Comparative Outcomes of Bilateral Versus Unilateral Total Knee Arthroplasty: A Big Data Analysis
Abstract
1. Introduction
Research Question
2. Methods
2.1. Dataset Acquisition and Inclusion Criteria
2.2. Study Period and Data Source
2.3. Patient Identification and Exclusions
2.4. Statistical Analyses
2.5. Outcome Measures and Procedure Identification
2.6. Ethical Considerations
3. Results
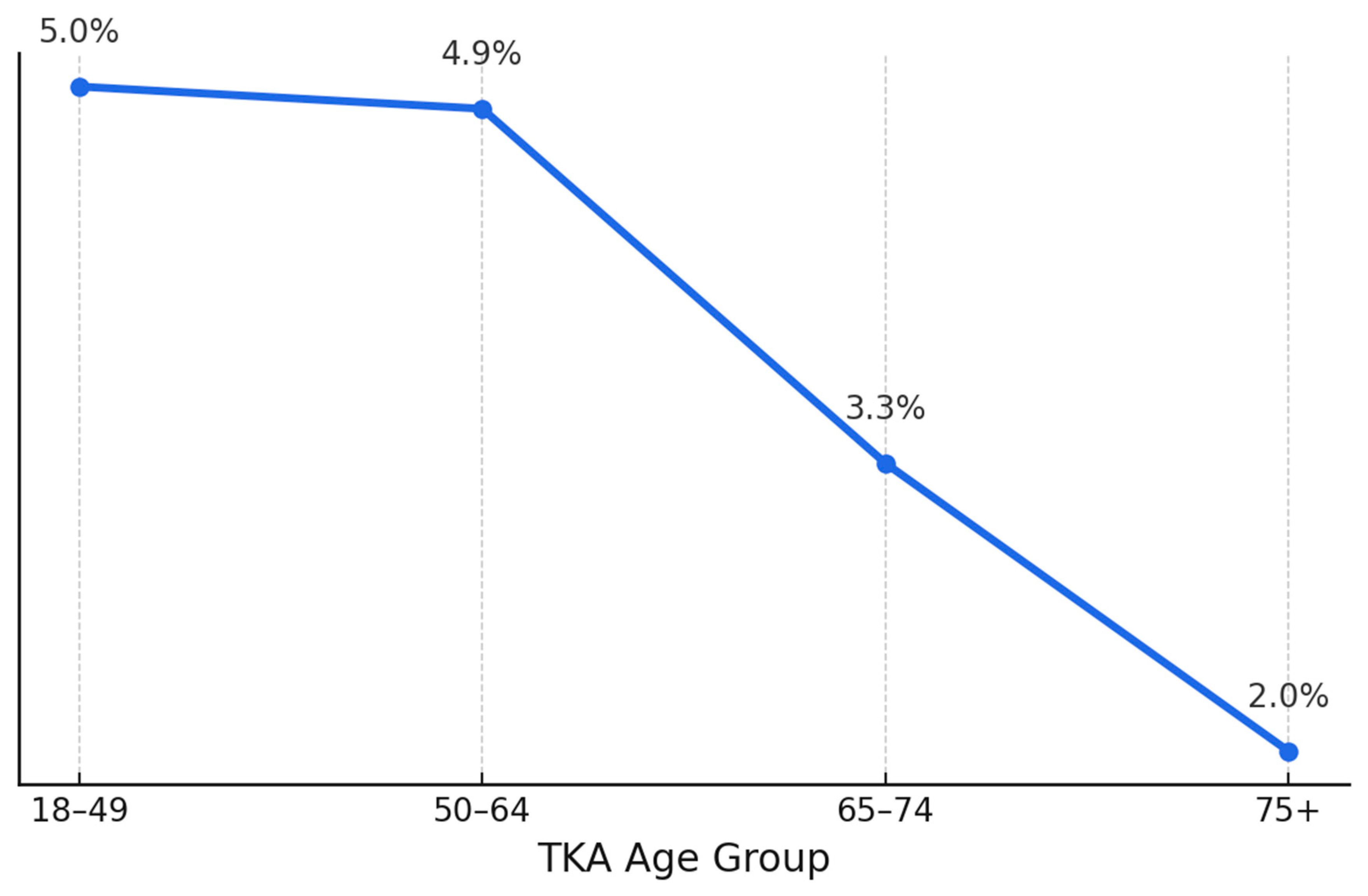
3.1. Demographic and Hospital Characteristics of Patients Undergoing Bilateral vs. Unilateral Total Knee Arthroplasty
3.2. Body Mass Index (BMI) Comparison Between Unilateral and Bilateral Total Knee Arthroplasty Patients
3.3. Comparison of Comorbidities Between Unilateral and Bilateral Total Knee Arthroplasty Patients
3.4. Propensity Score-Matched Analysis to Balance Baseline Characteristics
3.5. Comparison of Hospitalization Outcomes in Propensity Score-Matched Cohorts
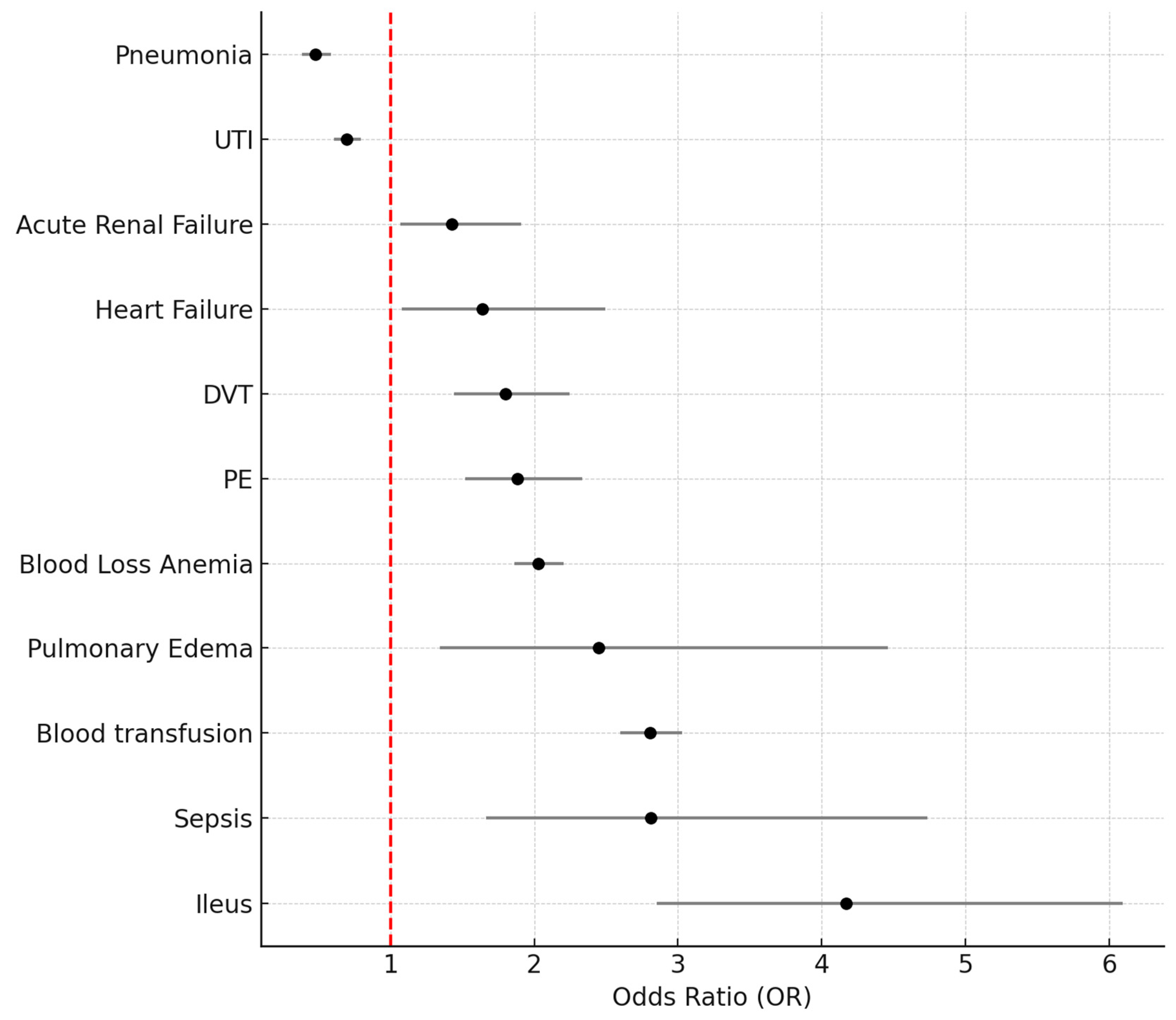
3.6. Odds Ratios of Postoperative Complications in Bilateral TKA Versus Unilateral TKA in a Propensity Score-Matched Cohort
- Acute renal failure (OR 1.429, 95% CI: 1.070–1.907, p = 0.015);
- Heart failure (OR 1.640, 95% CI: 1.078–2.494, p = 0.021);
- Deep vein thrombosis (DVT) (OR 1.798, 95% CI: 1.441–2.244, p < 0.001);
- Pulmonary embolism (PE) (OR 1.883, 95% CI: 1.519–2.335, p < 0.001);
- Blood loss anemia (OR 2.026, 95% CI: 1.862–2.204, p < 0.001);
- Pulmonary edema (OR 2.451, 95% CI: 1.346–4.462, p = 0.003);
- Blood transfusion (OR 2.806, 95% CI: 2.600–3.029, p < 0.001);
- Sepsis (OR 2.809, 95% CI: 1.666–4.737, p < 0.001);
- Ileus, which had the highest relative risk (OR 4.171, 95% CI: 2.855–6.094, p < 0.001).
4. Discussion
4.1. Main Findings
4.2. Patient Selection and Health Equity Considerations
4.3. Perioperative Risk and Complication Profiles
4.4. Economic Implications and Hospital Resource Utilization
4.5. Decision-Making and Clinical Relevance
4.6. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ASA | American Society of Anesthesiologists |
| B-TKA | Bilateral total knee arthroplasty |
| BMI | Body mass index |
| CCI | Charlson Comorbidity Index |
| CI | Confidence interval |
| CKD | Chronic kidney disease |
| DVT | Deep vein thrombosis |
| HCUP | Healthcare Cost and Utilization Project |
| ICD-10 | International Classification of Diseases, 10th Revision |
| LOS | Length of stay |
| NIS | Nationwide Inpatient Sample |
| NSQIP | National Surgical Quality Improvement Program |
| OR | Odds ratio |
| PE | Pulmonary embolism |
| SPSS | Statistical Package for the Social Sciences |
| TKA | Total knee arthroplasty |
| U-TKA | Unilateral total knee arthroplasty |
| UTI | Urinary tract infection |
References
- Spicer, E.; Thomas, G.R.; Rumble, E.J. Comparison of the major intraoperative and postoperative complications between unilateral and sequential bilateral total knee arthroplasty in a high-volume community hospital. Can. J. Surg. 2013, 56, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Putnis, S.E.; Klasan, A.; Redgment, J.D.; Smith, T.O. One-stage sequential bilateral total knee arthroplasty: An effective treatment for advanced bilateral knee osteoarthritis providing high patient satisfaction. J. Arthroplast. 2020, 35, 401–406. [Google Scholar] [CrossRef]
- Bohm, E.R.; Molodianovitsh, K.; Dragan, A.; Zhu, N.; Webster, G.; Masri, B.; Schemitsch, E.; Dunbar, M. Outcomes of unilateral and bilateral total knee arthroplasty in 238,373 patients. Acta Orthop. 2016, 87 (Suppl. 1), 24–30. [Google Scholar] [CrossRef] [PubMed]
- Wilkie, W.A.; Mohamed, N.S.; Remily, E.A.; Etcheson, J.I.; Castrodad, I.M.D.; Walker, A.J.; Delanois, R.E. Complications associated with same-day bilateral total knee arthroplasties. Orthopedics 2021, 44, e407–e413. [Google Scholar] [CrossRef]
- Mehta, B.; Ho, K.; Bido, J.; Hernandez, V.H. Bilateral vs unilateral total knee arthroplasty: Racial variation in utilization and in-hospital major complication rates. J. Arthroplast. 2021, 36, 1310–1317. [Google Scholar] [CrossRef]
- Hashimoto, S.; Terauchi, M.; Hatayama, K.; Saito, K.; Chikuda, H. Younger patients with high varus malalignment of the contralateral knee may be candidates for simultaneous bilateral total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2173–2180. [Google Scholar] [CrossRef]
- Yakkanti, R.R.; Ovadia, J.E.; Reddy, G.B.; Browne, J.A.; D’Apuzzo, M.R. In-hospital complications and costs of simultaneous bilateral total knee arthroplasty: The case for selection and potential cost savings. J. Arthroplast. 2022, 37, 1273–1277. [Google Scholar] [CrossRef]
- Richardson, M.K.; Liu, K.C.; Mayfield, C.K.; Kistler, N.M.; Christ, A.B.; Heckmann, N.D. Complications and safety of simultaneous bilateral total knee arthroplasty: A patient characteristic and comorbidity-matched analysis. J. Bone Jt. Surg. Am. 2023, 105, 1072–1079. [Google Scholar] [CrossRef]
- Hart, A.; Antoniou, J.; Brin, Y.S.; Huk, O.L.; Zukor, D.J.; Bergeron, S.G. Simultaneous bilateral versus unilateral total knee arthroplasty: A comparison of 30-day readmission rates and major complications. J. Arthroplast. 2016, 31, 31–35. [Google Scholar] [CrossRef]
- Warren, J.A.; Siddiqi, A.; Krebs, V.E.; Molloy, R.; Higuera, C.A.; Piuzzi, N.S. Bilateral simultaneous total knee arthroplasty may not be safe even in the healthiest patients. J. Bone Jt. Surg. Am. 2021, 103, 303–311. [Google Scholar] [CrossRef]
- Odum, S.M.; Springer, B.D. In-hospital complication rates and associated factors after simultaneous bilateral versus unilateral total knee arthroplasty. J. Bone Jt. Surg. Am. 2014, 96, 1058–1065. [Google Scholar] [CrossRef] [PubMed]
- Davidson, I.U.; Brigati, D.P.; Faour, M.; UdoInyang, I.J.; Ibrahim, M.; Murray, T.G. Same-day bilateral total knee arthroplasty candidacy criteria decrease length of stay and facility discharge. Orthopedics 2018, 41, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Odum, S.M.; Troyer, J.L.; Kelly, M.P.; Dedini, R.D.; Bozic, K.J. A cost-utility analysis comparing the cost-effectiveness of simultaneous and staged bilateral total knee arthroplasty. J. Bone Jt. Surg. Am. 2013, 95, 1441–1449. [Google Scholar] [CrossRef] [PubMed]
- Wunderlich, F.; Schröder, M.; Appelmann, P.; Piontek, T.; Strube, P.; Friederich, H.C. Simultaneous bilateral TKA in the context of fast-track surgery—Do patients meet discharge criteria as anticipated? J. Orthop. Sci. 2024, 29, 861–866. [Google Scholar] [CrossRef]
- Tsui, O.W.K.; Chan, P.-K.; Cheung, A.; Chan, V.W.K.; Luk, M.H.; Cheung, M.-H.; Lau, L.C.; Leung, T.K.; Fu, H.; Chiu, K.-Y. Comparison of the cost-effectiveness and safety between staged bilateral total knee arthroplasty and simultaneous bilateral total knee arthroplasty: A retrospective cohort study between 2001 and 2022. J. Knee Surg. 2024, 37, 916–923. [Google Scholar] [CrossRef]
- Remily, E.A.; Wilkie, W.A.; Mohamed, N.S.; Johnson, A.S. Same-day bilateral total knee arthroplasty: Incidence and perioperative outcome trends from 2009 to 2016. Knee 2020, 27, 1963–1970. [Google Scholar] [CrossRef]
- Chen, A.T.; Bronsther, C.I.; Stanley, E.E.; Paltiel, A.D.; Sullivan, J.K.; Collins, J.E.; Neogi, T.; Katz, J.N.; Losina, E. The value of total knee replacement in patients with knee osteoarthritis and a body mass index of 40 kg/m2 or greater: A cost-effectiveness analysis. Ann. Intern. Med. 2021, 174, 747–757. [Google Scholar] [CrossRef]
- Jette, D.U.; Hunter, S.J.; Burkett, L.; Kielhofner, G.; Reilly, K.; Nelson, A. Physical therapist management of total knee arthroplasty. Phys. Ther. 2020, 100, 1603–1631. [Google Scholar] [CrossRef]
- Matsumura, Y.; Fujii, M.; Yamaguchi, Y.; Nagamine, S.; Sakai, T.; Ide, S.; Tajima, T.; Shimazaki, T.; Eto, S.; Mawatari, M. Complications following bilateral simultaneous versus staged total knee arthroplasty in the Japanese population: A propensity-matched case-control study. Sci. Rep. 2024, 14, 29987. [Google Scholar] [CrossRef]
- Hummel, A.; Matsumoto, M.; Shimoda, B.; Au, D.L.M.T.; Andrews, S.N.; Nakasone, C.K. Complications following single-stage bilateral total knee arthroplasty and unilateral procedures: Experience of a high-volume community hospital. Arch. Orthop. Trauma. Surg. 2024, 144, 315–322. [Google Scholar] [CrossRef]
- Franceschetti, E.; Campi, S.; Gregori, P.; Pace, F.; Mancuso, A.; Capuano, N. No differences in terms of complications, readmissions, reoperations, and patient-reported outcomes in simultaneous bilateral versus staged bilateral total knee arthroplasty in selected patients. Knee 2024, 47, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Ashkenazi, I.; Rajahraman, V.; Lawrence, K.W.; D’Souza, S.; Frankel, S.; Simhon, D. The financial feasibility of bilateral total knee arthroplasty: A matched cohort analysis of revenue and contribution margin between simultaneous and staged procedures. J. Arthroplast. 2024, 39, 1645–1649. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.Y.; Puvanesarajah, V.; Raad, M.; Barry, K.; Srikumaran, U.; Thakkar, S.C. The BTK safety score: A novel scoring system for risk stratifying patients undergoing simultaneous bilateral total knee arthroplasty. J. Knee Surg. 2023, 36, 702–709. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Unilateral TKA | Bilateral TKA | Significance |
|---|---|---|---|
| Total surgeries (%) | 2,215,999 | 83,980 | |
| Average age (y) | 66.1 | 67.1 | p < 0.001 |
| Female (%) | 62.0% | 54.0% | p < 0.001 |
| Primary expected payer—Medicare (%) | 57.7% | 43.0% | p < 0.001 |
| Payer—Medicaid (%) | 4.3% | 3.7% | |
| Payer—private (%) | 34.4% | 50.3% | |
| Payer—self-pay (%) | 0.5% | 0.7% | |
| Primary—no charge (%) | 0.0% | 0.0% | |
| Primary—other (%) | 3.1% | 2.3% | |
| Location/teaching status—rural (%) | 10.4% | 9.7% | p < 0.001 |
| Location/teaching status—urban nonteaching (%) | 27.4% | 22.8% | |
| Location/teaching status—urban teaching (%) | 62.2% | 67.4% |
| Unilateral TKA | Bilateral TKA | Significance | |
|---|---|---|---|
| Mean BMI | 36.7 | 35.9 | p = 0.41 |
| Std. Deviation | 4.5 | 4.5 |
| Parameter | Unilateral TKA | Bilateral TKA | Significance |
|---|---|---|---|
| Hypertension (%) | 59.7% | 55.5% | p < 0.001 |
| Dyslipidemia (%) | 46.9% | 40.8% | p < 0.001 |
| Obstructive Sleep Apnea (%) | 13.2% | 12.8% | p = 0.01 |
| Chronic Anemia (%) | 5.7% | 6.5% | p < 0.001 |
| Alcohol Abuse (%) | 0.9% | 1.1% | p < 0.001 |
| Osteoporosis (%) | 4.0% | 2.7% | p < 0.001 |
| Parkinson Disease (%) | 0.6% | 0.3% | p < 0.001 |
| Alzheimer Disease (%) | 0.2% | 0.1% | p < 0.001 |
| Chronic Kidney Disease (%) | 7.0% | 4.8% | p < 0.001 |
| Congestive Heart Failure (%) | 1.2% | 0.7% | p < 0.001 |
| Chronic Lung Disease (%) | 6.1% | 3.8% | p < 0.001 |
| Diabetes Mellitus (%) | 22.0% | 15.9% | p < 0.001 |
| IBD (%) | 0.5% | 0.5% | p = 0.357 |
| Liver Disease (%) | 1.3% | 1.3% | p = 0.819 |
| Obesity (%) | 31.1% | 30.7% | p = 0.040 |
| Fibromyalgia (%) | 2.8% | 2.2% | p < 0.001 |
| Disorders of Thyroid (%) | 18.0% | 15.4% | p < 0.001 |
| History of Myocardial Infarction (%) | 3.2% | 2.0% | p < 0.001 |
| Peripheral Vascular Disease (%) | 1.5% | 1.0% | p < 0.001 |
| History of Cerebrovascular Accident (%) | 4.1% | 2.3% | p < 0.001 |
| Dementia (%) | 0.5% | 0.3% | p < 0.001 |
| Neoplasms (%) | 0.9% | 1.0% | p = 0.479 |
| Neoplasms of Lymphoid and Hematopoietic Tissue (%) | 0.4% | 0.4% | p = 0.634 |
| Parameter | Unilateral TKA | Bilateral TKA | Significance |
|---|---|---|---|
| Total surgeries (number) | 83,980 | 83,980 | |
| Average age (years) | 63.9 | 63.9 | p = 0.90 |
| Female (%) | 54.2 | 54.0 | p = 0.59 |
| Payer—Medicare (%) | 43.0 | 43.0 | p = 0.10 |
| Payer—Medicaid (%) | 3.7 | 3.7 | |
| Payer—private (%) | 50.3 | 50.3 | |
| Payer—other (including self-pay) (%) | 2.3 | 2.3 | |
| Location/teaching status—rural (%) | 10.0 | 9.7 | p = 0.61 |
| Location/teaching status—urban nonteaching (%) | 22.7 | 22.9 | |
| Location/teaching status—urban teaching (%) | 67.3 | 67.4 | |
| Hypertension diagnosis (%) | 55.5 | 55.5 | p = 0.94 |
| Dyslipidemia diagnosis (%) | 40.8 | 40.8 | p = 0.85 |
| Sleep apnea diagnosis (%) | 12.7 | 12.8 | p = 0.59 |
| Chronic anemia (%) | 6.3 | 6.5 | p = 0.08 |
| Alcohol abuse (%) | 1.1 | 1.1 | p = 0.82 |
| Osteoporosis (%) | 2.6 | 2.7 | p = 0.60 |
| Parkinson disease (%) | 0.2 | 0.3 | p = 0.09 |
| Type 2 diabetes (%) | 15.8 | 15.9 | p = 0.87 |
| Renal disease (%) | 4.7 | 4.8 | p = 0.10 |
| Chronic heart failure (%) | 0.7 | 0.7 | p = 0.46 |
| Chronic lung disease (%) | 3.7 | 3.8 | p = 0.52 |
| Obesity (%) | 30.7 | 30.7 | p = 0.11 |
| Fibromyalgia (%) | 2.3 | 2.2 | p = 0.08 |
| Thyroid disorders (%) | 15.3 | 15.4 | p = 0.09 |
| History of MI (%) | 2.1 | 2.0 | p = 0.07 |
| Peripheral vascular disease (%) | 1.2 | 1.0 | p = 0.07 |
| History of CVA (%) | 2.3 | 2.3 | p = 0.08 |
| Dementia (%) | 0.3 | 0.3 | p = 0.09 |
| Peptic ulcer disease (%) | 0.3 | 0.4 | p = 0.08 |
| Neoplasms (%) | 1.0 | 1.0 | p = 0.07 |
| Neoplasms (lymphoid/hematopoietic) (%) | 0.4 | 0.4 | p = 0.08 |
| Unilateral TKA | Bilateral TKA | Significance | |
|---|---|---|---|
| Died during hospitalization | 0.00% | 0.02% | p < 0.001 |
| Length of stay mean in days | 2.49 (Std. deviation 1.3) | 3.03 (Std. deviation 2.8) | p < 0.001 |
| Total charges mean in USD | 59,215 (Std. deviation 33,120) | 83,639 (Std. deviation 52,551) | p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maman, D.; Dumov, D.; Nandakumar, M.; Litmanowicz, B.; Shpigelman, D.; Fournier, L.; Steinfeld, Y.; Yonai, Y.; Berkovich, Y. Comparative Outcomes of Bilateral Versus Unilateral Total Knee Arthroplasty: A Big Data Analysis. Healthcare 2025, 13, 1033. https://doi.org/10.3390/healthcare13091033
Maman D, Dumov D, Nandakumar M, Litmanowicz B, Shpigelman D, Fournier L, Steinfeld Y, Yonai Y, Berkovich Y. Comparative Outcomes of Bilateral Versus Unilateral Total Knee Arthroplasty: A Big Data Analysis. Healthcare. 2025; 13(9):1033. https://doi.org/10.3390/healthcare13091033
Chicago/Turabian StyleMaman, David, Daniel Dumov, Maneesh Nandakumar, Batia Litmanowicz, Daniel Shpigelman, Linor Fournier, Yaniv Steinfeld, Yaniv Yonai, and Yaron Berkovich. 2025. "Comparative Outcomes of Bilateral Versus Unilateral Total Knee Arthroplasty: A Big Data Analysis" Healthcare 13, no. 9: 1033. https://doi.org/10.3390/healthcare13091033
APA StyleMaman, D., Dumov, D., Nandakumar, M., Litmanowicz, B., Shpigelman, D., Fournier, L., Steinfeld, Y., Yonai, Y., & Berkovich, Y. (2025). Comparative Outcomes of Bilateral Versus Unilateral Total Knee Arthroplasty: A Big Data Analysis. Healthcare, 13(9), 1033. https://doi.org/10.3390/healthcare13091033






