Malnutrition in Substance Use Disorders: A Critical Issue in Their Treatment and Recovery
Abstract
1. Introduction
2. Materials and Methods
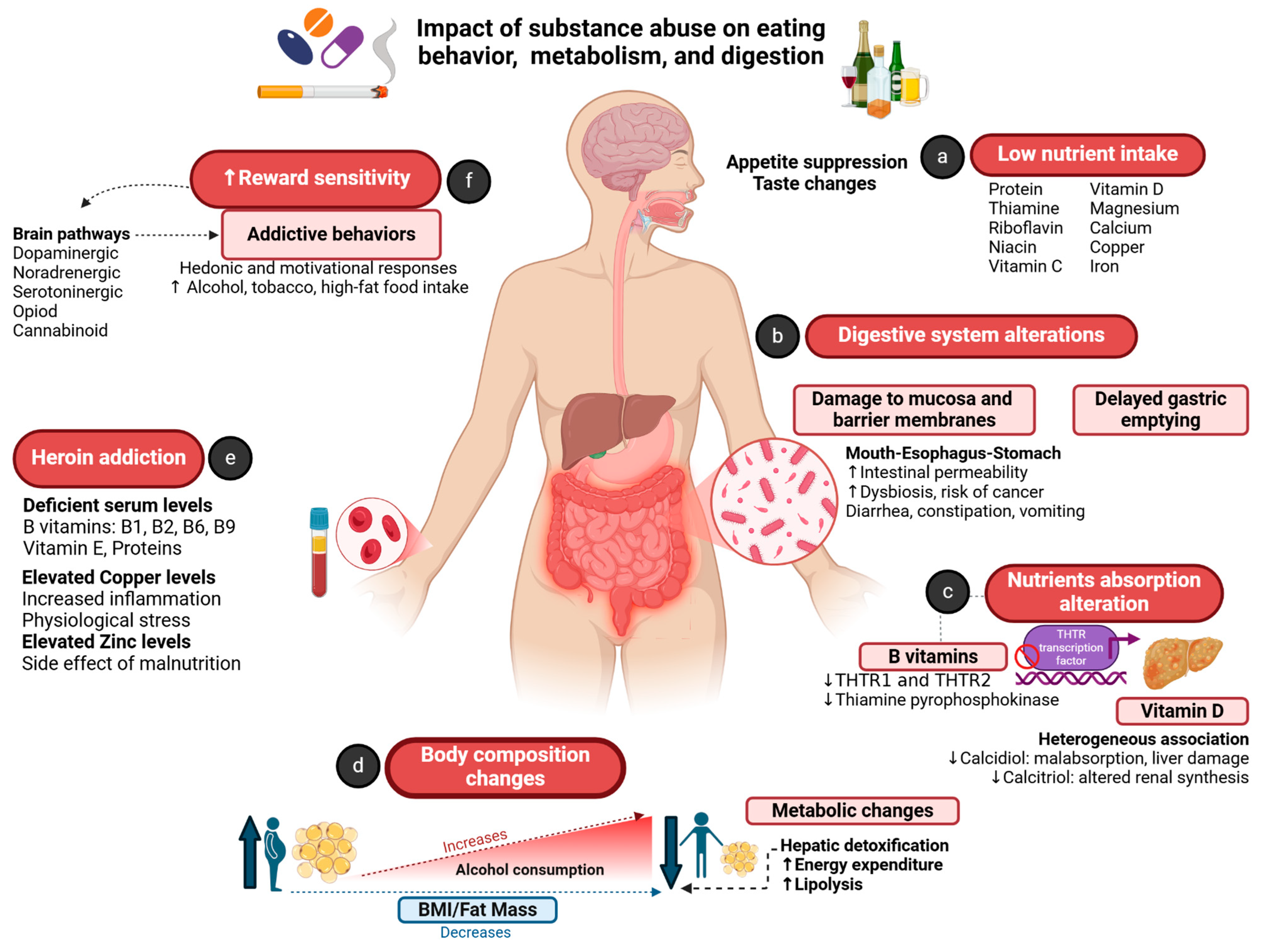
3. Malnutrition in the Context of SUDs
Pathophysiology of Malnutrition in People with SUD
4. Eating Behavior: Overlap of Food Addiction and SUDs
Hunger and Craving Related to SUDs
5. Nutritional Approaches to the Treatment and Recovery of SUDs
5.1. Alcohol and Alcoholism as a Trigger for Malnutrition
5.2. Cocaine
5.3. Opioids
5.4. Methamphetamines
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Volkow, N.D.; Blanco, C. Substance use disorders: A comprehensive update of classification, epidemiology, neurobiology, clinical aspects, treatment and prevention. World Psychiatry 2023, 22, 203–229. [Google Scholar] [CrossRef] [PubMed]
- Ross, L.J.; Wilson, M.; Banks, M.; Rezannah, F.; Daglish, M. Prevalence of malnutrition and nutritional risk factors in patients undergoing alcohol and drug treatment. Nutrition 2012, 28, 738–743. [Google Scholar] [CrossRef]
- Santolaria, F.; Pérez-Manzano, J.L.; Milena, A.; González-Reimers, E.; Gómez-Rodríguez, M.A.; Martínez-Riera, A.; Alemán-Valls, M.R.; de la Vega-Prieto, M.J. Nutritional assessment in alcoholic patients. Its relationship with alcoholic intake, feeding habits, organic complications and social problems. Drug Alcohol Depend. 2000, 59, 295–304. [Google Scholar] [CrossRef]
- Kobylińska, M.; Antosik, K.; Decyk, A.; Kurowska, K. Malnutrition in Obesity: Is It Possible? Obes. Facts 2022, 15, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Virmani, A.; Binienda, Z.; Ali, S.; Gaetani, F. Links between Nutrition, Drug Abuse, and the Metabolic Syndrome. Ann. N. Y. Acad. Sci. 2006, 1074, 303–314. [Google Scholar] [CrossRef]
- Nagarajan, M.K.; Goodman, D. Not just substance use: The critical gap in nutritional interventions for pregnant women with opioid use disorders. Public Health 2020, 180, 114–116. [Google Scholar] [CrossRef]
- Ströhle, A.; Wolters, M.; Hahn, A. Alcohol intake—A two-edged sword. Part 1: Metabolism and pathogenic effects of alcohol. Med. Monatsschrift Pharm. 2012, 35, 281–292, quiz 293–294. [Google Scholar]
- Smith, L.O.; Vest, M.T.; Rovner, A.J.; Shapero, M.; Suminski, R.R.; Trabulsi, J.C.; Earthman, C.P. Prevalence and characteristics of starvation-related malnutrition in a mid-Atlantic healthcare system: A cohort study. J. Parenter. Enter. Nutr. 2022, 46, 357–366. [Google Scholar] [CrossRef]
- Coelho, M.P.P.; Diniz, K.G.D.; Bering, T.; Ferreira, L.D.S.A.; Vieira, D.A.; Castro, M.R.C.; Correia, M.I.T.D.; Rocha, G.A.; Teixeira, R.; Garcia, F.D.; et al. Skeletal muscle mass index and phase angle are decreased in individuals with dependence on alcohol and other substances. Nutrition 2020, 71, 110614. [Google Scholar] [CrossRef]
- Lee, J.; Kim, S.; Lee, Y.; Kwon, Y.J.; Lee, J.W. Higher Adherence to the Mediterranean Diet Is Associated with a Lower Risk of Steatotic, Alcohol-Related, and Metabolic Dysfunction-Associated Steatotic Liver Disease: A Retrospective Analysis. Nutrients 2024, 16, 3551. [Google Scholar] [CrossRef]
- Ghaderi, A.; Banafshe, H.R.; Motmaen, M.; Rasouli-Azad, M.; Bahmani, F.; Asemi, Z. Clinical trial of the effects of vitamin D supplementation on psychological symptoms and metabolic profiles in maintenance methadone treatment patients. Prog. Neuropsychopharmacol. Biol. Psychiatry 2017, 79, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Imam, S.Z.; Ali, S.F. Selenium, an antioxidant, attenuates methamphetamine-induced dopaminergic toxicity and peroxynitrite generation. Brain Res. 2000, 855, 186–191. [Google Scholar] [CrossRef]
- Loebens, M.; Barros, H.M.T. Diet influences cocaine withdrawal behaviors in the forced swimming test. Pharmacol. Biochem. Behav. 2003, 74, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Nazrul Islam, S.K.; Hossain, K.J.; Ahmed, A.; Ahsan, M. Nutritional status of drug addicts undergoing detoxification: Prevalence of malnutrition and influence of illicit drugs and lifestyle. Br. J. Nutr. 2002, 88, 507–513. [Google Scholar] [CrossRef]
- Sæland, M.; Haugen, M.; Eriksen, F.-L.; Wandel, M.; Smehaugen, A.; Böhmer, T.; Oshaug, A. High sugar consumption and poor nutrient intake among drug addicts in Oslo, Norway. Br. J. Nutr. 2011, 105, 618–624. [Google Scholar] [CrossRef]
- Yazici, A.B.; Akcay Ciner, O.; Yazici, E.; Cilli, A.S.; Dogan, B.; Erol, A. Comparison of vitamin B12, vitamin D and folic acid blood levels in patients with schizophrenia, drug addiction and controls. J. Clin. Neurosci. 2019, 65, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Bemanian, M.; Chowdhury, R.; Stokke, K.; Aas, C.F.; Johansson, K.A.; Vold, J.H.; Fadnes, L.T. Vitamin D status and associations with substance use patterns among people with severe substance use disorders in Western Norway. Sci. Rep. 2022, 12, 13695. [Google Scholar] [CrossRef]
- Madebo, T.; Bemanian, M.; Vold, J.H.; Chowdhury, R.; Aas, C.F.; Druckrey-Fiskaaen, K.T.; Johansson, K.A.; Fadnes, L.T. Vitamin B12 Levels, Substance Use Patterns and Clinical Characteristics among People with Severe Substance Use Disorders: A Cohort Study from Western Norway. Nutrients 2022, 14, 1941. [Google Scholar] [CrossRef]
- Bemanian, M.; Vold, J.H.; Chowdhury, R.; Aas, C.F.; Gjestad, R.; Johansson, K.A.; Fadnes, L.T. Folate Status as a Nutritional Indicator among People with Substance Use Disorder; A Prospective Cohort Study in Norway. Int. J. Environ. Res. Public Health 2022, 19, 5754. [Google Scholar] [CrossRef]
- Mahboub, N.; Rizk, R.; Karavetian, M.; De Vries, N. Nutritional status and eating habits of people who use drugs and/or are undergoing treatment for recovery: A narrative review. Nutr. Rev. 2021, 79, 627–635. [Google Scholar] [CrossRef]
- Nabipour, S.; Ayu Said, M.; Hussain Habil, M. Burden and nutritional deficiencies in opiate addiction—Systematic review article. Iran. J. Public Health 2014, 43, 1022–1032. [Google Scholar]
- Carmela, D. Substance Use Disorder Treatment and Nutrition: A Multidisciplinary Approach. J. Ment. Health Soc. Behav. 2020, 2, 2. [Google Scholar]
- Urhan, M.; Gezmen Karadağ, M. Diet quality, nutritional status and taste recognition are impaired in men with substance use disorder. Nutr. Bull. 2024, 49, 40–51. [Google Scholar] [CrossRef]
- Badaoui, A.; De Saeger, C.; Duchemin, J.; Gihousse, D.; De Timary, P.; Stärkel, P. Alcohol dependence is associated with reduced plasma and fundic ghrelin levels. Eur. J. Clin. Investig. 2008, 38, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Preedy, V.R. Alcohol and the Gastrointestinal Tract; CRC Press: Boca Raton, FL, USA, 2017; 358p. [Google Scholar]
- Chopra, K.; Tiwari, V. Alcoholic neuropathy: Possible mechanisms and future treatment possibilities. Br. J. Clin. Pharmacol. 2012, 73, 348–362. [Google Scholar] [CrossRef] [PubMed]
- Jeynes, K.D.; Gibson, E.L. The importance of nutrition in aiding recovery from substance use disorders: A review. Drug Alcohol Depend. 2017, 179, 229–239. [Google Scholar] [CrossRef]
- Encuesta Nacional de Salud y Nutrición (ENSANUT) 2018. Presentación de Resultados. Available online: https://ensanut.insp.mx/encuestas/ensanut2018/doctos/informes/ensanut_2018_presentacion_resultados.pdf (accessed on 23 November 2024).
- Addolorato, G.; Capristo, E.; Marini, M.; Santini, P.; Scognamiglio, U.; Attilia, M.L.; Messineo, D.; Sasso, G.F.; Gasbarrini, G.; Ceccanti, M. Body composition changes induced by chronic ethanol abuse: Evaluation by dual energy x-ray absorptiometry. Am. J. Gastroenterol. 2000, 95, 2323–2327. [Google Scholar] [CrossRef]
- de Timary, P.; Cani, P.D.; Duchemin, J.; Neyrinck, A.M.; Gihousse, D.; Laterre, P.-F.; Badaoui, A.; Leclercq, S.; Delzenne, N.M.; Stärkel, P. The Loss of Metabolic Control on Alcohol Drinking in Heavy Drinking Alcohol-Dependent Subjects. PLoS ONE 2012, 7, e38682. [Google Scholar] [CrossRef]
- Liangpunsakul, S.; Crabb, D.W.; Qi, R. Relationship Among Alcohol Intake, Body Fat, and Physical Activity: A Population-Based Study. Ann. Epidemiol. 2010, 20, 670–675. [Google Scholar] [CrossRef]
- Volkow, N.D.; Wang, G.J.; Shokri Kojori, E.; Fowler, J.S.; Benveniste, H.; Tomasi, D. Alcohol decreases baseline brain glucose metabolism more in heavy drinkers than controls but has no effect on stimulation-induced metabolic increases. J. Neurosci. Off. J. Soc. Neurosci. 2015, 35, 3248–3255. [Google Scholar] [CrossRef]
- Levine, J.A.; Harris, M.M.; Morgan, M.Y. Energy expenditure in chronic alcohol abuse. Eur. J. Clin. Investig. 2000, 30, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Hossain, K.J.; Kamal, M.M.; Ahsan, M.; Islam, S.N. Serum antioxidant micromineral (Cu, Zn, Fe) status of drug dependent subjects: Influence of illicit drugs and lifestyle. Subst. Abus. Treat. Prev. Policy 2007, 2, 12. [Google Scholar] [CrossRef] [PubMed][Green Version]
- el-Nakah, A.; Frank, O.; Louria, D.B.; Quinones, M.A.; Baker, H. A vitamin profile of heroin addiction. Am. J. Public Health. 1979, 69, 1058–1060. [Google Scholar] [CrossRef]
- Neale, J.; Nettleton, S.; Pickering, L.; Fischer, J. Eating patterns among heroin users: A qualitative study with implications for nutritional interventions. Addiction 2012, 107, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Volkow, N.D.; Wang, G.J.; Fowler, J.S.; Tomasi, D.; Baler, R. Food and Drug Reward: Overlapping Circuits in Human Obesity and Addiction. In Brain Imaging Behavioral Neuroscience; Carter, C.S., Dalley, J.W., Eds.; Springer: Berlin/Heidelberg, Germany, 2011; pp. 1–24. [Google Scholar]
- Volkow, N.D.; Wang, G.J.; Fowler, J.S.; Tomasi, D. Addiction Circuitry in the Human Brain. Annu. Rev. Pharmacol. Toxicol. 2012, 52, 321–336. [Google Scholar] [CrossRef]
- Tapper, K.; Baker, L.; Jiga-Boy, G.; Haddock, G.; Maio, G.R. Sensitivity to reward and punishment: Associations with diet, alcohol consumption, and smoking. Personal. Individ. Differ. 2015, 72, 79–84. [Google Scholar] [CrossRef]
- Higgins, G.A.; Sellers, E.M.; Fletcher, P.J. From obesity to substance abuse: Therapeutic opportunities for 5-HT2C receptor agonists. Trends Pharmacol. Sci. 2013, 34, 560–570. [Google Scholar] [CrossRef]
- Hill, J.O.; Berridge, K.; Avena, N.M.; Ziauddeen, H.; Alonso-Alonso, M.; Allison, D.B.; Khan, N.A.; Kelley, M. Neurocognition: The Food–Brain Connection. Adv. Nutr. 2014, 5, 544–546. [Google Scholar] [CrossRef][Green Version]
- Boggiano, M.M.; Chandler, P.C.; Viana, J.B.; Oswald, K.D.; Maldonado, C.R.; Wauford, P.K. Combined dieting and stress evoke exaggerated responses to opioids in binge-eating rats. Behav. Neurosci. 2005, 119, 1207–1214. [Google Scholar] [CrossRef]
- Davis, C. A Narrative Review of Binge Eating and Addictive Behaviors: Shared Associations with Seasonality and Personality Factors. Front. Psychiatry 2013, 4, 183. [Google Scholar] [CrossRef]
- Witek, K.; Wydra, K.; Filip, M. A High-Sugar Diet Consumption, Metabolism and Health Impacts with a Focus on the Development of Substance Use Disorder: A Narrative Review. Nutrients 2022, 14, 2940. [Google Scholar] [CrossRef]
- Leonardo, F.H.; Fernández-Demeneghi, R.; Moreno, A.G.M.; Huerta-Canseco, C.; Camacho-Morales, A. El rol del azúcar y los edulcorantes en la adicción a la comida: Una mirada desde la neurociencia. J. Behav. Feed. 2024, 4, 1–10. [Google Scholar] [CrossRef]
- Winterdahl, M.; Noer, O.; Orlowski, D.; Schacht, A.C.; Jakobsen, S.; Alstrup, A.K.O.; Gjedde, A.; Landau, A.M. Sucrose intake lowers μ-opioid and dopamine D2/3 receptor availability in porcine brain. Sci. Rep. 2019, 9, 16918. [Google Scholar] [CrossRef] [PubMed]
- Brunault, P.; Salamé, E.; Jaafari, N.; Courtois, R.; Réveillère, C.; Silvain, C.; Benyamina, A.; Blecha, L.; Belin, D.; Ballon, N. Why do liver transplant patients so often become obese? The addiction transfer hypothesis. Med. Hypotheses 2015, 85, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Leggio, L.; Cardone, S.; Ferrulli, A.; Kenna, G.A.; Diana, M.; Swift, R.M.; Addolorato, G. Turning the Clock Ahead: Potential Preclinical and Clinical Neuropharmacological Targets for Alcohol Dependence. Curr. Pharm. Des. 2010, 16, 2159–2181. [Google Scholar] [CrossRef]
- Verzr, F. Nutrition as a Factor against Addiction. Am. J. Clin. Nutr. 1955, 3, 363–374. [Google Scholar] [CrossRef]
- American Dietetic Association. Position of The American Dietetic Association: Nutrition intervention in treatment and recovery from chemical dependency. J. Am. Diet. Assoc. 1990, 90, 1274–1277. [Google Scholar] [CrossRef]
- Noble, C.; McCombie, L. Nutritional considerations in intravenous drug misusers: A review of the literature and current issues for dietitians. J. Hum. Nutr. Diet. 1997, 10, 181–191. [Google Scholar] [CrossRef]
- Wiss, D.A. The Role of Nutrition in Addiction Recovery. In The Assessment and Treatment of Addiction; Elsevier: Amsterdam, The Netherlands, 2019; pp. 21–42. [Google Scholar]
- Degenhardt, L.; Charlson, F.; Ferrari, A.; Santomauro, D.; Erskine, H.; Mantilla-Herrara, A.; Whiteford, H.; Leung, J.; Naghavi, M.; Griswold, M.; et al. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry 2018, 5, 987–1012. [Google Scholar] [CrossRef]
- McClain, C.J.; Rios, C.D.; Condon, S.; Marsano, L.S. Malnutrition and Alcohol-Associated Hepatitis. Clin. Liver Dis. 2021, 25, 557–570. [Google Scholar] [CrossRef]
- Calvani, R.; Picca, A.; Coelho-Júnior, H.J.; Tosato, M.; Marzetti, E.; Landi, F. Diet for the prevention and management of sarcopenia. Metabolism 2023, 146, 155637. [Google Scholar] [CrossRef]
- Nowson, C.; O’Connell, S. Protein Requirements and Recommendations for Older People: A Review. Nutrients 2015, 7, 6874–6899. [Google Scholar] [CrossRef]
- Moreno Otero, R.; Cortés, J.R. Nutrición y alcoholismo crónico. Nutr. Hosp. 2008, 23, 3–7. [Google Scholar] [PubMed]
- Rasiah, R.; Gregoriano, C.; Mueller, B.; Kutz, A.; Schuetz, P. Hospital Outcomes in Medical Patients With Alcohol-Related and Non–Alcohol-Related Wernicke Encephalopathy. Mayo Clin. Proc. 2024, 99, 740–753. [Google Scholar] [CrossRef] [PubMed]
- Mancinelli, R.; Ceccanti, M. Biomarkers in Alcohol Misuse: Their Role in the Prevention and Detection of Thiamine Deficiency. Alcohol Alcohol. 2009, 44, 177–182. [Google Scholar] [CrossRef]
- Kizilgul, M.; Ozcelik, O.; Delibasi, T. Bone health and vitamin D status in alcoholic liver disease. Indian J. Gastroenterol. 2016, 35, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Savić, Ž.; Vračarić, V.; Milić, N.; Nićiforović, D.; Damjanov, D.; Pellicano, R.; Medić-Stojanoska, M.; Abenavoli, L. Vitamin D supplementation in patients with alcoholic liver cirrhosis: A prospective study. Minerva Medica 2018, 109, 352–357. [Google Scholar] [CrossRef]
- Wilkens Knudsen, A.; Jensen, J.E.B.; Nordgaard-Lassen, I.; Almdal, T.; Kondrup, J.; Becker, U. Nutritional intake and status in persons with alcohol dependency: Data from an outpatient treatment programme. Eur. J. Nutr. 2014, 53, 1483–1492. [Google Scholar] [CrossRef]
- Kiela, P.R. Unraveling the pathophysiology of alcohol-induced thiamine deficiency. Am. J. Physiol. Renal. Physiol. 2010, 299, 26–27. [Google Scholar] [CrossRef]
- Zuluaga, P.; Casado-Carbajo, J.; Hernández-Rubio, A.; Bueno-Vélez, M.; García-Martin, C.; Muga, R.; Fuster, D. Vitamin D Deficiency Is Associated with Advanced Liver Fibrosis and Impaired Fasting Glucose in Alcohol Use Disorder. Nutrients 2024, 16, 1099. [Google Scholar] [CrossRef]
- Liu, Y.; Xu, Y.; Wang, Y.; Pang, L.; Zhang, X. Relationship between serum vitamin D and thyroid hormone profiles in male patients with alcohol dependence. BMC Psychiatry 2023, 23, 775. [Google Scholar] [CrossRef] [PubMed]
- Tardelli, V.S.; Lago, M.P.P.D.; Silveira, D.X.D.; Fidalgo, T.M. Vitamin D and alcohol: A review of the current literature. Psychiatry Res. 2017, 248, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Banjac Baljak, V.; Mihajlovic, G.; Zivlak-Radulovic, N.; Nezic, L.; Miskovic, M.; Banjac, V. Association between Vitamin D and Cognitive Deficiency in Alcohol Dependence. Healthcare 2022, 10, 1772. [Google Scholar] [CrossRef] [PubMed]
- García-Quiroz, J.; García-Becerra, R.; Lara-Sotelo, G.; Avila, E.; López, S.; Santos-Martínez, N.; Halhali, A.; Ordaz-Rosado, D.; Barrera, D.; Olmos-Ortiz, A.; et al. Chronic moderate ethanol intake differentially regulates vitamin D hydroxylases gene expression in kidneys and xenografted breast cancer cells in female mice. J. Steroid Biochem. Mol. Biol. 2017, 173, 148–156. [Google Scholar] [CrossRef]
- Hsu, C.H.; Patel, S.; Buchsbaum, B.L. Calcitriol Metabolism in Patients With Chronic Renal Failure. Am. J. Kidney Dis. 1991, 17, 185–190. [Google Scholar] [CrossRef]
- Medici, V.; Halsted, C.H. Folate, alcohol, and liver disease. Mol. Nutr. Food Res. 2013, 57, 596–606. [Google Scholar]
- Zhong, W.; Wei, X.; Hao, L.; Lin, T.D.; Yue, R.; Sun, X.; Guo, W.; Dong, H.; Li, T.; Ahmadi, A.R.; et al. Paneth Cell Dysfunction Mediates Alcohol-related Steatohepatitis Through Promoting Bacterial Translocation in Mice: Role of Zinc Deficiency. Hepatology 2020, 71, 1575–1591. [Google Scholar] [CrossRef] [PubMed]
- Poikolainen, K.; Alho, H. Magnesium treatment in alcoholics: A randomized clinical trial. Subst. Abus. Treat. Prev. Policy 2008, 3, 1. [Google Scholar]
- Fialla, A.D.; Israelsen, M.; Hamberg, O.; Krag, A.; Gluud, L.L. Nutritional therapy in cirrhosis or alcoholic hepatitis: A systematic review and meta-analysis. Liver Int. 2015, 35, 2072–2078. [Google Scholar] [CrossRef]
- Sung, H.; Kim, S.W.; Hong, M.; Suk, K.T. Microbiota-based treatments in alcoholic liver disease. World J. Gastroenterol. 2016, 22, 6673. [Google Scholar] [CrossRef]
- Carito, V.; Ceccanti, M.; Cestari, V.; Natella, F.; Bello, C.; Coccurello, R.; Mancinelli, R.; Fiore, M. Olive polyphenol effects in a mouse model of chronic ethanol addiction. Nutrition 2017, 33, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Gandía, M.d.C.; Ródenas-González, F.; Pascual, M.; Reguilón, M.D.; Guerri, C.; Miñarro, J.; Rodríguez-Arias, M. Ketogenic Diet Decreases Alcohol Intake in Adult Male Mice. Nutrients 2021, 13, 2167. [Google Scholar] [CrossRef] [PubMed]
- Kirpich, I.A.; Solovieva, N.V.; Leikhter, S.N.; Shidakova, N.A.; Lebedeva, O.V.; Sidorov, P.I.; Bazhukova, T.A.; Soloviev, A.G.; Barve, S.S.; McClain, C.J.; et al. Probiotics restore bowel flora and improve liver enzymes in human alcohol-induced liver injury: A pilot study. Alcohol 2008, 42, 675–682. [Google Scholar]
- Chen, D.; Liu, Y.; He, W.; Wang, H.; Wang, Z. Neurotransmitter-precursor-supplement intervention for detoxified heroin addicts. J. Huazhong Univ. Sci. Technol. Med. Sci. 2012, 32, 422–427. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi-Ardekani, K.; Haghighi, M.; Zarrin, R. Effects of omega-3 fatty acid supplementation on cigarette craving and oxidative stress index in heavy-smoker males: A double-blind, randomized, placebo-controlled clinical trial. J. Psychopharmacol. 2018, 32, 995–1002. [Google Scholar] [CrossRef]
- LaRowe, S.D.; Myrick, H.; Hedden, S.; Mardikian, P.; Saladin, M.; McRae, A.; Brady, K.; Kalivas, P.W.; Malcolm, R. Is Cocaine Desire Reduced by N -Acetylcysteine? Am. J. Psychiatry 2007, 164, 1115–1117. [Google Scholar] [CrossRef]
- Hakimian, J.K.; Dong, T.S.; Barahona, J.A.; Lagishetty, V.; Tiwari, S.; Azani, D.; Barrera, M.; Lee, S.; Severino, A.L.; Mittal, N.; et al. Dietary Supplementation with Omega-3 Polyunsaturated Fatty Acids Reduces Opioid-Seeking Behaviors and Alters the Gut Microbiome. Nutrients 2019, 11, 1900. [Google Scholar] [CrossRef]
- Anema, A.; Wood, E.; Weiser, S.D.; Qi, J.; Montaner, J.S.; Kerr, T. Hunger and associated harms among injection drug users in an urban Canadian setting. Subst. Abus. Treat. Prev. Policy 2010, 5, 20. [Google Scholar] [CrossRef]
- Santolaria-Fernández, F. Nutritional assessment of drug addicts. Drug Alcohol Depend. 1995, 38, 11–18. [Google Scholar]
- Varela, P.; Marcos, A.; Santacruz, I.; Ripoll, S.; Requejo, A. Human immunodeficiency virus infection and nutritional status in female drug addicts undergoing detoxification: Anthropometric and immunologic assessments. Am. J. Clin. Nutr. 1997, 66, 504S–508S. [Google Scholar] [CrossRef]
- Chivero, E.T.; Ahmad, R.; Thangaraj, A.; Periyasamy, P.; Kumar, B.; Kroeger, E.; Feng, D.; Guo, M.-L.; Roy, S.; Dhawan, P.; et al. Cocaine Induces Inflammatory Gut Milieu by Compromising the Mucosal Barrier Integrity and Altering the Gut Microbiota Colonization. Sci. Rep. 2019, 9, 12187. [Google Scholar] [CrossRef]
- Guindalini, C.; Howard, M.; Haddley, K.; Laranjeira, R.; Collier, D.; Ammar, N.; Craig, I.; O’gara, C.; Bubb, V.J.; Greenwood, T.; et al. A dopamine transporter gene functional variant associated with cocaine abuse in a Brazilian sample. Proc. Natl. Acad. Sci. USA 2006, 103, 4552–4557. [Google Scholar] [CrossRef] [PubMed]
- Koob, G.; Kreek, M.J. Stress, Dysregulation of Drug Reward Pathways, and the Transition to Drug Dependence. Am. J. Psychiatry 2007, 164, 1149–1159. [Google Scholar] [CrossRef]
- Uys, J.D.; Mulholland, P.J.; Townsend, D.M. Glutathione and redox signaling in substance abuse. Biomed. Pharmacother. 2014, 68, 799–807. [Google Scholar] [CrossRef]
- Peles, E.; Schreiber, S.; Sason, A.; Adelson, M. Risk Factors for Weight Gain during Methadone Maintenance Treatment. Subst. Abus. 2016, 37, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Glasner-Edwards, S.; Mooney, L.J.; Marinelli-Casey, P.; Hillhouse, M.; Ang, A.; Rawson, R.; Proje, T.M.T. Bulimia Nervosa Among Methamphetamine Dependent Adults: Association With Outcomes Three Years After Treatment. Eat. Disord. 2011, 19, 259–269. [Google Scholar] [CrossRef][Green Version]
- Gonçalves, J.; Martins, J.; Baptista, S.; Ambrósio, A.F.; Silva, A.P. Effects of drugs of abuse on the central neuropeptide Y system: NPY and drug abuse. Addict. Biol. 2016, 21, 755–765. [Google Scholar] [CrossRef] [PubMed]
- Lv, D.; Zhang, M.; Jin, X.; Zhao, J.; Han, B.; Su, H.; Zhang, J.; Zhang, X.; Ren, W.; He, J. The Body Mass Index, Blood Pressure, and Fasting Blood Glucose in Patients With Methamphetamine Dependence. Medicine 2016, 95, e3152. [Google Scholar] [CrossRef]
- Li, Y.; Kong, D.; Bi, K.; Luo, H. Related Effects of Methamphetamine on the Intestinal Barrier via Cytokines, and Potential Mechanisms by Which Methamphetamine May Occur on the Brain-Gut Axis. Front. Med. 2022, 9, 783121. [Google Scholar] [CrossRef]
- Curd, P.; Ohlmann, K.; Bush, H. Effectiveness of a Voluntary Nutrition Education Workshop in a State Prison. J. Correct. Health Care 2013, 19, 144–150. [Google Scholar] [CrossRef]
- Barbadoro, P.; Ponzio, E.; Pertosa, M.E.; Aliotta, F.; D’Errico, M.M.; Prospero, E.; Minelli, A. The Effects of Educational Intervention on Nutritional Behaviour in Alcohol-Dependent Patients. Alcohol Alcohol. 2011, 46, 77–79. [Google Scholar] [CrossRef] [PubMed]
- Cowan, J.A.; Devine, C.M. Process evaluation of an environmental and educational nutrition intervention in residential drug-treatment facilities. Public Health Nutr. 2012, 15, 1159–1167. [Google Scholar] [CrossRef] [PubMed]
| Author | Population | Substance | Results | Conclusion |
|---|---|---|---|---|
| Saeland et al., 2011 [15] | 123 male and 72 female drug addicts from Norway. | Multi-drug users | Added sugar accounted for 30% of the energy intake. Sugar and sugar-sweetened food items were preferred by 61% of the respondents. | Drug addicts have a high risk of inadequacy of food and nutrient intake. |
| Ross et al., 2012 [2] | 67 patients (48 male, 19 female) drug addicts from Australia. | Multi-drug users | The prevalence of mild/moderate malnutrition was found to be 24%. 50% of all subjects were deficient in iron or vitamins (low vitamin A levels in 21%, low iron levels in 18%, low-range potassium in 12%, and low vitamin C levels in 8%). | Chronic substance abuse affects the nutritional status and is associated with nutrient deficiencies and malnutrition. |
| Nazrul Islam et al., 2002 [14] | 253 male drug addicts from Bangladesh. | Multi-drug users | The drug addicts had significantly lowered BMI *, hemoglobin, and serum total protein and albumin levels. 60% of drug addicts were suffering from multiple malnutrition. | Drug addicts have poor nutritional status. Multiple malnutrition or nutrient deficiency is prevalent among them. |
| Santolaria et al., 2000 [3] | 181 hospitalized male alcoholics from Spain. | Alcohol | BMI was under 18.5 kg/m2 in 8.9%. Malnutrition was related to the intensity of ethanol intake, development of social or familial problems, irregularity of feeding habits, and cirrhosis with ascites. | Malnutrition related to alcoholism seems multifactorial in its pathogenesis. |
| Yazici et al., 2019 [16] | 189 schizophrenia patients, 119 substance use disorder patients and, and 109 controls from Turkey. | Multi-drug users | The prevalence of vitamin B12 deficiency in the SUD group was significantly higher than that in the control group (28.3% vs. 11.5%). Compared with the control group, vitamin D and B12 levels were significantly lower in the schizophrenia group, and folic acid and B12 levels were significantly lower in the SUD group. | Several vitamin deficiencies appear to be common in both schizophrenia and substance use disorder patients. |
| Bemanian et al., 2022 [17] | 666 participants drawn from outpatient opioid agonist therapy from Norway. | Opiods | 57% of all subjects had vitamin D deficiency (<50 nmol/L), and 19% were severely deficient (<25 nmol/L). | Patients with severe substance use disorders have a high prevalence of vitamin D deficiency. |
| Madebo et al., 2022 [18] | 672 SUD patients from Norway. | Multi-drug users | 22% of the population had suboptimal B12 levels (<300 pmol/L) and 1.2% were deficient (<175 pmol/L). | People with SUDs have B12 suboptimal levels that might or might not be adequate for metabolic needs. |
| Bemanian et al., 2022 [19] | 663 participants drawn from outpatient opioid agonist therapy from Norway. | Opioids | 48% of the population had low serum folate levels (<10 nmol/L), and 23% were deficient (<6.8 nmol/L). | Injecting substances is associated with a reduction in serum folate over time. |
| Author | Substance | Study Design | Population | Nutritional Approach | Outcome |
|---|---|---|---|---|---|
| Evidence in humans | |||||
| Kirpich et al., 2009. [77] | Alcohol | Randomized, prospective clinical trial | 66 adult alcoholics from Russia | Probiotic therapy of 0.9 × 108 colony-forming unit (CFU) Bifidobacterium bifidum and 0.9 × 109 CFU Lactobacillus plantarum 8PA3 for 6 days. | Repopulation of the intestinal microbiota. |
| Lee et al., 2024 [10] | Retrospective cohort study | 5725 alcoholic subjects from Korea | High adherence to the Mediterranean diet. | Decrease in the risk of steatotic liver disease, metabolic dysfunction-associated steatotic liver disease and alcohol-related liver diseases. | |
| Ghaderi et al., 2017. [11] | Opioids | Randomized, prospective clinical trial | 68 patients with methadone treatment from Iran. | 50,000 UI of vitamin D every 2 weeks for 12 weeks. | Improvements in sleep quality and decreased depression. |
| Chen et al., 2012. [78] | Randomized, prospective clinical trial | 83 detoxified heroin addicts from China. | 50 mg/kg/day of supplements containing neurotransmitter precursors (tyrosine, lecithin, L-glutamine, and 5-hydroxytryptophan). | Reduction in withdrawal and mood symptoms during recovery. | |
| Ardekani et al., 2018 [79] | Cigarette | Randomized, prospective clinical trial | 54 heavy-smoker males from Iran. | 5 capsules of fish-oil-derived omega-3 fatty acid supplements (containing 180 mg of eicosapentaenoic acid and 120 mg of docosahexaenoic acid) for 3 months. | Reduction in cigarette craving and oxidative stress index in heavy-smoker males. |
| LaRowe et al., 2007. [80] | Cocaine | Randomized, prospective clinical trial | Six subjects with criteria for cocaine dependence from EE.UU. | 600 mg of N-acetylcysteine for 3 days. | Decreased cue-induced craving in cocaine-dependent individuals. |
| Evidence in murine models | |||||
| Carito et al., 2017. [75] | Alcohol | Experimental | Murine model | 20 mg/kg of olive polyphenols for two months. | Protective effect on alcohol-induced oxidative stress. |
| Imam and Ali, 2000 [12] | Methampheta-mines | Experimental | Murine model | Supplementation with 0.5 mg/kg of selenium for one week. | Reduction in neurotoxicity. |
| Hakimian et al., 2019 [81] | Opioids | Experimental | Murine model | Omega-3 fatty acids-enriched diet. | Decrease in anxiety-induced opioid-seeking behavior. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Estrada, J.; Luquin, S.; Pesqueda-Cendejas, K.; Ruiz-Ballesteros, A.I.; Campos-López, B.; Meza-Meza, M.R.; Parra-Rojas, I.; González-Castañeda, R.E.; Ramos-Lopez, O.; De la Cruz-Mosso, U. Malnutrition in Substance Use Disorders: A Critical Issue in Their Treatment and Recovery. Healthcare 2025, 13, 868. https://doi.org/10.3390/healthcare13080868
García-Estrada J, Luquin S, Pesqueda-Cendejas K, Ruiz-Ballesteros AI, Campos-López B, Meza-Meza MR, Parra-Rojas I, González-Castañeda RE, Ramos-Lopez O, De la Cruz-Mosso U. Malnutrition in Substance Use Disorders: A Critical Issue in Their Treatment and Recovery. Healthcare. 2025; 13(8):868. https://doi.org/10.3390/healthcare13080868
Chicago/Turabian StyleGarcía-Estrada, Joaquín, Sonia Luquin, Karen Pesqueda-Cendejas, Adolfo I. Ruiz-Ballesteros, Bertha Campos-López, Mónica R. Meza-Meza, Isela Parra-Rojas, Rocío Elizabeth González-Castañeda, Omar Ramos-Lopez, and Ulises De la Cruz-Mosso. 2025. "Malnutrition in Substance Use Disorders: A Critical Issue in Their Treatment and Recovery" Healthcare 13, no. 8: 868. https://doi.org/10.3390/healthcare13080868
APA StyleGarcía-Estrada, J., Luquin, S., Pesqueda-Cendejas, K., Ruiz-Ballesteros, A. I., Campos-López, B., Meza-Meza, M. R., Parra-Rojas, I., González-Castañeda, R. E., Ramos-Lopez, O., & De la Cruz-Mosso, U. (2025). Malnutrition in Substance Use Disorders: A Critical Issue in Their Treatment and Recovery. Healthcare, 13(8), 868. https://doi.org/10.3390/healthcare13080868









