Healthcare-Associated Infections: Knowledge Score and Awareness Among Nurses in Hospitals from North-East Romania
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Settings
2.3. Study Population
2.4. The Applied Questionnaire
2.4.1. Construction of Our Own Questionnaire
2.4.2. Questionnaire Validation
2.5. Statistical Processing
2.6. Scientific Research Ethics and GenAI Using
3. Results
3.1. Demographic Characteristics
3.2. Multivariate Analysis Models
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HAI | Healthcare-associated infection |
| AMR | Antimicrobial resistance |
| CDC | Centers for Disease Prevention and Control |
| ECDC | European Centre for Disease Prevention and Control |
References
- Zingg, W.; Holmes, A.; Dettenkofer, M.; Goetting, T.; Secci, F.; Clack, L.; Allegranzi, B.; Magiorakos, A.P.; Pittet, D. systematic review and evidence-based guidance on organization of hospital infection control programmes (SIGHT) study group. Hospital organisation, management, and structure for prevention of health-care-associated infection: A systematic review and expert consensus. Lancet Infect. Dis. 2015, 15, 212. [Google Scholar] [CrossRef] [PubMed]
- Viti, F.; Cartocci, A.; Perinti, R.; Guarducci, G.; Nante, N. Analysis and Impact of Infection Prevention Procedures in Long-Term Care Facilities. J. Prev. Med. Hyg. 2025, 66, E75. [Google Scholar] [CrossRef] [PubMed]
- Cristina, M.L.; Spagnolo, A.M.; Giribone, L.; Demartini, A.; Sartini, M. Epidemiology and Prevention of Healthcare-Associated Infections in Geriatric Patients: A Narrative Review. Int. J. Environ. Res. Public Health 2021, 18, 5333. [Google Scholar] [CrossRef] [PubMed]
- Alrebish, S.A.; Yusufoglu, H.S.; Alotibi, R.F.; Abdulkhalik, N.S.; Ahmed, N.J.; Khan, A.H. Epidemiology of Healthcare-Associated Infections and Adherence to the HAI Prevention Strategies. Healthcare 2023, 11, 63. [Google Scholar] [CrossRef]
- Duceac, L.D.; Stafie, L.; Păvăleanu, I.; Mitrea, G.; Baciu, G.; Banu, E.A.; Romila, L.; Luca, A.C. Sepsis in Paediatrics—A Special Form of Infection Associated to Medical Assistance. Int. J. Med. Dent. 2018, 22, 229. [Google Scholar]
- Suetens, C.; Latour, K.; Kärki, T.; Ricchizzi, E.; Kinross, P.; Moro, M.L.; Jans, B.; Hopkins, S.; Hansen, S.; Lyytikäinen, O.; et al. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: Results from two European point prevalence surveys, 2016 to 2017. Eurosurveillance 2018, 23, 1800516. [Google Scholar] [CrossRef]
- Alqurashi, M.S.; Sawan, A.A.; Berekaa, M.M.; Hunasemarada, B.C.; Al Shubbar, M.D.; Al Qunais, A.A.; Huldar, A.S.; Bojabara, L.M.; Alamro, S.A.; El-Badry, A.A. Hospital Hygiene Paradox: MRSA and Enterobacteriaceae Colonization Among Cleaning Staff in a Tertiary Hospital in Saudi Arabia. Medicina 2025, 61, 384. [Google Scholar] [CrossRef]
- Stewart, S.; Robertson, C.; Pan, J.; Kennedy, S.; Dancer, S.; Haahr, L.; Manoukian, S.; Mason, H.; Kavanagh, K.; Cook, B.; et al. Epidemiology of Healthcare-Associated Infection Reported from a Hospital-Wide Incidence Study: Considerations for Infection Prevention and Control Planning. J. Hosp. Infect. 2021, 114, 10. [Google Scholar] [CrossRef]
- Zahari, N.I.N.; Engku Abd Rahman, E.N.S.; Irekeola, A.A.; Ahmed, N.; Rabaan, A.A.; Alotaibi, J.; Alqahtani, S.A.; Halawi, M.Y.; Alamri, I.A.; Almogbel, M.S.; et al. A Review of the Resistance Mechanisms for β-Lactams, Macrolides and Fluoroquinolones among Streptococcus pneumoniae. Medicina 2023, 59, 1927. [Google Scholar] [CrossRef]
- Alhazmi, A.H.; Alameer, K.M.; Abuageelah, B.M.; Alharbi, R.H.; Mobarki, M.; Musawi, S.; Haddad, M.; Matabi, A.; Dhayhi, N. Epidemiology and Antimicrobial Resistance Patterns of Urinary Tract Infections: A Cross-Sectional Study from Southwestern Saudi Arabia. Medicina 2023, 59, 1411. [Google Scholar] [CrossRef]
- Alamer, A.; Alharbi, F.; Aldhilan, A.; Almushayti, Z.; Alghofaily, K.; Elbehiry, A.; Abalkhail, A. Healthcare-Associated Infections (HAIs): Challenges and Measures Taken by the Radiology Department to Control Infection Transmission. Vaccines 2022, 10, 2060. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, F.; Forrester, M.; Advinha, A.M.; Coutinho, A.; Landeira, N.; Pereira, M. Clostridioides difficile Infection in Hospitalized Patients—A Retrospective Epidemiological Study. Healthcare 2024, 12, 76. [Google Scholar] [CrossRef]
- Merza, M.A.; Mohammed, S.A.; Qasim, A.M.; Abdulah, D.M. Sero-prevalence and associated risk factors of blood-borne viral infection among healthcare workers of a tertiary referral hospital: A single-center experience. Health Probl. Civ. 2023, 17, 328. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention Control. Healthcare-associated infections acquired in intensive care units. In Annual Epidemiological Report for 2021; ECDC: Stockholm, Sweden, 2024. [Google Scholar]
- Coman, A.; Pop, D.; Muresan, F.; Oprescu, F.; Fjaagesund, S. Surveillance and Reporting of Hospital-Associated Infections—A Document Analysis of Romanian Healthcare Legislation Evolution over 20 Years. Healthcare 2025, 13, 229. [Google Scholar] [CrossRef]
- Olaru, I.; Stefanache, A.; Gutu, C.; Lungu, I.I.; Mihai, C.; Grierosu, C.; Calin, G.; Marcu, C.; Ciuhodaru, T. Combating Bacterial Resistance by Polymers and Antibiotic Composites. Polymers 2024, 16, 3247. [Google Scholar] [CrossRef]
- Luchian, N.; Olaru, I.; Pleșea-Condratovici, A.; Duceac, M.; Mătăsaru, M.; Dabija, M.G.; Elkan, E.M.; Dabija, V.A.; Eva, L.; Duceac, L.D. Clinical and Epidemiological Aspects on Healthcare-Associated Infections with Acinetobacter spp. in a Neurosurgery Hospital in North-East Romania. Medicina 2025, 61, 990. [Google Scholar] [CrossRef]
- Haque, M.; Sartelli, M.; McKimm, J.; Abu Bakar, M. Health care-associated infections—An overview. Infect. Drug Resist. 2018, 11, 2321. [Google Scholar] [CrossRef]
- Freitas, J.; Lomba, A.; Sousa, S.; Gonçalves, V.; Brois, P.; Nunes, E.; Veloso, I.; Peres, D.; Alves, P. Consensus-Based Guidelines for Best Practices in the Selection and Use of Examination Gloves in Healthcare Settings. Nurs. Rep. 2025, 15, 9. [Google Scholar] [CrossRef]
- Luchian, N.; Salim, C.; Condratovici, A.P.; Marcu, C.; Buzea, C.G.; Matei, M.N.; Dinu, C.A.; Duceac, M.; Elkan, E.M.; Rusu, D.I.; et al. Episode- and Hospital-Level Modeling of Pan-Resistant Healthcare-Associated Infections (2020–2024) Using TabTransformer and Attention-Based LSTM Forecasting. Diagnostics 2025, 15, 2138. [Google Scholar] [CrossRef]
- World Health Organization. Global Antimicrobial Resistance and Use Surveillance System (GLASS) Report 2022; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Sartelli, M.; Marini, C.P.; McNelis, J.; Coccolini, F.; Rizzo, C.; Labricciosa, F.M.; Petrone, P. Preventing and Controlling Healthcare-Associated Infections: The First Principle of Every Antimicrobial Stewardship Program in Hospital Settings. Antibiotics 2024, 13, 896. [Google Scholar] [CrossRef]
- Croskerry, P. To err is human--and let's not forget it. CMAJ 2010, 182, 524. [Google Scholar] [CrossRef]
- Upadhyay, S.; Smith, D.G. Healthcare Associated Infections, Nurse Staffing, and Financial Performance. Inquiry 2023, 60, 469580231159315. [Google Scholar] [CrossRef] [PubMed]
- Peutere, L.; Terho, K.; Pentti, J.; Ropponen, A.; Kivimäki, M.; Härmä, M.; Krutova, O.; Ervasti, J.; Koskinen, A.; Virtanen, M. Nurse Staffing Level, Length of Work Experience, and Risk of Health Care-Associated Infections Among Hospital Patients: A Prospective Record Linkage Study. Med. Care 2023, 61, 279. [Google Scholar] [CrossRef] [PubMed]
- Baranowska-Tateno, K.; Micek, A.; Gniadek, A.; Wójkowska-Mach, J.; Różańska, A. Healthcare-Associated Infections and Prevention Programs in General Nursing versus Residential Homes—Results of the Point Prevalence Survey in Polish Long-Term Care Facilities. Medicina 2024, 60, 137. [Google Scholar] [CrossRef]
- Economou, A. Public Perceptions on the Efficiency of National Healthcare Systems Before and After the COVID-19 Pandemic. Healthcare 2025, 13, 2146. [Google Scholar] [CrossRef]
- Audet, L.A.; Bourgault, P.; Rochefort, C.M. Associations between nurse education and experience and the risk of mortality and adverse events in acute care hospitals: A systematic review of observational studies. Int. J. Nurs. Stud. 2018, 80, 128. [Google Scholar] [CrossRef]
- Ichim, D.L.; Duceac, L.D.; Marcu, C.; Iordache, A.C.; Ciomaga, I.C.; Luca, A.C.; Mitrea, G.; Goroftei, E.R.B.; Stafie, L. Synthesis and Characterization of Colistin Intercalated Nanoparticles Used to Combat Multi-Drug Resistant Microorganisms. Rev. Chim. 2019, 70, 3734–3737. [Google Scholar] [CrossRef]
- Marczewski, K.P.; Piegza, M.; Gospodarczyk, N.J.; Gospodarczyk, A.Z.; Marcinek, M.; Tkocz, M.; Sosada, K. Evaluation of selected factors influencing sleep disorders in paramedics during the COVID-19 pandemic. Arch. Med. Sci. 2024, 20, 86–93. [Google Scholar] [CrossRef]
- Teixeira, J.; Reis, N.; Chawłowska, E.; Rocha, P.; Czech-Szczapa, B.; Godinho, A.C.; Bączyk, G.; Agrelos, J.; Jaracz, K.; Fontoura, C.; et al. Current Approaches on Nurse-Performed Interventions to Prevent Healthcare-Acquired Infections: An Umbrella Review. Microorganisms 2025, 13, 463. [Google Scholar] [CrossRef]
- Hirani, R.; Podder, D.; Stala, O.; Mohebpour, R.; Tiwari, R.K.; Etienne, M. Strategies to Reduce Hospital Length of Stay: Evidence and Challenges. Medicina 2025, 61, 922. [Google Scholar] [CrossRef]
- Fattori, A.; Comotti, A.; Mazzaracca, S.; Consonni, D.; Bordini, L.; Colombo, E.; Brambilla, P.; Bonzini, M. Long-Term Trajectory and Risk Factors of Healthcare Workers’ Mental Health during COVID-19 Pandemic: A 24 Month Longitudinal Cohort Study. Int. J. Environ. Res. Public Health 2023, 20, 4586. [Google Scholar] [CrossRef]
- Garcia, C.d.L.; Abreu, L.C.d.; Ramos, J.L.S.; Castro, C.F.D.d.; Smiderle, F.R.N.; Santos, J.A.d.; Bezerra, I.M.P. Influence of Burnout on Patient Safety: Systematic Review and Meta-Analysis. Medicina 2019, 55, 553. [Google Scholar] [CrossRef]
- Malheiro, R.; Gomes, A.A.; Fernandes, C.; Fareleira, A.; Lebre, A.; Pascoalinho, D.; Gonçalves-Pereira, J.; Paiva, J.-A.; Sá-Machado, R. Hospital Context Determinants of Variability in Healthcare-Associated Infection Prevalence: Multi-Level Analysis. Microorganisms 2024, 12, 2522. [Google Scholar] [CrossRef] [PubMed]
- Todo Bom, L.F.P.; Mata, E.S.F.; Cunha, H.M.P.; Marquês, M.d.C.M.P.; Dixe, M.d.A. Effectiveness of Nursing Interventions on Preventing the Risk of Infection in Adult Inpatients: Protocol for a Systematic Review. Nurs. Rep. 2025, 15, 210. [Google Scholar] [CrossRef] [PubMed]
- Pappa, D.; Koutelekos, I.; Evangelou, E.; Dousis, E.; Mangoulia, P.; Gerogianni, G.; Zartaloudi, A.; Toulia, G.; Kelesi, M.; Margari, N.; et al. Investigation of Nurses’ Wellbeing towards Errors in Clinical Practice—The Role of Resilience. Medicina 2023, 59, 1850. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Bachani, R. Knowledge Attitude Practice Perceived Barriers for the Compliance of Standard Precautions among Medical Nursing Students in Central India. Int. J. Environ. Res. Public Health 2023, 20, 5487. [Google Scholar] [CrossRef]
- Antolí-Jover, A.M.; Gázquez-López, M.; Brieba-del Río, P.; Martín-Salvador, A.; Martínez-García, E.; Sánchez-García, I.; Álvarez-Serrano, M.A. Prevalence and Predictors of Work–Life Balance Among Nursing Personnel During the Sixth Wave of the Pandemic: The Role of Stress and Sociodemographic and Work-Related Variables. Behav. Sci. 2025, 15, 751. [Google Scholar] [CrossRef]
- Huang, Y.; Wang, Z.; Li, Y.; Zhao, Z.; Wang, W.; Cai, C.; Wu, X.; Liu, L.; Chen, M. Anxiety and burnout in infectious disease nurses: The role of perceived stress and resilience. BMC Nurs. 2025, 24, 3. [Google Scholar] [CrossRef]
- Claponea, R.M.; Iorga, M. The Relationship between Burnout and Wellbeing Using Social Support, Organizational Justice, and Lifelong Learning in Healthcare Specialists from Romania. Medicina 2023, 59, 1352. [Google Scholar] [CrossRef]
- Peñacoba-Puente, C.; Gil-Almagro, F.; García-Hedrera, F.J.; Carmona-Monge, F.J. From Anxiety to Hopelessness: Examining Influential Psychological Processes Affecting Mental Health Status of Spanish Nurses During the COVID-19 Pandemic. Medicina 2025, 61, 236. [Google Scholar] [CrossRef]
- Rozmann, N.; Fusz, K.; Macharia, J.M.; Sipos, D.; Kivés, Z.; Kövesdi, O.; Raposa, B. Occupational Stress and Sleep Quality Among Hungarian Nurses in the Post-COVID Era: A Cross-Sectional Study. Healthcare 2025, 13, 2029. [Google Scholar] [CrossRef]
| Scoring Principle | Response Elaboration |
|---|---|
| For each subject the score is the sum of the answers to each of the questions regarding the level of knowledge about the prevention and limitation of HAIs: | 1 yes 0 no 1 not at all 2 a little 3 moderately 4 quite a bit 5 very much |
| For questions regarding health status: | 1 much worse 2 worse 3 deficient 4 much better 5 excellent |
| The primary score is standardized as follows: | a low score is interpreted as “worse” a high score is interpreted as “better” |
| Statistical Variables | Number (n = 288) | % |
|---|---|---|
| Distribution by age group | ||
| 18–30 years | 23 | 8.1 |
| 31–40 years | 56 | 19.4 |
| 41–60 years | 206 | 71.5 |
| 61+ years | 3 | 1 |
| Distribution by gender | ||
| female | 243 | 84.4 |
| male | 45 | 15.6 |
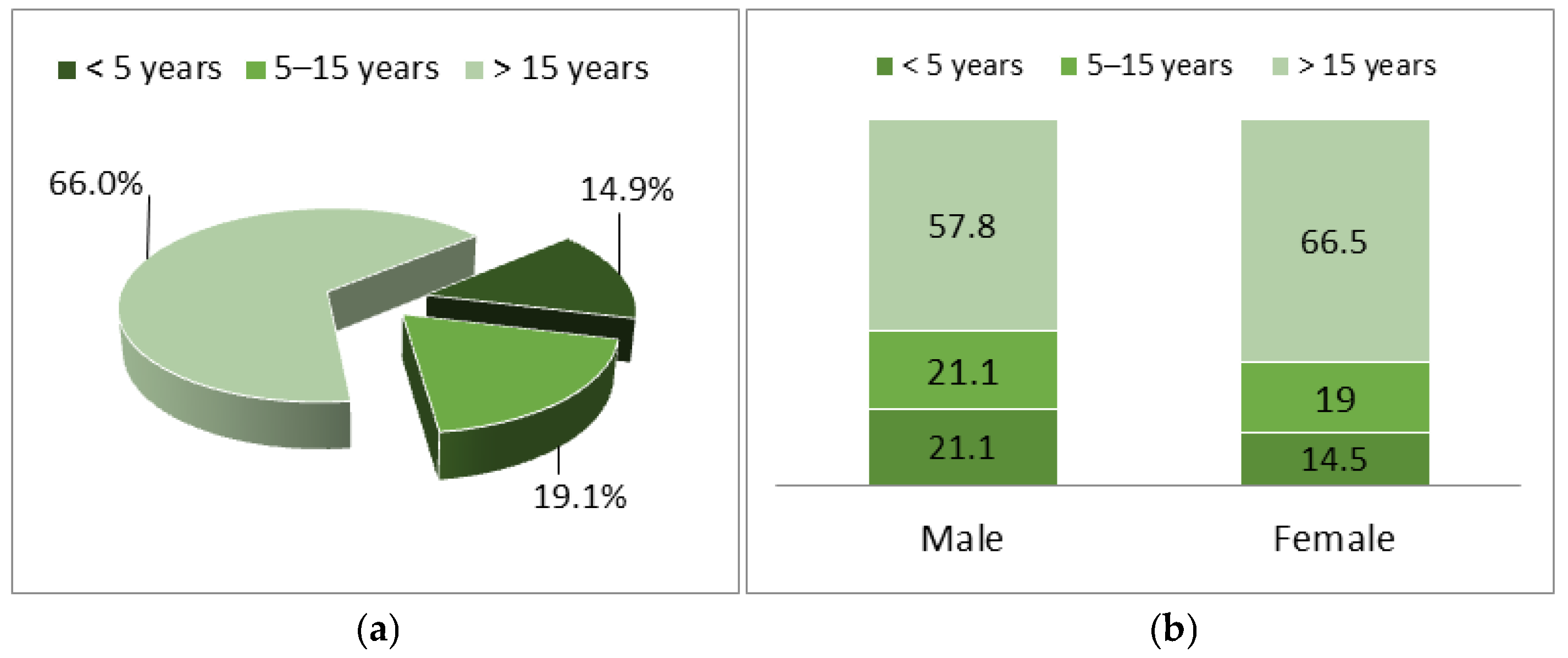
| Length of service | ||
| <5 years | 55 | 19.1 |
| 5–15 years | 190 | 66.0 |
| >15 years | 43 | 14.9 |
| Model | R | R-Squared | Adjusted R-Squared | Estimated Standard Error | Statistical Test | ||||
|---|---|---|---|---|---|---|---|---|---|
| R-Squared Change | F Change | df1 | df2 | Sig. F Change | |||||
| 1 | 0.293 (a) * | 0.086 | 0.083 | 11.910 | 0.086 | 26.927 | 1 | 286 | 0.000 |
| 2 | 0.330 (b) | 0.109 | 0.103 | 11.780 | 0.023 | 7.320 | 1 | 285 | 0.007 |
| 3 | 0.339 (c) | 0.115 | 0.105 | 11.764 | 0.006 | 1.821 | 1 | 284 | 0.178 |
| 4 | 0.644 (d) | 0.414 | 0.406 | 9.586 | 0.300 | 144.674 | 1 | 283 | 0.000 |
| 5 | 0.677 (e) | 0.459 | 0.449 | 9.231 | 0.045 | 23.192 | 1 | 282 | 0.000 |
| 6 | 0.683 (f) | 0.467 | 0.455 | 9.177 | 0.008 | 4.325 | 1 | 281 | 0.038 |
| Model | R | R-Squared | Adjusted R-Squared | Estimated Standard Error | Statistical Test | ||||
|---|---|---|---|---|---|---|---|---|---|
| R-Squared Change | F Change | df1 | df2 | Sig. F Change | |||||
| 1 | 0.618 (a) * | 0.382 | 0.380 | 9.790 | 0.382 | 177.123 | 1 | 286 | 0.001 |
| 2 | 0.703 (b) | 0.494 | 0.491 | 8.873 | 0.112 | 63.170 | 1 | 285 | 0.001 |
| 3 | 0.855 (c) | 0.732 | 0.729 | 6.477 | 0.237 | 250.892 | 1 | 284 | 0.001 |
| 4 | 0.880 (d) | 0.774 | 0.770 | 5.960 | 0.042 | 52.381 | 1 | 283 | 0.001 |
| 5 | 0.897 (e) | 0.804 | 0.801 | 5.554 | 0.030 | 43.881 | 1 | 282 | 0.001 |
| 6 | 0.899 (f) | 0.808 | 0.804 | 5.510 | 0.004 | 5.511 | 1 | 281 | 0.020 |
| 7 | 0.910 (g) | 0.829 | 0.825 | 5.207 | 0.021 | 34.707 | 1 | 280 | 0.001 |
| 8 | 0.919 (h) | 0.844 | 0.839 | 4.984 | 0.015 | 26.594 | 1 | 279 | 0.001 |
| 9 | 0.922 (i) | 0.851 | 0.846 | 4.884 | 0.007 | 12.521 | 1 | 278 | 0.001 |
| Model | R | R-Squared | Adjusted R-Squared | Estimated Standard Error | Statistical Test | ||||
|---|---|---|---|---|---|---|---|---|---|
| R-Squared Change | F Change | df1 | df2 | Sig. F Change | |||||
| 1 | 0.194 (a) * | 0.038 | 0.034 | 12.222 | 0.038 | 11.143 | 1 | 286 | 0.001 |
| 2 | 0.200 (b) | 0.040 | 0.033 | 12.227 | 0.003 | 0.759 | 1 | 285 | 0.384 |
| 3 | 0.683 (c) | 0.466 | 0.460 | 9.136 | 0.426 | 26.520 | 1 | 284 | 0.000 |
| 4 | 0.697 (d) | 0.486 | 0.479 | 8.978 | 0.020 | 11.074 | 1 | 283 | 0.001 |
| 5 | 0.703 (e) | 0.494 | 0.485 | 8.928 | 0.008 | 4.199 | 1 | 282 | 0.041 |
| 6 | 0.711 (f) | 0.506 | 0.495 | 8.834 | 0.012 | 6.999 | 1 | 281 | 0.009 |
| 7 | 0.715 (g) | 0.512 | 0.500 | 8.798 | 0.006 | 3.335 | 1 | 280 | 0.069 |
| 8 | 0.717 (h) | 0.514 | 0.500 | 8.795 | 0.002 | 1.143 | 1 | 279 | 0.286 |
| 9 | 0.719 (i) | 0.517 | 0.501 | 8.784 | 0.003 | 1.718 | 1 | 278 | 0.191 |
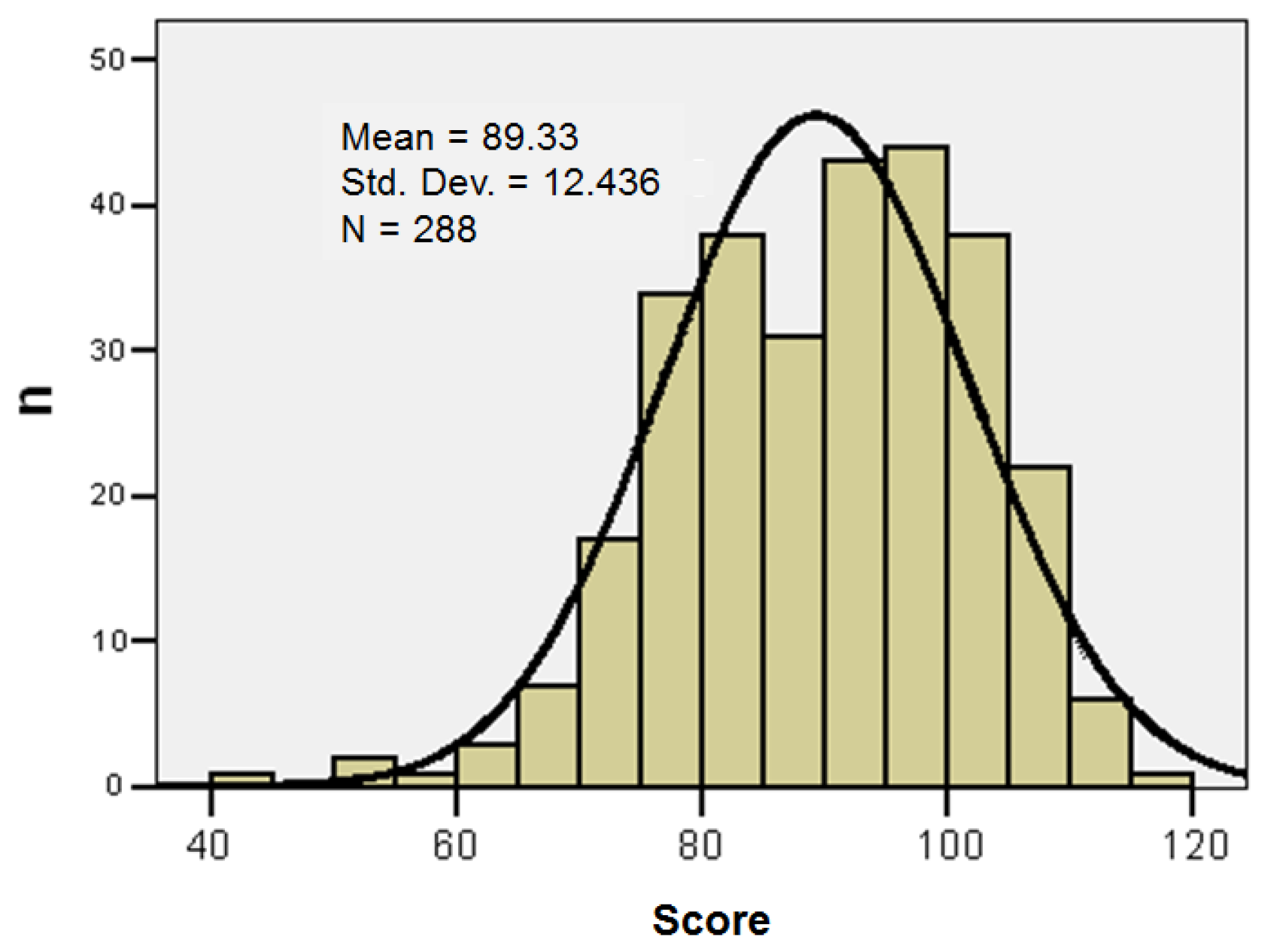
| N | 288 | |
|---|---|---|
| Mean | 89.33 | |
| Median | 91 | |
| Standard Deviation | 12.44 | |
| Variance | 13.93 | |
| Skewness Test | −0.473 | |
| Standard Error Skewness | 0.144 | |
| Minimum | 43 | |
| Maximum | 118 | |
| Percentile | 25 | 80 |
| 50 | 91 | |
| 75 | 99 | |
| Score | n | % |
|---|---|---|
| Low | 65 | 22.6 |
| Moderate | 156 | 54.2 |
| High | 67 | 23.3 |
| Items/Demographics | Low Score (n = 65) | Moderate Score (n = 156) | High Score (n = 67) | Chi-Squared Test (p) | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Female | 59 | 90.8 | 149 | 95.5 | 61 | 91.0 | 0.292 |
| Age > 40 years | 48 | 73.8 | 115 | 73.7 | 46 | 68.7 | 0.753 |
| Length of service > 15 years | 47 | 72.3 | 101 | 64.7 | 42 | 62.7 | 0.196 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Luchian, N.; Guțu, C.; Pleșea-Condratovici, A.; Salim, C.; Ciuhodaru, M.I.; Stafie, L.; Popescu, M.R.; Matei, M.N.; Voinescu, D.C.; Duceac, M.; et al. Healthcare-Associated Infections: Knowledge Score and Awareness Among Nurses in Hospitals from North-East Romania. Healthcare 2026, 14, 44. https://doi.org/10.3390/healthcare14010044
Luchian N, Guțu C, Pleșea-Condratovici A, Salim C, Ciuhodaru MI, Stafie L, Popescu MR, Matei MN, Voinescu DC, Duceac M, et al. Healthcare-Associated Infections: Knowledge Score and Awareness Among Nurses in Hospitals from North-East Romania. Healthcare. 2026; 14(1):44. https://doi.org/10.3390/healthcare14010044
Chicago/Turabian StyleLuchian, Nicoleta, Cristian Guțu, Alina Pleșea-Condratovici, Camer Salim, Mădălina Irina Ciuhodaru, Liviu Stafie, Mihaela Roxana Popescu, Mădalina Nicoleta Matei, Doina Carina Voinescu, Mădălina Duceac (Covrig), and et al. 2026. "Healthcare-Associated Infections: Knowledge Score and Awareness Among Nurses in Hospitals from North-East Romania" Healthcare 14, no. 1: 44. https://doi.org/10.3390/healthcare14010044
APA StyleLuchian, N., Guțu, C., Pleșea-Condratovici, A., Salim, C., Ciuhodaru, M. I., Stafie, L., Popescu, M. R., Matei, M. N., Voinescu, D. C., Duceac, M., Elkan, E. M., & Duceac, L. D. (2026). Healthcare-Associated Infections: Knowledge Score and Awareness Among Nurses in Hospitals from North-East Romania. Healthcare, 14(1), 44. https://doi.org/10.3390/healthcare14010044






