Adult Triage in the Emergency Department: Introducing a Multi-Layer Triage System
Abstract
:1. Introduction
2. Evaluating Existing Scoring Systems
2.1. Symptom-Based Triage Systems—Clinical Impression Triage Systems
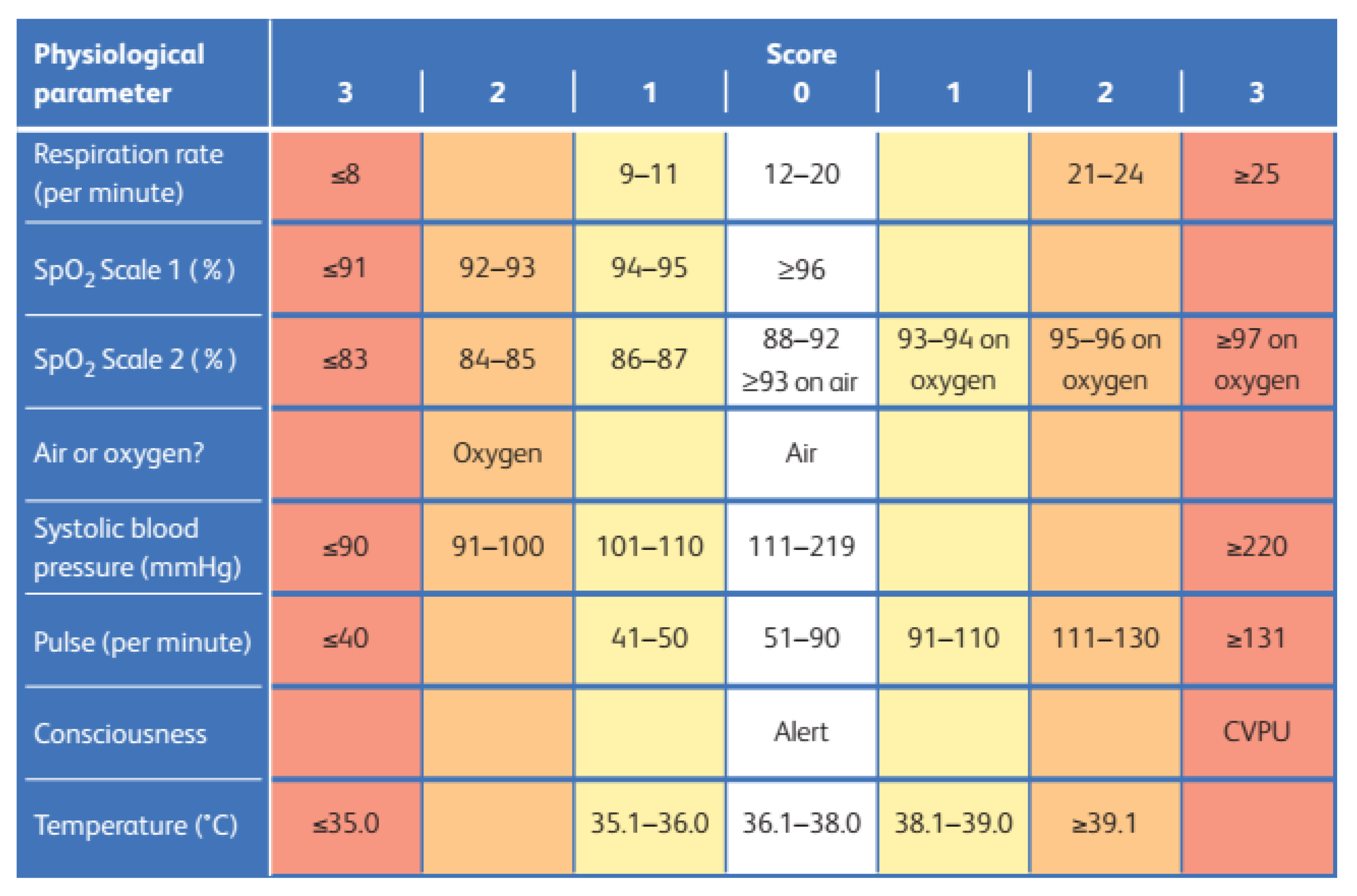
2.2. Early Warning Scores (EWSs)
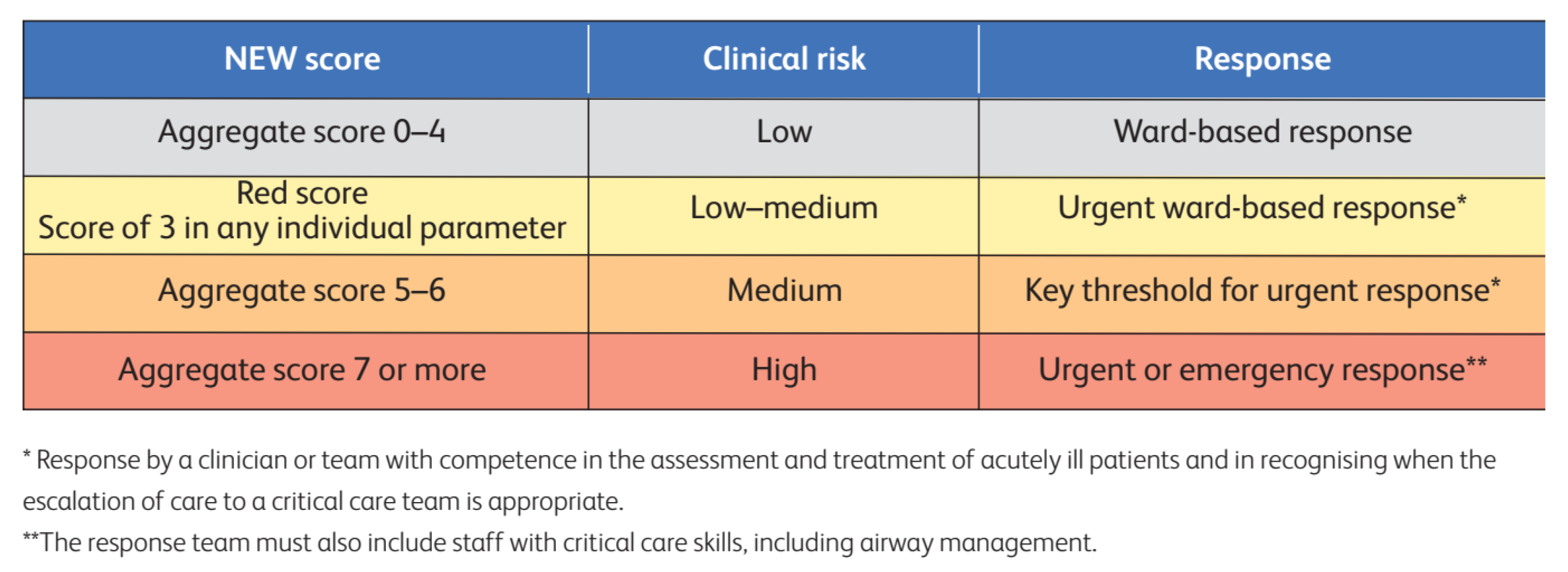
2.3. Specific Disease Scores
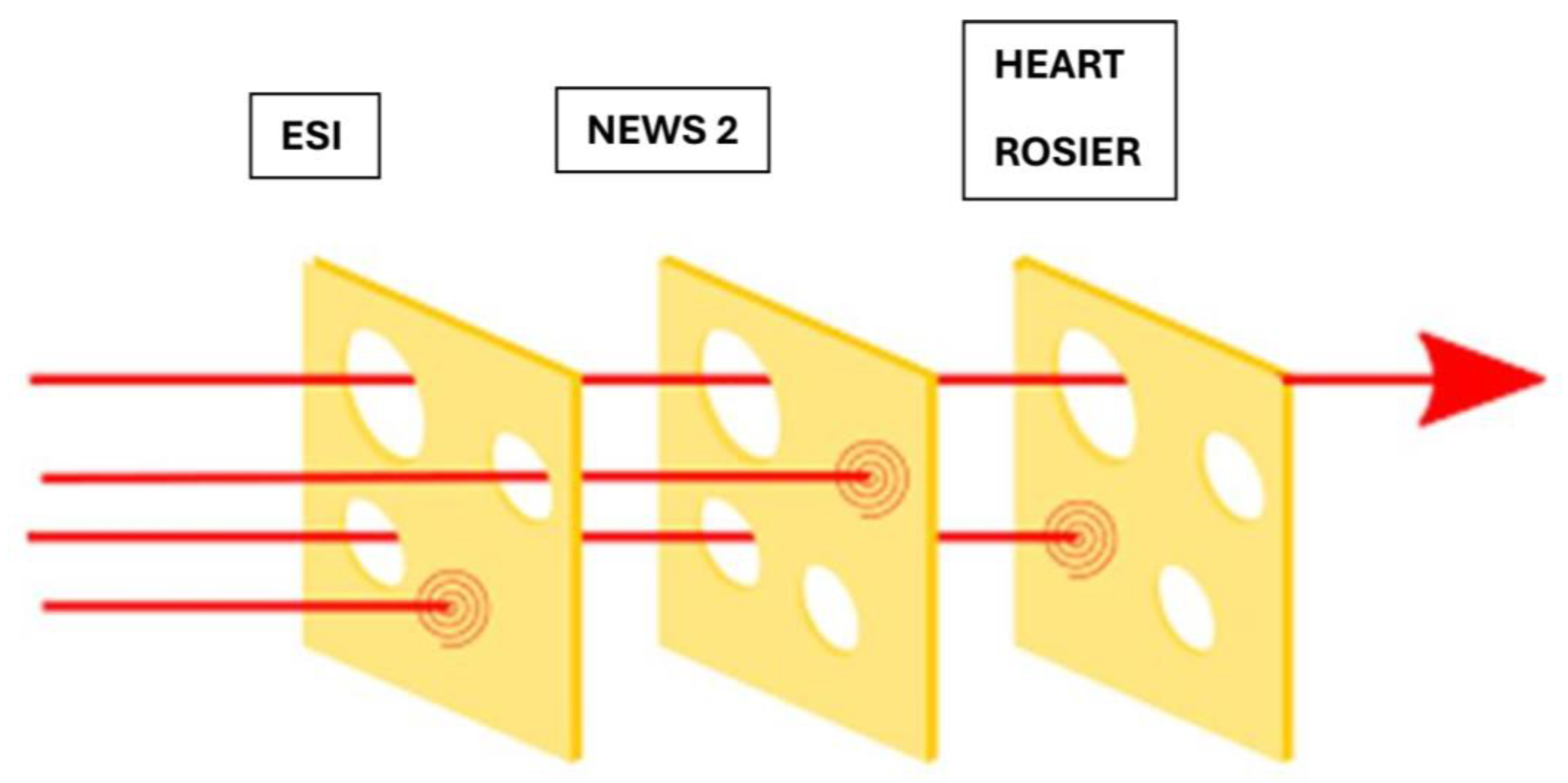
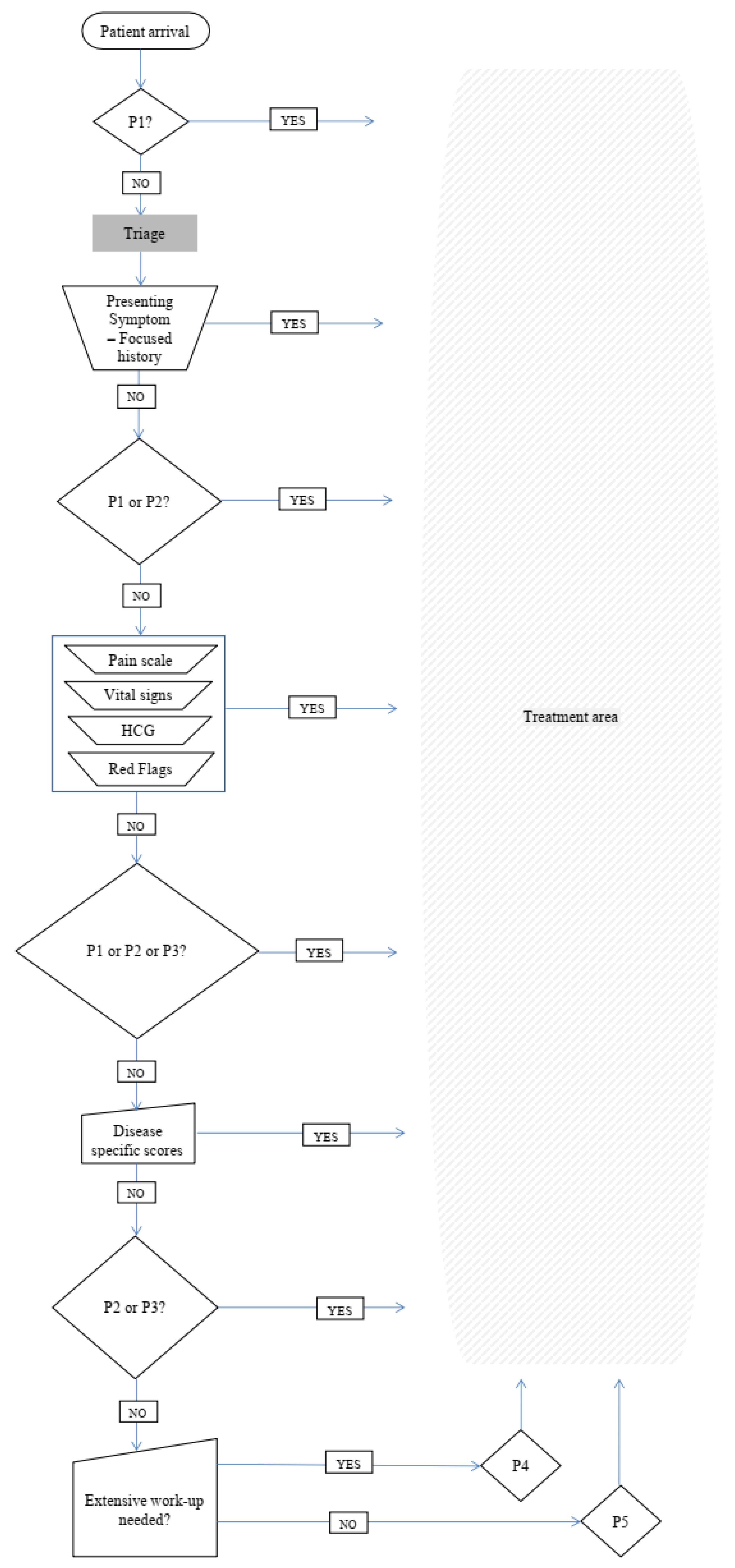
3. Proposing a Multilayer Triage System
- Seeking Priority 1 patients—Clinical impression.
- Use the basic principles of clinical impression triage systems such as ESI;
- “Is there an immediate risk for life or limb?”;
- If the answer is YES, the patient is Priority 1;
- If the answer is NO, proceed to the next step.
- Seeking Priority 2 Patients—Basic history taking and clinical impression.
- Use the basic principles of clinical impression triage systems such as ESI;
- “Is the patient’s condition serious enough or deteriorating so rapidly that there is the potential of threat to life or organ system failure?”;
- “Is the patient in severe pain?”;
- “Does the patient have altered mental status?”;
- “Are there any “Red Flags”?” CTAS, ATS, and MTS;
- If the answer is YES to any of the above questions, the Patient is Priority 2;
- If the answer is NO, proceed to the next step.
- Are you sure the Patient is NOT Priority 1 or 2?—Vital signs.
- Use NEWS 2 to interpret vital signs;
- Prioritize the patient according to the EWS you have chosen;
- NEWS2 Score > 7: the patient is Priority 2;
- NEWS2 Score 5–6 or a red score of 3 in any individual parameter: the patient is Priority 3
- NEWS2 Score 0–4: proceed to the next step.
- Could the patient have an atypical presentation of a time-sensitive disease?—Disease-specific scores.
- Use one of the accredited disease-specific scores depending on the clinical question;
- Prioritize the patient according to the score you have chosen;
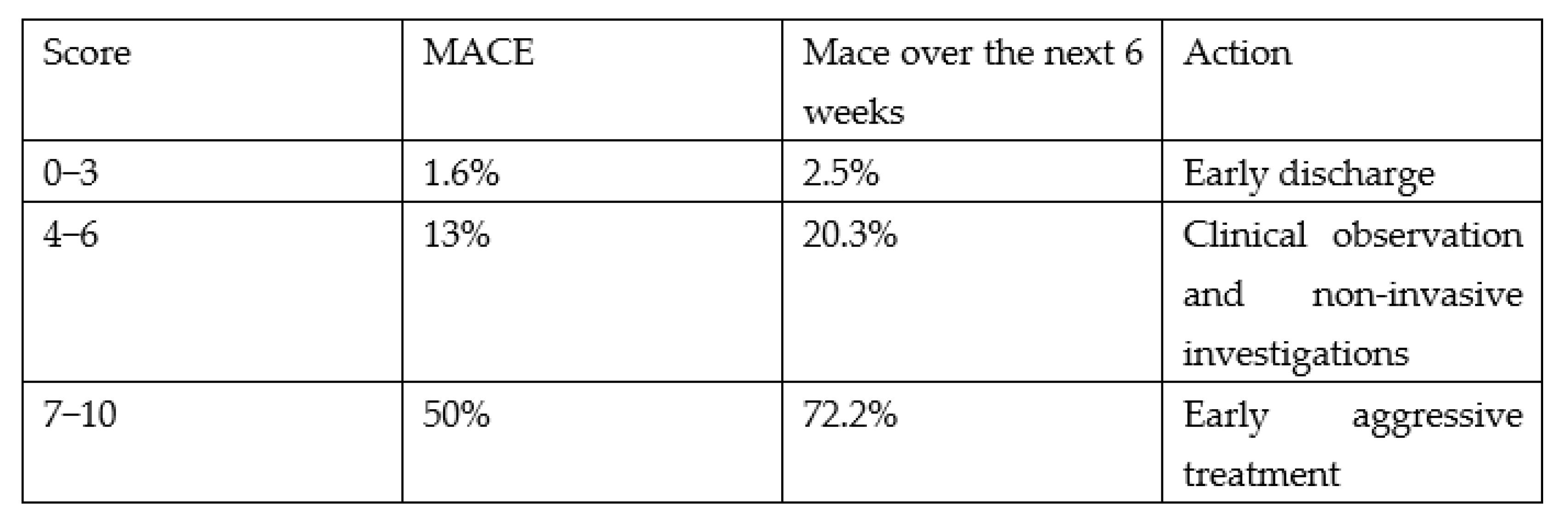
- Use the HEART score for a possible ACS;
- For a HEART score of 7–10, the patient is Priority 2;
- For a HEART score between 4 and 6, the patient is Priority 3;
- For a HEART score of 0–3, proceed to the next step;
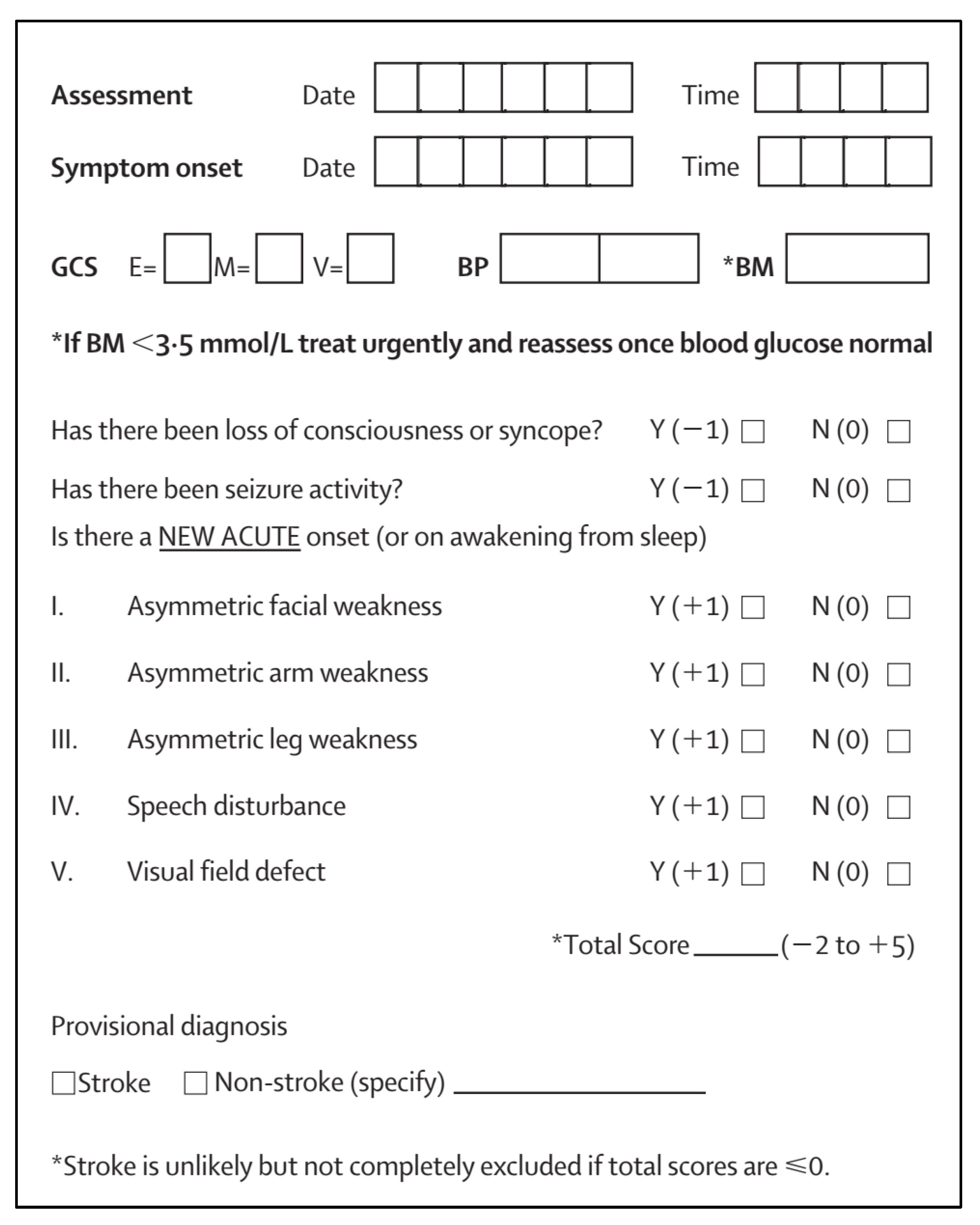
- Use the Rosier score for a possible stroke;
- For Rosier > 1, the patient is Priority 2;
- For Rosier ≤ 0, proceed to the next step.
- Will this patient require extensive work-up?—Focused history-taking.
- Use the basic principles of clinical impression triage systems such as ESI, and CTAS;
- “Will the patient, due to his age or comorbidities, require extensive work-up?”;
- If the answer is YES, the patient is Priority 4;
- If the answer is NO, the Patient is Priority 5.
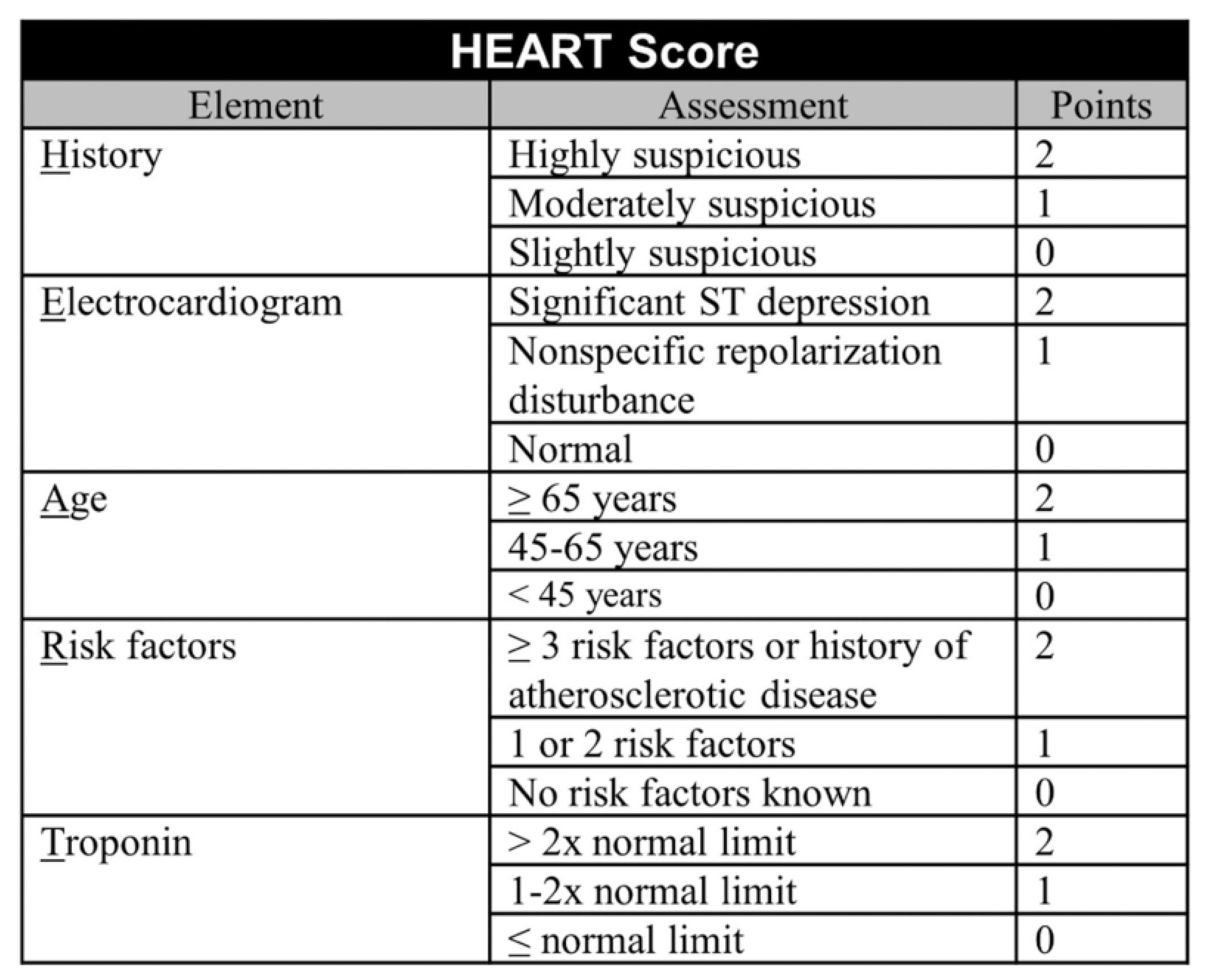
4. Results
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ingielewicz, A.; Rychlik, P.; Sieminski, M. Drinking from the Holy Grail- Does a Perfect Triage System Exist? And Where to Look for It? J. Pers. Med. 2024, 14, 590. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- FitzGerald, G.; Jelinek, G.A.; Scott, D.; Gerdtz, M.F. Emergency department triage revisited. Emerg. Med. J. 2010, 27, 86–92. [Google Scholar] [CrossRef]
- Alonso, P.S. Comparative analysis of global triage systems: Competencies of nursing and hospital and prehospital application. J. Nurs. Valencia. 2024, 1–31. [Google Scholar]
- Reason, J. Managing the Risks of Organizational Accidents, 1st ed.; Routledge: England, UK, 1997. [Google Scholar] [CrossRef]
- Tsiftsis, D.; El-Fellah, N.; Dermatis, P. Systems and algorithms of Hospital Triage and patient Acuity Assessment in the Emer-gency Department. In Intensive and Emergency Medicine: Scales, Algorithms, Protocols, Limits, Criteria and Indicators, 22nd ed.; Baltopoulos, G., Ed.; Chapter in Greek; Ekdosis Epistimon: Athens, Attica Greece, 2019; pp. 301–309. ISBN 978-618-83535-5-8. [Google Scholar]
- BenAveling—File: Swiss Cheese model.svg, CC BY-SA 4.0. Available online: https://commons.wikimedia.org/w/index.php?curid=133912327 (accessed on 3 March 2025).
- Gatsouli, M.; Gerakari, S.; Ivkovitz, Z.; Intas, G.; Kalogridaki, M.; Karametos, I.; Lymperopoulou, D.; Pantazopoulos, I.; Paylidou, E.; Stavroulakis, S.; et al. Proposal of the Hellenic Society for Emergency Medicine for the Pilot Implementation of a National Triage System in Sites Providing Emergency Care Services. (Article in Greek). Available online: https://www.hesem.gr/%cf%80%cf%81%cf%8c%cf%84%ce%b1%cf%83%ce%b7-%ce%b5%ce%bb%ce%bb%ce%b7%ce%bd%ce%b9%ce%ba%ce%ae%cf%82-%ce%b5%cf%84%ce%b1%ce%b9%cf%81%ce%b5%ce%af%ce%b1%cf%82-%ce%b5%cf%80%ce%b5%ce%af%ce%b3%ce%bf%cf%85/ (accessed on 2 March 2025).
- Kuriyama, A.; Urushidani, S.; Nakayama, T. Five-level emergency triage systems: Variation in assessment of validity. Emerg. Med. J. 2017, 34, 703–710. [Google Scholar] [CrossRef] [PubMed]
- Christ, M.; Grossmann, F.; Winter, D.; Bingisser, R.; Platz, E. Modern triage in the emergency department. Dtsch. Arztebl. Int. 2010, 107, 892–898. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tam, H.L.; Chung, S.F.; Lou, C.K. A review of triage accuracy and future direction. BMC Emerg. Med. 2018, 18, 58. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Storm-Versloot, M.N.; Ubbink, D.T.; Kappelhof, J.; Luitse, J.S. Comparison of an informally structured triage system, the emergency severity index, and the Manchester triage system to distinguish patient priority in the emergency department. Acad. Emerg. Med. 2011, 18, 822–829. [Google Scholar] [CrossRef] [PubMed]
- Mistry, B.; Stewart De Ramirez, S.; Kelen, G.; Schmitz, P.S.K.; Balhara, K.S.; Levin, S.; Martinez, D.; Psoter, K.; Anton, X.; Hinson, J.S. Accuracy and Reliability of Emergency Department Triage Using the Emergency Severity Index: An International Multicenter Assessment. Ann. Emerg. Med. 2018, 71, 581–587.e3. [Google Scholar] [CrossRef] [PubMed]
- Sax, D.R.; Warton, E.M.; Mark, D.G.; Vinson, D.R.; Kene, M.V.; Ballard, D.W.; Vitale, T.J.; McGaughey, K.R.; Beardsley, A.; Pines, J.M.; et al. Evaluation of the Emergency Severity Index in US Emergency Departments for the Rate of Mistriage. JAMA Netw. Open 2023, 6, e233404, Erratum in JAMA Netw. Open 2024, 7, e2423536. 10.1001/jamanetworkopen.2024.23536. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zachariasse, J.M.; van der Hagen, V.; Seiger, N.; Mackway-Jones, K.; van Veen, M.; Moll, H.A. Performance of triage systems in emergency care: A systematic review and meta-analysis. BMJ Open 2019, 9, e026471. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Suamchaiyaphum, K.; Jones, A.R.; Polancich, S. The accuracy of triage classification using Emergency Severity Index. Int. Emerg. Nurs. 2024, 77, 101537. [Google Scholar] [CrossRef] [PubMed]
- Peta, D.; Day, A.; Lugari, W.S.; Gorman, V.; Ahayalimudin, N.; Pajo, V.M.T. Triage: A Global Perspective. J. Emerg. Nurs. 2023, 49, 814–825. [Google Scholar] [CrossRef] [PubMed]
- El-Fellah, N.; Dritsa, A.; Dermatis, P.; Intas, G.; Papadopoulos, G.; Kaklamanou, E.; Tsiftsis, D. Knowledge of Health Care Professionals of the Emergency Department of the Hospital of N. Attica in the Emergency Severity Index Triage System. Hell. J. Nurs. 2017, 56, 358–365. (In Greek) [Google Scholar]
- Rashid, K.; Ullah, M.; Ahmed, S.T.; Sajid, M.Z.; Hayat, M.A.; Nawaz, B.; Abbas, K. Accuracy of Emergency Room Triage Using Emergency Severity Index (ESI): Independent Predictor of Under and Over Triage. Cureus 2021, 13, e20229. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Goldhill, D.R.; McNarry, A.F. Physiological abnormalities in early warning scores are related to mortality in adult inpatients. Br. J. Anaesth. 2004, 92, 882–884. [Google Scholar] [CrossRef] [PubMed]
- Ridley, S. The recognition and early management of critical illness. Ann. R. Coll. Surg. Engl. 2005, 87, 315–322. [Google Scholar] [CrossRef]
- Spencer, W.; Smith, J.; Date, P.; de Tonnerre, E.; Taylor, D.M. Determination of the best early warning scores to predict clinical outcomes of patients in the emergency department. Emerg. Med. J. 2019, 36, 716–721. [Google Scholar] [CrossRef] [PubMed]
- Kramer, A.A.; Sebat, F.; Lissauer, M. A review of early warning systems for prompt detection of patients at risk for clinical decline. J. Trauma. Acute Care Surg. 2019, 87 (Suppl. S1), S67–S73. [Google Scholar] [CrossRef] [PubMed]
- Downey, C.L.; Tahir, W.; Randell, R.; Brown, J.M.; Jayne, D.G. Strengths and limitations of early warning scores: A systematic review and narrative synthesis. Int. J. Nurs. Stud. 2017, 76, 106–119. [Google Scholar] [CrossRef] [PubMed]
- Schinkel, M.; Bergsma, L.; Veldhuis, L.I.; Ridderikhof, M.L.; Holleman, F. Comparing complaint-based triage scales and early warning scores for emergency department triage. Emerg. Med. J. 2022, 39, 691–696. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Williams, B. The National Early Warning Score: From concept to NHS implementation. Clin. Med. 2022, 22, 499–505. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Royal College of Physicians. National Early Warning Score (NEWS) 2: Standardising the Assessment of Acute-Illness Severity in the NHS. Updated Report of a Working Party; RCP: London, UK, 2017. [Google Scholar]
- Smith, G.B.; Prytherch, D.R.; Meredith, P.; Schmidt, P.E.; Featherstone, P.I. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation 2013, 84, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.A.; Karim, H.M.R.; Panda, C.K.; Ahmed, G.; Nayak, S. Atypical Presentations of Myocardial Infarction: A Systematic Review of Case Reports. Cureus 2023, 15, e35492. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vilela, P. Acute stroke differential diagnosis: Stroke mimics. Eur. J. Radiol. 2017, 96, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Pohl, M.; Hesszenberger, D.; Kapus, K.; Meszaros, J.; Feher, A.; Varadi, I.; Pusch, G.; Fejes, E.; Tibold, A.; Feher, G. Ischemic stroke mimics: A comprehensive review. J. Clin. Neurosci. 2021, 93, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Nishi, F.A.; de Oliveira Motta Maia, F.; de Souza Santos, I.; de Almeida Lopes Monteiro da Cruz, D. Assessing sensitivity and specificity of the Manchester Triage System in the evaluation of acute coronary syndrome in adult patients in emergency care: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2017, 15, 1747–1761. [Google Scholar] [CrossRef] [PubMed]
- Ashburn, N.P.; O’Neill, J.C.; Stopyra, J.P.; Mahler, S.A. Scoring systems for the triage and assessment of short-term cardiovascular risk in patients with acute chest pain. Rev. Cardiovasc. Med. 2021, 22, 1393–1403. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ke, J.; Chen, Y.; Wang, X.; Wu, Z.; Chen, F. Indirect comparison of TIMI, HEART, and GRACE for predicting major cardiovascular events in patients admitted to the emergency department with acute chest pain: A systematic review and meta-analysis. BMJ Open 2021, 11, e048356. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aung, S.S.M.; Roongsritong, C. A Closer Look at the HEART Score. Cardiol. Res. 2022, 13, 255–263. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhelev, Z.; Walker, G.; Henschke, N.; Fridhandler, J.; Yip, S. Prehospital stroke scales as screening tools for early identification of stroke and transient ischemic attack. Cochrane Database Syst. Rev. 2019, 4, CD011427. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chehregani Rad, I.; Azimi, A. Recognition of Stroke in the Emergency Room (ROSIER) Scale in Identifying Strokes and Transient Ischemic Attacks (TIAs); a Systematic Review and Meta-Analysis. Arch. Acad. Emerg. Med. 2023, 11, e67. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nor, A.M.; Davis, J.; Sen, B.; Shipsey, D.; Louw, S.J.; Dyker, A.G.; Davis, M.; Ford, G.A. The Recognition of Stroke in the Emergency Room (ROSIER) scale: Development and validation of a stroke recognition instrument. Lancet Neurol. 2005, 4, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Tyler, S.; Olis, M.; Aust, N.; Patel, L.; Simon, L.; Triantafyllidis, C.; Patel, V.; Lee, D.W.; Ginsberg, B.; Ahmad, H.; et al. Use of Artificial Intelligence in Triage in Hospital Emergency Departments: A Scoping Review. Cureus 2024, 16, e59906. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Piliuk, K.; Tomforde, S. Artificial intelligence in emergency medicine. A systematic literature review. Int. J. Med. Inform. 2023, 180, 105274. [Google Scholar] [CrossRef] [PubMed]
| Parameter | ATS | MTS | CTAS | ESI |
|---|---|---|---|---|
| Time to initial assessment | 10 min | ns | ns | ns |
| Time to contact with doctor with the right to treat | Immediate/10/60/120 min | Immediate/10/60/120/240 min | Immediate/15/30/60/120 min | Immediate/10 min/n. s |
| Re-triage | ns | As required | I:continuously; II: 15 min; III: 30 min; IV: 60 min; V: 120 min | As required |
| List of diagnoses or key symptoms | YES | 52 key symptoms | YES | No |
| Training material | YES | YES | YES | YES |
| Patient Priority | Clinical Condition | Tools Used to Identify |
|---|---|---|
| Priority 1 | Immediate risk for life or limb | ESI |
| Priority 2 | Serious enough or deteriorating so rapidly | ESI and/or Red Flags and/or NEWS 2 > 7 and/or HEART score >7 and/or Rosier > 1 |
| Priority 3 | Not serious enough, but could have atypical or early presentation of a serious condition | NEWS 2 = 5–6 and/or HEART score = 4–6 |
| Priority 4 | No serious underlying condition, but will require extensive work-up | ESI and NEWS 2 = 0–4 and HEART = 0–3 and Rosier ≤ 0 |
| Priority 5 | Acute but non-urgent or chronic problem without deterioration. Needs minimum investigation | ESI and NEWS 2 = 0–4 and HEART = 0–3 and Rosier < 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsiftsis, D.; Tasioulis, A.; Bampalis, D. Adult Triage in the Emergency Department: Introducing a Multi-Layer Triage System. Healthcare 2025, 13, 1070. https://doi.org/10.3390/healthcare13091070
Tsiftsis D, Tasioulis A, Bampalis D. Adult Triage in the Emergency Department: Introducing a Multi-Layer Triage System. Healthcare. 2025; 13(9):1070. https://doi.org/10.3390/healthcare13091070
Chicago/Turabian StyleTsiftsis, Dimitrios, Andreas Tasioulis, and Dimitrios Bampalis. 2025. "Adult Triage in the Emergency Department: Introducing a Multi-Layer Triage System" Healthcare 13, no. 9: 1070. https://doi.org/10.3390/healthcare13091070
APA StyleTsiftsis, D., Tasioulis, A., & Bampalis, D. (2025). Adult Triage in the Emergency Department: Introducing a Multi-Layer Triage System. Healthcare, 13(9), 1070. https://doi.org/10.3390/healthcare13091070







