel der Arbeit–Wandel der Belastungen. In Immer Schneller, immer Mehr; Springer: Wiesbaden, Germany, 2013; pp. 195–220. [Google Scholar]
- Bundesministerium für Arbeit und Soziales (BMAS). Sicherheit und Gesundheit bei der Arbeit 2013. Unfallverhütungsbericht Arbeit. Available online: http://www.baua.de/de/Publikationen/Fachbeitraege/Suga-2013.html (accessed on 29 June 2016).
- DAK. DAK-Gesundheitsreport 2014. Available online: https://www.dak.de/dak/download/Vollstaendiger_bundesweiter_Gesundheitsreport_2014–1374196.pdf (accessed on 29 June 2016).
- BKK. BKK-Gesundheitsreport 2013. Available online: http://www.bkk-dachverband.de/fileadmin/publikationen/gesundheitsreport/fruehere_gesundheitsreporte/BKK-Gesundheitsreport_2013.pdf (accessed on 29 June 2016).
- Barmer GEK. Barmer GEK-Gesundheitsreport 2013. Available online: http://firmenangebote.barmer-gek.de/barmer/web/Portale/Firmenangebote/Gesundheitsangebote-fuer-Beschaeftigte/Gesundheit-im-Unternehmen/Gesundheitsfakten/Gesundheitsreport/Gesundheitsreports-2013__PDF/Baden-Wuerttemberg,property=Data.pdf (accessed on 29 June 2016).
- Bundesministerium für Arbeit und Soziales (BMAS). Sicherheit und Gesundheit bei der Arbeit 2012. Unfallverhütungsbericht Arbeit. Available online: http://www.baua.de/de/Publikationen/Fachbeitraege/Suga-2012.html (accessed on 29 June 2016).
- Grieco, A.; Molteni, G.; Vito, G.D.; Sias, N. Epidemiology of musculoskeletal disorders due to biomechanical overload. Ergonomics 1998, 41, 1253–1260. [Google Scholar] [CrossRef] [PubMed]
- Latko, W.A.; Armstrong, T.J.; Franzblau, A.; Ulin, S.S.; Werner, R.A.; Albers, J.W. Cross-sectional study of the relationship between repetitive work and the prevalence of upper limb musculoskeletal disorders. Am. J. Ind. Med. 1999, 36, 248–259. [Google Scholar] [CrossRef]
- Wollesen, B.; Lex, H.; Mattes, K. BASE als Programm zur Prävention von (Rücken-) Beschwerden in der betrieblichen Gesundheitsförderung (BASE as a programme in the prevention of back pain in occupational health promotion). Gruppendynamik Organisationsberatung 2012, 43, 389–411. [Google Scholar] [CrossRef]
- Muggleton, J.M.; Allen, R.; Chappell, P.H. Hand and arm injuries associated with repetitive manual work in industry: A review of disorders, risk factors and preventive measures. Ergonomics 1999, 42, 714–739. [Google Scholar] [CrossRef] [PubMed]
- Punnett, L.; Wegman, D.H. Work-related musculoskeletal disorders: The epidemiologic evidence and the debate. J. Electromyogr. Kinesiol. 2004, 14, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Waddell, G.; Burton, A.K. Occupational health guidelines for the management of low back pain at work: Evidence review. Occup. Med. 2001, 51, 124–135. [Google Scholar] [CrossRef]
- Andersen, J.H.; Fallentin, N.; Thomsen, J.F.; Mikkelsen, S. Risk factors for neck and upper extremity disorders among computers users and the effect of interventions: An overview of systematic reviews. PLoS ONE 2011, 6, e19691. [Google Scholar] [CrossRef] [PubMed]
- Ijmker, S.; Huysmans, M.; Blatter, B.M.; van der Beek, A.J.; van Mechelen, W.; Bongers, P.M. Should office workers spend fewer hours at their computer? A systematic review of the literature. Occup. Environ. Med. 2007, 64, 211–222. [Google Scholar] [CrossRef] [PubMed]
- Macedo, A.C.; Trindade, C.S.; Brito, A.P.; Dantas, M.S. On the effects of a workplace fitness program upon pain perception: A case study encompassing office workers in a Portuguese context. J. Occup. Rehabil. 2011, 21, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Lühmann, D.; Zimolog, B. Prävention von Rückenerkrankungen in der Arbeitswelt (Prevention of back disorders in the workplace). In Fehlzeiten-Report 2006. Chronische Krankheiten; Badura, B., Schellschmidt, H., Vetter, C., Eds.; Springer: Heidelberg, Germany, 2007; pp. 63–80. [Google Scholar]
- Leclerc, A.; Franchi, P.; Cristofari, M.F.; Delemotte, B.; Mereau, P.; Teyssier-Cotte, C.; Touranchet, A. Carpal tunnel syndrome and work organisation in repetitive work: A cross sectional study in France. Study Group on Repetitive Work. Occup. Environ. Med. 1998, 55, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Kahlmeier, S.; Alpiger, P.; Martin, B.W. National recommendations for health-enhancing physical activity: The situation for Switzerland in 2011 and options for further developments. Schweizerische Zeitschrift Sportmedizin Sporttraumatologie 2012, 60, 96–101. [Google Scholar]
- Dishman, R.K.; Oldenburg, B.; O’Neal, H.; Shephard, R.J. Worksite physical activity interventions. Am. J. Prev. Med. 1998, 15, 344–361. [Google Scholar] [CrossRef]
- Marshall, A.L. Challenges and opportunities for promoting physical activity in the workplace. J. Sci. Med. Sport 2004, 7, 60–66. [Google Scholar] [CrossRef]
- Proper, K.I.; Koning, M.; Van der Beek, A.J.; Hildebrandt, V.H.; Bosscher, R.J.; van Mechelen, W. The effectiveness of worksite physical activity programs on physical activity, physical fitness, and health. Clin. J. Sport Med. 2003, 13, 106–117. [Google Scholar] [CrossRef] [PubMed]
- Taylor, N.; Conner, M.; Lawton, R. The impact of theory on the effectiveness of worksite physical activity interventions: A meta-analysis and meta-regression. Health Psychol. Rev. 2012, 6, 33–73. [Google Scholar] [CrossRef]
- Proper, K.I.; Staal, B.J.; Hildebrandt, V.H.; Van der Beek, A.J.; Van Mechelen, W. Effectiveness of physical activity programs at worksites with respect to work-related outcomes. Scand. J. Work Environ. Health 2002, 28, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Malik, S.H.; Blake, H.; Suggs, L.S. A systematic review of workplace health promotion interventions for increasing physical activity. Br. J. Health Psychol. 2014, 19, 149–180. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.L.; Saervoll, C.A.; Mortensen, O.S.; Poulsen, O.M.; Hannerz, H.; Zebis, M.K. Effectiveness of small daily amounts of progressive resistance training for frequent neck/shoulder pain: Randomised controlled trial. Pain 2011, 152, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Oesch, P.; Kool, J.; Hagen, K.B.; Bachmann, S. Effectiveness of exercise on work disability in patients with non-acute non-specific low back pain: Systematic review and metaanalysis of randomized controlled trials. J. Rehabil. Med. 2010, 42, 193–205. [Google Scholar] [CrossRef] [PubMed]
- Van Tulder, M.; Malmivaara, A.; Esmail, R.; Koes, B. Exercise therapy for low back pain: A systematic review within the framework of the cochrane collaboration back review group. Spine 2000, 25, 2784–2796. [Google Scholar] [CrossRef] [PubMed]
- Lelis, C.M.; Battaus, M.R.B.; Freitas, F.C.T.D.; Rocha, F.L.R.; Marziale, M.H.P.; Robazzi, M.L.D.C.C. Work-related musculoskeletal disorders in nursing professionals: An integrative literature review. Acta Paulista Enfermagem 2012, 25, 477–482. [Google Scholar] [CrossRef]
- Sihawong, R.; Janwantanakul, P.; Jiamjarasrangsi, W. Effects of an exercise programme on preventing neck pain among office workers: A 12-month cluster-randomised controlled trial. Occup. Environ. Med. 2014, 71, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Pereira, M.J.; Coombes, B.K.; Comans, T.A.; Johnston, V. The impact of onsite workplace health-enhancing physical acitivity interventions on worker productivity: A systematic review. Occup. Environ. Med. 2015, 72, 401–412. [Google Scholar] [CrossRef] [PubMed]
- Vuillemin, A.; Rostami, C.; Maes, L.; Van Cauwenberghe, E.; van Lenthe, F.J.; Brug, J.; de Bourdeaudhuij, I.; Oppert, J.M. Worksite physical activity interventions and obesity: A review of European studies (the HOPE project). Obes. Facts 2011, 4, 479–488. [Google Scholar] [CrossRef] [PubMed]
- Trost, S.G.; Owen, N.; Bauman, A.E.; Sallis, J.F.; Brown, W. Correlates of adults’ participation in physical activity: Review and update. Med. Sci. Sports Exerc. 2002, 34, 1996–2001. [Google Scholar] [CrossRef] [PubMed]
- Rongen, A.; Robroek, S.J.; van Lenthe, F.J.; Burdorf, A. Workplace health promotion: A meta-analysis of effectiveness. Am. J. Prev. Med. 2013, 44, 406–415. [Google Scholar] [CrossRef] [PubMed]
- Healy, G.; Lawler, S.; Thorp, A.; Neuhaus, M.; Robson, E.; Owen, N.; Dunstan, D. Reducing Prolonged Sitting in the Workplace. Human Factors and Ergonomics Society. Available online: http://www.uq.edu.au/cprc/docs/Reducing_Sitting_Workplace_Full.pdf (accessed on 29 June 2016).
- Rosenbrock, R. Was ist New Public Health (What’s New Public Health)? Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2001, 44, 753–762. [Google Scholar] [CrossRef]
- Schwarzer, R. Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Appl. Psychol. Int. Rev. 2008, 57, 1–29. [Google Scholar] [CrossRef]
- Wickström, G. Evaluation of Work-Related Intervention Studies to Prevent Chronification of Back Disorders; Forschungsgruppe Gesundheitsrisiken und Präventionspolitik: Berlin, Germany, 1992; p. 99. [Google Scholar]
- Lenhardt, U. Zehn Jahre betriebliche Gesundheitsförderung, Veröffentlichungen der Arbeitsgruppe Public Health Wissenschaftszentrum Berlin für Sozialforschung (WZB), 1997, No. P97–201, Berlin. Available online: https://core.ac.uk/download/files/153/6628143.pdf (accessed on 19 June 2016).
- Ritter, P.; Winkelmann, T.; Tidow, G. Prävention von Wirbelsäulenschäden. Modellvorhaben im Steinkohlebau: Krafttraining und Koordinationsschulung mit Auszubildenden (Prevention of Spinal Injuries. Pilot Projects in Coal: Strength Training and Coordination Training with Trainees); HVBG: St. Augustin, Germany, 2001. [Google Scholar]
- Zimolong, B. Erfolgsfaktoren Betrieblicher Gesundheitsförderung (Success Factors of Workplace Health Promotion). 2007. Available online: http://www.ruhr-uni-bochum.de/imperia/md/content/psy_auo/bzwob2007.pdf (accessed on 11 May 2016).
- Caffier, G.; Steinberg, U.; Liebers, F. Praxisorientiertes Methodeninventar zur Belastungs- und Beanspruchungsbeurteilung im Zusammenhang mit Arbeitsbedingten Muskel-Skelett-Erkrankungen (Practice-Oriented Methods for the Assessment of Strains and Stresses in Connection with Work-Related Musculoskeletal Disorders). Schriftenreihe der Bundesanstalt für Arbeitsschutz und Arbeitsmedizin, 1999, Dortmund/Berlin. Available online: http://www.baua.de/cae/servlet/contentblob/673906/publicationFile/46978/Fb850.pdf (accessed on 1 March 2016).
- Slesina, W. Fragebogen zur Einschätzung der Arbeitsplatzbelastung (Questionnaire for Assessment of job Stress). In Praxisorientiertes Methodeninventar zur Belastungs- und Beanspruchungsbeurteilung im Zusammenhang mit arbeitsbedingten Muskel-Skelett-Erkrankungen; Caffier, G., Steinberg, U., Liebers, F., Eds.; Wirtschaftsverlag NW: Bremerhaven, Germany, 1999. [Google Scholar]
- Bullinger, M.; Kirchberger, I. SF 36-Fragebogen zum Gesundheitszustand (SF-36 Health Survey). Handanweisung; Hogref: Göttingen, Germany, 1998. [Google Scholar]
- Baecke, A.H.; Burema, J.; Frijters, J.E. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am. J. Clin. Nutr. 1982, 36, 936–942. [Google Scholar] [PubMed]
- Karhu, O.; Kansi, P.; Kourinka, I. Correcting working postures in industry:A practical mthod for analysis. Appl. Ergonom. 1977, 8, 199–201. [Google Scholar] [CrossRef]
- Steinberg, U.; Caffier, G.; Liebers, F. Assessment of manual material handling based on key indicators—German guidelines. In Handbook of Standards in Ergonomics and Human Factors; Karwowski, W., Ed.; Lawrenz Erlbaum Associates: Mahwah, NJ, USA; London, UK, 2006; pp. 319–338. [Google Scholar]
- Janda, V. Manuelle Muskelfunktionsdiagnostik; Urban&Fischer Verlag: München, Germany, 2009. [Google Scholar]
- Mayer, T.G.; Barnes, D.; Kishino, N.D.; Nichols, G.; Gatchel, R.J.; Mayer, H.; Mooney, V. Progressive Isoinertial Lifting Evaluation: I. A Standardized Protocol and Normative Database. Spine 1988, 13, 993–997. [Google Scholar] [CrossRef] [PubMed]
- Schack, T. Measuring mental representations. In Measurement in Sport and Exercise Psychology; Tenenbaum, G., Eklund, R.C., Kamata, A., Eds.; Human Kinetics: Champaign, IL, USA, 2011; pp. 203–214. [Google Scholar]
- Schack, T.; Mechsner, F. Representation of motor skills in human long-term memory. Neurosci. Lett. 2006, 391, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Schack, T.; Ritter, H. The cognitive nature of action—Functional links between cognitive psychology, movement science, and robotics. Prog. Brain Res. 2009, 174, 231–250. [Google Scholar] [PubMed]
- Braun, S.M.; Beurskens, A.J.; Schack, T.; Marcellis, R.G.; Oti, K.C.; Schols, J.M.; Wade, D.T. Is it possible to use the Structural Dimension Analysis of Motor Memory (SDA-M) to investigate representations of motor actions in stroke patients? Clin. Rehabil. 2007, 21, 822–832. [Google Scholar] [CrossRef] [PubMed]
- Lex, H.; Essig, K.; Knoblauch, A.; Schack, T. Cognitive Representations and Cognitive Processing of Team-Specific Tactics in Soccer. PLoS ONE 2015, 10, e0118219. [Google Scholar] [CrossRef] [PubMed]
- Hammer, S.S.; Liebherr, M.; Kersten, S.; Haas, C.T. Adherence to Worksite Health Interventions: Practical Recommendations Based on a Theoretical Framework. J. Workplace Behav. Health 2015, 30, 325–343. [Google Scholar] [CrossRef]
- Menzel, J.; Drögemüller, R.; Hartwig, C.; Wollesen, B. Innerbetriebliche Strukturen für Betriebliches Gesundheitsmanagement in kleinen und mittleren Unternehmen–Ein Ländervergleich aus Querschnittsdaten des EU-Projekts “Fit for Business” (Teil 2) (Internal structures for health promotion in small and medium-sized businesses—A coun try comparison by cross-sectional data of the European project “Fit for Business” (Part 2)). Bewegungstherapie Gesundheitssport 2016, 32, 85–90. [Google Scholar]
- Rasotto, C.; Bergamin, M.; Simonetti, A.; Maso, S.; Bartolucci, G.B.; Ermolao, A.; Zaccaria, M. Tailored exercise program reduces symptoms of upper limb work-related musculoskeletal disorders in a group of metalworkers: A randomized controlled trial. Man. Ther. 2015, 20, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Rasotto, C.; Bergamin, M.; Sieverdes, J.C.; Gobbo, S.; Alberton, C.L.; Neunhaeuserer, D.; Ermolao, A. A tailored workplace exercise program for women at risk for neck and upper limb musculoskeletal disorders: A randomized controlled trial. J. Occup. Environ. Med. 2015, 57, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Martimo, K.P.; Verbeek, J.; Karppinen, J.; Furlan, A.D.; Takala, E.P.; Kuijer, P.P.F.; Viikari-Juntura, E. Effect of training and lifting equipment for preventing back pain in lifting and handling: Systematic review. BMJ 2008, 336, 429–431. [Google Scholar] [CrossRef] [PubMed]
- Roepke, A.M.; Jayawickreme, E.; Riffle, O.M. Meaning and health: A systematic review. Appl. Res. Qual. Life 2014, 9, 1055–1079. [Google Scholar] [CrossRef]
- DeSteno, D.; Gross, J.J.; Kubzansky, L. Affective science and health: The importance of emotion and emotion regulation. Health Psychol. 2013, 32, 474–486. [Google Scholar] [CrossRef] [PubMed]
- Lally, P.; van Jaarsveld, C.; Potts, H.; Wardle, J. How are habits formed: Modelling habit formation in the real world. Eur. J. Soc. Psychol. 2010, 40, 998–1009. [Google Scholar] [CrossRef]



| Participants | Age (Years) | Body Height (cm) | Body Mass (kg) | Affiliation (Years) | ||||
|---|---|---|---|---|---|---|---|---|
| Application Field 1 (n = 51) | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Intervention (n = 29) | 36.0 | 11.7 | 176.6 | 7.6 | 83.5 | 12.3 | 9.4 | 7.9 |
| Control (n = 12) | 39.6 | 9.9 | 176.3 | 7.6 | 83.3 | 13.4 | 13.0 | 8.5 |
| Application Field 2 (n =34) | 38.9 | 9.9 | 176 | 8.8 | 81.2 | 13.8 | 8.1 | 9.75 |
| Application Field 3 (n = 174) | ||||||||
| Woman (n = 132) | 42.9 | 11.4 | 168.7 | 6.9 | 68.9 | 15.6 | n.a | |
| Men (n = 32) | 45.3 | 10.6 | 181.8 | 7.3 | 77.1 | 12.8 | n.a | |
| Application Field 1 Logistic Workers | Application Field 2 Industry Workers | Application Field 3 Office Workers | |
|---|---|---|---|
| Analysis of requirements | Slesina Questionnaire | Slesina Questionnaire | Slesina Questionnaire |
| Nordic questionnaire | Nordic questionnaire | Nordic questionnaire | |
| OWAS | OWAS | OWAS | |
| Key Indicators | Key Indicators | Key Indicators | |
| SF12 | SF12 | SF12 | |
| Muscle function | Cognitive representation | ||
| Cognitive representation | |||
| Pre-post analysis | Slesina Questionnaire | Movement analysis | Feedback (acceptance of intervention) |
| Nordic questionnaire | Cognitive representation | ||
| PILE-Test | Feedback (acceptance) | ||
| Cognitive representation | |||
| Feedback (acceptance) | |||
| Retention analysis | PILE-Test Cognitive representation | Movement analysis | Feedback (acceptance and outcomes of ongoing physical activity) |
| Cognitive representation | |||
| Feedback (acceptance) |
| Number of Feedback Responses for All Intervention Sessions (n = 143) | Yes, I Totally Agree | I Agree | No, I Disagree |
|---|---|---|---|
| Questions | (%) | (%) | (%) |
| 1. I liked the exercises. | 57 | 29 | 14 |
| 2. The exercises hindered my work. | 18 | 33 | 49 |
| 3. I think that the exercises are useful. | 64 | 26 | 10 |
| 4. Today I learnt something new. | 58 | 27 | 15 |
| 5. I remembered previous teaching of ergonomic behaviour. | 20 | 38 | 42 |
| 6. I had fun during the exercises. | 52 | 36 | 12 |
| 7. The exercises beared reference to my daily working situations. | 51 | 36 | 13 |
| 8. I was able to execute the exercises. | 50 | 38 | 12 |
| 9. The trainers explanations were clear and comprehensible. | 72 | 19 | 9 |
| 10. I was satisfied with the support I received. | 72 | 20 | 8 |
| 11. The duration of the exercises was suitable. | 33 | 46 | 21 |
| 12. I would like to get more information about health promotion. | 60 | 28 | 12 |
| Movement Phase/Cluster | Body Segment | Ergonomic Criteria of the BAC | Execution beforeIntervention (%) | Execution 9 MonthPost Intervention (%) | Chi2p-Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| No | Partly | Yes | No | Partly | Yes | ||||
Body position at the work space | Foot positon | BAC 1: feet parallel and shoulder width apart/whole foot on the floor | 0 | 82 | 18 | 0 | 27 | 73 | 60.98 |
| <0.001 | |||||||||
| knee | BAC 2: knee slightly bent | 34 | 64 | 0 | 18 | 36 | 46 | 52.42 | |
| <0.001 | |||||||||
| hip | BAC 3: hip centred over BoS | 0 | 91 | 9 | 0 | 64 | 36 | 20.9 | |
| 0.033 | |||||||||
| trunk | BAC 4: trunk in upright position/ straight back | 0 | 55 | 45 | 9 | 36 | 55 | not significant | |
Grip position of the working tool | hands | BAC 5: grip position according to the working tool | 0 | 64 | 37 | 0 | 18 | 82 | 42.82 |
| <0.001 | |||||||||
| arms | BAC 6: arms near the trunk/flexed | 0 | 73 | 27 | 0 | 18 | 82 | 60.94 | |
| <0.001 | |||||||||
| shoulders | BAC 7: shoulders lowered | 36 | 55 | 19 | 9 | 64 | 27 | n.s. | |
Working activity | hands | BAC 8: wrist joint straight and fixed | 36 | 64 | 0 | 0 | 18 | 82 | 104.98 |
| <0.001 | |||||||||
| elbow | BAC 9: elbow stays near the trunk | 46 | 46 | 8 | 0 | 9 | 91 | 91.12 | |
| <0.001 | |||||||||
| shoulder | BAC 10: shoulders stay in a lowered position | 64 | 27 | 9 | 18 | 82 | 0 | 22.19 | |
| <0.001 | |||||||||
| trunk | BAC 11: back stays straight | 9 | 55 | 36 | 9 | 55 | 36 | not significant | |
| Number of Feedback Responses for All Intervention Sessions (n = 1112) | Yes, I Totally Agree | I Agree | No, I Disagree |
|---|---|---|---|
| Questions | (%) | (%) | (%) |
| 1. I liked the exercises. | 84 | 15 | 1 |
| 2. The exercises hindered my work. | 26 | 38 | 37 |
| 3. I think that the exercises are useful. | 92 | 7 | 1 |
| 4. Today I learnt something new. | 72 | 24 | 4 |
| 5. I remembered previous teaching of ergonomic behavior. | 39 | 39 | 22 |
| 6. I had fun during the exercises. | 74 | 24 | 2 |
| 7. The exercises bore reference to my daily working situations. | 88 | 12 | 0 |
| 8. I was able to execute the exercises. | 93 | 6 | 1 |
| 9. The trainers’ explanations were clear and comprehensible. | 96 | 2 | 2 |
| 10. I was satisfied with the support I received. | 72 | 20 | 8 |
| 11. The duration of the exercises was suitable. | 51 | 40 | 9 |
| 12. I would like to get more information about health promotion. | 55 | 35 | 10 |
| Number of Feedback Responses (n = 37) | Yes, I Totally Agree | I Agree | No, I Disagree |
|---|---|---|---|
| Questions | (%) | (%) | (%) |
| 1. I liked the exercises. | 95 | 5 | 0 |
| 2. I liked the health education during the exercises. | 95 | 5 | 0 |
| 3. I think that the physical exercises are useful. | 100 | 0 | 0 |
| 4.The intervention improved my physical well-being | 92 | 8 | 0 |
| 5. The intervention improved my mental well-being | 84 | 16 | 0 |
| 6. I would like to take part in ongoing exercises at the workplace. | 92 | 8 | 0 |
| 7. The exercises beared reference to my daily working situations. | 84 | 16 | 0 |
| 8. I was able to execute the exercises. | 92 | 8 | |
| 9. The trainer explanations were clear and comprehensible. | 97 | 3 | 2 |
| 10. I would only take part in ongoing exercises if there are no fees. | 41 | 38 | 16 |
| 11. I would take part in ongoing exercises if there are fees (e.g., 25 Euro for 10 sessions). | 32 | 46 | 22 |
| 12. I would take part in ongoing exercises after working hours. | 30 | 40 | 30 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wollesen, B.; Menzel, J.; Lex, H.; Mattes, K. The BASE-Program—A Multidimensional Approach for Health Promotion in Companies. Healthcare 2016, 4, 91. https://doi.org/10.3390/healthcare4040091
Wollesen B, Menzel J, Lex H, Mattes K. The BASE-Program—A Multidimensional Approach for Health Promotion in Companies. Healthcare. 2016; 4(4):91. https://doi.org/10.3390/healthcare4040091
Chicago/Turabian StyleWollesen, Bettina, Josefine Menzel, Heiko Lex, and Klaus Mattes. 2016. "The BASE-Program—A Multidimensional Approach for Health Promotion in Companies" Healthcare 4, no. 4: 91. https://doi.org/10.3390/healthcare4040091
APA StyleWollesen, B., Menzel, J., Lex, H., & Mattes, K. (2016). The BASE-Program—A Multidimensional Approach for Health Promotion in Companies. Healthcare, 4(4), 91. https://doi.org/10.3390/healthcare4040091






