Multimodal Prehabilitation in Colorectal Cancer: Improving Fitness, Lifestyle, and Post-Surgery Outcomes
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
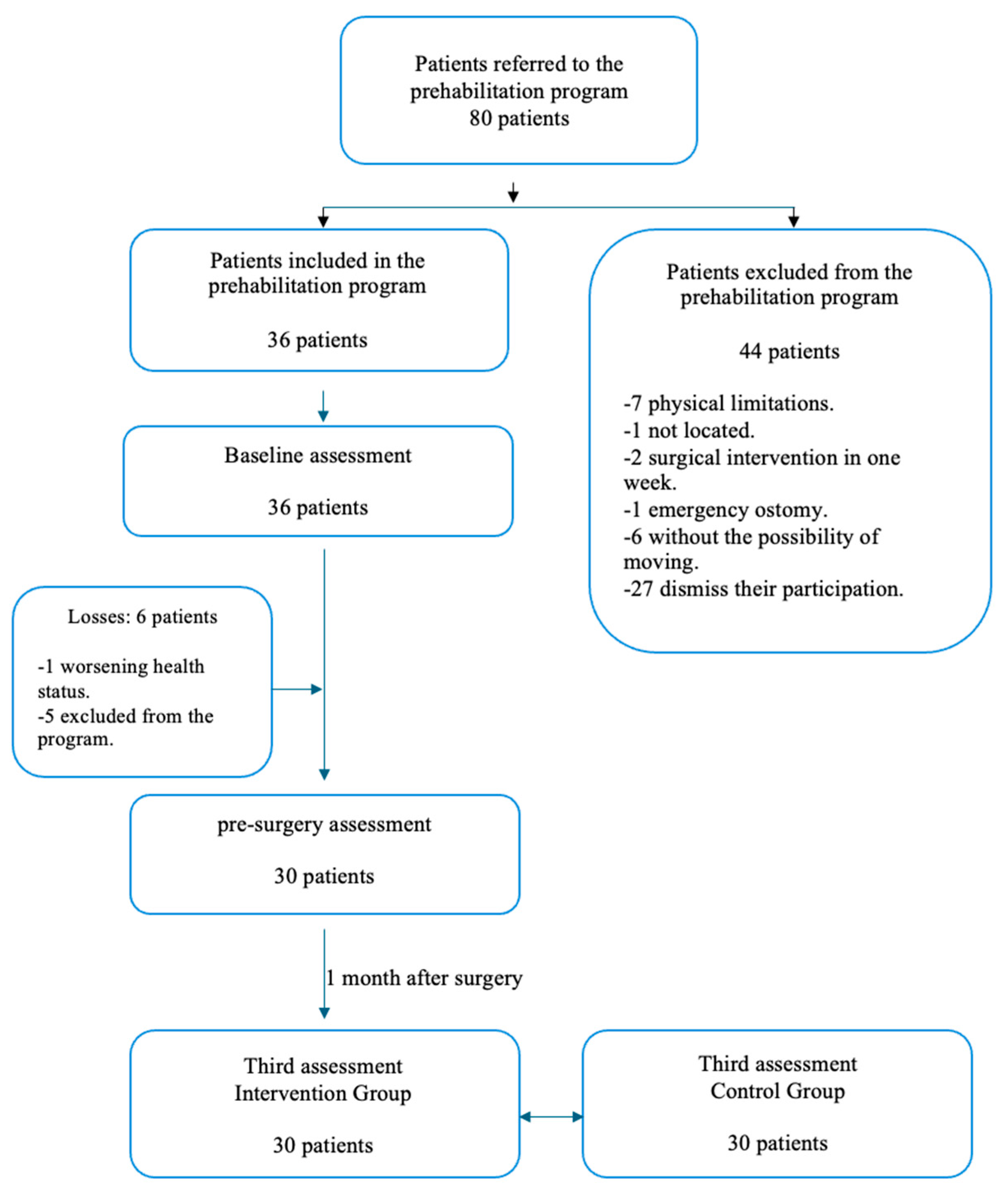
2.2. Sample
2.2.1. Selection Criteria
2.2.2. Sample Size Calculation
2.3. Intervention
2.3.1. Health Education and Self-Care
2.3.2. Nutritional Counseling
2.3.3. Psychological Support
2.3.4. Supervised Physical Exercise
2.4. Outcomes
2.5. Assessments
2.6. Statistical Analysis
2.7. Ethical Considerations
3. Results
3.1. Participants and Sociodemographic Characteristics
3.2. Anthropometry and Body Composition
3.3. Anxiety and Malnutrition Screening
3.4. Physical and Cardiorespiratory Fitness
3.5. Minutes According to the Activity Level of the Participants
3.6. Surgical Variables
4. Discussion
Strengths and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 6MWT | Six minutes walking test |
| BMI | Body mass index |
| CMJ | Counter-movement jump |
| FTSTS | Five sit to stand |
| HUGCS | Hospital Universitario General de Castellón |
| MUST | Malnutrition universal screening tool |
| SCT | Stair climbing test |
| SJ | Squat jump |
| STAI-S | State-trait anxiety inventory-state |
| TUG | Time up and go |
References
- Suárez-Alcázar, M.P.; Collado-Boira, E.J.; Recacha-Ponce, P.; Salas-Medina, P.; García-Roca, M.E.; Hernando, C.; Muriach, M.; Baliño, P.; Flores-Buils, R.; Latorre, M.L.M.; et al. Prehabilitation Consultation on Self-Care and Physical Exercise in Patients Diagnosed with Abdominopelvic Cancer: Protocol of the Study. Healthcare 2024, 12, 1423. [Google Scholar] [CrossRef] [PubMed]
- Mina, D.S.; Brahmbhatt, P.; Lopez, C.; Baima, J.; Gillis, C.; Trachtenberg, L.; Silver, J.K. The Case for Prehabilitation Prior to Breast Cancer Treatment. Phys. Med. Rehabil. 2017, 9, S305–S316. [Google Scholar] [CrossRef]
- Wu, F.; Laza-Cagigas, R.; Pagarkar, A.; Olaoke, A.; El Gammal, M.; Rampal, T. The Feasibility of Prehabilitation as Part of the Breast Cancer Treatment Pathway. Phys. Med. Rehabil. 2021, 13, 1237–1246. [Google Scholar] [CrossRef] [PubMed]
- Falandry, C.; Fauvet, R.; Alfonsi, P.; Foulon, A.; Texier, C.; Bourdel, N.; Simonet, T.; Azaïs, H.; Lambaudie, E. Combining prehabilitation with enhanced recovery programs in gynecological surgery. J. Gynecol. Obstet. Hum. Reprod. 2022, 51, 102376. [Google Scholar] [CrossRef]
- Treanor, C.; Kyaw, T.; Donnelly, M. An international review and meta-analysis of prehabilitation compared to usual care for cancer patients. J. Cancer Surviv. 2018, 12, 64–73. [Google Scholar] [CrossRef]
- Yang, A.; Sokolof, J.; Gulati, A. The effect of preoperative exercise on upper extremity recovery following breast cancer surgery: A systematic review. Int. J. Rehabil. Res. 2018, 41, 189–196. [Google Scholar] [CrossRef]
- Brito-Baños, C. Surgical prehabilitation in oncology patients: Is it possible in our environment? Rev. Mex. Anest. 2019, 42, 198–200. [Google Scholar]
- Amaro-Gahete, F.J.; Jurado, J.; Cisneros, A.; Corres, P.; Marmol-Perez, A.; Osuna-Prieto, F.J.; Fernández-Escabias, M.; Salcedo, E.; Hermán-Sánchez, N.; Gahete, M.D.; et al. Multidisciplinary Prehabilitation and Postoperative Rehabilitation for Avoiding Complications in Patients Undergoing Resection of Colon Cancer: Rationale, Design, and Methodology of the ONCOFIT Study. Nutrients 2022, 14, 4647. [Google Scholar] [CrossRef]
- Berkel, A.E.M.; Bongers, B.C.; Kotte, H.; Weltevreden, P.; de Jongh, F.H.C.; Eijsvogel, M.M.M.; Wymenga, M.; Bigirwamungu-Bargeman, M.; van der Palen, J.; van Det, M.J.; et al. Effects of Community-based Exercise Prehabilitation for Patients Scheduled for Colorectal Surgery with High Risk for Postoperative Complications: Results of a Randomized Clinical Trial. Ann. Surg. 2022, 275, e299–e306. [Google Scholar] [CrossRef]
- Wang, X.; Chen, R.; Ge, L.; Gu, Y.; Zhang, L.; Wang, L.; Zhuang, C.; Wu, Q. Effect of short-term prehabilitation of older patients with colorectal cancer: A propensity score-matched analysis. Front. Oncol. 2023, 13, 1076835. [Google Scholar] [CrossRef]
- Raichurkar, P.; Denehy, L.; Solomon, M.; Koh, C.; Pillinger, N.; Hogan, S.; McBride, K.; Carey, S.; Bartyn, J.; Hirst, N.; et al. Research Priorities in Prehabilitation for Patients Undergoing Cancer Surgery: An International Delphi Study. Ann. Surg. Oncol. 2023, 30, 7226–7235. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Carli, F.; Lee, L.; Charlebois, P.; Stein, B.; Liberman, A.S.; Kaneva, P.; Augustin, B.; Wongyingsinn, M.; Gamsa, A.; et al. Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: A pilot study. Surg. Endosc. 2013, 27, 1072–1082. [Google Scholar] [CrossRef] [PubMed]
- van Rooijen, S.; Carli, F.; Dalton, S.; Thomas, G.; Bojesen, R.; Le Guen, M.; Barizien, N.; Awasthi, R.; Minnella, E.; Beijer, S.; et al. Multimodal prehabilitation in colorectal cancer patients to improve functional capacity and reduce postoperative complications: The first international randomized controlled trial for multimodal prehabilitation. BMC Cancer 2019, 19, 98. [Google Scholar] [CrossRef] [PubMed]
- Molenaar, C.J.L.; Reudink, M.; Sabajo, C.R.; Janssen, L.; Roumen, R.M.H.; Klaase, J.M.; Slooter, G.D. Prehabilitation for patients with colorectal cancer: A snapshot of current daily practice in Dutch hospitals. Perioper. Med. 2023, 12, 15. [Google Scholar] [CrossRef]
- Bruns, E.R.; van Rooijen, S.J.; Argillander, T.E.; van der Zaag, E.S.; van Grevenstein, W.M.; van Duijvendijk, P.; Buskens, C.J.; Bemelman, W.A.; van Munster, B.C.; Slooter, G.D.; et al. Improving Outcomes in Oncological Colorectal Surgery by Prehabilitation. Am. J. Phys. Med. Rehabil. 2019, 98, 231–238. [Google Scholar] [CrossRef]
- Chabner, B.A.; Lynch, T.J.; Longo, D.L. Harrison Oncology Manual, 1st ed.; McGraw-Hill: New York, NY, USA, 2009; pp. 423–429. [Google Scholar]
- Moreira-Gonçalvez, D. Prehabilitation fulfilling an unmet need of the preoperative care. Rev. Port. Cirugía 2021, 51, 9–12. [Google Scholar] [CrossRef]
- Bojesen, R.D.; Jørgensen, L.B.; Grube, C.; Skou, S.T.; Johansen, C.; Dalton, S.O.; Gögenur, I. Fit for Surgery feasibility of short course multi modal individualized prehabilitation in high-risk frail colon cancer patients prior to surgery. Pilot Feasibility Stud. 2022, 8, 11. [Google Scholar] [CrossRef]
- Bojesen, R.D.; Dalton, S.O.; Skou, S.T.; Jørgensen, L.B.; Walker, L.R.; Eriksen, J.R.; Grube, C.; Justesen, T.F.; Johansen, C.; Slooter, G.; et al. Preoperative multimodal prehabilitation before elective colorectal cancer surgery in patients with WHO performance status I or II: Randomized clinical trial. BJS Open 2023, 7, zrad134. [Google Scholar] [CrossRef]
- Bruns, E.R.; Argillander, T.E.; Schuijt, H.J.; van Duijvendijk, P.; van der Zaag, E.S.; Wassenaar, E.B.; Gerhards, M.F.; Consten, E.C.; Buskens, C.J.; van Munster, B.C.; et al. Fit4SurgeryTV At-home Prehabilitation for Frail Older Patients Planned for Colorectal Cancer Surgery: A Pilot Study. Am. J. Phys. Med. Rehabil. 2019, 98, 399–406. [Google Scholar] [CrossRef]
- Awasthi, R.; Minnella, E.M.; Ferreira, V.; Ramanakumar, A.V.; Scheede-Bergdahl, C.; Carli, F. Supervised exercise training with multimodal pre-habilitation leads to earlier functional recovery following colorectal cancer resection. Acta Anaesthesiol. Scand. 2019, 63, 461–467. [Google Scholar] [CrossRef]
- Wu, F.; Rotimi, O.; Laza-Cagigas, R.; Rampal, T. The Feasibility and Effects of a Telehealth-Delivered Home-Based Prehabilitation Program for Cancer Patients during the Pandemic. Curr. Oncol. 2021, 28, 2248–2259. [Google Scholar] [CrossRef] [PubMed]
- Waller, E.; Sutton, P.; Rahman, S.; Allen, J.; Saxton, J.; Aziz, O. Prehabilitation with wearables versus standard of care before major abdominal cancer surgery: A randomized controlled pilot study (trial registration: NCT04047524). Surg. Endosc. 2022, 36, 1008–1017. [Google Scholar] [CrossRef] [PubMed]
- van Rooijen, S.J.; Molenaar, C.J.; Schep, G.; van Lieshout, R.H.; Beijer, S.; Dubbers, R.; Rademakers, N.; Papen-Botterhuis, N.E.; van Kempen, S.; Carli, F.; et al. Making Patients Fit for Surgery: Introducing a Four Pillar Multimodal Prehabilitation Program in Colorectal Cancer. Am. J. Phys. Med. Rehabil. 2019, 98, 888–896. [Google Scholar] [CrossRef] [PubMed]
- Carli, F.; Bousquet-Dion, G.; Awasthi, R.; Elsherbini, N.; Liberman, S.; Boutros, M.; Stein, B.; Charlebois, P.; Ghitulescu, G.; Morin, N.; et al. Effect of Multimodal Prehabilitation vs Postoperative Rehabilitation on 30-Day Postoperative Complications for Frail Patients Undergoing Resection of Colorectal Cancer: A Randomized Clinical Trial. JAMA Surg. 2020, 155, 233–242. [Google Scholar] [CrossRef]
- Furyk, C.; Senthuran, S.; Nye, D.; Ho, Y.H.; Leicht, A.S. Prehabilitation for Frail Patients Undergoing Colorectal Surgery: Lessons Learnt from a Randomized Feasibility Study. Front. Rehabil. Sci. 2021, 2, 650835. [Google Scholar] [CrossRef]
- Ministerio de Sanidad; Instituto Aragonés de Ciencias de la Salud; Grupo Español de Rehabilitación Multimodal (GERM). Vía Clínica de Recuperación intensificada en Cirugía del Adulto (RICA). 2021. Available online: https://seguridaddelpaciente.sanidad.gob.es/informacion/publicaciones/2021/rica.htm (accessed on 3 February 2025).
- Usquiano-Cardenas, G.A. Self-Care Agency in Breast Cancer Patients Undergoing Cancer Treatment in the National Hospital Edgardo Rebagliati Martins; Privacy University Norbert Wiener: Lima, Perú, 2021. [Google Scholar]
- Romero-Ruiz, A.; Gómez-Salgado, J.; Bennasar-Veny, M. Cancer Treatments. Principles, Therapeutics and Evolutionary Response, 1st ed.; FUDEN: Madrid, Spain, 2008. [Google Scholar]
- Hojman, P.; Gehl, J.; Christensen, J.F.; Pedersen, B.K. Molecular Mechanisms Linking Exercise to Cancer Prevention and Treatment. Cell Metab. 2018, 27, 10–21. [Google Scholar] [CrossRef]
- West, M.; Loughney, L.; Lythgoe, D.; Barben, C.; Sripadam, R.; Kemp, G.; Grocott, M.; Jack, S. Effect of prehabilitation on objectively measured physical fitness after neoadjuvant treatment in preoperative rectal cancer patients: A blinded interventional pilot study. Br. J. Anaesth. 2015, 114, 244–251. [Google Scholar] [CrossRef]
- Lucia, A.; Alejo, L.; Pagola-Aldazabal, I.; Fiuza-Luces, C.; Huerga, D.; de Torres, M.; Verdugo, A.; Solano, M.O.; Felipe, J.; Ruiz-Casado, A. Exercise prehabilitation program for patients under neoadjuvant treatment for rectal cancer: A pilot study. J. Cancer Res. Ther. 2019, 15, 20–25. [Google Scholar] [CrossRef]
- Fernandez, P. Guía: Determinación del Tamaño Muestral—Fisterra. 1996. Available online: https://www.fisterra.com/formacion/metodologia-investigacion/determinacion-tamano-muestral/#sec6 (accessed on 22 April 2023).
- Borg, G. Borg’s Perceived Exertion and Pain Scales. Hum. Kinet. 1998. Available online: https://psycnet.apa.org/record/1998-07179-000 (accessed on 23 January 2025).
- Byrne, N.M.; Hills, A.P.; Hunter, G.R.; Weinsier, R.L.; Schutz, Y.; Byrne, N.M. Metabolic equivalent: One size does not fit all. J. Appl. Physiol. 2005, 99, 1112–1119. [Google Scholar] [CrossRef]
- Esparza, F.; Aragonés, M.; Casajús, J.; Rodriguez, F.; Cabañas, M. Manual de Cineantropometría; FEMEDE: Madrid, Spain, 1984. [Google Scholar]
- Jimenez, Y.A.; Cumming, S.; Wang, W.; Stuart, K.; Thwaites, D.I.; Lewis, S.J. Patient education using virtual reality increases knowledge and positive experience for breast cancer patients undergoing radiation therapy. Support. Care Cancer 2018, 26, 2879–2888. [Google Scholar] [CrossRef]
- Gupta, A.; Gupta, E.; Hilsden, R.; Hawel, J.D.; Elnahas, A.I.; Schlachta, C.M.; Alkhamesi, N.A. Preoperative malnutrition in patients with colorectal cancer. Can. J. Surg. 2021, 64, E621–E629. [Google Scholar] [CrossRef] [PubMed]
- Stratton, R.J.; Hackston, A.; Longmore, D.; Dixon, R.; Price, S.; Stroud, M.; King, C.; Elia, M. Malnutrition in hospital outpatients and inpatients: Prevalence, concurrent validity and ease of use of the ‘malnutrition universal screening tool’ (‘MUST’) for adults. Br. J. Nutr. 2004, 92, 799–808. [Google Scholar] [CrossRef] [PubMed]
- NutriActiva. Dynamometer Camry. Available online: https://nutriactiva.com/es/products/camry-dynamometer (accessed on 5 February 2025).
- De Blas, X.; Padullés, J.M.; Del Amo, J.L.L.; Guerra-Balic, M. Creation and Validation of Chronojump-Boscosystem: A Free Tool to Measure Vertical Jumps. Rev. Int. Cienc. Deport. 2012, 8, 334–356. [Google Scholar] [CrossRef]
- Centeno-Pradas, R.A. Reference Values for Jumps on a Dynamometric Platform in a Population of Andalusian Athletes. Ph.D. Thesis, Universidad Pablo de Olavide, Sevilla, Spain, July 2013. [Google Scholar]
- van Soom, T.; Gebruers, N.; Tjalma, W.; Schep, G.; van Breda, E. Physical Testing in Cancer Patients: Practical Testing in a Clinical Setting. Arch. Health Sci. Res. 2021, 8, 77–88. [Google Scholar] [CrossRef]
- Hadzibegovic, S.; Porthun, J.; Lena, A.; Weinländer, P.; Lück, L.C.; Potthoff, S.K.; Rösnick, L.; Fröhlich, A.; Ramer, L.V.; Sonntag, F.; et al. Hand grip strength in patients with advanced cancer: A prospective study. J. Cachex-Sarcopenia Muscle 2023, 14, 1682–1694. [Google Scholar] [CrossRef]
- Waterland, J.L.; McCourt, O.; Edbrooke, L.; Granger, C.L.; Ismail, H.; Riedel, B.; Denehy, L. Efficacy of Prehabilitation Including Exercise on Postoperative Outcomes Following Abdominal Cancer Surgery: A Systematic Review and Meta-Analysis. Front. Surg. 2021, 8, 628848. [Google Scholar] [CrossRef]
- Wells, K.F.; Dillon, E.K. The sit and reach a test of back and leg flexibility. Res. Q. Am. Assoc. Health Phys. Educ. Recreat. 1952, 23, 115–118. [Google Scholar] [CrossRef]
- León-Reyes, L.I.; Canto, P.; Coral-Vázquez, R.M. The muscle and cancer: A bidirectional relationship. Pathophysiology and con sequences. Disabil. Res. 2023, 9, 136–146. [Google Scholar]
- Schmidt, K.; Vogt, L.; Thiel, C.; Jäger, E.; Banzer, W. Validity of the Six-Minute Walk Test in Cancer Patients. Int. J. Sport Med. 2013, 34, 631–636. [Google Scholar] [CrossRef]
- Moriello, C.; Mayo, N.E.; Feldman, L.; Carli, F. Validating the Six-Minute Walk Test as a Measure of Recovery After Elective Colon Resection Surgery. Arch. Phys. Med. Rehabil. 2008, 89, 1083–1089. [Google Scholar] [CrossRef]
- Esliger, D.W.; Rowlands, A.V.; Hurst, T.L.; Catt, M.; Murray, P.; Eston, R.G. Validation of the GENEA accelerometer. Med. Sci. Sports Exerc. 2011, 43, 1085–1093. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; A Wanigatunga, A.; A Schrack, J. Assessment of Physical Activity in Adults Using Wrist Accelerometers. Epidemiol. Rev. 2021, 43, 65–93. [Google Scholar] [CrossRef] [PubMed]
- Fisher, M.I.; Davies, C.C.; Uhl, T.L. A quantitative comparison of arm activity between survivors of breast cancer and healthy controls: Use of accelerometry. Support. Care Cancer 2020, 28, 5307–5313. [Google Scholar] [CrossRef] [PubMed]
- Evenson, K.R.; Scherer, E.; Peter, K.M.; Cuthbertson, C.C.; Eckman, S. Historical development of accelerometry measures and methods for physical activity and sedentary behavior research worldwide: A scoping review of observational studies of adults. PLoS ONE 2022, 17, e0276890. [Google Scholar] [CrossRef]
- Klein, I.; Danzi, S. Thyroid disease and the heart. Circulation 2007, 116, 1725–1735. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.-A. Classification of Surgical Complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect size estimates: Current use, calculations, and interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef]
- Lenhard, W.; Lenhard, A. Computation of Different Effect; Psychometrica: Dettelbach, Germany, 2016; Available online: https://www.psychometrica.de/effect_size.html (accessed on 7 June 2021).
- Northgraves, M.J.; Arunachalam, L.; Madden, L.A.; Marshall, P.; Hartley, J.E.; MacFie, J.; Vince, R.V. Feasibility of a novel exercise prehabilitation programme in patients scheduled for elective colorectal surgery: A feasibility randomised controlled trial. Support. Care Cancer 2020, 28, 3197–3206. [Google Scholar] [CrossRef]
- Jones, S.E.; Kon, S.S.C.; Canavan, J.L.; Patel, M.S.; Clark, A.L.; Nolan, C.M.; I Polkey, M.; Man, W.D.-C. The five-repetition sit-to-stand test as a functional outcome measure in COPD. Thorax 2013, 68, 1015–1020. [Google Scholar] [CrossRef]
- Dronkers, J.J.; Lamberts, H.; Reutelingsperger, I.M.M.D.; Naber, R.H.; Dronkers-Landman, C.M.; Veldman, A.; Van Meeteren, N.L.U. Preoperative therapeutic programme for elderly patients scheduled for elective abdominal oncological surgery: A randomized controlled pilot study. Clin. Rehabil. 2010, 24, 614–622. [Google Scholar] [CrossRef]
- Bogani, G.; Sarpietro, G.; Ferrandina, G.; Gallotta, V.; DI Donato, V.; Ditto, A.; Pinelli, C.; Casarin, J.; Ghezzi, F.; Scambia, G.; et al. Enhanced recovery after surgery (ERAS) in gynecology oncology. Eur. J. Surg. Oncol. 2021, 47, 952–959. [Google Scholar] [CrossRef] [PubMed]
- Fulop, A.; Lakatos, L.; Susztak, N.; Szijarto, A.; Banky, B. The effect of trimodal prehabilitation on the physical and psychological health of patients undergoing colorectal surgery: A randomised clinical trial. Anaesthesia 2020, 76, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Gillis, C.; Li, C.; Lee, L.; Awasthi, R.; Augustin, B.; Gamsa, A.; Liberman, A.S.; Stein, B.; Charlebois, P.; Feldman, L.S.; et al. Prehabilitation versus Rehabilitation. A Randomized Control Trial in Patients Undergoing Colorectal Resection for Cancer. Anesthesiology 2014, 121, 937–947. [Google Scholar] [CrossRef] [PubMed]
- López-Rodríguez-Arias, F.; Sánchez-Guillén, L.; Aranaz-Ostáriz, V.; Triguero-Cánovas, D.; Lario-Pérez, S.; Barber-Valles, X.; Lacueva, F.J.; Ramirez, J.M.; Arroyo, A. Effect of home-based prehabilitation in an enhanced recovery after surgery program for patients undergoing colorectal cancer surgery during the COVID-19 pandemic. Support. Care Cancer 2021, 29, 7785–7791. [Google Scholar] [CrossRef]
| Male | Female | Both Male and Female | p-Value | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Sex | 17 | 56.7% | 13 | 43.3% | 30 | 100% | |
| Marital status | 0.125 | ||||||
| Single | 3 | 17.6% | 1 | 7.7% | 4 | 13.3% | |
| Married or in a relationship | 13 | 76.5% | 8 | 61.5% | 21 | 70.0% | |
| Widowed | 2 | 15.4% | 2 | 6.7% | |||
| Separated or divorced | 1 | 5.9% | 2 | 15.4% | 3 | 10% | |
| Study level | 0.397 | ||||||
| Primary | 7 | 41.2% | 7 | 53.8% | 14 | 46.7% | |
| High-School | 7 | 41.2% | 5 | 38.5% | 12 | 40.0% | |
| University | 3 | 17.6% | 1 | 7.7% | 4 | 13.35% | |
| Employment Status | |||||||
| Employed | 5 | 29.4% | 0 | 0% | 5 | 16.7% | 0.330 |
| Unemployed | 12 | 70.6% | 13 | 100% | 25 | 83.3% | |
| mean ± sd | mean ± sd | mean ± sd | p-Value | ||||
| Age (years) | 66.53 ± 8.01 | 62.54 ± 10.1 | 64.8 ± 9.08 | 0.240 | |||
| Sons (number) | 1.47 ± 0.94 | 1.31 ± 0.75 | 1.4 ± 0.85 | 0.614 | |||
| Height (meters) | 1.70 ± 0.55 | 1.55 ± 0.06 | 1.63 ± 0.09 | ||||
| VARIABLES | Male | Female | Both Male and Female | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | p-Value/d | Pre | Post | p-Value/d | Pre | Post | p-Value/d | |
| Mean ± sd | Mean ± sd | Mean ± sd | Mean ± sd | Mean ± sd | Mean ± sd | ||||
| Weigh (kg) | 83.32 ± 11.51 | 83.19 ± 11.89 | 0.917 | 65.37 ± 15.80 | 65.57 ± 15.91 | 0.327 | 75.55 ± 16.07 | 75.56 ± 16.17 | 0.647 |
| BMI (kg/m2) | 28.24 ± 4.10 | 28.52 ± 4.17 | 0.394 | 27.37 ± 7.20 | 27.44 ± 7.20 | 0.412 | 27.86 ± 5.56 | 28.05 ± 5.60 | 0.526 |
| % body fat | 29.62 ± 8.88 | 28.69 ± 8.89 | 0.028/0.10 | 34.93 ± 9.64 | 34.90 ± 9.32 | 0.944 | 31.92 ± 9.44 | 31.38 ± 9.45 | 0.054 |
| Muscle mass (kg) | 32.47 ± 4.85 | 32.57 ± 4.95 | 0.736 | 21.79 ± 3.90 | 21.86 ± 3.87 | 0.581 | 27.84 ± 6.94 | 27.93 ± 6.99 | 0.616 |
| Male | Female | Both Male and Female | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | p-Value/d | Pre | Post | p-Value/d | Pre | Post | p-Value/d | |
| Mean ± sd | Mean ± sd | Mean ± sd | Mean ± sd | Mean ± sd | Mean ± sd | ||||
| Strength (kg) | |||||||||
| Right | 37.71 ± 9.19 | 38.87 ± 8.71 | 0.109 | 22.48 ± 3.39 | 22.62 ± 3.26 | 0.624 | 31.11 ± 10.50 | 31.83 ± 10.65 | 0.120 |
| Left | 35.12 ± 9.09 | 35.68 ± 7.94 | 0.378 | 20.50 ± 4.32 | 20.63 ± 4.49 | 0.972 | 28.82 ± 10.35 | 29.16 ± 10.04 | 0.502 |
| SJ (cm) | 14.17 ± 6.13 | 14.85 ± 5.33 | 0.121 | 8.66 ± 1.97 | 9.58 ± 2.52 | 0.099 | 11.89 ± 5.56 | 12.67 ± 5.07 | 0.021/0.14 |
| SJ (W) | 699.13 ± 182.72 | 679.21 ± 148.74 | 0.469 | 402.18 ± 182.72 | 435.05 ± 108.81 | 0.023/0.21 | 558.67 ± 203.10 | 578.18 ± 169.74 | 0.043/0.10 |
| CMJ (cm) | 15.66 ± 6.69 | 15.96 ± 5.91 | 0.569 | 10.14 ± 2.18 | 9.89 ± 2.73 | 0.638 | 13.37 ± 5.92 | 13.45 ± 5.67 | 0.802 |
| CMJ (W) | 701.47 ± 190.36 | 1043.21 ± 1363.64 | 0.234 | 513.51 ± 266.24 | 439.54 ± 98.455 | 0.209 | 623.69 ± 239.64 | 793.43 ± 1076.08 | 0.855 |
| Chair-Stand | 19.47 ± 3.04 | 21.71 ± 3.73 | 0.021/0.65 | 28.31 ± 3.47 | 31.71 ± 2.83 | 0.004/2.08 | 18.97 ± 3.23 | 21.73 ± 3.32 | 0.000/0.84 |
| Sit & Reach (cm) | −3.22 ± 11.62 | −2.20 ± 11.27 | 0.044/0.08 | 1.34 ± 9.91 | 3.06 ± 8.34 | 0.080 | −1.13 ± 10.95 | 0.23 ± 10.19 | 0.005/0.12 |
| 6MWT (m) | 544.71 ± 89.03 | 571.82 ± 68.23 | 0.044/0.34 | 505.23 ± 81.91 | 563.31 ± 109.47 | 0.008/0.60 | 527.6 ± 86.60 | 568.13 ± 86.86 | 0.001/0.46 |
| Pre (Mean ± sd) | Post (Mean ± sd) | p-Value/d | |
|---|---|---|---|
| Sedentary | |||
| Both sexes | 5981.56 ± 1289.70 | 5958.61 ± 1359.30 | 0.744 |
| Male | 5382.25 ± 1365.20 | 6396.50 ± 882.70 | 0.093 |
| Female | 6461.00 ± 992.95 | 5608.30 ± 1557.69 | 0.037/0.65 |
| Light | |||
| Both sexes | 3289.61 ± 1160.15 | 3288.28 ± 1331.05 | 0.744 |
| Male | 3810.00 ± 1288.33 | 2794.00 ± 644.32 | 0.093 |
| Female | 2873.30 ± 839.59 | 3683.70 ± 1582.76 | 0.037/0.63 |
| Moderate | |||
| Both sexes | 784.67 ± 356.60 | 811.94 ± 354.78 | 0.248 |
| Male | 841.75 ± 283.63 | 848.13 ± 299.29 | 0.889 |
| Female | 739.00 ± 399.80 | 783.00 ± 391.18 | 0.169 |
| Vigorous | |||
| Both sexes | 24.173 ± 71.15 | 21.17 ± 64.44 | 0.073 |
| Male | 46.00 ± 102.27 | 41.38 ± 92.49 | 0.173 |
| Female | 6.70 ± 79.59 | 5.00 ± 6.69 | 0.206 |
| Control (Mean ± sd) | Intervention (Mean ± sd) | p-Value/d | ||||
|---|---|---|---|---|---|---|
| Hospitalization (days) | 6.14 ± 4.98 | 5.45 ± 1.80 | 0.607 | |||
| Time in Resuscitation Unit (min) | 1488.08 ± 563 | 1118.77 ± 504 | 0.009/0.69 | |||
| Control (n (%)) | Intervención (n (%)) | |||||
| Type of Surgery | ||||||
| Laparoscopy | 25 (83.3%) | 30 (100%) | ||||
| Laparotomy | 2 (6.6%) | - | ||||
| Conversion from laparoscopy to laparotomy | 3 (10.1%) | - | ||||
| Ostomy | ||||||
| Yes | 1 (3.4%) | 7 (30%) | ||||
| No | 29 (96.6%) | 23 (70%) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suárez-Alcázar, M.-P.; Folch Ayora, A.; Muriach, M.; Recacha-Ponce, P.; Garcia-Roca, M.-E.; Coret-Franco, A.; Pastor-Mora, J.C.; Salas-Medina, P.; Collado-Boira, E.J. Multimodal Prehabilitation in Colorectal Cancer: Improving Fitness, Lifestyle, and Post-Surgery Outcomes. Healthcare 2025, 13, 1083. https://doi.org/10.3390/healthcare13091083
Suárez-Alcázar M-P, Folch Ayora A, Muriach M, Recacha-Ponce P, Garcia-Roca M-E, Coret-Franco A, Pastor-Mora JC, Salas-Medina P, Collado-Boira EJ. Multimodal Prehabilitation in Colorectal Cancer: Improving Fitness, Lifestyle, and Post-Surgery Outcomes. Healthcare. 2025; 13(9):1083. https://doi.org/10.3390/healthcare13091083
Chicago/Turabian StyleSuárez-Alcázar, María-Pilar, Ana Folch Ayora, María Muriach, Paula Recacha-Ponce, M.-Elena Garcia-Roca, Alba Coret-Franco, Juan Carlos Pastor-Mora, Pablo Salas-Medina, and Eladio J. Collado-Boira. 2025. "Multimodal Prehabilitation in Colorectal Cancer: Improving Fitness, Lifestyle, and Post-Surgery Outcomes" Healthcare 13, no. 9: 1083. https://doi.org/10.3390/healthcare13091083
APA StyleSuárez-Alcázar, M.-P., Folch Ayora, A., Muriach, M., Recacha-Ponce, P., Garcia-Roca, M.-E., Coret-Franco, A., Pastor-Mora, J. C., Salas-Medina, P., & Collado-Boira, E. J. (2025). Multimodal Prehabilitation in Colorectal Cancer: Improving Fitness, Lifestyle, and Post-Surgery Outcomes. Healthcare, 13(9), 1083. https://doi.org/10.3390/healthcare13091083








