Emotional Labour and Wellbeing: What Protects Nurses?
Abstract
:1. Introduction
1.1. Benefits and Drawbacks of Delivering Compassionate Care
1.2. Emotional Labour
1.3. The Job Demands-Resources Model
1.4. The Matching Hypothesis
1.5. Emotional Support and Emotion-Focused Coping
1.6. Aims of the Study
2. Methods
2.1. Participants
2.2. Measures
2.2.1. Emotional Labour
2.2.2. Emotional Exhaustion
2.2.3. Emotional Support
2.2.4. Emotion-Focused Coping
2.3. Procedure
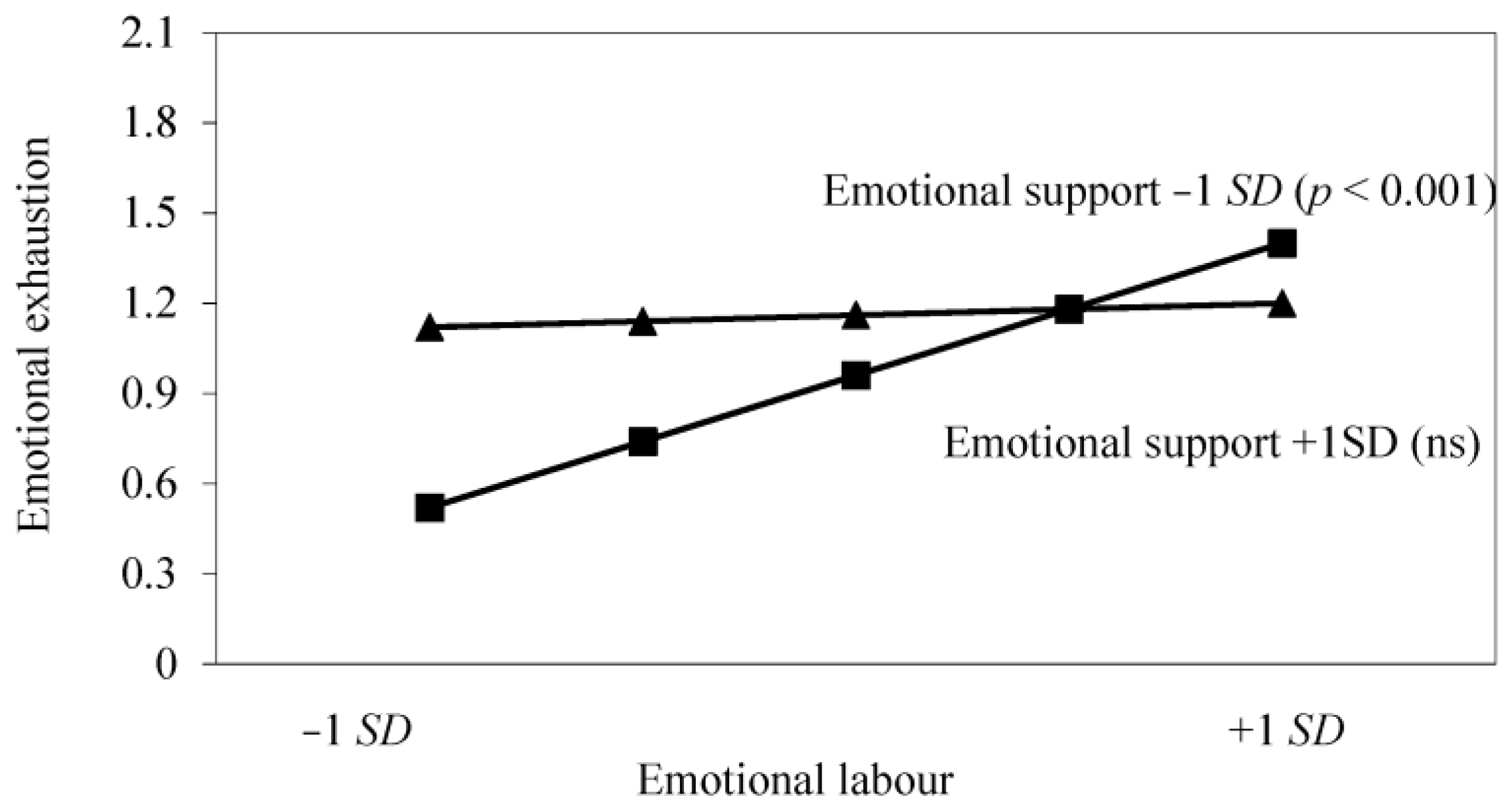
3. Results
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Chochinov, H.M. Dignity and the essence of medicine: The A, B, C and D of dignity-conserving care. BMJ 2007, 335, 184–187. [Google Scholar] [CrossRef] [PubMed]
- Bolton, S.C. Emotion here, emotion there, emotional organisations everywhere. Crit. Perspect. Account. 2000, 11, 155–171. [Google Scholar] [CrossRef]
- Fry, M.; MacGregor, C.; Ruperto, K.; Jarrett, K.; Wheeler, J.; Fong, J.; Fetchet, W. Nursing praxis, compassionate caring and interpersonal relations: An observational study. Aust. Emerg. Nurs. J. 2013, 16, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Wysong, P.R.; Driver, E. Patients’ perceptions of nurses’ skill. Crit. Care Nurse 2009, 29, 24–37. [Google Scholar] [CrossRef] [PubMed]
- Attree, M. Patients’ and relatives’ experiences and perspectives of ‘good’ and ‘not so good’ quality care. J. Adv. Nurs. 2001, 33, 456–466. [Google Scholar] [CrossRef] [PubMed]
- Hill, K. Improving quality and patient safety by retaining nursing expertise. Online J. Issues Nurs. 2010. [Google Scholar] [CrossRef]
- Firth-Cozens, J.; Cornwell, J. Enabling Compassionate Care in Acute Hospital Settings; The King’s Fund: London, UK, 2009; Available online: https://www.kingsfund.org.uk/sites/files/kf/Compassion%20report_set.pdf (accessed on 26 November 2016).
- Reader, T.W.; Gillespie, A.; Roberts, J. Patient complaints in healthcare systems: A systematic review and coding taxonomy. BMJ Qual. Saf. 2014, 23, 678–689. [Google Scholar] [CrossRef] [PubMed]
- Francis, R.; Lingard, H. Final Report. Mid Staffordshire NHS Foundation Trust Public Inquiry. 2013. Available online: http://webarchive.nationalarchives.gov.uk/20150407084003/http://www.midstaffspublicinquiry.com/report (accessed on 26 November 2016). [Google Scholar]
- GOV.UK. Patients First and Foremost: The Initial Government Response to the Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry 2013. Available online: https://www.gov.uk/government/publications/government-initial-response-to-the-mid-staffs-report (accessed on 26 November 2016).
- Kinman, G.; Grant, L. Enhancing empathy in the helping professions. In Psychology and Neurobiology of Empathy; Watt, D., Panksepp, J., Eds.; Nova Science: New York, NY, USA, 2016; pp. 297–320. [Google Scholar]
- Slocum-Gori, S.; Hemsworth, D.; Chan, W.W.; Carson, A.; Kazanjian, A. Understanding compassion satisfaction, compassion fatigue and burnout: A survey of the hospice palliative care workforce. Palliat. Med. 2013, 27, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Lilius, J.M. Recovery at work: Understanding the restorative side of “depleting” client interactions. Acad. Manag. Rev. 2012, 37, 569–588. [Google Scholar] [CrossRef]
- Health and Safety Executive. Work-Related Stress, Anxiety and Depression Statistics in Great Britain 2015. Available online: http://www.hse.gov.uk/statistics/causdis/stress/stress.pdf (accessed on 26 November 2016).
- Aiken, L.H.; Sermeus, W.; Van den Heede, K.; Sloane, D.M.; Busse, R.; McKee, M.; Bruyneel, L.; Rafferty, A.M.; Griffiths, P.; Moreno-Casbas, M.T.; et al. Patient safety, satisfaction, and quality of hospital care: Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 2012, 344. [Google Scholar] [CrossRef] [PubMed]
- McVicar, A. Workplace stress in nursing: A literature review. J. Adv. Nurs. 2003, 44, 633–642. [Google Scholar] [CrossRef] [PubMed]
- Bakker, A.B.; Sanz-Vergel, A. Weekly work engagement and flourishing: The role of hindrance and challenge job demands. J. Vocat. Behav. 2013, 83, 397–409. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S. MBI-Human Services Survey; CPP. Mountain View: San Francisco, CA, USA, 1996. [Google Scholar]
- Poghosyan, L.; Clarke, S.; Finlayson, M.; Aiken, L. Nurse burnout and quality of care: Cross-national investigation in six countries. Res. Nurs. Health 2010, 33, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Morris, J.; Feldman, D.C. Managing emotions in the workplace. J. Manag. Issues 1997, 1, 257–274. [Google Scholar]
- Hochschild, A.R. The Managed Heart: Commercialization of Human Feeling; University of California Press: Berkeley, CA, USA, 2003. [Google Scholar]
- Zapf, D. Emotion work and psychological well-being: A review of the literature and some conceptual considerations. Hum. Resour. Manag. Rev. 2002, 12, 237–268. [Google Scholar] [CrossRef]
- Grandey, A.A. Emotional regulation in the workplace: A new way to conceptualize emotional labor. J. Occup. Health Psychol. 2000, 5, 95–110. [Google Scholar] [CrossRef] [PubMed]
- Bolton, S. Changing faces: Nurses as emotional jugglers. Sociol. Health Illn. 2001, 23, 85–100. [Google Scholar] [CrossRef]
- Mann, S.; Cowburn, J. Emotional labour and stress within mental health nursing. J. Psychiatr. Ment. Health Nurs. 2005, 12, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Gray, B. The emotional labour of nursing—Defining and managing emotions in nursing work. Nurs. Educ. Today 2009, 29, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Chou, H.Y.; Hecker, R.O.; Martin, A. Predicting nurses’ well-being from job demands and resources: A cross-sectional study of emotional labour. J. Nurs. Manag. 2012, 20, 502–511. [Google Scholar] [CrossRef] [PubMed]
- Grandey, A.; Foo, S.C.; Groth, M.; Goodwin, R.E. Free to be you and me: A climate of authenticity alleviates burnout from emotional labor. J. Occup. Health Psychol. 2012, 17, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Strazdins, L.M. Integrating emotions: Multiple role measurement of emotional work. Aust. J. Psychol. 2000, 52, 41–50. [Google Scholar] [CrossRef]
- Diefendorff, J.M.; Erickson, R.J.; Grandey, A.A.; Dahling, J.J. Emotional display rules as work unit norms: A multilevel analysis of emotional labor among nurses. J. Occup. Health Psychol. 2011, 16, 170–186. [Google Scholar] [CrossRef] [PubMed]
- Bolton, S.C. Emotion Management in the Workplace; Palgrave Macmillan: London, UK, 2004. [Google Scholar]
- Donoso, L.M.; Demerouti, E.; Hernández, E.G.; Moreno-Jiménez, B.; Cobo, I.C. Positive benefits of caring on nurses’ motivation and well-being: A diary study about the role of emotional regulation abilities at work. Int. J. Nurs. Stud. 2015, 52, 804–816. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.; Laschinger, H.S.; Wong, C. Workplace empowerment, work engagement and organizational commitment of new graduate nurses. Nurs. Leadersh. 2006, 19, 43–60. [Google Scholar] [CrossRef]
- Erickson, R.J.; Grove, W.J. Emotional labor and health care. Sociol. Comp. 2008, 2, 704–733. [Google Scholar] [CrossRef]
- Msiska, G.; Smith, P.; Fawcett, T. Exposing emotional labour experienced by nursing students during their clinical learning experience: A Malawian perspective. Int. J. Afr. Nurs. Sci. 2014, 1, 43–50. [Google Scholar] [CrossRef]
- Demerouti, E.; Bakker, A.B.; Nachreiner, F.; Schaufeli, W.B. The job demands-resources model of burnout. J. Appl. Psychol. 2001, 86, 499–512. [Google Scholar] [CrossRef] [PubMed]
- Bakker, A.B.; Demerouti, E.; Taris, T.W.; Schaufeli, W.B.; Schreurs, P.J. A multigroup analysis of the job demands-resources model in four home care organizations. Int. J. Stress Manag. 2003, 10, 16–38. [Google Scholar] [CrossRef]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1989, 8, 310–357. [Google Scholar] [CrossRef]
- De Jonge, J.; Dormann, C. The DISC model: Demand-induced strain compensation mechanisms in job stress. In Occupational Stress in the Service Professions; Dollard, M., Winefield, A., Winefield, H., Eds.; Taylor & Francis: London, UK, 2003; pp. 43–74. [Google Scholar]
- De Jonge, J.; Dormann, C. Stressors, resources, and strain at work: A longitudinal test of the triple-match principle. J. Appl. Psychol. 2006, 91, 1359–1374. [Google Scholar] [CrossRef] [PubMed]
- Chrisopoulos, S.; Dollard, M.; Winefield, A.; Dormann, C. Increasing the probability of finding an interaction in work-stress research; a two wave longitudinal test of the triple-match principle. J. Occup. Organ. Psychol. 2010, 1, 17–37. [Google Scholar] [CrossRef]
- Van den Tooren, M.; de Jong, E.J. Managing job stress in nursing: What kind of resources do we need? J. Adv. Nurs. 2008, 63, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Van de Ven, B.; Vlerick, P. Testing the triple-match principle among technology employees. Eur. J. Work Organ. Psychol. 2013, 22, 658–669. [Google Scholar] [CrossRef]
- Lavoie-Tremblay, M.; Trépanier, S.G.; Fernet, C.; Bonneville-Roussy, A. Testing and extending the triple match principle in the nursing profession: A generational perspective on job demands, job resources and strain at work. J. Adv. Nurs. 2014, 70, 310–322. [Google Scholar] [CrossRef] [PubMed]
- Ozbay, F.; Fitterling, H.; Charney, D.; Southwick, S. Social support and resilience to stress across the life span: A neurobiologic framework. Curr. Psychiatry Rep. 2008, 10, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Grant, L.; Kinman, G. The Importance of Resilience for Staff and Students in the ‘Helping’ Professions: Developing an Emotional Curriculum; Higher Education Academy: York, UK, 2014; Available online: https://www.heacademy.ac.uk/sites/default/files/emotional_resilience_louise_grant_march_2014_0.pdf (accessed on 26 November 2016).
- Drury, V.; Craigie, M.; Francis, K.; Aoun, S.; Hegney, D. Compassion satisfaction, compassion fatigue, anxiety, depression and stress in registered nurses in Australia: Phase 2 results. J. Nurs. Manag. 2014, 22, 519–531. [Google Scholar] [CrossRef] [PubMed]
- Baruch-Feldman, C.; Brondolo, E.; Ben-Dayan, D.; Schwartz, J. Sources of social support and burnout, job satisfaction, and productivity. J. Occup. Health Psychol. 2002, 7, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.; Folkman, S. Stress Appraisal and Coping 1984; Springer: New York, NY, USA, 1984. [Google Scholar]
- Arieli, D. Emotional work and diversity in clinical placements of nursing students. J. Nurs. Scholarsh. 2013, 45, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.M.; Bidewell, J.W.; Huntington, A.D.; Daly, J.; Johnson, A.; Wilson, H.; Lambert, V.A.; Lambert, C.E. A survey of role stress, coping and health in Australian and New Zealand hospital nurses. Int. J. Nurs. Stud. 2007, 44, 1354–1362. [Google Scholar] [CrossRef] [PubMed]
- Lambert, V.A.; Lambert, C.E. Nurses’ workplace stressors and coping strategies. Indian J. Palliat. Care 2008, 14, 38–44. [Google Scholar] [CrossRef]
- Kato, T. Coping with interpersonal stress and psychological distress at work: Comparison of hospital nursing staff and salespeople. Psychol. Res. Behav. Manag. 2014, 7, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Van der Colff, J.J.; Rothmann, S. Occupational stress of professional nurses in South Africa. J. Psychol. Afr. 2014, 24, 375–384. [Google Scholar]
- Dewe, P.; O’Driscoll, M.; Cooper, C. Coping with Work Stress: A Review and Critique; Wiley-Blackwell: London, UK, 2010. [Google Scholar]
- Strickland, B. Catharsis; Gale: Farmington Hills, MI, USA, 2001. [Google Scholar]
- Pennebaker, J.; Evans, J. Expressive Writing: Words That Heal 2014; Idyll Arbor: Enumclaw, WA, USA, 2014. [Google Scholar]
- Stanton, A.L.; Danoff-Burg, S.; Cameron, C.L.; Bishop, M.; Collins, C.A.; Kirk, S.B.; Sworowski, L.A.; Twillman, R. Emotionally expressive coping predicts psychological and physical adjustment to breast cancer. J. Consult. Clin. Psychol. 2000, 68, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Grandey, A. When “the show must go on”: Surface acting and deep acting as determinants of emotional exhaustion and peer-rated service delivery. Acad. Manag. J. 2003, 46, 86–96. [Google Scholar] [CrossRef]
- Zapf, D.; Vogt, C.; Seifert, C.; Mertini, H.; Isic, A. Emotion work as a source of stress: The concept and development of an instrument. Eur. J. Work Organ. Psychol. 1999, 8, 371–400. [Google Scholar] [CrossRef]
- Carver, C.S.; Scheier, M.F.; Weintraub, J.K. Assessing coping strategies: A theoretically-based approach. J. Personal. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Aiken, L.H.; Clarke, S.P.; Sloane, D.M.; Sochalski, J.; Silber, J.H. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 2002, 288, 1987–1993. [Google Scholar] [CrossRef] [PubMed]
- Harwood, L.; Ridley, J.; Wilson, B.; Laschinger, H.K. Occupational burnout, retention and health outcomes in nephrology nurses. CANNT J. 2009, 20, 18–23. [Google Scholar]
- Vahey, D.; Aiken, L.; Sloane, D.; Clarke, S.P.; Vargas, D. Nurse burnout and patient satisfaction. Med. Care 2004, 42, 1157–1166. [Google Scholar] [CrossRef] [PubMed]
- Wood, C. Choosing the ‘right’ people for nursing: Can we recruit to care? Br. J. Nurs. 2014, 23, 528–530. [Google Scholar] [CrossRef] [PubMed]
- Görgens-Ekermans, G.; Brand, T. Emotional intelligence as a moderator in the stress-burnout relationship: A questionnaire study on nurses. J. Clin. Nurs. 2012, 21, 2275–2285. [Google Scholar] [CrossRef] [PubMed]
- Burridge, L.H.; Winch, S.; Kay, M.; Henderson, A. Building compassion literacy: Enabling care in primary health care nursing. Collegian 2015. [Google Scholar] [CrossRef]
- Cheng, C.; Bartram, T.; Karimi, L.; Leggat, S.G. The role of team climate in the management of emotional labour: Implications for nurse retention. J. Adv. Nurs. 2013, 69, 2812–2824. [Google Scholar] [CrossRef] [PubMed]
- Winch, S.; Henderson, A.; Kay, M.; Burridge, L.; Livesay, G.; Sinnott, M. Understanding compassion literacy in nursing through a clinical compassion café. J. Contin. Educ. Nurs. 2014, 45, 484–486. [Google Scholar] [PubMed]
- Sundin, L.; Hochwälder, J.; Bildt, C.; Lisspers, J. The relationship between different work-related sources of social support and burnout among registered and assistant nurses in Sweden: A questionnaire survey. Int. J. Nurs. Stud. 2007, 44, 758–769. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.; Gray, B. Emotional labour of nursing revisited: Caring and learning. Nurse Educ. Pract. 2001, 1, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Sergeant, J.; Laws-Chapman, C. Creating a positive workplace culture. Nurse Manag. 2012, 18, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, A.; Bell, A. Peer learning partnerships: Exploring the experience of pre-registration nursing students. J. Clin. Nurs. 2010, 24, 803–810. [Google Scholar] [CrossRef] [PubMed]
- Baker, S.; Jones, K. Peer support and peer coaching. In Developing Resilience for Social Work Practice; Grant, L., Kinman, G., Eds.; Palgrave: London, UK, 2014; pp. 128–147. [Google Scholar]
- Short, E.; Kinman, G.; Baker, S. Evaluating the impact of a peer coaching intervention on wellbeing among psychology graduates. Int. Coach. Psychol. Rev. 2010, 5, 27–35. [Google Scholar]
- Smyth, J.; Pennebaker, J.; Arigo, D. What are the health effects of disclosure? In Handbook of Health Psychology; Baum, A., Revenson, R., Singer, J., Eds.; Taylor & Francis: London, UK, 2012; pp. 175–192. [Google Scholar]
- Sexton, J.D.; Pennebaker, J.W. The healing powers of expressive writing. In The Psychology of Creative Writing; Kaufman, S., Kaufman, J., Eds.; Cambridge University Press: New York, NY, USA, 2009; pp. 64–73. [Google Scholar]
- Grant, L.; Kinman, G.; Alexander, K. What’s all this talk about emotion? Developing emotional intelligence in social work students. Soc. Work Educ. 2014, 33, 874–889. [Google Scholar] [CrossRef]
- Misra-Hebert, A.D.; Isaacson, J.H.; Kohn, M.; Hull, A.L.; Hojat, M.; Papp, K.K.; Calabrese, L. Improving empathy of physicians through guided reflective writing. Int. J. Med. Educ. 2012, 3, 71–77. [Google Scholar] [CrossRef]
- Lee, Y.; Seomun, G. Development and validation of an instrument to measure nurses’ compassion competence. Appl. Nurs. Res. 2016, 30, 76–82. [Google Scholar] [CrossRef] [PubMed]

| Study Variables | M | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| 1. Emotional labour | 3.36 | 0.46 | 1.0 | |||
| 2. Emotional exhaustion | 4.24 | 0.96 | 0.36 *** | 1.0 | ||
| 3. Emotional support | 3.93 | 0.68 | −0.22 ** | −0.34 *** | 1.0 | |
| 4. Emotion-focused coping | 2.04 | 0.41 | −0.21 ** | −0.23 ** | 0.24 ** | 1.0 |
| Emotional Support as Moderator between Emotional Labour and Emotional Exhaustion | |||
| Predictor | Step 1 | Step 2 | Step 3 |
| Job experience | 0.02 ** | 0.01 | 0.01 |
| Emotional labour | 0.20 ** | 0.32 ** | |
| Emotion-focused coping | −0.23 *** | −0.21 ** | |
| Interaction (a × b) | 0.22 ** | ||
| Total R2 | 0.03 ** | 23 *** | 0.03 ** |
| Emotion-Focused Coping as Moderator between Emotional Labour and Emotional Exhaustion | |||
| Predictor | Step 1 | Step 2 | Step 3 |
| Job experience | 0.02 ** | 0.01 * | 0.01 * |
| Emotional labour | 0.43 *** | 0.16 ** | |
| Emotional support | −0.35 *** | −0.63 *** | |
| Interaction (a × b) | 0.18 ** | ||
| Total R2 | 0.03 *** | 0.54 *** | 0.02 ** |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kinman, G.; Leggetter, S. Emotional Labour and Wellbeing: What Protects Nurses? Healthcare 2016, 4, 89. https://doi.org/10.3390/healthcare4040089
Kinman G, Leggetter S. Emotional Labour and Wellbeing: What Protects Nurses? Healthcare. 2016; 4(4):89. https://doi.org/10.3390/healthcare4040089
Chicago/Turabian StyleKinman, Gail, and Sandra Leggetter. 2016. "Emotional Labour and Wellbeing: What Protects Nurses?" Healthcare 4, no. 4: 89. https://doi.org/10.3390/healthcare4040089
APA StyleKinman, G., & Leggetter, S. (2016). Emotional Labour and Wellbeing: What Protects Nurses? Healthcare, 4(4), 89. https://doi.org/10.3390/healthcare4040089





