Justice and Equity Implications of Climate Change Adaptation: A Theoretical Evaluation Framework
Abstract
:1. Introduction: Climate Change Affects Human Health
2. The Need for an Alternative Framework: Evaluation Problems and the Precautionary Principle
Causality as an Evaluation Problem
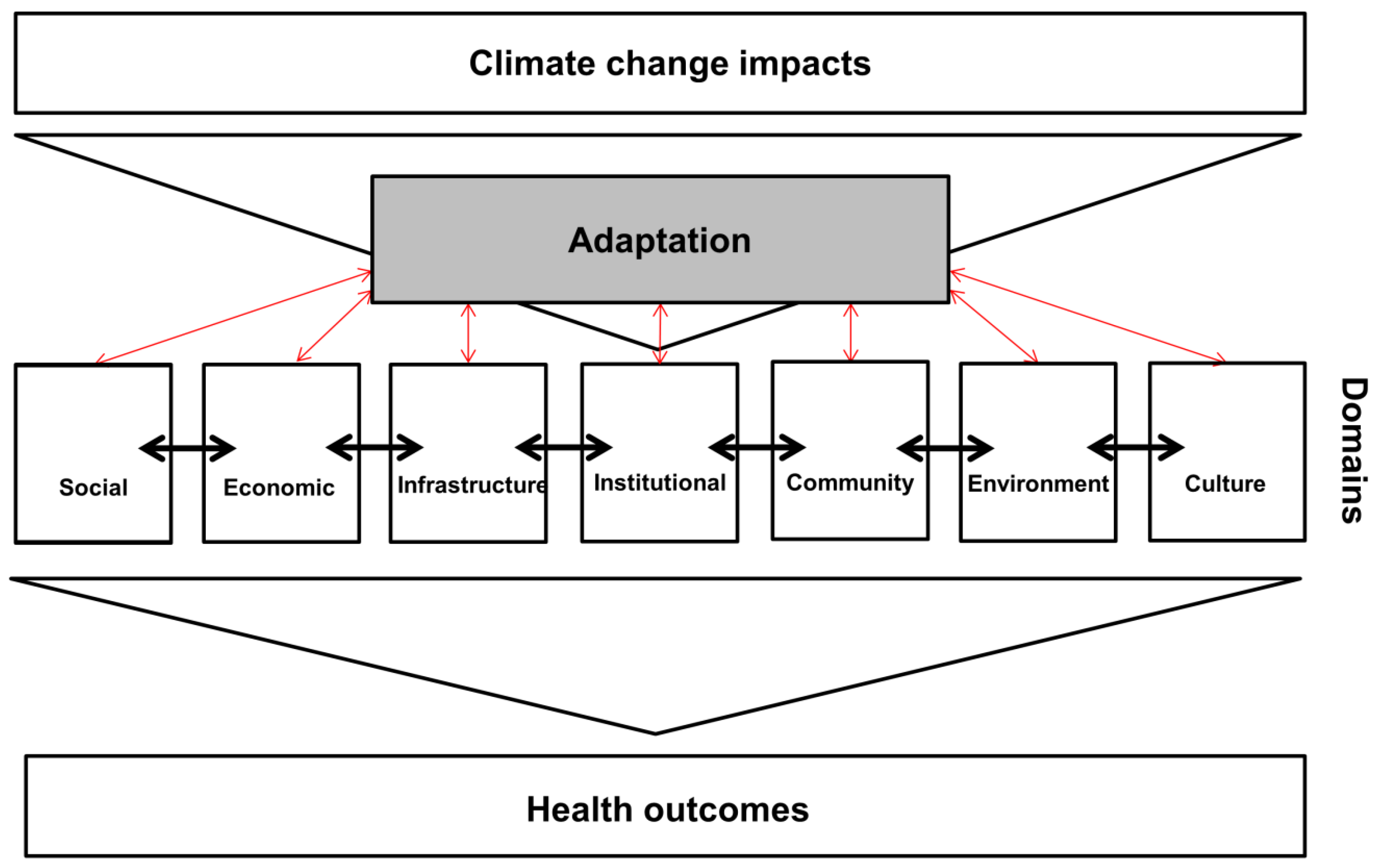
3. Results: A Theoretical Framework for Adaptation Evaluation Based on Social and Environmental Health Determinants
4. Framework Application
Example: Applying the Framework to an Adaptation Action Plan
5. Discussion
6. Challenges to Framework Application
7. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Smith, K.R.; Woodward, A.; Campbell-Lendrum, D.; Chadee, D.; Honda, Y.; Liu, Q.; Olwoch, J.; Revich, B.; Sauerborn, R. Human health: Impacts, adaptation and co-benefits. In Climate Change 2014: Impacts, Adaptation and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Field, C.B., Barros, V.R., Dokken, D.J., Mach, K.J., Mastrandrea, M.D., Bilir, T.E., Chatterjee, M., Ebi, K.L., Estrada, Y.O., Genova, R.C., et al., Eds.; Cambridge University Press: Cambridge, NY, USA, 2014; pp. 709–754. [Google Scholar]
- Kjellstrom, T.; McMichael, A.J. Climate change threats to population health and well-being: The imperative of protective solutions that will last. Glob. Health Action 2013. [Google Scholar] [CrossRef] [PubMed]
- Frumkin, H.; McMichael, A.J.; Hess, J.J. Climate change and the health of the public. Am. J. Prev. Med. 2008, 35, 401–402. [Google Scholar] [CrossRef] [PubMed]
- Gardiner, S.M.; Hartzell-Nichols, L. Ethics and Global Climate Change. Available online: http://www.nature.com/scitable/knowledge/library/ethics-and-global-climate-change-84226631 (accessed on 29 August 2016).
- Wilson, S.M.; Richard, R.; Joseph, L.; Williams, E. Climate Change, Environmental Justice, and Vulnerability: An Exploratory Spatial Analysis. Environ. Justice 2010, 3, 13–19. [Google Scholar] [CrossRef]
- Bulkeley, H.; Edwards, G.A.S.; Fuller, S. Contesting climate justice in the city: Examining politics and practice in urban climate change experiments. Glob. Environ. Chang. 2014, 25, 31–40. [Google Scholar] [CrossRef]
- Zehetmair, S. Societal Aspects of Vulnerability to Natural Hazards. Raumforsch. Raumordn. 2012, 70, 273–284. [Google Scholar] [CrossRef]
- Thomalla, F.; Downing, T.; Spanger-Siegfried, E.; Han, G.; Rockström, J. Reducing hazard vulnerability: Towards a common approach between disaster risk reduction and climate adaptation. Disasters 2006, 30, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Birkmann, J.; Kienberger, S.; Alexander, D.E. Assessment of Vulnerability to Natural Hazards: A European Perspective; Elsevier: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Handmer, J.; Honda, Y.; Kundzewicz, Z.W.; Arnell, N.; Benito, G.; Hatfield, J.; Mohamed, I.F.; Peduzzi, P.; Wu, S.; Sherstyukov, B.; et al. Changes in impacts of climate extremes: Human systems and ecosystems. In Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation. A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change (IPCC); Field, C.B., Barros, V., Stocker, T.F., Qin, D., Dokken, D.J., Ebi, K.L., Mastrandrea, M.D., Mach, K.J., Plattner, G.-K., Allen, S.K., et al., Eds.; Cambridge University Press: Cambridge, NY, USA, 2012; pp. 231–290. [Google Scholar]
- IPCC. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation. A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change; Field, C.B., Barros, V., Stocker, T.F., Qin, D., Dokken, D., Ebi, K.L., Mastrandrea, M.D., Mach, K.J., Plattner, G.-K., Allen, S.K., et al., Eds.; Cambridge University Press: Cambridge, NY, USA, 2012. [Google Scholar]
- Adger, W.N.; Barnett, J.; Brown, K.; Marshall, N.; O’Brien, K. Cultural dimensions of climate change impacts and adaptation. Nat. Clim. Chang. 2013, 3, 112–117. [Google Scholar] [CrossRef]
- Harlan, S.L.; Brazel, A.J.; Prashad, L.; Stefanov, W.L.; Larsen, L. Neighborhood microclimates and vulnerability to heat stress. Soc. Sci. Med. 2006, 63, 2847–2863. [Google Scholar] [CrossRef] [PubMed]
- Schaffer, A.; Muscatello, D.; Broome, R.; Corbett, S.; Smith, W. Emergency department visits, ambulance calls, and mortality associated with an exceptional heat wave in Sydney, Australia, 2011: A time-series analysis. Environ. Health 2012. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Barnett, A.G.; Wang, X.; Tong, S. Effects of extreme temperatures on years of life lost for cardiovascular deaths: A time series study in Brisbane, Australia. Circ. Cardiovasc. Qual. Outcomes 2012, 5, 609–614. [Google Scholar] [CrossRef] [PubMed]
- Bélanger, D.; Gosselin, P.; Valois, P.; Abdous, B. Perceived Adverse Health Effects of Heat and Their Determinants in Deprived Neighbourhoods: A Cross-Sectional Survey of Nine Cities in Canada. Int. J. Environ. Res. Public Health 2014, 11, 11028–11053. [Google Scholar] [CrossRef] [PubMed]
- Jesdale, B.M.; Morello-frosch, R.; Cushing, L. The racial/ethnic distribution of heat risk-related land cover in relation to residential segregation. Environ. Health Perspect. 2013, 121, 811–817. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Social Dimensions of Climate Change; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- World Health Organization. Atlas of Health and Climate; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Sovacool, B.K. Adaptation: The complexity of climate justice. Nat. Clim. Chang. 2013, 3, 959–960. [Google Scholar] [CrossRef]
- Schlosberg, D.; Collins, L.B. From environmental to climate justice: Climate change and the discourse of environmental justice. Wiley Interdiscip. Rev. Clim. Chang. 2014, 5, 359–374. [Google Scholar] [CrossRef]
- Lee, C. Environmental justice. In Environmental Health: From Global to Local; Frumkin, H., Ed.; Jossey-Bass: San Francisco, CA, USA, 2010; pp. 227–256. [Google Scholar]
- Biagini, B.; Bierbaum, R.; Stults, M.; Dobardzic, S.; McNeeley, S.M. A typology of adaptation actions: A global look at climate adaptation actions financed through the Global Environment Facility. Glob. Environ. Chang. 2014, 25, 97–108. [Google Scholar] [CrossRef]
- Bouzid, M.; Hooper, L.; Hunter, P.R. The effectiveness of public health interventions to reduce the health impact of climate change: A systematic review of systematic reviews. PLoS ONE 2013, 8, e62041. [Google Scholar] [CrossRef] [PubMed]
- Boeckmann, M.; Rohn, I. Is planned adaptation to heat reducing heat-related mortality and illness? A systematic review. BMC Public Health 2014. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.J.; Berry, P. Health co-benefits and risks of public health adaptation strategies to climate change: A review of current literature. Int. J. Public Health 2013, 58, 305–311. [Google Scholar] [CrossRef] [PubMed]
- McDonald, Y.J.; Grineski, S.E.; Collins, T.W.; Kim, Y.-A. A scalable climate health justice assessment model. Soc. Sci. Med. 2015, 133, 242–252. [Google Scholar] [CrossRef] [PubMed]
- Brown, H.; Spickett, J. Health Consequence Scales for Use in Health Impact Assessments of Climate Change. Int. J. Environ. Res. Public Health 2014, 11, 9607–9620. [Google Scholar] [CrossRef] [PubMed]
- Blankenship, K.M.; Friedman, S.R.; Dworkin, S.; Mantell, J.E. Structural interventions: Concepts, challenges and opportunities for research. J. Urban Health 2006, 83, 59–72. [Google Scholar] [CrossRef] [PubMed]
- Broadbent, A. Epidemiology, risk and causation. In Conceptual and Methodological Issues in Public Health Science; Cambridge University Press: Cambridge, UK, 2011. [Google Scholar]
- Broadbent, A. Inferring causation in epidemiology: Mechanisms, black boxes, and contrasts. In Causality in the Sciences; McKay, P.I., Russo, F., Williamson, J., Eds.; Oxford University Press: Oxford, UK, 2011; pp. 45–69. [Google Scholar]
- Pearl, J. Causality: Models, Reasoning, and Inference, 2nd ed.; Cambridge University Press: Cambridge, UK, 2009. [Google Scholar]
- Toloo, G.; Fitzgerald, G.; Aitken, P.; Verrall, K.; Tong, S. Evaluating the effectiveness of heat warning systems: Systematic review of epidemiological evidence. Int. J. Public Health 2013, 58, 667–681. [Google Scholar] [CrossRef] [PubMed]
- Craig, P.; Cooper, C.; Gunnell, D.; Haw, S.; Lawson, K.; Macintyre, S.; Ogilvie, D.; Petticrew, M.; Reeves, B.; Sutton, M.; et al. Using natural experiments to evaluate population health interventions: New Medical Research Council guidance. J. Epidemiol. Community Health 2012, 66, 1182–1186. [Google Scholar] [CrossRef] [PubMed]
- Benmarhnia, T.; Bailey, Z.; Kaiser, D.; Auger, N.; King, N.; Kaufman, J. A Difference-in-Differences Approach to Assess the Effect of a Heat Action Plan on Heat-Related Mortality, and Differences in Effectiveness According to Gender, Age, and Socioeconomic Status (Montreal, Quebec). Environ. Health Perspect. 2016. [Google Scholar] [CrossRef] [PubMed]
- Movsisyan, A.; Melendez-Torres, G.J.; Montgomery, P. Outcomes in systematic reviews of complex interventions never reached “high” GRADE ratings when compared to those of simple interventions. J. Clin. Epidemiol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, J.Ø.; D’haen, S.A.L. Asking about climate change: Reflections on methodology in qualitative climate change research published in Global Environmental Change since 2000. Glob. Environ. Chang. 2014, 24, 402–409. [Google Scholar] [CrossRef]
- Paschen, J.-A.; Ison, R. Narrative research in climate change adaptation—Exploring a complementary paradigm for research and governance. Res. Policy 2014, 43, 1083–1092. [Google Scholar] [CrossRef]
- Gould, S.; Rudolph, L. Challenges and Opportunities for Advancing Work on Climate Change and Public Health. Int. J. Environ. Res. Public Health 2015, 12, 15649–15672. [Google Scholar] [CrossRef] [PubMed]
- Silverman, D. Doing Qualitative Research, 3rd ed.; SAGE Publications: Los Angeles, CA, USA, 2011. [Google Scholar]
- World Health Organization. The Precautionary Principle: Protecting Public Health, the Environment and the Future of our Children; Martuzzi, M., Tickner, J.A., Eds.; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2004. [Google Scholar]
- Allwood, J.M.; Bosetti, V.; Dubash, N.K.; Gómez-Echeverri, L.; von Stechow, C. Climate Change 2014: Mitigation of Climate Change. Contribution of Working Group III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Edenhofer, O., Pichs-Madruga, R., Sokona, Y., Farahani, E., Kadner, S., Seyboth, K., Adler, A., Baum, I., Brunner, S., Eickemeier, P., et al., Eds.; Cambridge University Press: Cambridge, NY, USA, 2014; pp. 1249–1279. [Google Scholar]
- Frumkin, H.; Hess, J.; Luber, G.; Malilay, J.; McGeehin, M. Climate change: The public health response. Am. J. Public Health 2008, 98, 435–445. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.; O’Riordan, T. The precautionary principle in contemporary environmental policy and politics. In Protecting Public Health and the Environment: Implementing The Precautionary Principle; Raffensperger, C., Tickner, J.A., Eds.; Island Press: Washington, DC, USA, 1999; pp. 15–35. [Google Scholar]
- Barrett, S. Local level climate justice? Adaptation finance and vulnerability reduction. Glob. Environ. Chang. 2013, 23, 1819–1829. [Google Scholar] [CrossRef]
- Boeckmann, M.; Zeeb, H. Using a social justice and health framework to assess European climate change adaptation strategies. Int. J. Environ. Res. Public Health 2014, 11, 12389–12411. [Google Scholar] [CrossRef] [PubMed]
- Gostin, L.O.; Powers, M. What does social justice require for the public’s health? Public health ethics and policy imperatives. Health Aff. 2006, 25, 1053–1060. [Google Scholar] [CrossRef] [PubMed]
- Asada, Y. A framework for measuring health inequity. J. Epidemiol. Community Health 2005, 59, 700–705. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.; Allen, J.; Bell, R.; Bloomer, E.; Goldblatt, P. WHO European review of social determinants of health and the health divide. Lancet 2012, 380, 1011–1129. [Google Scholar] [CrossRef]
- Friel, S.; Hancock, T.; Kjellstrom, T.; McGranahan, G.; Monge, P.; Roy, J. Urban health inequities and the added pressure of climate change: An action-oriented research agenda. J. Urban Health 2011, 88, 886–895. [Google Scholar] [CrossRef] [PubMed]
- Janssen, M.A.; Ostrom, E. Resilience, vulnerability, and adaptation: A cross-cutting theme of the International Human Dimensions Programme on Global Environmental Change. Glob. Environ. Chang. 2006, 16, 237–239. [Google Scholar] [CrossRef]
- Seaman, P.; McNeice, V.; Yates, G.; McLean, J. Resilience for Public Health: Supporting Transformation in People and Communities; Glasgow Centre for Population Health: Glasgow, UK, 2014. [Google Scholar]
- Cutter, S.L.; Ash, K.D.; Emrich, C.T. The geographies of community disaster resilience. Glob. Environ. Chang. 2014, 29, 65–77. [Google Scholar] [CrossRef]
- Napier, A.D.; Ancarno, C.; Butler, B.; Calabrese, J.; Chater, A.; Chatterjee, H.; Guesnet, F.; Horne, R.; Jacyna, S.; Jadhav, S.; et al. Culture and health. Lancet 2014, 384, 1607–1639. [Google Scholar] [CrossRef]
- Suhrcke, M.; de Paz Nieves, C. The Impact of Health and Health Behaviours on Educational Outcomes in High Income Countries: A Review of the Evidence; World Health Organization: Copenhagen, Denmark, 2011. [Google Scholar]
- Ahnquist, J.; Wamala, S.P.; Lindstrom, M. Social determinants of health—A question of social or economic capital? Interaction effects of socioeconomic factors on health outcomes. Soc. Sci. Med. 2012, 74, 930–939. [Google Scholar] [CrossRef] [PubMed]
- Feliciano, D.; Berkhout, F. Dealing with “wicked” environmental problems. In World Social Science Report 2013: Changing Global Environments; International Social Science Council and UNESCO: Paris, Franch, 2013; pp. 415–419. [Google Scholar]
- Nagel, J. Intersecting identities and global climate change. Identities 2012, 19, 467–476. [Google Scholar] [CrossRef]
- World Health Organization. Gender, Climate Change and Health; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Kaijser, A.; Kronsell, A. Climate change through the lens of intersectionality. Env. Polit. 2013, 23, 417–433. [Google Scholar] [CrossRef]
- Bunce, A.; Ford, J. How is adaptation, resilience, and vulnerability research engaging with gender? Environ. Res. Lett. 2015. [Google Scholar] [CrossRef]
- Preet, R.; Nilsson, M.; Schumann, B.; Evengård, B. The gender perspective in climate change and global health. Glob. Health Action 2010. [Google Scholar] [CrossRef] [PubMed]
- Bauer, G.R. Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Soc. Sci. Med. 2014, 110, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Bolte, G. Gender in epidemiology. State of discussion and perspectives. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2008, 51, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Springer, K.W.; Hankivsky, O.; Bates, L.M. Gender and health: Relational, intersectional, and biosocial approaches. Soc. Sci. Med. 2012, 74, 1661–1666. [Google Scholar] [CrossRef] [PubMed]
- Bee, B. Who Reaps what is Sown? A Feminist Inquiry into Climate Change Adaptation in Two Mexican Ejidos. ACME 2013, 12, 131–154. [Google Scholar]
- English, P.B.; Sinclair, A.H.; Ross, Z.; Anderson, H.; Boothe, V.; Davis, C.; Ebi, K.; Kagey, B.; Malecki, K.; Shultz, R.; et al. Environmental health indicators of climate change for the United States: Findings from the State Environmental Health Indicator Collaborative. Environ. Health Perspect. 2009, 117, 1673–1681. [Google Scholar] [CrossRef] [PubMed]
- Ford, J.D.; Berrang-Ford, L.; Lesnikowski, A.; Barrera, M.; Heymann, S.J. How to track adaptation to climate change: A typology of approaches for national-level application. Ecol. Soc. 2013. [Google Scholar] [CrossRef]
- Bundesministerium für Land-und Forstwirtschaft Umwelt und Wasserwirtschaft. Die österreichische Strategie zur Anpassung an den Klimawandel. Teil 2—Aktionsplan Handlungsempfehlungen für die Umsetzung; Bundesministerium für Land-und Forstwirtschaft Umwelt und Wasserwirtschaft: Vienna, Austria, 2012. (In German) [Google Scholar]
- Resnik, D.B. Environmental Health Ethics; Cambridge University Press: Cambridge, NY, USA, 2012. [Google Scholar]
- Kruize, H.; Droomers, M.; van Kamp, I.; Ruijsbroek, A. What Causes Environmental Inequalities and Related Health Effects? An Analysis of Evolving Concepts. Int. J. Environ. Res. Public Health 2014, 11, 5807–5827. [Google Scholar] [CrossRef] [PubMed]
- Hall, M.J. Advancing climate justice and the right to health through procedural rights. Health Hum. Rights 2014, 16, 8–18. [Google Scholar] [PubMed]
- Clarke, J. Climate Change and Gender Justice. Health Promot. J. Aust. 2011, 22, S73–S73. [Google Scholar]
- Horton, R.; Beaglehole, R.; Bonita, R.; Raeburn, J.; McKee, M.; Wall, S. From public to planetary health: A manifesto. Lancet 2014. [Google Scholar] [CrossRef]
- Gahagan, J.; Gray, K.; Whynacht, A. Sex and gender matter in health research: Addressing health inequities in health research reporting. Int. J. Equity Health 2015. [Google Scholar] [CrossRef] [PubMed]
- Bendlin, L. Women’s human rights in a changing climate: Highlighting the distributive effects of climate policies. Camb. Rev. Int. Aff. 2014, 27, 680–698. [Google Scholar] [CrossRef]
- Johnson, J.L.; Greaves, L.; Repta, R. Better science with sex and gender: Facilitating the use of a sex and gender-based analysis in health research. Int. J. Equity Health 2009. [Google Scholar] [CrossRef] [PubMed]
- Hammarström, A.; Johansson, K.; Annandale, E.; Ahlgren, C.; Aléx, L.; Christianson, M.; Elwér, S.; Eriksson, C.; Fjellman-Wiklund, A.; Gilenstam, K.; et al. Central gender theoretical concepts in health research: The state of the art. J. Epidemiol. Community Health 2014, 68, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, M.J. Beside My Sister, Facing the Enemy: Legal Theory out of Coalition. Stanf. Law Rev. 1991, 43, 1183–1192. [Google Scholar] [CrossRef]
- Bolte, G.; Lahn, U. Geschlecht in der Public-Health-Forschung zu gesundheitlichen Ungleichheiten: Potenziale und Begrenzungen des Intersektionalitätsansatzes. Gend.—Zeitschrift Geschlecht Kult. Gesellschaft 2015, 2, 51–67. (In German) [Google Scholar] [CrossRef] [Green Version]
- Arora-Jonsson, S. Virtue and vulnerability: Discourses on women, gender and climate change. Glob. Environ. Chang. 2011, 21, 744–751. [Google Scholar] [CrossRef]
| Domain | Selected Indicators |
|---|---|
| Social | Gender relations |
| Education | |
| Ethnicity | |
| Economic | Income |
| Employment | |
| Infrastructure | Health services |
| Built environment | |
| Access to information (e.g., Internet access) | |
| Institutional | Local governance |
| Community | Civic engagement |
| Environment | Green spaces |
| Exposure | |
| Culture | Cultural construction of health |
| Values |
| Domain | Indicator | Suggested General Questions Related to Indicators |
|---|---|---|
| Social | Gender equity | Does the adaptation measure require special attention to gender relations? For example, does the measure require unpaid care work to support older persons or children during extreme temperature events? Is the measure targeting only one gender, and, if so, do data support such an approach? Is the language used, i.e., in information material, gender-sensitive? |
| Education | Does the adaptation measure require a specific type of knowledge and experience that the target group might need to acquire? For behavior change adaptation, are instructions suitably formulated and distributed for all targeted groups? Are language and distribution channels used in the measure appropriate for the target groups? | |
| Ethnicity | Is there diversity within the target group? Are the adaptation materials targeting specific ethnic groups, and, if so, why? Do data support such an approach? Is the adaptation measure, i.e., information material, perpetuating stereotypes? Are materials culturally appropriate? Who is creating and disseminating the adaptation measure: how diverse is the team? | |
| Economic | Income | What are potential effects of the adaptation measure on income equality? Could the proposed adaptation strategy require target groups to spend money, i.e., for electricity or new household items? |
| Employment | Will the adaptation measure change provide more income opportunities through new jobs, i.e., in green technology or in adaptation policy? Will socially disadvantaged populations have the opportunity to profit from these new jobs? Are potentially targeted professions, i.e., nurses, included in strategy design? | |
| Infrastructure | Health services | Is the health system sufficiently prepared and staffed to respond to emergencies, i.e., during heat events or floods? Are the distances to health services longer for vulnerable groups than for others? Can the targeted groups get health-related adaptation information easily through widely accessible channels? |
| Built environment | Does the built environment pose a risk from climate change impacts, i.e., through dense concrete buildings during heat? Does the built environment pose obstacles to effective adaptation, i.e., fear of crime, inaccessible or expensive to access green or cool spaces? | |
| Access to information | Can all targeted groups regularly access relevant information about the adaptation measure, i.e., via TV, radio, or the Internet? How frequently is information about measures distributed? Are potential language barriers among target groups taken into account? | |
| Institutional | Local governance | How is the involvement of affected groups into local decision-making organized? |
| Community | Civic engagement | Are affected communities involved in planning or implementing of the adaptation measure? |
| Environment | Green spaces | Are green spaces safely accessible to all targeted groups? |
| Exposure | Are some groups disproportionately affected by environmental hazards such as waste, air pollution, or polluted waters? Is there a disaster risk reduction plan that has been well communicated to communities at risk? | |
| Culture | Cultural construction of health | Does the adaptation measure account for different perceptions of health risks and vulnerabilities in the affected communities? |
| Values | How does the adaptation measure consider multiple societal values about the environment and human health? |
| Domain | Indicator | Suggested Questions Related to Indicators | Sections of Strategy Document Replying to Questions |
|---|---|---|---|
| Social | Gender equity | Does the adaptation measure require special attention to gender relations? For example, does the measure require unpaid care work to support older persons or children during extreme temperature events? | Volunteer work to support older persons during heat events is recommended: no reflection on who these volunteers might be is available in document (p. 224) [69]. Might indicate effects on gender relations. |
| Education | Does the adaptation measure require a specific type of knowledge and experience that the target group might need to acquire? | Information campaign on health effects of extreme events and infections is planned to be tailored to target groups: dissemination via social media for youths, as part of teaching curricula, and via TV and radio for adults (p. 221) [69]. | |
| Ethnicity | Are the adaptation materials targeting specific ethnic groups, and, if so, why? | No specific mention of ethnicity. Might be included in “hard to reach target groups”, further analysis is necessary (p. 220) [69]. | |
| Economic | Income | What are potential effects of the adaptation measure on income equality? | No information provided. An analysis of the workforce structure in targeted fields could yield pointers on potential effects. |
| Employment | Will the adaptation measure change provide more income opportunities through new jobs, i.e., in green technology or in adaptation policy? | The outlined measures will provide additional opportunities in existing fields, i.e., in infectious disease monitoring or drinking water monitoring. Whether additional resources will be provided is unspecified (p. 228 for water) [69]. | |
| Infrastructure | Health services | Is the health system sufficiently prepared and staffed to respond to emergencies, i.e., during heat events or floods? | Additional need to further educate health personnel on climate change risks is acknowledged (p. 221) [69]. No information on health system preparedness is given: might indicate a need for better cross-sectoral integration. |
| Built environment | Does the built environment pose a risk from climate change impacts, i.e., through dense concrete buildings during heat? | This risk is acknowledged. It is planned to disseminate information on regional, cool spaces with easy access for use during heat events (p. 221) [69]. | |
| Access to information | How frequently is information about measures distributed? | No information on frequency of general awareness campaign. Heat warnings are disseminated during heat events (p. 220) [69]. | |
| Institutional | Local governance | How is the involvement of affected groups into local decision-making organized? | No information provided. Could be included in strategy for sector other than health. Comprehensive analyses of all sectors targeted in a strategy beyond health could yield further information. |
| Community | Civic engagement | Are affected communities involved in planning or implementing of the adaptation measure? | Calls for volunteers are issued regarding post-disaster reconstruction, for example (p. 228) [69]. The extent of participation is not clear. |
| Environment | Green spaces | Are green spaces safely accessible to all targeted groups? | No information provided. |
| Exposure | Is there a disaster risk reduction plan that has been well communicated to communities at risk? | Flood risk management plans exist (p. 227) [69]. Their dissemination is not specified. | |
| Culture | Cultural construction of health | Does the adaptation measure account for different perceptions of health risks and vulnerabilities in the affected communities? | The document outlines different vulnerabilities (p. 221) but does not link these to cultural differences or perception differences [69]. |
| Values | How does the adaptation measure consider multiple societal values about the environment and human health? | The document portrays scientific values in repeated calls for data collection (i.e., p. 235 on plant and pollen changes) [69]. Societal diversity is targeted only in relation to vulnerability. |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boeckmann, M.; Zeeb, H. Justice and Equity Implications of Climate Change Adaptation: A Theoretical Evaluation Framework. Healthcare 2016, 4, 65. https://doi.org/10.3390/healthcare4030065
Boeckmann M, Zeeb H. Justice and Equity Implications of Climate Change Adaptation: A Theoretical Evaluation Framework. Healthcare. 2016; 4(3):65. https://doi.org/10.3390/healthcare4030065
Chicago/Turabian StyleBoeckmann, Melanie, and Hajo Zeeb. 2016. "Justice and Equity Implications of Climate Change Adaptation: A Theoretical Evaluation Framework" Healthcare 4, no. 3: 65. https://doi.org/10.3390/healthcare4030065
APA StyleBoeckmann, M., & Zeeb, H. (2016). Justice and Equity Implications of Climate Change Adaptation: A Theoretical Evaluation Framework. Healthcare, 4(3), 65. https://doi.org/10.3390/healthcare4030065







