Spiritual Pain in Meals on Wheels’ Clients
Abstract
:1. Introduction
1.1. Spiritual Pain
1.2. Stress, Depression, Loneliness, and Religious Coping
1.3. Biological Influence
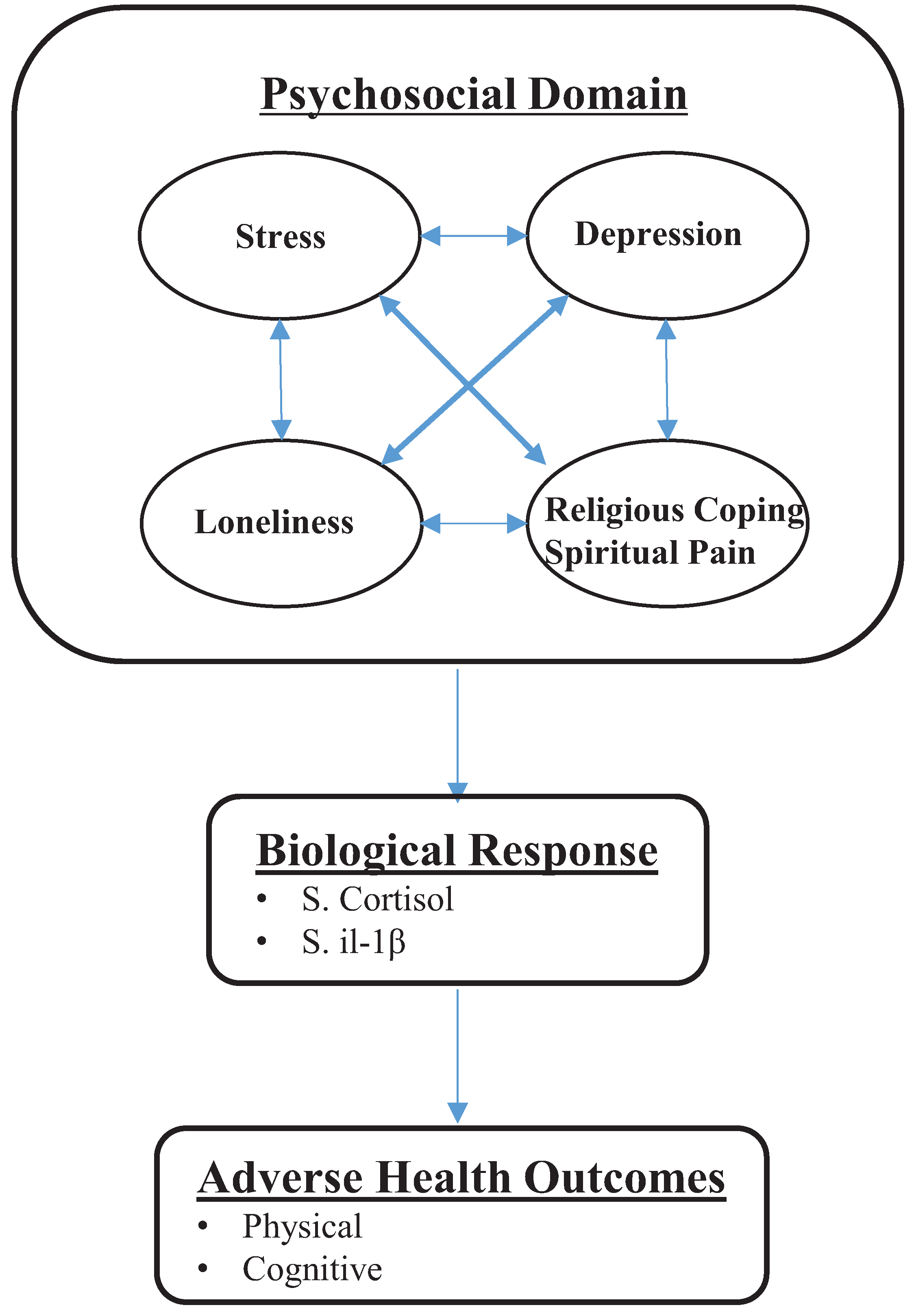
1.4. Theoretical Framework
1.5. Purpose and Hypothesis
2. Experimental Section
2.1. Design and Sample
2.2. Setting and Recruitment
2.3. Measurement
2.4. Data Analysis
3. Results
3.1. Participant Characteristics
| N (%) | Mean | SD | Range | |
|---|---|---|---|---|
| Age (years) | 88 | 75.4 | 9.0 | 60–95 |
| Males | 74.9 | 10.1 | 60–95 | |
| Females | 75.6 | 8.5 | 60–94 | |
| Gender | ||||
| Males | 30 (34.0) | |||
| Females | 58 (66.0) | |||
| Race | ||||
| Caucasian | 83 (94.3) | |||
| Black | 5 (5.7) | |||
| Other | 0 | |||
| BMI | ||||
| Males | 30 (34.0) | 28.5 | 6.54 | 17.9–46.9 |
| Females | 58 (66.0) | 30.6 | 7.7 | 13.7–51.5 |
| Marital Status | ||||
| Married | 26 (29.5) | |||
| Widowed | 29 (33.0) | |||
| Divorced | 25 (28.4) | |||
| Single | 8 (9.1) | |||
| Education (years) | 88 | 12.39 | 2.25 | 7–18 |
3.2. Levels of Psychosocial Factors and Biological Responses
| Possible Range | Score Range | Mean | SD | |
|---|---|---|---|---|
| Spiritual Pain | 1–4 | 1–4 | 1.56 | 0.89 |
| Males | 1–4 | 1.57 | 0.86 | |
| Females | 1–4 | 1.55 | 0.91 | |
| Stress | 0–40 | 0–38 | 15.02 | 6.21 |
| Males | 3–26 | 13.40 | 5.55 | |
| Females | 0–38 | 16.64 | 13.33 | |
| Depression | 0–15 | 0–13 | 4.31 | 3.02 |
| Males | 0–11 | 3.63 | 3.03 | |
| Females | 0–13 | 4.99 | 3.32 | |
| Loneliness | 20–80 | 20–67 | 39.9 | 12.22 |
| Males | 20–63 | 39.40 | 11.20 | |
| Females | 20–67 | 40.47 | 13.33 | |
| +Relig. Coping | 7–28 | 7–28 | 21.98 | 5.04 |
| Males | 11–28 | 21.03 | 5.00 | |
| Females | 7–28 | 22.93 | 5.76 | |
| −Relig. Coping | 7–28 | 7–25 | 9.72 | 3.35 |
| Males | 7–18 | 9.49 | 3.19 | |
| Females | 7–25 | 9.95 | 3.79 | |
| Cortisol µg/dL | ||||
| Both Genders | 0.01–5.17 | 0.33 | 0.76 | |
| Males | 0.03–5.17 | 0.58 | 1.30 | |
| Females | 0.01–1.75 | 0.19 | 0.24 | |
| IL-1β pg/mL | ||||
| Both Genders | 6.0–5253.19 | 554.86 | 872.44 | |
| Males | 6.0–5253.19 | 638.16 | 1142.06 | |
| Females | 6.0–3592.11 | 485.19 | 607.82 |
3.3. Correlations of Spiritual Pain
| Spiritual Pain | p Value | |
|---|---|---|
| Stress | r = 0.35 | ≤ 0.001 |
| Depression | r = 0.27 | 0.01 |
| Loneliness | r = 0.15 | 0.16 |
| +Religious Coping | r = −0.12 | 0.27 |
| −Religious Coping | r = 0.27 | 0.01 |
| Cortisol | r = 0.02 | 0.87 |
| IL-1β | r = −0.07 | 0.50 |
4. Discussion
4.1. Stress, Depression, and Religious Coping
4.2. Loneliness
4.3. Cortisol and IL-1β
5. Clinical Implications
6. Conclusions
7. Limitations
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Gallup, G. The Religiosity Cycle. Gallup Tuesday Briefing (2 June 2002). Available online: http://www.gallup.com/poll/tb/religValue/20020604asp (accessed on 26 May 2015).
- Koenig, H.; King, D.E.; Carson, V.B. Handbook of Religion and Health, 2nd ed.; Oxford University Press: New York, NY, USA, 2012. [Google Scholar]
- Barnes, P.M.; Powell-Griner, E.; McFann, K.; Nahin, R.L. Complementary and Alternative Medicine Rise among Adults: United States, 2002. Available online: http://www.cdc.gov/nchs/data/ad/ad343.pdf (accessed on 26 May 2015).
- Idler, E.L.; Kasl, S.V.; Hays, J.C. Patterns of religious practice and belief in the last year of life. J. Gerontol. B 2001, 56B, 2326–2334. [Google Scholar] [CrossRef]
- Taylor, H. While Most Americans Believe in God, Only 36% Attend a Religious Service Once a Month or More Often, 2003. Available online: http://www.harrisinteractive.com/harris_poll/index.asp?PID=900 (accessed on 12 June 2015).
- O’Neill, M.T.; Mako, C. Addressing spiritual pain. Health Prog. 2011, 92, 42–45. [Google Scholar] [PubMed]
- Levin, J. How faith heals: A theoretical model. Explore 2009, 5, 77–96. [Google Scholar] [CrossRef] [PubMed]
- Brunjes, G.B. Spiritual pain and suffering. Asian Pac. J. Cancer Prev. 2010, 11, 31–36. [Google Scholar] [PubMed]
- North American Nursing Diagnosis Association (NANDA). NANDA Nursing Diagnoses: Definitions and Characteristics; NANDA: Philadelphia, PA, USA, 1992. [Google Scholar]
- Murata, H. Spiritual pain and its care in patients with terminal cancer: Construction of a conceptual framework by philosophical approach. Palliat. Support. Care 2003, 1, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Guay, M.O.; Hui, D.; Parsons, H.A.; Govan, K.; de la Cruz, M.; Thorney, S.; Bruera, E. Spirituality, religiosity, and spiritual pain in advanced cancer patients. J. Pain Symptom Manag. 2011, 41, 986–994. [Google Scholar] [CrossRef] [PubMed]
- Mako, C.; Galek, K.; Poppito, S.R. Spiritual pain among patients with advanced cancer in palliative care. J. Palliat. Med. 2006, 9, 1106–1113. [Google Scholar] [CrossRef] [PubMed]
- McGrath, P. Spiritual pain: A comparison of findings from survivors and hospice patients. Am. J. Hosp. Palliat. Care 2003, 20, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Fitchett, G.; Murphy, P.E.; Kim, J.; Gibbons, J.L.; Cameron, J.R.; Davis, J.A. Religious struggle: Prevalence correlates and mental health risks in diabetic, congestive heart, failure, and oncology patients. Int. J. Psychiatry Med. 2004, 34, 179–196. [Google Scholar] [CrossRef] [PubMed]
- Exline, J.J.; Yali, A.M.; Sanderson, W.C. Guilt, discord, and alienation: The role of religious strain in depression and suicidality. J. Clin. Psychol. 2000, 56, 1481–1496. [Google Scholar] [CrossRef]
- Krause, H.; Ingersoll-Dayton, B.; Ellison, C.G.; Wulff, K.M. Aging, religious doubt, and psychological well-being. Gerontologist 1999, 39, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Fitchett, G.; Rybarczyk, B.D.; DeMarco, G.A.; Nicholas, J.J. The role of religion in medical rehabilitation outcomes: A longitudinal study. Rehabil. Psychol. 1999, 44, 333–353. [Google Scholar] [CrossRef]
- Pargament, K.; Koenig, H.; Tarakeshwar, N.; Hahn, J. Religious struggle as a predictor of mortality among medically ill patients: A two year longitudinal study. Arch. Int. Med. 2001, 161, 1881–1885. [Google Scholar] [CrossRef]
- Pizzagalli, D.A.; Bogdan, R.; Ratner, K.G.; Jahn, A.L. Increased perceived stress is associated with blunted hedonic capacity: Potential implications for depression research. Behav. Res. Ther. 2007, 45, 2742–2753. [Google Scholar] [CrossRef] [PubMed]
- Tennant, C. Life events, stress, and depression: A review of recent findings. Aust. N. Z. J. Psychiatry 2002, 36, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Dickerson, S.S.; Kemeny, M.E. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychol. Bull. 2004, 130, 355–391. [Google Scholar] [CrossRef] [PubMed]
- Maier, S.F.; Watkins, L.R. Stressor controllability and learned helplessness: The roles of the dorsal raphe nucleus, serotonin, and corticotropin-releasing factor. Neurosci. Biobehav. Rev. 2007, 29, 829–841. [Google Scholar] [CrossRef] [PubMed]
- Aylaz, R.; Akturk, U.; Erci, B.; Ozturk, H.; Aslan, H. Relationship between depression and loneliness in elderly and examination of influential factors. Arch. Gerontol. Geriatr. 2012, 55, 548–554. [Google Scholar] [CrossRef] [PubMed]
- Krause, N. Stress and isolation from close ties in later life. J. Gerontol. Soc. Sci. 1991, 46, 183–194. [Google Scholar] [CrossRef]
- Mann, A. Social support deficits loneliness and life events as risk factors for depression in old age. Psychol. Med. 1997, 27, 323–332. [Google Scholar]
- Pargament, K.; Koenig, H.; Perez, L.M. The many methods of religious coping: Development and initial validation of the RCOPE. J. Clin. Psychol. 2000, 56, 519–543. [Google Scholar] [CrossRef]
- Epel, E.S. Psychological and metabolic stress: A recipe for accelerated cellular aging? Hormones 2009, 8, 7–22. [Google Scholar] [CrossRef] [PubMed]
- Beluche, I.; Carriere, I.; Ritchie, K.; Ancelin, M. A prospective study of diurnal cortisol and cognitive function in community-dwelling elderly people. Psychol. Med. 2010, 40, 1039–1049. [Google Scholar] [CrossRef] [PubMed]
- Fiocco, A.; Wan, N.; Weekes, N.; Pim, H.; Lupien, S. Diurnal cycle of salivary cortisol in older adult men and women with subjective complaints of memory deficits and/or depressive symptoms: Relation to cognitive functioning. Stress 2006, 9, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Glaser, R.; Kiecolt-Glaser, J. Stress-induced immune dysfunction: Implications for health. Nat. Rev. Immunol. 2005, 5, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Jaremka, L.; Fagundes, C.; Peng, J.; Bennett, J.; Glaser, R.; Malarkey, W.; Kiecolt-Glaser, J. Loneliness promotes inflammation during acute stress. Psychol. Sci. 2013, 24, 1089–1097. [Google Scholar] [CrossRef] [PubMed]
- Mahon, N.E.; Yarcheski, A.; Yarcheski, T.J. Social support and positive health practices in young adults loneliness as a mediating variable. Clin. Nurs. Res. 1998, 7, 292–308. [Google Scholar] [CrossRef] [PubMed]
- Nolen-Hoeksama, S.; Ahrens, C. Age differences and similarities in the correlates of depressive symptoms. Psychol. Aging 2002, 17, 116–124. [Google Scholar] [CrossRef]
- Penninx, B.W.; van Tilburg, T.; Kriegsman, D.M.; Deeg, D.J.; Boeke, A.J.; van Eijk, J.T. Effects of social support and personal coping resources on mortality in older age: The Longitudinal Aging Study Amsterdam. Am. J. Epidemiol. 1997, 146, 510–519. [Google Scholar] [CrossRef] [PubMed]
- Adam, E.K.; Hawkley, L.C.; Kudielka, B.M.; Cacioppo, J.T. Day-to-day dynamics of experience-cortisol associations in a population based-sample of older adults. Proc. Natl. Acad. Sci. USA 2006, 103, 17058–17063. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Owen, N.; Kunz-Ebrecht, S.R.; Brydon, L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology 2004, 29, 593–611. [Google Scholar] [CrossRef]
- Ano, G.; Vasconcelles, E. Religious coping and psychological adjustment to stress: A meta-analysis. J. Clin. Psychol. 2005, 61, 461–480. [Google Scholar] [CrossRef] [PubMed]
- Koenig, H.G.; McCullough, M.E.; Larson, D.B. Handbook of Religion and Health; Oxford University Press: New York, NY, USA, 2001. [Google Scholar]
- Katz, J.; Weiner, H.; Gallagher, T.; Hellman, L. Stress, distress, and ego defenses. Arch. Gen. Psychiatry 1970, 23, 355–362. [Google Scholar] [CrossRef]
- Sudsuang, R.; Chenanez, V.; Veluvan, K. Effect of Buddhist meditation on serum cortisol and total protein levels, blood pressure, pulse rate, lung volume, and reaction time. Physiol. Behav. 1991, 50, 543–548. [Google Scholar] [CrossRef]
- Lutgendorf, S.K.; Russell, D.; Ulrich, P.; Harris, T.B.; Wallace, R. Religious participation, interleukin-6, and mortality in older adults. Health Psychol. 2004, 23, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Woods, T.E.; Antoni, M.H.; Ironson, G.H.; Kling, D.W. Religiosity is associated with affective and immune status in symptomatic HIV-infected gay men. J. Psychosom. Res. 1999, 46, 165–176. [Google Scholar] [CrossRef]
- Lissoni, P.G.; Messina, A.; Balestra, M.; Colciago, M.; Brivio, F.; Fumagalli, L.; Fumagalli, G.; Parolini, D. Efficacy of cancer chemotherapy in relation to synchronization of cortisol rhythm, immune status, and psychospiritual profile in metastatic non-small cell lung cancer. In Vivo 2008, 22, 257–262. [Google Scholar] [PubMed]
- Sephton, S.E.; Koopman, C.; Schaal, M.; Thoreson, C.; Spiegel, D. Spiritual expression and immune status in women with metastatic breast cancer: An exploratory study. Breast J. 2001, 7, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.; Rice, M.; Park, N.; Turner-Henson, A.; Downs, C. Stress and inflammation: A biobehavioral approach for nursing research. West. J. Nurs. Res. 2010, 32, 730–760. [Google Scholar] [CrossRef] [PubMed]
- Meals on Wheels Association of America. Available online: http://www.mowaa.org (accessed on 24 January 2014).
- Moran, M. Challenges in the meals on wheels program. J. Am. Diet. Assoc. 2004, 104, 1219–1221. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulos, G. Depression in the elderly. Lancet 2005, 365, 1961–1970. [Google Scholar] [CrossRef]
- Saito, T.; Kai, I.; Takizawa, A. Effects of a program to prevent social isolation on loneliness, depression, and subjective well-being of older adults: A randomized trail among older migrants in Japan. Arch. Gerontol. Geriatr. 2012, 55, 539–547. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 386–396. [Google Scholar] [CrossRef]
- Boss, L.; Kang, D.H.; Bergstrom, N.; Leasure, J.L. Biobehavioral correlates of cognitive function in the elderly: A biobehavioral approach. Int. J. Nurs 2015, in press. [Google Scholar] [CrossRef]
- Yesavage, J.; Brink, T.; Rose, T.; Lum, O.; Huang, V.; Adey, M.; Leirer, V. Development and validation of a geriatric depression screening scale; a preliminary report. J. Psychiatr. Res. 1983, 17, 37–49. [Google Scholar] [CrossRef]
- Russell, D.; Peplau, L.A.; Cutrona, C.E. The revised UCLA loneliness scale: Concurrent and discriminant validity evidence. J. Personal. Soc. Psychol. 1980, 39, 472–480. [Google Scholar] [CrossRef]
- Pargament, K.; Feuille, M.; Burdzy, D. The Brief RCOPE: Current psychometric status of a short measure of religious coping. Religions 2011, 2, 51–76. [Google Scholar] [CrossRef]
- The Power of Team Science. Available online: https://www.salimetrics.com/ (accessed on 6 April 2012).
- Harrison, M.O.; Koenig, H.; Hays, H.G.; Eme-Akwari, A.G.; Pargament, K.I. The epidemiology of religious coping: A review of recent literature. Int. Rev. Psychiatry 2001, 13, 86–93. [Google Scholar] [CrossRef]
- Musick, D.W.; Wilson, J. Volunteering and depression: The role of psychological and social resources in different age groups. Soc. Sci. Med. 2003, 56, 259–269. [Google Scholar] [CrossRef]
- Meertens, V.P.; Scheepers, P.; Tax, B. Depressive symptoms in the Netherlands 1975–1996: A theoretical framework and an empirical analysis of socio-demographic characteristics, gender differences, and changes. Sociol. Health Illn. 2003, 25, 208–231. [Google Scholar] [CrossRef] [PubMed]
- Hills, J.; Paice, J.; Cameron, J.; Shott, S. Spirituality and distress in palliative care consultation. J. Palliat. Med. 2005, 8, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Sherman, A.C.; Simonton, S.; Latif, U.; Spohn, R.; Tricot, G. Religious struggle and religious comfort in response to illness: Health outcomes among stem cell transplant patients. J. Behav. Med. 2005, 28, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Benore, E.; Pargament, K.; Pendleton, S. An initial examination of religious coping in children with asthma. Int. J. Psychol. Relig. 2008, 18, 267–290. [Google Scholar] [CrossRef]
- Sherman, A.; Plante, T.; Simonton, S.; Latif, U.; Anaissie, E. Prospective study of religious coping among patients undergoing autologous stem cell transplantation. J. Behav. Med. 2009, 32, 118–128. [Google Scholar] [CrossRef] [PubMed]
- Koenig, H. Spirituality and Health Research; Templeton Press: West Conshohocken, PA, USA, 2011. [Google Scholar]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boss, L.; Branson, S.; Cron, S.; Kang, D.-H. Spiritual Pain in Meals on Wheels’ Clients. Healthcare 2015, 3, 917-932. https://doi.org/10.3390/healthcare3040917
Boss L, Branson S, Cron S, Kang D-H. Spiritual Pain in Meals on Wheels’ Clients. Healthcare. 2015; 3(4):917-932. https://doi.org/10.3390/healthcare3040917
Chicago/Turabian StyleBoss, Lisa, Sandy Branson, Stanley Cron, and Duck-Hee Kang. 2015. "Spiritual Pain in Meals on Wheels’ Clients" Healthcare 3, no. 4: 917-932. https://doi.org/10.3390/healthcare3040917
APA StyleBoss, L., Branson, S., Cron, S., & Kang, D.-H. (2015). Spiritual Pain in Meals on Wheels’ Clients. Healthcare, 3(4), 917-932. https://doi.org/10.3390/healthcare3040917






