Changes in Psychophysical Parameters in Seniors During the COVID-19 Pandemic—A Repeated Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Methods
- SF-12v2 Health Survey—assessment of health-related quality of life [20].
2.3. Statistical Method
3. Results
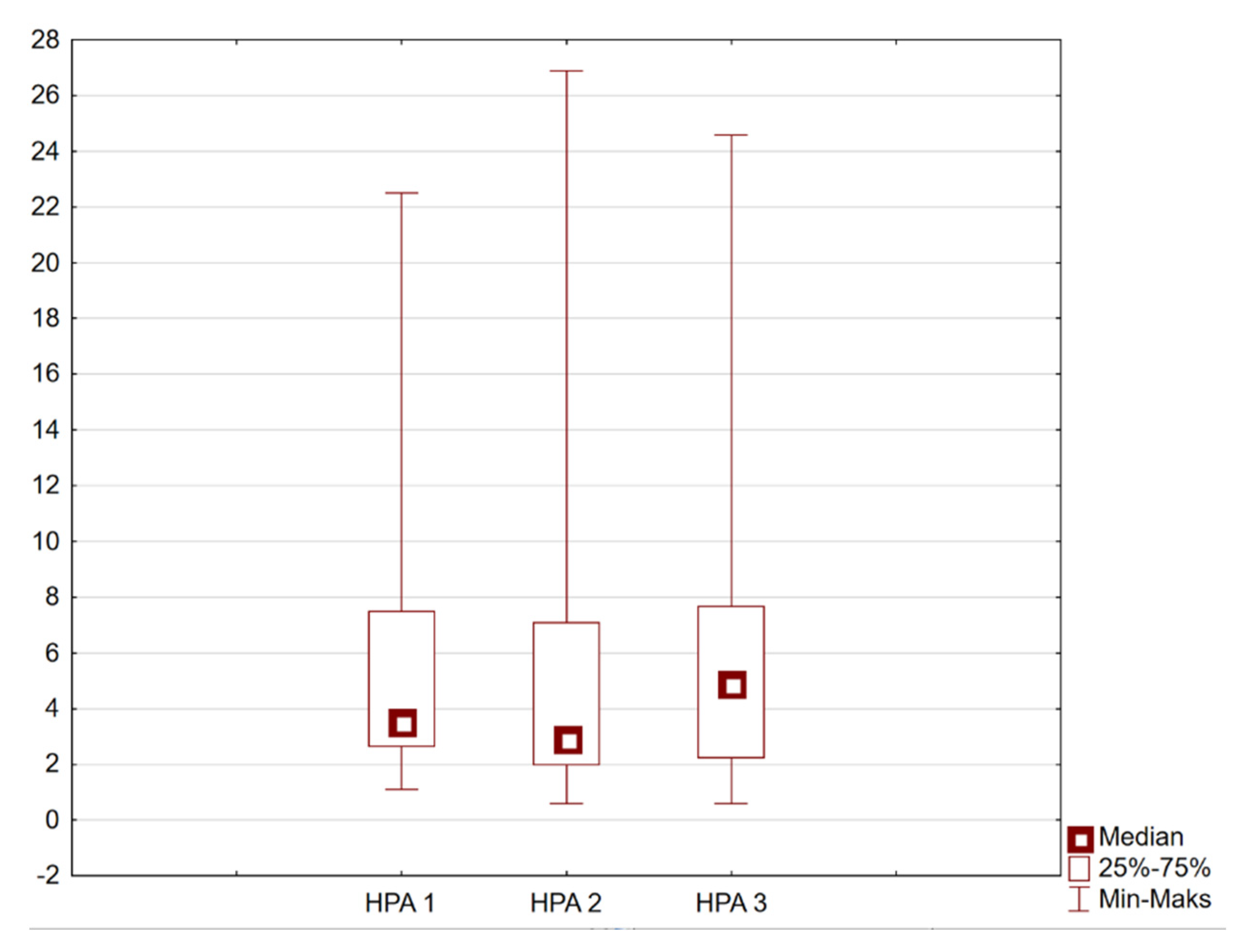
3.1. The Physical Activity of the Surveyed Individuals and Its Changes During the Pandemic
3.2. Analyzing the Quality of Life of the Respondents and Its Changes During the Pandemic
3.3. Anxiety, Depression, Aggression, and Insomnia Among the Surveyed Individuals and Their Changes During the Pandemic
3.4. Correlations Between Level of Physical Activity and Quality of Life, Anxiety, Depression, Aggression, or Sleep Disorders
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sepúlveda-Loyola, W.; Rodríguez-Sánchez, I.; Pérez-Rodríguez, P.; Ganz, F.; Torralba, R.; Oliveira, D.V.; Rodríguez-Mañas, L. Impact of Social Isolation Due to COVID-19 on Health in Older People: Mental and Physical Effects and Recommendations. J. Nutr. Health Aging 2020, 24, 938–947. [Google Scholar] [CrossRef] [PubMed]
- Loyola, W.S.; Camillo, C.A.; Torres, C.V.; Probst, V.S. Effects of an exercise model based on functional circuits in an older population with different levels of social participation. Geriatr. Gerontol. Int. 2018, 18, 216–223. [Google Scholar] [CrossRef]
- Sirven, N.; Debrand, T. Social participation and healthy ageing: An international comparison using SHARE data. Soc. Sci. Med. 2008, 67, 2017–2026. [Google Scholar] [CrossRef]
- Pollack, C.E.; von dem Knesebeck, O. Social capital and health among the aged: Comparisons between the United States and Germany. Health Place 2004, 10, 383–391. [Google Scholar] [CrossRef]
- Yazawa, A.; Inoue, Y.; Fujiwara, T.; Stickley, A.; Shirai, K.; Amemiya, A.; Kondo, N.; Watanabe, C.H.; Kondo, K. Association between social participation and hypertension among older people in Japan: The JAGES Study. Hypertens. Res. 2016, 39, 818–824. [Google Scholar] [CrossRef] [PubMed]
- WHO. Guidelines on Physical Activity and Sedentary Behaviour. 2020. Available online: https://www.who.int/publications/i/item/9789240015128 (accessed on 3 April 2024).
- Ozemek, C.; Lavie, C.J.; Rognmo, Ø. Global physical activity levels—Need for intervention. Prog. Cardiovasc. Dis. 2019, 62, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Molesztak, A. Nordic walking jako współczesna forma aktywności seniorów. J. Educ. Health Sport 2016, 6, 365–375. [Google Scholar] [CrossRef]
- Trabelsi, K. Globally altered sleep patterns and physical activity levels by confinement in 5056 individuals: ECLB COVID-19 international online survey. Biol. Sport 2021, 38, 495–506. [Google Scholar] [CrossRef]
- Dhama, K.; Patel, S.K.; Kumar, R.; Rana, J.; Yatoo, M.I.; Kumar, A.; Tiwari, R.; Dhama, J.; Natesan, S.; Singh, R.; et al. Geriatric Population During the COVID-19 Pandemic: Problems, Considerations, Exigencies, and Beyond. Front. Public Health 2020, 8, 574198. [Google Scholar] [CrossRef]
- Dunford, S.; Brooke, J. Effects of social isolation and restrictions on older people during the COVID-19 pandemic. Nurs. Older People 2022, 34, 20–26. [Google Scholar] [CrossRef]
- Brooke, J.; Dunford, S.; Clark, M. Older adult’s longitudinal experiences of household isolation and social distancing during the COVID-19 pandemic. Int. J. Older People Nurs. 2022, 17, e12459. [Google Scholar] [CrossRef] [PubMed]
- Naughton, L.; Cunha, F.; Padeiro, M.; Santana, P. What the pandemic and its impact on the mobility and well-being of older people can teach us about age-friendly cities and communities. Soc. Sci. Med. 2023, 338, 116329. [Google Scholar] [CrossRef]
- Badawy, A.; Solberg, M.; Obstfelder, A.U.; Alnes, R.E. Together, at a distance: Experiences with a novel technology for social contact among older people and their relatives in Norway during the COVID-19 pandemic. BMC Geriatr. 2023, 23, 218. [Google Scholar] [CrossRef]
- Hall Dykgraaf, S.; Desborough, J.; Sturgiss, E.; Parkinson, A.; Dut, G.M.; Kidd, M. Older people, the digital divide and use of telehealth during the COVID-19 pandemic. Aust. J. Gen. Pract. 2022, 51, 721–724. [Google Scholar] [CrossRef] [PubMed]
- Otorkpa, H.J. World Health Organization Definition of Health. Available online: https://www.researchgate.net/publication/387931721_World_Health_Organization_WHO_Definition_Of_Health (accessed on 17 December 2025).
- Hertogh, E.M.; Monninkhof, E.M.; Schouten, E.G.; Peeters, P.H.; Schuit, A.J. Validity of the modified Baecke questionnaire: Comparison with energy expenditure according to the doubly labeled water method. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 30. [Google Scholar] [CrossRef]
- Baecke, J.A.; Burema, J.; Frijters, J.E. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am. J. Clin. Nutr. 1982, 36, 936–942. [Google Scholar] [CrossRef]
- Voorrips, L.E.; Ravelli, A.C.; Dongelmans, P.; Deurenberg, P.; Van Staveren, W.A. A physical activity questionnaire for the elderly. Med. Sci. Sports Exerc. 1991, 23, 974–979. [Google Scholar] [CrossRef]
- Schron, E.; Friedmann, E.; Thomas, S.A. Does Health-Related Quality of Life Predict Hospitalization or Mortality in Patients with Atrial Fibrillation? J. Cardiovas. Electrophysiol. 2014, 25, 23–28. [Google Scholar] [CrossRef]
- Kozieł, P.; Lomper, K.; Uchmanowicz, B.; Polański, J. Association between acceptance of illness, anxiety and depression with assessment quality of life of breast cancer patients. Med. Paliat. Prakt. 2016, 10, 28–36. [Google Scholar]
- Sivertsen, H.E.; Helvik, A.S.; Gjøra, L.; Haugan, G. Psychometric validation of the Hospital Anxiety and Depression Scale (HADS) in community-dwelling older adults. BMC Psychiatry 2023, 23, 903. [Google Scholar] [CrossRef]
- Daniłosio, M.; Wysocki, J.; Prus, M. Occurrence of insomnia among patients with diagnosed obstructive sleep apnea. Pol. Prz. Otolaryngol. 2018, 7, 16–23. [Google Scholar] [CrossRef]
- Fornal-Pawłowska, M.; Wołyńczyk-Gmaj, D.; Szelenberger, W. Walidacja Ateńskiej Skali Bezsenności. Psychiatr. Pol. 2011, 45, 211–221. [Google Scholar]
- McCarthy, H.; Potts, H.W.; Fisher, A. Physical Activity Behavior Before, During, and After COVID-19 Restrictions: Longitudinal Smartphone-Tracking Study of Adults in the United Kingdom. J. Med. Internet Res. 2021, 23, e23701. [Google Scholar] [CrossRef] [PubMed]
- Voitsidis, P.; Gliatas, I.; Bairachtari, V.; Papadopoulou, K.; Papageorgiou, G.; Parlapani, E.; Syngelakis, M.; Holeva, V.; Diakogiannis, I. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 2020, 289, 113076. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.Z.; Sudati, I.P.; De Mello Konzen, V. COVID-19 and the impact on the physical activity level of elderly people: A systematic review. Ekspert Gerontol. 2022, 159, 111675. [Google Scholar] [CrossRef] [PubMed]
- Elliott, J.; Munford, L.; Ahmed, S.; Littlewood, A.; Todd, C. The impact of COVID-19 lockdowns on physical activity amongst older adults: Evidence from longitudinal data in the UK. BMC Public Health 2022, 22, 1802. [Google Scholar] [CrossRef]
- Kosowski, P.; Mróz, J. Ocena komunikacji a poczucie samotności i satysfakcji z życia w czasie pandemii. Kwart. Nauk. Fides Ratio 2020, 42, 214–226. [Google Scholar] [CrossRef]
- Ashdown-Franks, G.; Sabiston, C.M.; Stubbs, B. The evidence for physical activity in the management of major mental illnesses: A concise overview to inform busy clinicians’ practice and guide policy. Curr. Opin. Psychiatry 2019, 32, 375–380. [Google Scholar] [CrossRef]
- Szara, K.; Frejtag-Mika, E. Wpływ ograniczeń epidemiologicznych COVID-19 na działalność instytucji kultury w Polsce. Nierówności Społecz. A Wzrost Gospod. 2021, 1, 212–223. [Google Scholar] [CrossRef]
- De Saliva Santos Castelo Branco de Oliveira, L.; Souza, E.C.; Rodrigues, R.A.S.; Fett, C.A.; Piva, A.B. The effects of physical activity on anxiety, depression, and quality of life in elderly people living in the community. Trends Psychiatry Psychother. 2019, 41, 36–42. [Google Scholar] [CrossRef]
- Wasiuk-Zowada, D.; Knapik, A.; Szefler-Derela, J.; Brzęk, A.; Krzystanek, E. Kinesiophobia in Stroke Patients, Multiple Sclerosis and Parkinson’s Disesase. Diagnostic 2021, 11, 796. [Google Scholar] [CrossRef]
- Atıcı, E.; Girgin, N.; Çevik Saldıran, T. The effects of social isolation due to COVID-19 on the fear of movement, falling, and physical activity in older people. Australas. J. Ageing 2022, 41, 407–413. [Google Scholar] [CrossRef]
- Hoffman, G.J.; Malani, P.N.; Solway, E.; Kirch, M.; Singer, D.C.; Kullgren, J.T. Changes in activity levels, physical functioning, and fall risk during the COVID-19 pandemic. J. Am. Geriatr. Soc. 2022, 70, 49–59. [Google Scholar] [CrossRef]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, Anxiety and Stress during COVID-19: Associations with Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef]
- Sacre, J.W.; Holmes-Truscott, E.; Salim, A.; Kaarin, J.A.; Drummond, G.R.; Huxley, R.R.; Magliano, D.J.; van Wijngaarden, P.; Zimmet, P.Z.; Speight, J.; et al. Impact of the COVID-19 pandemic and lockdown restrictions on psychosocial and behavioural outcomes among Australian adults with type 2 diabetes: Findings from the PREDICT cohort study. Diabet. Med. 2021, 38, e14611. [Google Scholar] [CrossRef]
- Briere, J.; Wang, S.H.; Khanam, U.A.; Lawson, J.; Goodridge, D. Quality of life and well-being during the COVID-19 pandemic: Associations with loneliness and social isolation in a cross-sectional, online survey of 2207 community-dwelling older Canadians. BMC Geriatr. 2023, 23, 615. [Google Scholar] [CrossRef]
- Nightingale, T.E.; Heneghan, N.R.; Fenton, S.A.M.; Veldhuijzen van Zanten, S.J.J.C.S.; Jutzeler, C.R. Physical Activity and Health-Related Quality of Life in Adults with a Neurologically-Related Mobility Disability During the COVID-19 Pandemic: An Exploratory Analysis. Front. Neurol. 2021, 12, 699884. [Google Scholar] [CrossRef] [PubMed]
- Constant, A.; Conserve, D.F.; Gallopel-Morvan, K.; Raude, J. Socio-Cognitive Factors Associated with Lifestyle Changes in Response to the COVID-19 Epidemic in the General Population: Results from a Cross-Sectional Study in France. J. Front. Psychol. 2020, 11, 579460. [Google Scholar] [CrossRef]
- Knapik, A.; Rottermund, J.; Mysliwiec, A. Aktywność fizyczna a samoocena zdrowia osób w starszym wieku. Prz. Med. Uniw. Rzesz. I Nar. Inst. Leków W Warszawie Rzesz. 2011, 2, 195–204. [Google Scholar]
- Pacian, A.; Kulik, T.B.; Chruściel, P. Jakość życia a ryzyko depresji wśród osób starszych. Hygeia Public Health 2014, 49, 820–824. [Google Scholar]
- Ahmed, Z.M.; Khalil, M.F.; Kohail, A.M.; Eldesouky, I.F.; Elkady, I.F.A.; Shuaib, A. The Prevalence and Predictors of Post-Stroke Depression and Anxiety During COVID-19 Pandemic. J. Stroke Cerebrovasc. Dis. 2020, 29, 105315. [Google Scholar] [CrossRef] [PubMed]
- Chiaravalloti, N.D.; Amato, M.P.; Brichetto, G.; Chataway, J.; Dalgas, U.; DeLuca, J.; Meza, C.; Moore, N.B.; Feys, P.; Filippi, M.; et al. The emotional impact of the COVID-19 pandemic on individuals with progressive multiple sclerosis. J. Neurol. 2021, 268, 1598–1607. [Google Scholar] [CrossRef] [PubMed]
- Ozdin, S.; Ozdin, S.B. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int. J. Soc. Psychiatry 2020, 66, 504–511. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Surveyl. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
- Patten, S.B.; Williams, J.V.A.; Lavorato, D.H.; Bulloch, A.G.M. Recreational physical activity ameliorates some of the negative impact of major depression on health-related quality of life. Front. Psychiatry 2013, 2, 22. [Google Scholar] [CrossRef]
- Kokou-Kpolou, C.K.; Megalakaki, O.; Laimou, D.; Marina Kousouri, M. Insomnia during COVID-19 pandemic and lockdown: Prevalence, severity, and associated risk factors in French population. Psychiatry Res. 2020, 290, 113128. [Google Scholar] [CrossRef] [PubMed]
| Variable | Sex | Study I | Study II | Study III | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| X (SD) | Me | Q1 | Q3 | X (SD) | Me | Q1 | Q3 | X (SD) | Me | Q1 | Q3 | ||
| Age [years] | W n = 32 | 69.59 (7.97) | 69 | 62.5 | 74 | 69.59 (7.97) | 69 | 62.5 | 74 | 70.36 (7.46) | 69 | 63 | 77 |
| M n = 21 | 69.67 (7.88) | 67 | 65 | 73 | 69.67 (7.88) | 67 | 65 | 73 | 70.19 (7.97) | 68 | 65 | 75 | |
| Height [m] | W n = 32 | 1.64 (0.07) | 1.64 | 1.59 | 1.68 | 1.64 (0.07) | 1.64 | 1.59 | 1.68 | 1.64 (0.07) | 1.64 | 1.59 | 1.68 |
| M n = 21 | 1.73 (0.05) | 1.72 | 1.7 | 1.74 | 1.73 (0.05) | 1.72 | 1.7 | 1.74 | 1.73 (0.05) | 1.72 | 1.7 | 1.74 | |
| Weight [kg] | W n = 32 | 71.78 (13.26) | 69 | 61.5 | 80 | 71.78 (13.26) | 69 | 61.5 | 80 | 74.09 (13.67) | 70 | 65 | 82.5 |
| M n = 21 | 87.29 (13.27) | 87 | 76 | 97 | 87.29 (13.27) | 87 | 76 | 97 | 87.57 (13.82) | 87 | 76 | 98 | |
| BMI | W n = 32 | 31.89 (4.79) | 31.79 | 27.9 | 34.91 | 31.89 (4.79) | 31.79 | 27.9 | 34.91 | 32.54 (4.74) | 32.5 | 27.98 | 35.1 |
| M n = 21 | 33.57 (4.3) | 32.56 | 30.44 | 36.62 | 33.57 (4.3) | 32.56 | 30.44 | 36.62 | 33.65 (4.47) | 33.22 | 30.44 | 37 | |
| Variable | Sex | Study I | Study II | Study III | p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Me Q1 Q3 | X (Min–Max) | SD | Me Q1 Q3 | X (Min–Max) | SD | Me Q1 Q3 | X (Min–Max) | SD | |||
| General activities score (HPA) | W n = 32 | 3.39 2.61 5.36 | 5.23 (1.6–22.51) | 5.06 | 2.73 2.05 4.89 | 4.75 (1.1–26.88) | 5.59 | 3.96 2.22 7.24 | 5.34 (1.8–23.87) | 4.65 | 0.07 |
| M n = 21 | 4.69 2.92 12.12 | 7.39 (1.1–16.78) | 5.59 | 4.19 2 11.52 | 6.68 (0.6–16.78) | 5.54 | 7.02 2.92 10.41 | 7.83 (0.6–24.57) | 6.48 | 0.09 | |
| Variable | Sex | Study I | Study II | Study III | p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Me | X (Min–Max) | SD | Me | X (Min–Max) | SD | Me | X (Min–Max) | SD | |||
| MCS | W n = 32 | 79.17 | 76.2 (15–100) | 17.29 | 70.83 | 70.66 (15–93.33) | 17.13 | 75 | 72.92 (40–100) | 15.79 | 0.02 * |
| M n = 21 | 81.67 | 80.79 (25–100) | 18.29 | 81.67 | 79.29 (25–100) | 19.83 | 83.33 | 79.44 (38.3–100) | 19.89 | 0.64 | |
| PCS | W n = 32 | 65 | 62.97 (4.17–95.83) | 19.27 | 63.75 | 63.07 (4.17–95.83) | 19.52 | 62.5 | 61.3 (6.67–95.83) | 20.5 | 0.89 |
| M n = 21 | 66.67 | 66.94 (23.3–95.83) | 19.08 | 66.67 | 66.78 (23.3–95.83) | 19.87 | 68.33 | 67.69 (23.3–95.83) | 19.81 | 0.73 | |
| Variable | Sex | Study I | Study II | Study III | p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Me | X (Min–Max) | SD | Me | X (Min–Max) | SD | Me | X (Min–Max) | SD | |||
| Anxiety | W n = 32 | 7 | 7.5 (2–15) | 2.76 | 9 | 8.78 (4–17) | 2.78 | 8.5 | 8.44 (4–15) | 2.46 | 0.004 * |
| M n = 21 | 7 | 6.57 (3–10) | 1.89 | 7 | 7 (3–10) | 1.54 | 2 | 6.95 (0–5) | 1.32 | 0.66 | |
| p | 0.03 * | 0.002 * | 0.03 * | ||||||||
| Depression | W n = 32 | 12 | 11.8 (7–15) | 1.59 | 12 | 11.3 (6–15) | 1.86 | 12 | 11.44 (6–14) | 1.76 | 0.64 |
| M n = 21 | 12 | 11.19 (7–13) | 1.47 | 11 | 10.76 (7–13) | 1.84 | 10 | 10.24 (5–15) | 2.3 | 0.02 * | |
| p | 0.18 | 0.79 | 0.94 | ||||||||
| Aggression | W n = 32 | 2 | 2.03 (0–4) | 1.4 | 3 | 2.56 (0–5) | 1.46 | 2.5 | 2.47 (0–5) | 1.68 | 0.03 * |
| M n = 21 | 1 | 1.57 (0–5) | 1.5 | 2 | 1.95 (0–5) | 1.75 | 2 | 1.57 (0–5) | 1.33 | 0.41 | |
| p | 0.18 | 0.07 | 0.46 | ||||||||
| Insomia | W n = 32 | 6 | 5.47 (0–11) | 3.1 | 6.5 | 6.34 (0–16) | 3.87 | 5.5 | 5.7 (0–12) | 3.09 | 0.17 |
| M n = 21 | 3 | 3.48 (0–13) | 3.04 | 3 | 4.33 (0–15) | 3.77 | 3 | 3.62 (0–15) | 3.49 | 0.14 | |
| p | 0.06 | 0.41 | 0.03 * | ||||||||
| Variable | Sex | Study I R | Study II R | Study III R |
|---|---|---|---|---|
| MCS | W n = 32 | 0.03 | 0.017 | −0.102 |
| M n = 21 | 0.27 | 0.217 | 0.397 | |
| PCS | W n = 32 | −0.081 | 0.11 | −0.077 |
| M n = 21 | 0.124 | 0.137 | 0.379 | |
| Anxiety | W n = 32 | 0.002 | 0.082 | −0.047 |
| M n = 21 | 0.202 | 0.098 | 0.082 | |
| Depression | W n = 32 | 0.364 * | 0.331 | 0.225 |
| M n = 21 | 0.201 | 0.398 | 0.487 * | |
| Aggression | W n = 32 | −0.087 | −0.091 | 0.091 |
| M n = 21 | 0.127 | −0.043 | −0.068 | |
| Insomia | W n = 32 | 0.128 | 0.31 | 0.118 |
| M n = 21 | −0.077 | −0.25 | −0.113 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Szydłak, D.; Grabska-Klein, E.; Brzęk, A. Changes in Psychophysical Parameters in Seniors During the COVID-19 Pandemic—A Repeated Observational Study. Healthcare 2026, 14, 84. https://doi.org/10.3390/healthcare14010084
Szydłak D, Grabska-Klein E, Brzęk A. Changes in Psychophysical Parameters in Seniors During the COVID-19 Pandemic—A Repeated Observational Study. Healthcare. 2026; 14(1):84. https://doi.org/10.3390/healthcare14010084
Chicago/Turabian StyleSzydłak, Dorota, Ewelina Grabska-Klein, and Anna Brzęk. 2026. "Changes in Psychophysical Parameters in Seniors During the COVID-19 Pandemic—A Repeated Observational Study" Healthcare 14, no. 1: 84. https://doi.org/10.3390/healthcare14010084
APA StyleSzydłak, D., Grabska-Klein, E., & Brzęk, A. (2026). Changes in Psychophysical Parameters in Seniors During the COVID-19 Pandemic—A Repeated Observational Study. Healthcare, 14(1), 84. https://doi.org/10.3390/healthcare14010084








