Telemedicine Adoption and Prospects in Sub-Sahara Africa: A Systematic Review with a Focus on South Africa, Kenya, and Nigeria
Abstract
1. Introduction
2. Methods
2.1. Transparency Statement
2.2. Search Strategy
2.3. Exclusion Criteria
2.4. Quality Assessment
2.5. Data Extraction
2.6. Data Synthesis
3. Results
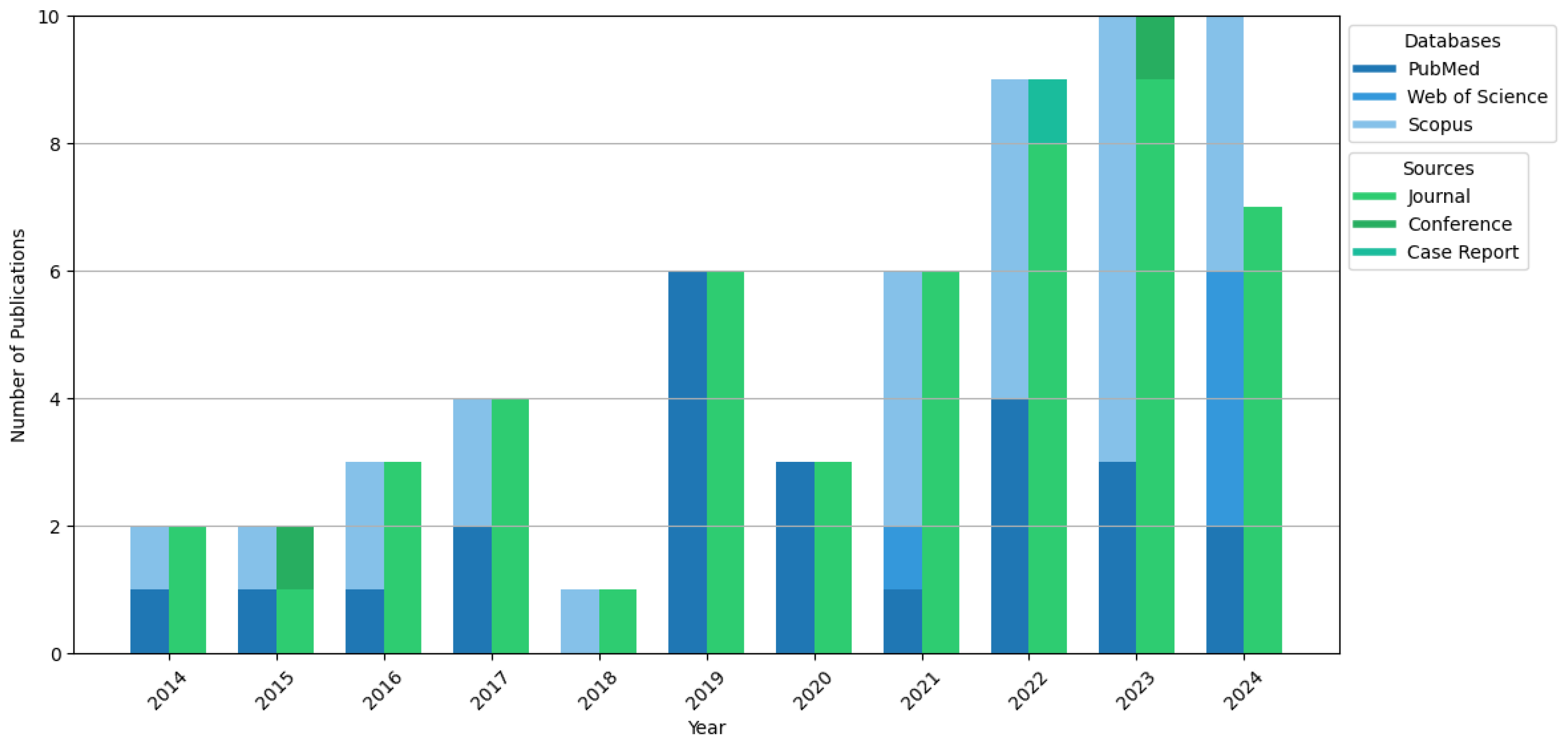
3.1. Search Results and Demographic Characteristics
3.2. Keywords Analysis
3.3. Findings
3.3.1. Telemedicine Innovations and Adoption
3.3.2. Healthcare Delivery and Public Health Impact
3.3.3. Equity, Policy, and Socioeconomic Factors of Telemedicine Adoption
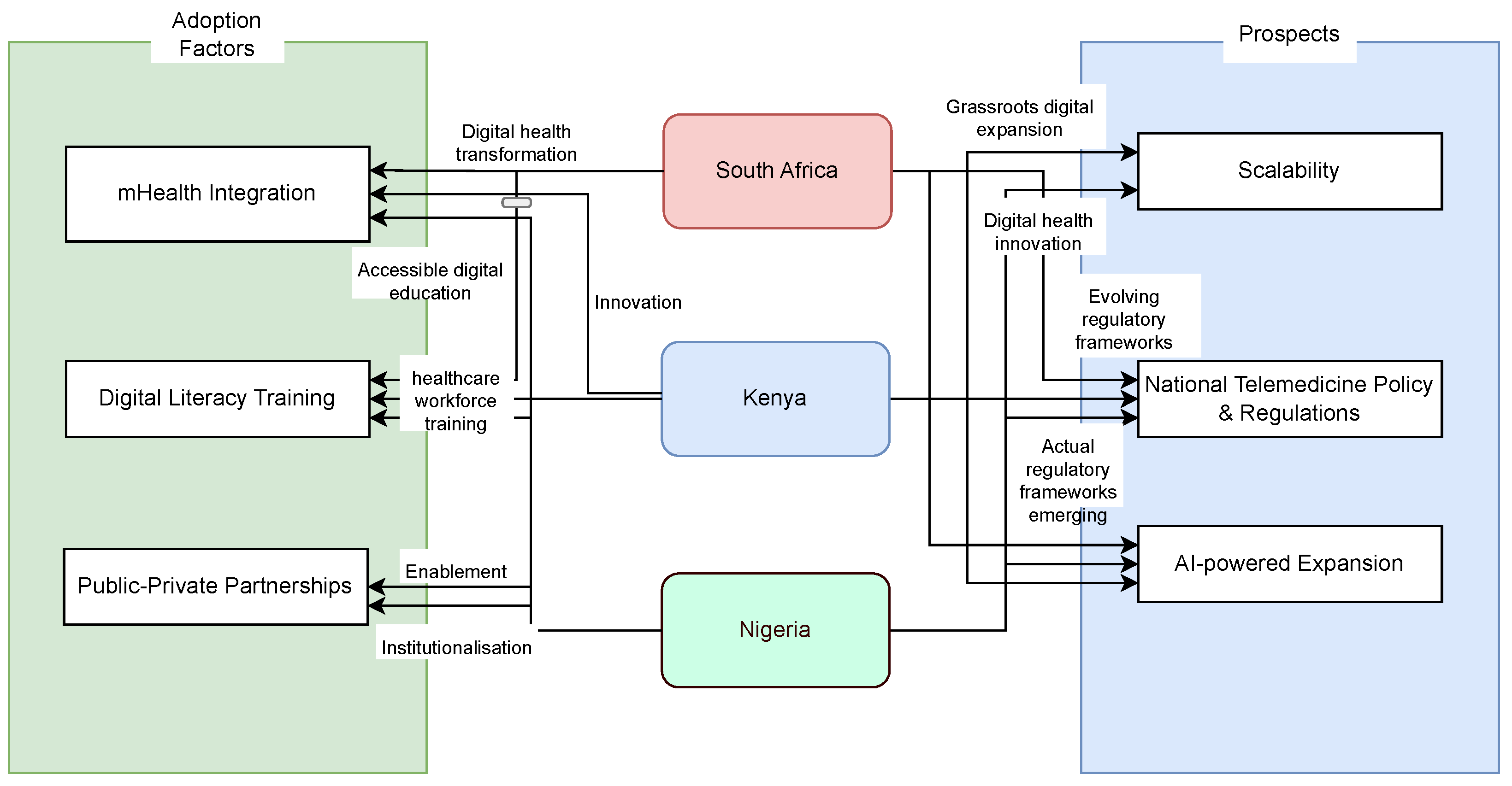
4. Comparative Insights on Adoption, Challenges, and Prospects
4.1. South Africa
- Government and Institutional Support: Existing telemedicine policies and professional guidelines, such as those by the Health Professions Council of South Africa (HPCSA), have provided a regulatory framework for telehealth services [83].
4.2. Kenya
4.3. Nigeria
- Mobile Technology Penetration: High mobile phone usage has facilitated mHealth adoption, particularly in maternal and child health services [25].
- Growing Mobile Health (mHealth) Integration: SMS-based health interventions, smartphone applications, and chatbots are increasing across all three countries.
- Urban–Rural Disparities in Digital Health Access: While urban populations have benefited from broadband-enabled telehealth services, rural communities still struggle with connectivity, affordability, and digital literacy barriers.
- Healthcare Provider Engagement as a Key Adoption Driver: The studies indicate that clinician readiness, training, and institutional support are crucial in determining telemedicine adoption levels.
- Policy and Regulatory Influence on Adoption Rates: Countries with formalised telemedicine policies (such as South Africa) exhibit higher adoption, whereas countries lacking structured frameworks (such as Nigeria and Kenya) face slower telemedicine integration.
- Limited policy support: The absence of national telemedicine frameworks in Nigeria and Kenya prevents widespread adoption. Even in South Africa, where some guidelines exist, gaps in regulatory structures hinder full-scale implementation.
- Financial constraints: The cost of internet, mobile data, and digital devices remains a significant obstacle, particularly in low-income and rural areas. Many patients and providers cannot afford the necessary technology to engage in telemedicine services.
- Infrastructure limitations: Unreliable electricity, weak broadband connectivity, and a lack of ICT infrastructure hinder telemedicine effectiveness, particularly in remote and underserved communities.
- Healthcare provider resistance: Many clinicians remain reluctant to adopt telemedicine due to workflow disruptions, lack of financial incentives, and concerns over diagnostic accuracy in virtual settings.
- Digital literacy gaps: A lack of patient and provider familiarity with telemedicine tools affects adoption rates, requiring greater digital education and training investment.
- Policy Reforms and Regulatory Advancements: The development of national telemedicine policies that include clear reimbursement structures, licensing regulations, and data protection laws will drive long-term sustainability and provider adoption. South Africa’s existing framework serves as a model that Nigeria and Kenya can adapt to suit their unique healthcare needs.
- Equity-Focused Interventions: Targeted digital inclusion programs, such as subsidised internet access, community-based telemedicine hubs, and digital literacy training, can improve access to telehealth services in rural and underserved communities.
- Expansion of Broadband and Mobile Infrastructure: Investments in broadband expansion, mobile network reliability, and electricity infrastructure will enhance telemedicine accessibility, particularly in remote regions.
- AI and Machine Learning in Telemedicine: Integrating AI-powered diagnostics, predictive analytics, and personalised health recommendations presents new opportunities for scalable, efficient healthcare delivery. AI-driven chatbots and virtual assistants can enhance patient engagement and triage systems, reducing the burden on overstretched healthcare facilities.
- Public–Private Partnerships: Strengthening collaborations between governments, technology firms, and healthcare institutions can accelerate investment in digital health infrastructure, subsidise access to telemedicine services, and support healthcare workforce training.
- Incentivising Healthcare Providers: Capacity-building programs and financial incentives for healthcare providers will improve digital literacy and encourage telemedicine integration into mainstream healthcare workflows.
5. Discussion
5.1. Recommendations and Future Directions
- Longitudinal Impact Studies: Assess the long-term effectiveness of telemedicine interventions in improving health outcomes, particularly for chronic disease management and maternal healthcare.
- Regulatory and Ethical Considerations: Explore data governance, cybersecurity, and patient consent frameworks to ensure ethical and secure telemedicine practices.
- Cultural and Social Acceptance: Research on the socio-cultural factors influencing telemedicine adoption, including trust in digital health solutions, is essential for tailoring interventions to diverse populations.
- Artificial Intelligence (AI) and Emerging Technologies: Investigating the integration of artificial intelligence, wearable health devices, and blockchain for data security can enhance telemedicine effectiveness.
5.2. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Agyepong, I.A.; Sewankambo, N.; Binagwaho, A.; Coll-Seck, A.M.; Corrah, T.; Ezeh, A.; Fekadu, A.; Kilonzo, N.; Lamptey, P.; Masiye, F.; et al. The path to longer and healthier lives for all Africans by 2030: The Lancet Commission on the future of health in sub-Saharan Africa. Lancet 2017, 390, 2803–2859. [Google Scholar] [PubMed]
- Dodoo, J.E.; Al-Samarraie, H.; Alsswey, A. The development of telemedicine programs in Sub-Saharan Africa: Progress and associated challenges. Health Technol. 2022, 12, 33–46. [Google Scholar] [CrossRef] [PubMed]
- Mbunge, E.; Muchemwa, B.; Batani, J. Are we there yet? Unbundling the potential adoption and integration of telemedicine to improve virtual healthcare services in African health systems. Sens. Int. 2022, 3, 100152. [Google Scholar] [CrossRef] [PubMed]
- Akande, O.W.; Muzigaba, M.; Igumbor, E.U.; Elimian, K.; Bolarinwa, O.A.; Musa, O.I.; Akande, T.M. The effectiveness of an m-Health intervention on the sexual and reproductive health of in-school adolescents: A cluster randomized controlled trial in Nigeria. Reprod. Health 2024, 21, 6. [Google Scholar] [CrossRef]
- Janssen, R.; Engel, N.; Esmail, A.; Oelofse, S.; Krumeich, A.; Dheda, K.; Pai, N.P. Alone but supported: A qualitative study of an HIV self-testing app in an observational cohort study in South Africa. AIDS Behav. 2020, 24, 467–474. [Google Scholar] [CrossRef]
- Macharia, P.; Pérez-Navarro, A.; Sambai, B.; Inwani, I.; Kinuthia, J.; Nduati, R.; Carrion, C. An Unstructured Supplementary Service Data–Based mHealth App Providing On-Demand Sexual Reproductive Health Information for Adolescents in Kibra, Kenya: Randomized Controlled Trial. JMIR Mhealth Uhealth 2022, 10, e31233. [Google Scholar] [CrossRef]
- Alegbeleye, B.J.; Mohammed, R.K. Challenges of healthcare delivery in the context of COVID-19 pandemic in Sub-Saharan Africa. Iberoam. J. Med. 2020, 2, 100–109. [Google Scholar]
- Gaobotse, G.; Mbunge, E.; Batani, J.; Muchemwa, B. The future of smart implants towards personalized and pervasive healthcare in Sub-Saharan Africa: Opportunities, barriers and policy recommendations. Sens. Int. 2022, 3, 100173. [Google Scholar] [CrossRef]
- Ahinkorah, B.O.; Budu, E.; Seidu, A.A.; Agbaglo, E.; Adu, C.; Ameyaw, E.K.; Ampomah, I.G.; Archer, A.G.; Kissah-Korsah, K.; Yaya, S. Barriers to healthcare access and healthcare seeking for childhood illnesses among childbearing women in sub-Saharan Africa: A multilevel modelling of Demographic and Health Surveys. PLoS ONE 2021, 16, e0244395. [Google Scholar]
- Nyande, F.K.; Ricks, E.; Williams, M.; Jardien-Baboo, S. Socio-cultural barriers to the delivery and utilisation of child healthcare services in rural Ghana: A qualitative study. BMC Health Serv. Res. 2022, 22, 289. [Google Scholar]
- Contreras, C.M.; Metzger, G.A.; Beane, J.D.; Dedhia, P.H.; Ejaz, A.; Pawlik, T.M. Telemedicine: Patient-Provider Clinical Engagement During the COVID-19 Pandemic and Beyond. J. Gastrointest. Surg. 2020, 24, 1692–1697. [Google Scholar] [CrossRef] [PubMed]
- Nittari, G.; Savva, D.; Tomassoni, D.; Tayebati, S.K.; Amenta, F. Telemedicine in the COVID-19 Era: A Narrative Review Based on Current Evidence. INternational J. Environ. Res. Public Health 2022, 19, 5101. [Google Scholar] [CrossRef] [PubMed]
- Lalla-Edward, S.T.; Mashabane, N.; Stewart-Isherwood, L.; Scott, L.; Fyvie, K.; Duncan, D.; Haile, B.; Chugh, K.; Zhou, Y.; Reimers, J.; et al. Implementation of an mHealth App to Promote Engagement During HIV Care and Viral Load Suppression in Johannesburg, South Africa (iThemba Life): Pilot Technical Feasibility and Acceptability Study. JMIR Form. Res. 2022, 6, e26033. [Google Scholar] [CrossRef]
- Bobrow, K.; Farmer, A.J.; Springer, D.; Shanyinde, M.; Yu, L.M.; Brennan, T.; Rayner, B.; Namane, M.; Steyn, K.; Tarassenko, L.; et al. Mobile phone text messages to support treatment adherence in adults with high blood pressure (StAR): A single-blind, randomized trial. Circulation 2016, 133, 592. [Google Scholar] [CrossRef]
- Khan, Z.; Mlawa, G.; Yousif, Y.; Afghan, A.; Balami, D.; Mohammed, M.; Muhammad, S.; Warrier, V.; Gupta, A.; Ibrahim, M. The future of cross-continental telemedicine in the management of complicated endocrine patients and its suitability based on a case report. Cureus 2022, 14, e22174. [Google Scholar] [CrossRef]
- Meffert, S.; Mathai, M.; Neylan, T.; Mwai, D.; Onyango, D.O.; Rota, G.; Otieno, A.; Obura, R.R.; Wangia, J.; Opiyo, E.; et al. Preference of mHealth versus in-person treatment for depression and post-traumatic stress disorder in Kenya: Demographic and clinical characteristics. BMJ Open 2024, 14, e083094. [Google Scholar] [CrossRef]
- Davies, E.H.; Fieggen, K.; Wilmshurst, J.; Anyanwu, O.; Burman, R.J.; Komarzynski, S. Demonstrating the feasibility of digital health to support pediatric patients in South Africa. Epilepsia Open 2021, 6, 653–662. [Google Scholar] [CrossRef]
- Koch, M.; Matzke, I.; Huhn, S.; Sié, A.; Boudo, V.; Compaoré, G.; Maggioni, M.A.; Bunker, A.; Bärnighausen, T.; Dambach, P.; et al. Assessing the Effect of Extreme Weather on Population Health Using Consumer-Grade Wearables in Rural Burkina Faso: Observational Panel Study. JMIR Mhealth Uhealth 2023, 11, e46980. [Google Scholar] [CrossRef]
- Mash, R.; Schouw, D.; Fischer, A.E. Evaluating the Implementation of the GREAT4Diabetes WhatsApp Chatbot to Educate People with Type 2 Diabetes During the COVID-19 Pandemic: Convergent Mixed Methods Study. JMIR Diabetes 2022, 7, e37882. [Google Scholar] [CrossRef]
- Ochieng’, S.; Hariharan, N.; Abuya, T.; Okondo, C.; Ndwiga, C.; Warren, C.E.; Wickramanayake, A.; Rajasekharan, S. Exploring the implementation of an SMS-based digital health tool on maternal and infant health in informal settlements. BMC Pregnancy Childbirth 2024, 24, 222. [Google Scholar] [CrossRef]
- Perez, K.; Wisniewski, D.; Ari, A.; Lee, K.; Lieneck, C.; Ramamonjiarivelo, Z. Investigation into Application of AI and Telemedicine in Rural Communities: A Systematic Literature Review. Healthcare 2025, 13, 324. [Google Scholar] [CrossRef] [PubMed]
- Akintunde, T.Y.; Akintunde, O.D.; Musa, T.H.; Sayibu, M.; Tassang, A.E.; Reed, L.M.; Chen, S. Expanding telemedicine to reduce the burden on the healthcare systems and poverty in Africa for a post-coronavirus disease 2019 (COVID-19) pandemic reformation. Glob. Health J. 2021, 5, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Clouse, K.; Phillips, T.K.; Camlin, C.; Noholoza, S.; Mogoba, P.; Naidoo, J.; Langford, R.; Weiss, M.; Seebregts, C.J.; Myer, L. CareConekta: Study protocol for a randomized controlled trial of a mobile health intervention to improve engagement in postpartum HIV care in South Africa. Trials 2020, 21, 1–12. [Google Scholar] [CrossRef]
- Agbeyangi, A.; Suleman, H. Advances and Challenges in Low-Resource-Environment Software Systems: A Survey. Informatics 2024, 11, 90. [Google Scholar] [CrossRef]
- Udenigwe, O.; Okonofua, F.E.; Ntoimo, L.F.; Yaya, S. Enablers and barriers to the acceptability of mHealth for maternal healthcare in rural Edo, Nigeria. Dialogues Health 2022, 1, 100067. [Google Scholar] [CrossRef]
- Onyeabor, U.S.; Okenwa, W.O.; Onwuasoigwe, O.; Lasebikan, O.A.; Schaaf, T.; Pinkwart, N.; Balzer, F. Telemedicine in the age of the pandemics: The prospects of web-based remote patient monitoring systems for orthopaedic ambulatory care management in the developing economies. Digit. Health 2024, 10, 20552076241226964. [Google Scholar] [CrossRef]
- Dodoo, J.E.; Al-Samarraie, H.; Alzahrani, A.I. Telemedicine use in Sub-Saharan Africa: Barriers and policy recommendations for COVID-19 and beyond. Int. J. Med. Inform. 2021, 151, 104467. [Google Scholar] [CrossRef]
- Onsongo, S.; Kamotho, C.; Rinke de Wit, T.F.; Lowrie, K. Experiences on the Utility and Barriers of Telemedicine in Healthcare Delivery in Kenya. Int. J. Telemed. Appl. 2023, 2023, 1487245. [Google Scholar] [CrossRef]
- Chigaro, S.; Ruredzo, I.M.; Marembo, T. Integration of telehealth systems into HIV care services in sub-Saharan Africa: A scoping review. Texila Int. J. Public Health 2023, 11, 1–13. [Google Scholar] [CrossRef]
- Chitungo, I.; Mhango, M.; Mbunge, E.; Dzobo, M.; Musuka, G.; Dzinamarira, T. Utility of telemedicine in sub-Saharan Africa during the COVID-19 pandemic. A rapid review. Hum. Behav. Emerg. Technol. 2021, 3, 843–853. [Google Scholar] [CrossRef]
- Dzando, G.; Akpeke, H.; Kumah, A.; Agada, E.; Lartey, A.A.; Nortu, J.; Nutakor, H.S.; Donyi, A.B.; Dordunu, R. Telemedicine in Ghana: Insight into the past and present, a narrative review of literature amidst the Coronavirus pandemic. J. Public Health Afr. 2022, 13, a369. [Google Scholar] [CrossRef]
- Kipruto, H.; Muneene, D.; Droti, B.; Jepchumba, V.; Okeibunor, C.J.; Nabyonga-Orem, J.; Karamagi, H.C. Use of Digital Health Interventions in Sub-Saharan Africa for Health Systems Strengthening Over the Last 10 Years: A Scoping Review Protocol. Front. Digit. Health 2022, 4, 874251. [Google Scholar] [CrossRef]
- Blocker, A.; Datay, M.I.; Mwangama, J.; Malila, B. Development of a telemedicine virtual clinic system for remote, rural, and underserved areas using user-centered design methods. Digit. Health 2024, 10, 20552076241256752. [Google Scholar] [CrossRef] [PubMed]
- Opoku, D.; Busse, R.; Quentin, W. Achieving Sustainability and Scale-Up of Mobile Health Noncommunicable Disease Interventions in Sub-Saharan Africa: Views of Policy Makers in Ghana. JMIR Mhealth Uhealth 2019, 7, e11497. [Google Scholar] [CrossRef]
- Adenuga, K.I.; Iahad, N.A.; Miskon, S. Towards reinforcing telemedicine adoption amongst clinicians in Nigeria. Int. J. Med. Inform. 2017, 104, 84–96. [Google Scholar] [CrossRef]
- Patel, A.R.; Kessler, J.; Braithwaite, R.S.; Nucifora, K.A.; Thirumurthy, H.; Zhou, Q.; Lester, R.T.; Marra, C.A. Economic evaluation of mobile phone text message interventions to improve adherence to HIV therapy in Kenya. Medicine 2017, 96, e6078. [Google Scholar] [CrossRef]
- Gbadamosi, S.O.; Eze, C.; Olawepo, J.O.; Iwelunmor, J.; Sarpong, D.F.; Ogidi, A.G.; Patel, D.; Oko, J.O.; Onoka, C.; Ezeanolue, E.E. A Patient-Held Smartcard With a Unique Identifier and an mHealth Platform to Improve the Availability of Prenatal Test Results in Rural Nigeria: Demonstration Study. J. Med. Internet Res. 2018, 20, e18. [Google Scholar] [CrossRef]
- Barteit, S.; Jahn, A.; Banda, S.S.; Bärnighausen, T.; Bowa, A.; Chileshe, G.; Guzek, D.; Jorge, M.M.; Lüders, S.; Malunga, G.; et al. E-Learning for Medical Education in Sub-Saharan Africa and Low-Resource Settings: Viewpoint. J. Med. Internet Res. 2019, 21, e12449. [Google Scholar] [CrossRef]
- Ferre, Z.; Gerstenblüth, M.; González, C.; Noboa, C.; Triunfo, P. Salud y acceso a cuidados médicos durante la pandemia en Uruguay. Rev. Méd. Del Urug. 2021, 37, e37307. [Google Scholar]
- Endler, M.; Petro, G.; Danielsson, K.G.; Grossman, D.; Gomperts, R.; Weinryb, M.; Constant, D. A telemedicine model for abortion in South Africa: A randomised, controlled, non-inferiority trial. Lancet 2022, 400, 670–679. [Google Scholar] [CrossRef]
- Karajeanes, E.; Bila, D.; Luis, M.; Tovela, M.; Anjos, C.; Ramanlal, N.; Vaz, P.; Lapão, L.V. The Infomóvel—An information system for managing HIV/AIDS patients in rural areas of Mozambique. BMC Med. Inform. Decis. Mak. 2023, 23, 187. [Google Scholar] [CrossRef] [PubMed]
- Gold-Olufadi, S.; Jesuyajolu, D.; Cole-Adeife, O.; Emokpare, D.; Enigbokan, O. Teledermatology During the COVID-19 Pandemic in a Developing Country: Could This Be the Answer to Improving the Reach of Dermatology Care? Int. J. Dermatol. Venereol. 2023, 6, 141–146. [Google Scholar] [CrossRef]
- Onu, J.U.; Onyeka, T.C. Digital psychiatry in Nigeria: A scoping review. S. Afr. J. Psychiatry 2024, 30, 2115. [Google Scholar] [CrossRef] [PubMed]
- Ikwu, A.N.; Komolafe, D.T.; Ahaneku, G.I.; Nwawudu, S.E. Advancement of telemedicine in Africa and the current laws: A case study of Nigeria. Med.-Leg. J. 2021, 89, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Paul Jen-Hwa Hu, P.Y.K.C.; Sheng, O.R.L. Adoption of Telemedicine Technology by Health Care Organizations: An Exploratory Study. J. Organ. Comput. Electron. Commer. 2002, 12, 197–221. [Google Scholar] [CrossRef]
- Yang, L.; Zhang, H.; Shen, H.; Huang, X.; Zhou, X.; Rong, G.; Shao, D. Quality Assessment in Systematic Literature Reviews: A Software Engineering Perspective. Inf. Softw. Technol. 2021, 130, 106397. [Google Scholar] [CrossRef]
- Cilliers, L.; Flowerday, S. User Acceptance of Telemedicine by Health Care Workers A Case of the Eastern Cape Province, South Africa. Electron. J. Inf. Syst. Dev. Ctries. 2014, 65, 1–10. [Google Scholar] [CrossRef]
- Kwame Owusu Kwateng, O.D.L.; Amanor, K. A modified UTAUT2 for the study of telemedicine adoption. Int. J. Healthc. Manag. 2023, 16, 207–223. [Google Scholar] [CrossRef]
- Nyamu, J.; De Coster, R.; Taib, S.M. An empirical study of collaborative innovation as a facilitator to telemedicine adoption in developing countries. In Proceedings of the 2015 International Conference on Information Society (i-Society), Cambridge, UK, 25–27 August 2025; pp. 33–38. [Google Scholar] [CrossRef]
- Smillie, K.; Borek, N.V.; Kop, M.L.V.D.; Lukhwaro, A.; Li, N.; Karanja, S.; Patel, A.R.; Ojakaa, D.; Lester, R.T. Mobile health for early retention in HIV care: A qualitative study in Kenya (WelTel Retain). Afr. J. AIDS Res. 2014, 13, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Aria, M.; Cuccurullo, C. bibliometrix: An R-tool for comprehensive science mapping analysis. J. Inf. 2017, 11, 959–975. [Google Scholar] [CrossRef]
- Obi-Jeff, C.; Garcia, C.; Onuoha, O.; Adewumi, F.; David, W.; Bamiduro, T.; Aliyu, A.B.; Labrique, A.; Wonodi, C. Designing an SMS reminder intervention to improve vaccination uptake in Northern Nigeria: A qualitative study. Bmc Health Serv. Res. 2021, 21, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Itanyi, I.U.; Iwelunmor, J.; Olawepo, J.O.; Gbadamosi, S.; Ezeonu, A.; Okoli, A.; Ogidi, A.G.; Conserve, D.; Powell, B.; Onoka, C.A.; et al. Acceptability and user experiences of a patient-held smart card for antenatal services in Nigeria: A qualitative study. BMC Pregnancy Childbirth 2023, 23, 198. [Google Scholar] [CrossRef] [PubMed]
- Day, S.; Ncube, V.; Maja, L.; Wasunna, B.; Pienaar, J.; Setswe, G.; Waweru, E.; Feldacker, C. Centering Frontline Health Care Workers in Digital Innovation Design to Inform the Optimization of an App for Improved Male Circumcision Follow-up in South Africa: Qualitative Usability Study. JMIR Form. Res. 2023, 7, e44122. [Google Scholar] [CrossRef]
- Obi-Jeff, C.; Garcia, C.; Adewumi, F.; Bamiduro, T.; David, W.; Labrique, A.; Wonodi, C. Implementing SMS reminders for routine immunization in Northern Nigeria: A qualitative evaluation using the RE-AIM framework. BMC Public Health 2022, 22, 2370. [Google Scholar] [CrossRef]
- Morris, C.; Scott, R.E.; Mars, M. Towards ‘Formalising’ WhatsApp Teledermatology Practice in KZ-N District Hospitals: Key Informant Interviews. Int. J. Environ. Res. Public Health 2024, 21, 1388. [Google Scholar] [CrossRef]
- Hasselberg, M.; Lee Wallis, P.B.; Laflamme, L. A smartphone-based consultation system for acute burns—Methodological challenges related to follow-up of the system. Glob. Health Action 2017, 10, 1328168. [Google Scholar] [CrossRef] [PubMed]
- Owolabi, E.O.; Goon, D.T.; Ajayi, A.I. Efficacy, acceptability and feasibility of daily text-messaging in promoting glycaemic control and other clinical outcomes in a low-resource setting of South Africa: A randomised controlled trial. PLoS ONE 2019, 14, 1–17. [Google Scholar] [CrossRef]
- Blocker, A.; Oladokun, A.; Datay, M.I.; Mwangama, J.; Malila, B. Evaluating the Capability of 3G, 4G, and 5G Networks in Delivering a Virtual Clinic Solution. In Proceedings of the 2023 IEEE AFRICON, Nairobi, Kenya, 20–22 September 2023; pp. 1–6. [Google Scholar] [CrossRef]
- Olufunlayo, T.F.; Ojo, O.O.; Ozoh, O.B.; Agabi, O.P.; Opara, C.R.; Taiwo, F.T.; Fasanmade, O.A.; Okubadejo, N.U. Telemedicine ready or not? A cross-sectional assessment of telemedicine maturity of federally funded tertiary health institutions in Nigeria. Digit. Health 2023, 9, 20552076221150072. [Google Scholar] [CrossRef]
- Jarvis, M.A.; Padmanabhanunni, A.; Chipps, J. An Evaluation of a Low-Intensity Cognitive Behavioral Therapy mHealth-Supported Intervention to Reduce Loneliness in Older People. Int. J. Environ. Res. Public Health 2019, 16, 1305. [Google Scholar] [CrossRef]
- Bergam, S.; Sibaya, T.; Ndlela, N.; Kuzwayo, M.; Fomo, M.; Goldstein, M.H.; Marconi, V.C.; Haberer, J.E.; Archary, M.; Zanoni, B.C. “I am not shy anymore”: A qualitative study of the role of an interactive mHealth intervention on sexual health knowledge, attitudes, and behaviors of South African adolescents with perinatal HIV. Reprod. Health 2022, 19, 217. [Google Scholar] [CrossRef]
- Ronen, K.; Mugo, C.; Kaggiah, A.; Seeh, D.; Kumar, M.; Guthrie, B.L.; Moreno, M.A.; John-Stewart, G.; Inwani, I. Facilitated WhatsApp Support Groups for Youth Living With HIV in Nairobi, Kenya: Single-Arm Pilot Intervention Study. JMIR Form. Res. 2023, 7, e49174. [Google Scholar] [CrossRef] [PubMed]
- Zanoni, B.C.; Archary, M.; Sibaya, T.; Musinguzi, N.; Gethers, C.T.; Goldstein, M.; Bergam, S.; Psaros, C.; Marconi, V.C.; Haberer, J.E. Acceptability, feasibility and preliminary effectiveness of the mHealth intervention, InTSHA, on retention in care and viral suppression among adolescents with HIV in South Africa: A pilot randomized clinical trial. AIDS Care 2024, 36, 983–992. [Google Scholar] [CrossRef] [PubMed]
- Atujuna, M.; Simpson, N.; Ngobeni, M.; Monese, T.; Giovenco, D.; Pike, C.; Figerova, Z.; Visser, M.; Biriotti, M.; Kydd, A.; et al. Khuluma: Using Participatory, Peer-Led and Digital Methods to Deliver Psychosocial Support to Young People Living with HIV in South Africa. Front. Reprod. Health 2021, 3, 687677. [Google Scholar] [CrossRef]
- Aunon, F.M.; Wanje, G.; Richardson, B.A.; Masese, L.; Odeny, T.A.; Kinuthia, J.; Mandaliya, K.; Jaoko, W.; Simoni, J.M.; McClelland, R.S. Randomized controlled trial of a theory-informed mHealth intervention to support ART adherence and viral suppression among women with HIV in Mombasa, Kenya: Preliminary efficacy and participant-level feasibility and acceptability. BMC Public Health 2023, 23, 837. [Google Scholar] [CrossRef]
- Feldacker, C.; Pienaar, J.; Wasunna, B.; Ndebele, F.; Khumalo, C.; Day, S.; Tweya, H.; Oni, F.; Sardini, M.; Adhikary, B.; et al. Expanding the Evidence on the Safety and Efficiency of 2-Way Text Messaging–Based Telehealth for Voluntary Medical Male Circumcision Follow-up Compared with In-Person Reviews: Randomized Controlled Trial in Rural and Urban South Africa. J. Med. Internet Res. 2023, 25, e42111. [Google Scholar] [CrossRef]
- Harrington, E.K.; Drake, A.L.; Matemo, D.; Ronen, K.; Osoti, A.O.; John-Stewart, G.; Kinuthia, J.; Unger, J.A. An mHealth SMS intervention on Postpartum Contraceptive Use Among Women and Couples in Kenya: A Randomized Controlled Trial. Am. J. Public Health 2019, 109, 934–941. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.; Juras, R.; Riley, P.; Chatterji, M.; Sloane, P.; Choi, S.K.; Johns, B. A randomized controlled trial of the impact of a family planning mHealth service on knowledge and use of contraception. Contraception 2017, 95, 90–97. [Google Scholar] [CrossRef]
- Zunza, M.; Cotton, M.F.; Mbuagbaw, L.; Lester, R.; Thabane, L. Interactive weekly mobile phone text messaging plus motivational interviewing in promotion of breastfeeding among women living with HIV in South Africa: Study protocol for a randomized controlled trial. Trials 2017, 18, 1–8. [Google Scholar] [CrossRef]
- Adam, M.; Kwinda, Z.; Dronavalli, M.; Leonard, E.; Nguyen, V.K.; Tshivhase, V.; Bärnighausen, T.; Pillay, Y. Effect of Short, Animated Video Storytelling on Maternal Knowledge and Satisfaction in the Perinatal Period in South Africa: Randomized Controlled Trial. J. Med. Internet Res. 2023, 25, e47266. [Google Scholar] [CrossRef]
- Constant, D.; Katherine de Tolly, J.H.; Myer, L. Assessment of completion of early medical abortion using a text questionnaire on mobile phones compared to a self-administered paper questionnaire among women attending four clinics, Cape Town, South Africa. Reprod. Health Matters 2014, 22, 83–93. [Google Scholar] [CrossRef]
- Iliyasu, Z.; Garba, R.M.; Bashir, H.A.; Saleh, N.S.; Jibo, A.M.; Amole, T.G.; Umar, A.A.; Tsiga-Ahmed, F.I.; Abdullahi, H.M.; Kwaku, A.A.; et al. Telemedicine Service Adoption During the COVID-19 Pandemic: Physicians’ Experience from Nigeria. Telemed. e-Health 2024, 30, 805–815. [Google Scholar] [CrossRef] [PubMed]
- Sarna, A.; Saraswati, L.R.; Okal, J.; Matheka, J.; Owuor, D.; Singh, R.J.; Reynolds, N.; Kalibala, S. Cell Phone Counseling Improves Retention of Mothers with HIV Infection in Care and Infant HIV Testing in Kisumu, Kenya: A Randomized Controlled Study. Glob. Health Sci. Pract. 2019, 7, 171–188. [Google Scholar] [CrossRef] [PubMed]
- Dulli, L.; Ridgeway, K.; Packer, C.; Murray, K.R.; Mumuni, T.; Plourde, K.F.; Chen, M.; Olumide, A.; Ojengbede, O.; McCarraher, D.R. A Social Media–Based Support Group for Youth Living with HIV in Nigeria (SMART Connections): Randomized Controlled Trial. J. Med. Internet Res. 2020, 22, e18343. [Google Scholar] [CrossRef] [PubMed]
- Vedanthan, R.; Kamano, J.H.; DeLong, A.K.; Naanyu, V.; Binanay, C.A.; Bloomfield, G.S.; Chrysanthopoulou, S.A.; Finkelstein, E.A.; Hogan, J.W.; Horowitz, C.R.; et al. Community Health Workers Improve Linkage to Hypertension Care in Western Kenya. J. Am. Coll. Cardiol. 2019, 74, 1897–1906. [Google Scholar] [CrossRef]
- Piotie, P.N.; Wood, P.; Webb, E.M.; Hugo, J.F.; Rheeder, P. Designing an integrated, nurse-driven and home-based digital intervention to improve insulin management in under-resourced settings. Ther. Adv. Endocrinol. Metab. 2021, 12, 20420188211054688. [Google Scholar] [CrossRef] [PubMed]
- Amoakoh, H.B.; Klipstein-Grobusch, K.; Agyepong, I.A.; Amoakoh-Coleman, M.; Kayode, G.A.; Reitsma, J.B.; Grobbee, D.E.; Ansah, E.K. Can an mhealth clinical decision-making support system improve adherence to neonatal healthcare protocols in a low-resource setting? BMC Pediatr. 2020, 20, 1–13. [Google Scholar] [CrossRef]
- Lodhia, V.; Karanja, S.; Lees, S.; Bastawrous, A. Acceptability, Usability, and Views on Deployment of Peek, a Mobile Phone mHealth Intervention for Eye Care in Kenya: Qualitative Study. JMIR mHealth uHealth 2016, 4, e30. [Google Scholar] [CrossRef]
- Harder, V.S.; Musau, A.M.; Musyimi, C.W.; Ndetei, D.M.; Mutiso, V.N. A randomized clinical trial of mobile phone motivational interviewing for alcohol use problems in Kenya. Addiction 2020, 115, 1050–1060. [Google Scholar] [CrossRef]
- Kurth, A.E.; Sidle, J.E.; Chhun, N.; Lizcano, J.A.; Macharia, S.M.; Garcia, M.M.; Mwangi, A.; Keter, A.; Siika, A.M. Computer-Based Counseling Program (CARE+ Kenya) to Promote Prevention and HIV Health for People Living with HIV/AIDS: A Randomized Controlled Trial. AIDS Educ. Prev. 2019, 31, 395–406. [Google Scholar] [CrossRef] [PubMed]
- Stocks, J.; Choi, Y.; Ibrahim, S.; Huchko, M. Iterative Development of a Mobile Phone App to Support Community Health Volunteers During Cervical Cancer Screening in Western Kenya: Qualitative Study. JMIR Form. Res. 2022, 6, e27501. [Google Scholar] [CrossRef]
- Pillay, L.; Govender, R.; Pillay, S. Doctor-perceived-barriers to telephone clinics at KwaZulu-Natal hospitals during the COVID-19 pandemic. S. Afr. Fam. Pract. 2021, 63, 6. [Google Scholar] [CrossRef] [PubMed]
- Salako, O.; Robert, A.A.; Okunade, K.S.; Olatunji, A.; Fakolade, A.; Isibor, V.; Falode, D. Utilization of cancer information system for breast cancer control in Lagos, Nigeria. Pan Afr. Med. J. 2016, 24, 323. [Google Scholar] [CrossRef] [PubMed]
- Balikuddembe, J.K.; Reinhardt, J.D. Can Digitization of Health Care Help Low-Resourced Countries Provide Better Community-Based Rehabilitation Services? Phys. Ther. 2019, 100, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Sumbana, V.; Dandadzi, T.A.; Nkobeni, L.M.; Ndobe, T.V.; Seeletse, S.M. The potential value of e-health in a rural Limpopo Province municipality. Int. J. Res. Bus. Soc. Sci. 2024, 13, 507–514. [Google Scholar] [CrossRef]
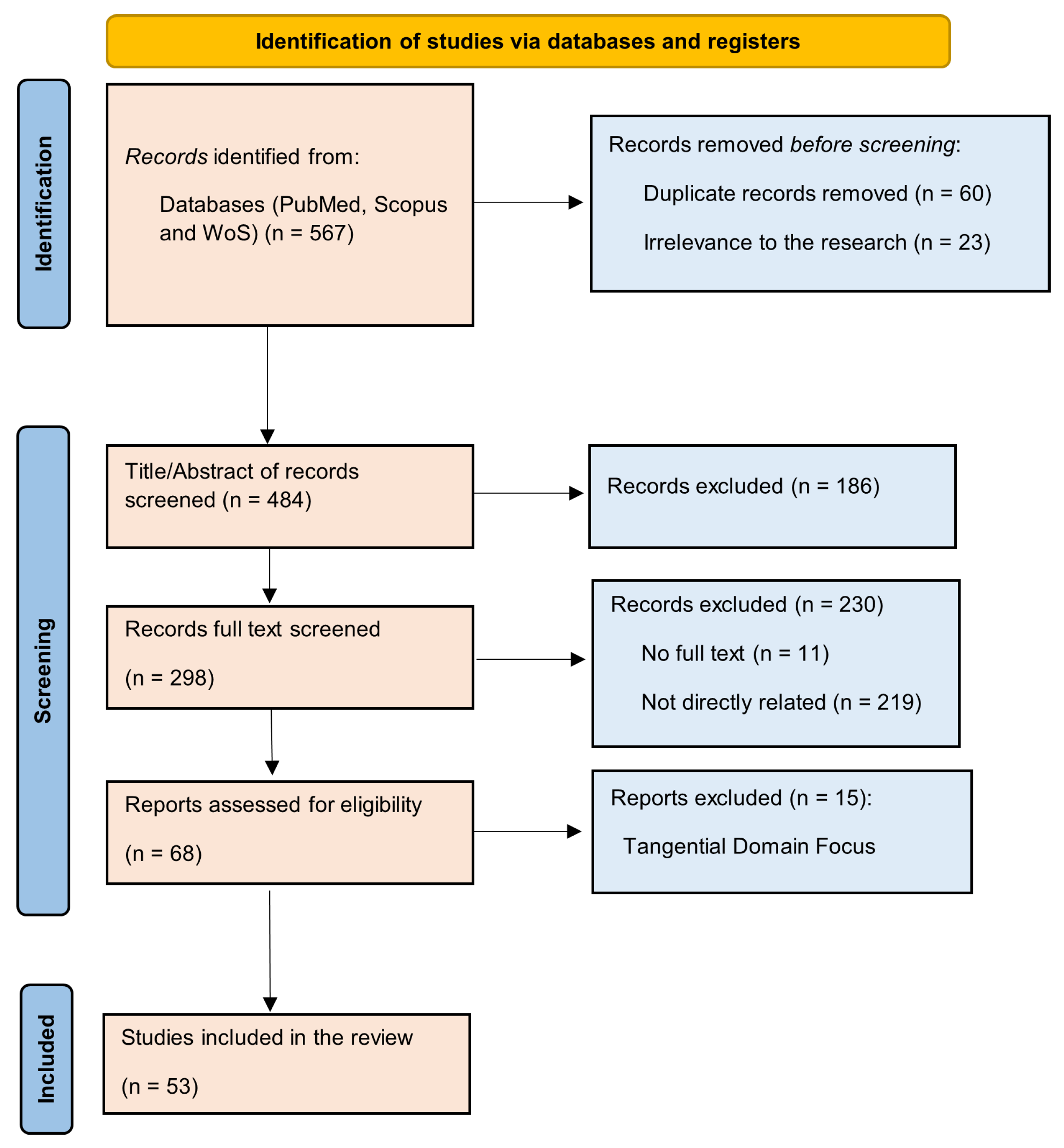

| Code | Exclusion Criteria Description | Number of Studies |
|---|---|---|
| DR | Duplicates removed to eliminate redundancy. | 60 |
| LA | Excluded editorials, reviews, trial protocols, and similar others. | 23 |
| US | Excluded studies that did not focus on telemedicine, digital health technologies, or healthcare delivery in the specified countries. | 186 |
| IST | Excluded articles that did not address telemedicine’s adoption, implementation, or technological aspects and those without the full text. | 230 |
| GM | Excluded studies focusing on regions outside Sub-Saharan Africa or countries other than South Africa, Kenya, and Nigeria. | 15 |
| Criterion | Inclusion | Exclusion | Justification | Examples |
|---|---|---|---|---|
| Population | Healthcare providers, patients, or policymakers in telemedicine interventions. | Studies not involving the target population. | Focuses on stakeholders directly impacted by telemedicine. | Inclusion: Blocker et al. [33]; Exclusion: Opoku et al. [34]. |
| Context | Studies on telemedicine adoption, implementation, or policy in healthcare. | Non-healthcare sectors or unrelated contexts. | Ensures relevance to the review’s scope. | Inclusion: Adenuga et al. [35]; Exclusion: Patel et al. [36]. |
| Concept | Telemedicine, telehealth, mHealth, or digital health technologies. | Tangential focus on non-healthcare domains. | Aligns with objectives on telemedicine technologies. | Inclusion: Gbadamosi et al. [37]; Exclusion: Barteit et al. [38]. |
| Language | Articles in English. | Non-English publications. | Ensures easy accessibility without translation. | Inclusion: Blocker et al. [33]; Exclusion: Ferre et al. [39]. |
| Geographic Focus | Sub-Saharan Africa and within South Africa, Kenya, and Nigeria. | Regions outside the specified geographic focus. | Maintains regional specificity. | Inclusion: Endler et al. [40]; Exclusion: Karajeanes et al. [41]. |
| Type of Source | Peer-reviewed articles, technical studies, or full-text publications. | Editorials, letters, reviews, or unavailable full texts. | Emphasises methodologically robust studies. | Inclusion: Gold-Olufadi et al. [42]; Exclusion: Onu and Onyeka [43]. |
| Publication Timeline | Published between 2014 and 2024. | Articles published before 2014. | Captures recent advancements in telemedicine. | Inclusion: Ikwu et al. [44]; Exclusion: Hu et al. [45]. |
| RQ | Description | Total Studies/Sample |
|---|---|---|
| RQ1 | Studies addressing research question 1 | 10 (Kwateng et al. [48], Nyamu et al. [49], …) |
| RQ2 | Studies addressing research question 2 | 11 (Endler et al. [40], Gbadamosi et al. [37], …) |
| RQ3 | Studies addressing research question 3 | 32 (Blocker et al. [33], Macharia et al. [6], …) |
| Study | Year | Country | Technology Platform | Target Population | Enablers | Adoption Level | Prospect |
|---|---|---|---|---|---|---|---|
| Day et al. [54] | 2023 | South Africa | Text message (SMS) | Healthcare providers | Digital infrastructure, healthcare readiness, provider engagement | Moderate | Improved access, cost-effectiveness, scalability |
| Morris et al. [56] | 2024 | South Africa | Healthcare providers | Digital infrastructure, system readiness, provider competency | Moderate | Healthcare accessibility, efficiency, service quality | |
| Blocker et al. [59] | 2023 | South Africa | Microsoft Teams | Patients | Infrastructure reliability, digital competency, system readiness | Moderate | Healthcare accessibility, infrastructure development, service adaptation |
| Obi-Jeff et al. [52] | 2021 | Nigeria | Mobile health application (IRISS) | Caregivers and parents | Digital access, literacy barriers, community engagement | Low | Healthcare outreach, community engagement, immunisation adherence |
| Udenigwe et al. [25] | 2022 | Nigeria | Text message (SMS) | Patients and healthcare providers | Community acceptance, user engagement, healthcare access | High | Healthcare access, maternal outcomes, service utilisation |
| Itanyi et al. [53] | 2023 | Nigeria | Integrated mobile health platform | Patients | Healthcare support, digital literacy, technology acceptance | Moderate | Healthcare accessibility, maternal care |
| Meffert et al. [16] | 2024 | Kenya | mHealth (audio-only mobile phone) | Patients | Digital accessibility, service delivery | Moderate | Healthcare access, cost-effectiveness |
| Smillie et al. [50] | 2014 | Kenya | mHealth (WelTel text) | Patients | Digital access, cost-efficiency | High | Patient engagement, care continuity, stigma reduction |
| Obi-Jeff et al. [55] | 2022 | Nigeria | mHealth (SMS Reminder System) | Patients | Community engagement, healthcare workforce, infrastructure development | Moderate | Healthcare outreach, immunisation adherence, service access |
| Onyeabor et al. [26] | 2024 | Nigeria | Web-based App | Patients | Healthcare access, digital solutions, patient engagement | Low | Healthcare accessibility, cost-effectiveness, system resilience |
| Study | Year | Country | Focus | Intervention | Adoption Level | Challenges |
|---|---|---|---|---|---|---|
| Mash et al. [19] | 2022 | South Africa | Diabetes management | mHealth (WhatsApp Chatbot) | Moderate | Digital Literacy, Infrastructure Issues, Technical Challenges, Sustainable Engagement. |
| Khan et al. [15] | 2022 | Nigeria | Endocrinology | Teleconsultation (video) | Moderate | Infrastructure Limitations, Digital Literacy, Data Protection and Privacy Concerns. |
| Harder et al. [80] | 2020 | Kenya | Mental health (AUDs) | mHealth (phone calls) | Moderate | Infrastructure barriers, literacy gaps, social stigma. |
| Sarna et al. [74] | 2019 | Kenya | Maternal health (PMTCT) | mHealth (phone calls) | High | Access barriers, contact challenges, scheduling limitations. |
| Owolabi et al. [58] | 2019 | South Africa | Diabetes management | mHealth (text messaging) | High | Digital barriers, literacy gaps, socioeconomic challenges |
| Hasselberg et al. [57] | 2017 | South Africa | Acute burns | Teleconsultation (Smartphone app) | Moderate | Infrastructure barriers, digital competency, resource constraints |
| Jarvis et al. [61] | 2019 | South Africa | Mental health (LI-CBT) | mHealth (WhatsApp) | Low | Technology barriers, participant retention, digital literacy. |
| Akande et al. [4] | 2024 | Nigeria | Sexual and reproductive health (SRH) | Web-based App | High | Privacy concerns, access barriers, socioeconomic factors. |
| Adam et al. [71] | 2023 | South Africa | Maternal health | mHealth (SAS videos) | High | Technology access, digital literacy, infrastructure barriers. |
| Lalla-Edward et al. [13] | 2022 | South Africa | HIV care | mHealth (mobile App) | High | Access barriers, technical limitations, connectivity issues. |
| Zunza et al. [70] | 2017 | South Africa | Maternal health | mHealth (text messaging) | Moderate | Healthcare resources, provider training, participant engagement. |
| Johnson et al. [69] | 2017 | Kenya | Family planning and reproductive health | mHealth (text messaging) | Moderate | Demographic bias, evaluation barriers. |
| Davies et al. [17] | 2021 | South Africa | Paediatric epilepsy | Wearable devices & App | Moderate | Technology access, security concerns, literacy barriers |
| Constant et al. [72] | 2014 | South Africa | Maternal health | mHealth (chat application & USSD) | Moderate | Digital literacy, infrastructure reliability. |
| Bobrow et al. [14] | 2014 | South Africa | Hypertension management | mHealth (SMS) | Moderate | Limited engagement, digital literacy. |
| Macharia et al. [6] | 2022 | Kenya | Sexual reproductive health (SRH) | mHealth (USSD-based app) | Moderate | Economic barriers, Privacy concerns, Digital literacy. |
| Janssen et al. [5] | 2020 | South Africa | HIV care | mHealth (mobile App) | Moderate | Technology access, literacy barriers, security concerns. |
| Ochieng et al. [20] | 2024 | Kenya | Maternal, newborn, and child health (MNCH) | AI-enabled SMS-based platform | High | Infrastructure, digital literacy, stakeholder engagement. |
| Atujuna et al. [65] | 2021 | South Africa | HIV care | mHealth (SMS) | Moderate | Infrastructure barriers, access limitations, digital literacy |
| Blocker 2024 [33] | 2024 | South Africa | Primary healthcare | Virtual clinic system (web-based app) | Moderate | Infrastructure barriers, digital literacy, implementation challenges. |
| Kurth et al. [81] | 2019 | Kenya | HIV care | mHealth (mobile App) | High | Infrastructure barriers, stigma concerns, provider resistance. |
| Zanoni et al. [64] | 2024 | South Africa | HIV care | mHealth (WhatsApp) | Moderate | Technology barriers, attendance challenges, infrastructure issues. |
| Piotie et al. [77] | 2021 | South Africa | Diabetes management | mobile App | Moderate | Infrastructure barriers, provider resistance, resource limitations. |
| Harrington et al. [68] | 2019 | Kenya | Maternal health | mHealth (SMS) | High | Partner engagement, recruitment challenges, reporting bias. |
| Dulli et al. [75] | 2020 | Nigeria | HIV care | Social media (Facebook) | High | Digital literacy, Supportive infrastructure. |
| Vedanthan et al. [76] | 2019 | Kenya | Hypertension care | mHealth (mobile App) | Moderate | Demographic inconsistencies, Economic barriers, Lack of health insurance. |
| Bergam et al. [62] | 2019 | South Africa | HIV care | mHealth (WhatsApp) | High | Technology access, digital literacy, connectivity barriers. |
| Feldacker at al. [67] | 2023 | South Africa | Voluntary medical male circumcision (VMMC) | mHealth (SMS) | Moderate | Technology barriers, provider literacy, patient confidence. |
| Lodhia et al. [79] | 2016 | Kenya | Ophthalmic health | mHealth (mobile App) | Moderate | Infrastructure barriers, digital literacy, sustainability challenges. |
| Gold-Olufadi et al. [42] | 2023 | Nigeria | Dermatology care | Teledermatology (WhatsApp) | Moderate | Infrastructure barriers, awareness gaps, cost limitations |
| Ronen et al. [63] | 2023 | Kenya | HIV care | mHealth (WhatsApp) | High | Technology access, digital literacy, implementation barriers |
| Aunon et al. [66] | 2023 | Kenya | HIV care | mHealth (SMS) | High | Technology access, recruitment barriers, literacy gaps |
| Study | Year | Country | Policy Focus | Socioeconomic Factors | Equity Considerations | Challenges | Recommendations |
|---|---|---|---|---|---|---|---|
| Pillay et al. [83] | 2021 | South Africa | Health Professions Council of South Africa (HPCSA) telemedicine guidelines | Affordability, digital literacy, infrastructure access | Yes (rural and underserved communities, low-income populations, and ethnic and linguistic minorities) | Infrastructure costs, technology access, digital literacy | Policy reforms. |
| Ikwu et al. [44] | 2021 | Nigeria | No | Affordability, digital literacy, inadequate infrastructure | Yes (rural and underserved communities) | No regulation, network issue, electricity issue, cultural beliefs | Legislation and advocacy. |
| Endler et al. [40] | 2022 | South Africa | No | Affordability, digital literacy, access to technology | Yes (women, low-income populations, ethnic and linguistic minorities, rural and underserved communities) | Digital access, literacy barriers, systemic constraints | Guided self-assessment protocols. |
| Gbadamosi et al. [37] | 2018 | Nigeria | No | Affordability, digital literacy, internet connectivity, health infrastructure | Yes (rural and underserved communities, low-income populations, and women) | Lack of reliable internet connectivity, affordability of technology, digital literacy, inadequate health infrastructure, and policy constraints | Integrated mHealth platforms. |
| Stocks et al. [82] | 2022 | Kenya | No | Affordability, digital literacy, and infrastructure | Yes (rural and underserved communities, low-income populations, and ethnic and linguistic minorities) | Infrastructure, financial resources, inadequate training and support | Context-specific development. |
| Salako et al. [84] | 2016 | Nigeria | No | Affordability, digital literacy, and infrastructure | Yes (rural and underserved communities) | Socioeconomic status, technology adoption, system integration | Public awareness programs. |
| Nyamu et al. [49] | 2015 | Kenya | No | Affordability, digital literacy, ICT infrastructure, and economic levels | Yes (rural and underserved communities) | Infrastructure limitations, cost barriers, resource scarcity | Organisational collaboration. |
| Onsongo et al. [28] | 2023 | Kenya | No | Infrastructure costs, digital literacy, resource limitations | Yes (rural and underserved communities, low-income populations, elderly populations, and people living with chronic disease) | Infrastructure limitations, provider readiness, regulatory gaps | Policy reform. |
| Olufunlayo et al. [60] | 2023 | Nigeria | No | Affordability, inadequate infrastructure, and digital literacy | Yes (rural and underserved communities, low-income populations, and elderly populations) | Infrastructure gaps, funding limitations, regulatory constraints | Policy reforms and capacity building. |
| Adenuga et al. [35] | 2017 | Nigeria | No | Affordability, digital literacy, and infrastructure | Yes (rural and underserved communities, low-income populations, and people living with chronic diseases) | Lack of reimbursement policy, erratic internet connectivity, and inadequate infrastructure | Reimbursement policy. |
| Cilliers and Flowerday [47] | 2014 | South Africa | No | Access to technology, digital literacy, affordability | Yes (rural and underserved communities) | Unreliable electricity supply, poor internet connectivity, digital literacy | Education and training. |
| Aspect | South Africa | Kenya | Nigeria |
|---|---|---|---|
| Policy Frameworks | Existing telemedicine guidelines (HPCSA) require updates for modern integration | No formal national policy; regulatory gaps hinder large-scale adoption | Absence of a national framework; weak enforcement mechanisms |
| Equity and Access | Digital divide remains a challenge, particularly in rural areas | High costs and limited access to technology restrict widespread adoption | Socioeconomic disparities and infrastructure gaps limit equitable access |
| Infrastructure | Fair internet coverage, but connectivity issues persist in underserved areas | Unstable power supply and limited broadband availability | Poor network coverage and frequent power outages hinder telemedicine adoption |
| Private Sector Role | Private investment is increasing, but policy gaps restrict full-scale expansion | Limited private sector engagement; greater public–private partnerships needed | Some government-backed initiatives exist, but long-term sustainability is uncertain |
| Digital Literacy | Inadequate digital literacy among healthcare providers and users | Insufficient digital skills impede telemedicine adoption | Limited digital literacy remains a key barrier to implementation |
| Economic Factors | Telemedicine costs vary; affordability remains a barrier for low-income populations | High data and device costs limit adoption, particularly in rural communities | High mobile data costs and limited financial incentives slow adoption |
| Opportunities | Policy reforms, digital incentives, and improved connectivity could drive expansion | Government support, mHealth integration, and USSD-based solutions offer potential | Strengthened public–private partnerships could enhance access and sustainability |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agbeyangi, A.O.; Lukose, J.M. Telemedicine Adoption and Prospects in Sub-Sahara Africa: A Systematic Review with a Focus on South Africa, Kenya, and Nigeria. Healthcare 2025, 13, 762. https://doi.org/10.3390/healthcare13070762
Agbeyangi AO, Lukose JM. Telemedicine Adoption and Prospects in Sub-Sahara Africa: A Systematic Review with a Focus on South Africa, Kenya, and Nigeria. Healthcare. 2025; 13(7):762. https://doi.org/10.3390/healthcare13070762
Chicago/Turabian StyleAgbeyangi, Abayomi O., and Jose M. Lukose. 2025. "Telemedicine Adoption and Prospects in Sub-Sahara Africa: A Systematic Review with a Focus on South Africa, Kenya, and Nigeria" Healthcare 13, no. 7: 762. https://doi.org/10.3390/healthcare13070762
APA StyleAgbeyangi, A. O., & Lukose, J. M. (2025). Telemedicine Adoption and Prospects in Sub-Sahara Africa: A Systematic Review with a Focus on South Africa, Kenya, and Nigeria. Healthcare, 13(7), 762. https://doi.org/10.3390/healthcare13070762








