Design, Implementation, and Evaluation of Healthcare Visual Map Tool for Health Workers to Improve Quality of Life of Home Care Patients: Study Protocol
Abstract
1. Introduction
2. Materials and Methods
2.1. Aim of Study
- Develop a visual map to be integrated into EMRs, ensuring that it effectively organizes and prioritizes key patient health information.
- Assess the effectiveness of the visual map in improving patient safety and care coordination through a cluster-randomized clinical trial conducted in primary care centers in the countryside of Tarragona, Spain.
- Explore healthcare professionals’ perceptions of the visual map’s impact on home care practices through a qualitative study, identifying strengths, challenges, and areas for improvement.
2.2. Setting of the Study
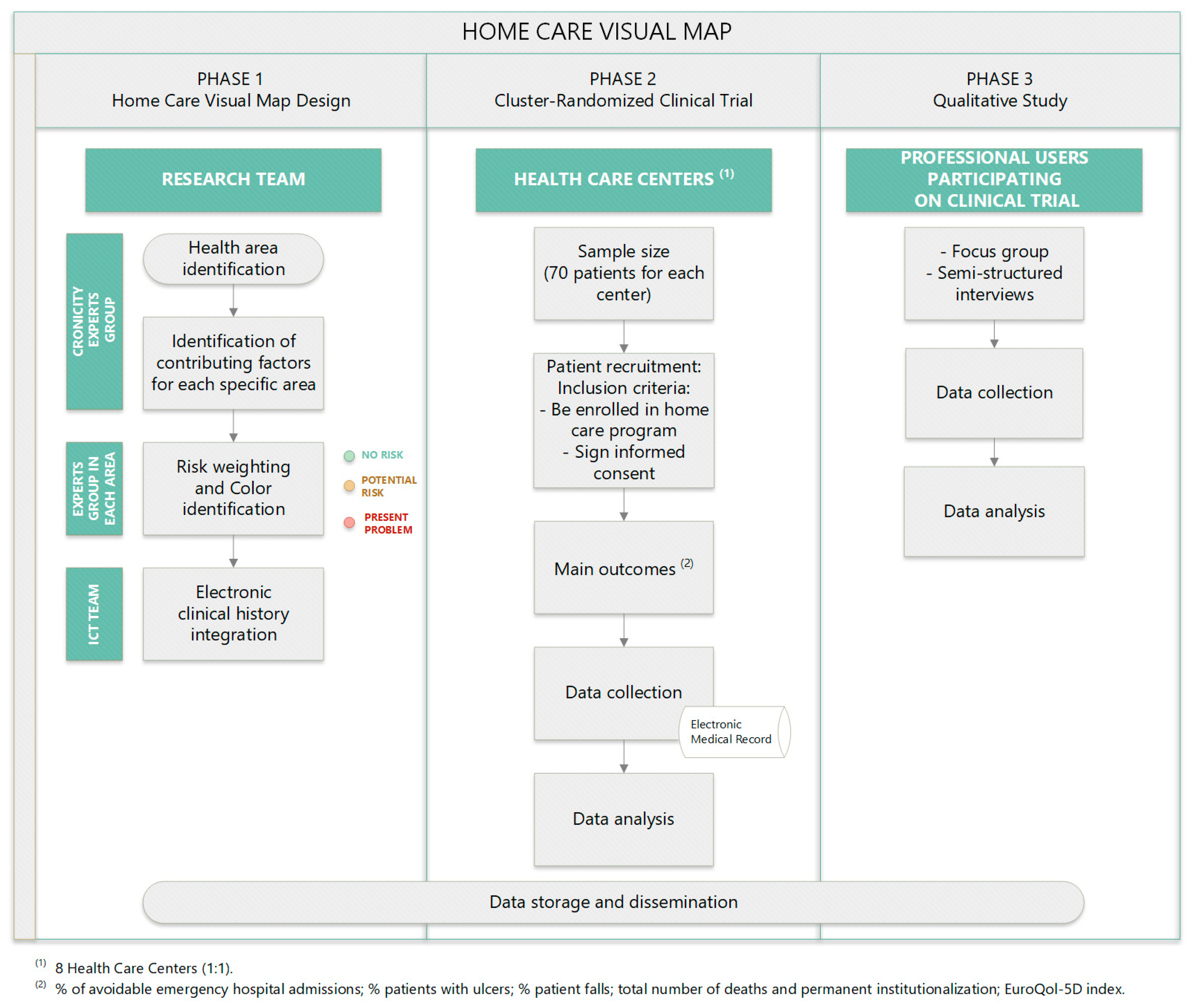
2.3. Study Development
- Phase (1): the design of the visual map included in the home care program.
- Phase (2): a cluster-randomized clinical trial across different primary care centers in the countryside of Tarragona, Spain.
- Phase (3): a qualitative study to evaluate the impact of the visual map’s implementation in the home care program by healthcare professionals.
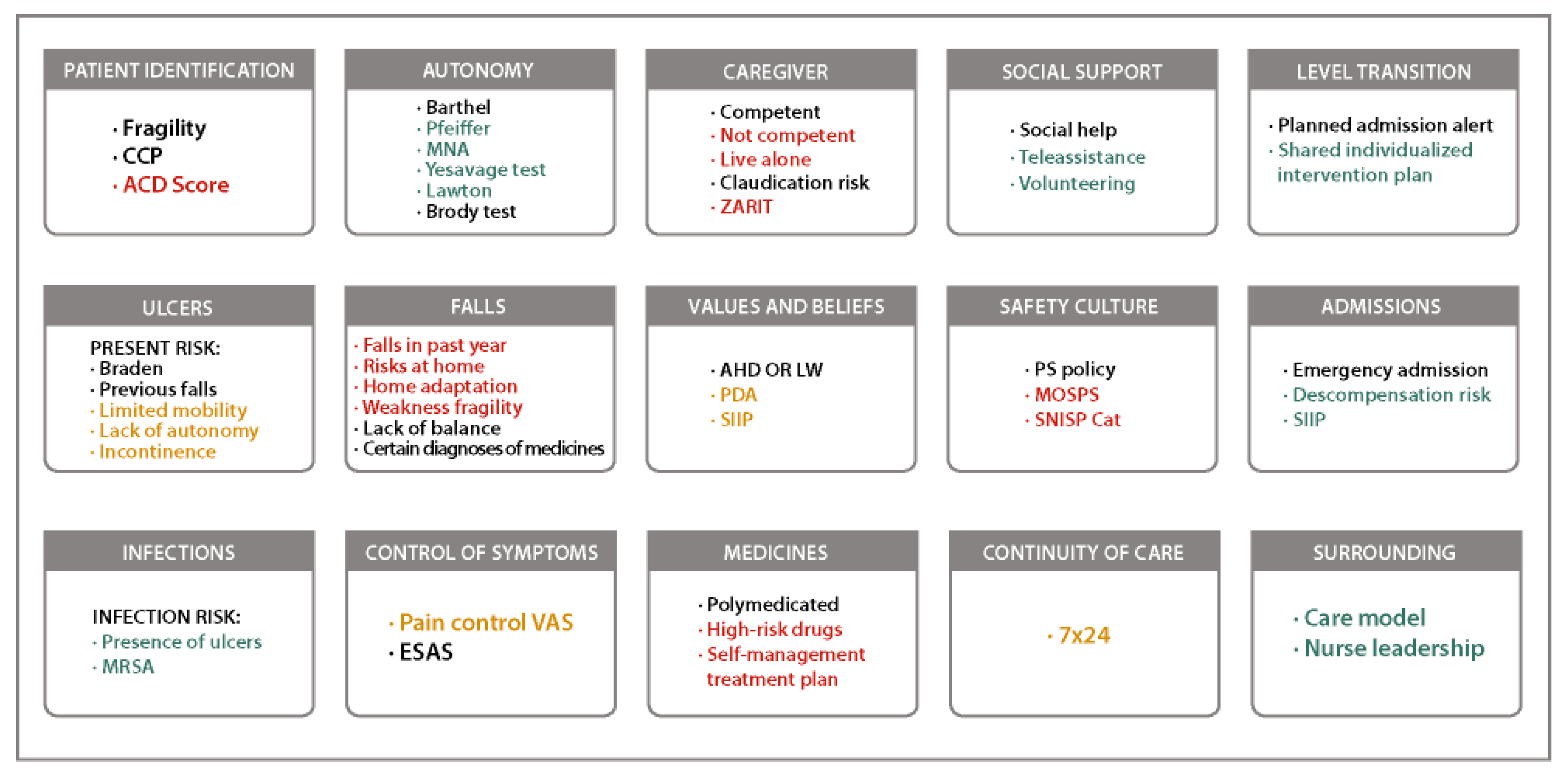
2.3.1. Phase 1: Design of Home Care Visual Map
- Identification of health areas and their contributing factors
- 2.
- Risk weighting with a group of experts
2.3.2. Phase 2: Cluster-Randomized Clinical Trial Across Different Primary Care Centers in Countryside of Tarragona, Spain
Sample Size
Recruitment
Variables
- The proportion of patients with hospital admissions and avoidable hospital emergency visits (main variable) during the follow-up period.
- The percentage of patients with ulcers and falls.
- The total number of avoidable admissions and hospital emergency visits during the follow-up period.
- The total number of deaths and definitive institutionalizations.
- Quality of life, measured using the EuroQol-5D index, a record currently available in EMRs [22].
Data Collection and Sources of Information
Data Analysis
2.3.3. Phase 3: Qualitative Study
Design
Participants
Data Collection and Resources
Data Analysis
Data Storage and Dissemination
3. Expected Results
- Phase 1: Development of Home Care Visual Map
- Phase 2: A clinical trial to assess the effectiveness of the Visual Map
- Phase 3: Understanding the experience of healthcare professionals
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AE | Adverse event |
| EMR | Electronic medical record |
| HCN | Home care nurses |
References
- Eurostat. Mortality and Life Expectancy Statistics. Eurostat 2024. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Mortality_and_life_expectancy_statistics (accessed on 23 May 2024).
- Instituto Nacional de Estadística. Notas de Prensa. Proyecciones de Población. 2018. Available online: https://www.ine.es/prensa/pp_2022_2072.pdf (accessed on 19 January 2023).
- Enquesta de Salut de Catalunya (ESCA). 2021. Available online: https://salutweb.gencat.cat/ca/el_departament/estadistiques_sanitaries/enquestes/esca/resultats_enquesta_salut_catalunya/ (accessed on 17 January 2023).
- Generalitat de Catalunya, Departament de Salut. Bases Conceptuals i Model D’atenció per a les Persones Fràgils, amb Cronicitat complexa (PCC) o Avançada (MACA); Generalitat de Catalunya: Barcelona, Spain, 2020. [Google Scholar]
- Cegri-Lombardo, F.; Aranzana-Martínez, A. Atención domiciliaria: Caminando hacia la excelencia [Home care: Walking towards excellence]. Aten. Primaria 2007, 39, 3–4. [Google Scholar] [CrossRef] [PubMed]
- Stall, N.; Nowaczynski, M.; Sinha, S.K. Systematic review of outcomes from home-based primary care programs for homebound older adults. J. Am. Geriatr. Soc. 2014, 62, 2243–2251. [Google Scholar] [CrossRef] [PubMed]
- Vincent, C.; René, A. Seguridad del Paciente. Estrategias para una atención sanitaria más segura, 1st ed.; Ed. Modus Laborandi: Madrid, Spain, 2016; pp. 1–271. [Google Scholar]
- Dowding, D.; Russell, D.; Trifilio, M.; McDonald, M.V.; Shang, J. Home care nurses’ identification of patients at risk of infection and their risk mitigation strategies: A qualitative interview study. Int. J. Nurs. Stud. 2020, 107, 103617. [Google Scholar] [CrossRef] [PubMed]
- Generalitat de Catalunya, Departament de Salut. Model del Programa D’atenció Domiciliària (ATDOM) de L’atenció Primària i Comunitària (APiC); Generalitat de Catalunya: Barcelona, Spain, 2022. [Google Scholar]
- Schildmeijer, K.G.I.; Unbeck, M.; Ekstedt, M.; Lindblad, M.; Nilsson, L. Adverse events in patients in home healthcare: A retrospective record review using trigger tool methodology. BMJ Open 2018, 8, e019267. [Google Scholar] [CrossRef]
- Masotti, P.; McColl, M.A.; Green, M. Adverse events experienced by homecare patients: A scoping review of the literature. Int. J. Qual. Health Care 2010, 22, 115–125. [Google Scholar] [CrossRef]
- Blais, R.; Sears, N.A.; Doran, D.; Baker, G.R.; Macdonald, M.; Mitchell, L.; Thalès, S. Assessing adverse events among home care clients in three Canadian provinces using chart review. BMJ Qual. Saf. 2013, 22, 989–997. [Google Scholar] [CrossRef]
- Sterling, M.R.; Lau, J.; Rajan, M.; Safford, M.M.; Akinyelure, O.P.; Kern, L.M. Self-reported gaps in care coordination and preventable adverse outcomes among older adults receiving home health care. J. Am. Geriatr. Soc. 2023, 71, 810–820. [Google Scholar] [CrossRef]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.M.; Lamb, S.E. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2012, 2012, CD007146. [Google Scholar] [CrossRef]
- Racey, M.; Ali, M.U.; Sherifali, D.; Fitzpatrick-Lewis, D.; Lewis, R.; Jovkovic, M.; Bouchard, D.R.; Giguère, A.; Holroyd-Leduc, J.; Tang, A.; et al. Effectiveness of physical activity interventions in older adults with frailty or prefrailty: A systematic review and meta-analysis. CMAJ Open 2021, 9, E728–E743. [Google Scholar] [CrossRef]
- Baker, G.R.; Flintoft, V.; Wojtak, A.; Blais, R. Contributing causes to adverse events in home care and potential interventions to reduce their incidence. Healthc. Manag. Forum 2018, 31, 178–185. [Google Scholar] [CrossRef]
- Bousquet, J.; Farrell, J.; Crooks, G.; Hellings, P.; Bel, E.H.; Bewick, M.; Chavannes, N.H.; de Sousa, J.C.; Cruz, A.A.; Haahtela, T.; et al. Scaling up strategies of the chronic respiratory disease programme of the European Innovation Partnership on Active and Healthy Ageing (Action Plan B3: Area 5). Clin. Transl. Allergy 2016, 6, 29. [Google Scholar] [CrossRef]
- Romera, L.; Orfila, F.; Segura, J.M.; Ramirez, A.; Möller, M.; Fabra, M.L.; Lancho, S.; Bastida, N.; Foz, G.; Fabregat, M.A.; et al. Effectiveness of a primary care based multifactorial intervention to improve frailty parameters in the elderly: A randomised clinical trial: Rationale and study design. BMC Geriatr. 2014, 14, 125. [Google Scholar] [CrossRef] [PubMed]
- NHS England. Proactive Care: Providing Care and Support for People Living at Home with Moderate or Severe Frailty; NHS England: England, UK, 2023. [Google Scholar]
- Langenberger, B.; Baier, N.; Hanke, F.C.; Fahrentholz, J.; Gorny, C.; Sehlen, S.; Reber, K.C.; Liersch, S.; Radomski, R.; Haftenberger, J.; et al. The detection and prevention of adverse drug events in nursing home and home care patients: Study protocol of a quasi-experimental study. Nurs. Open 2022, 9, 1477–1485. [Google Scholar] [CrossRef] [PubMed]
- Dubuc, N.; Brière, S.; Corbin, C.; N’Bouke, A.; Bonin, L.; Delli-Colli, N. Computerized Care-Pathways (CCPs) System to Support Person-Centered, Integrated, and Proactive Care in Home-Care Settings. Inform. Health Soc. Care 2021, 46, 100–111. [Google Scholar] [CrossRef]
- Herdman, M.; Badia, X.; Berra, S. El EuroQol-5D: Una alternativa sencilla para la medición de la calidad de vida relacionada con la salud en atención primaria [EuroQol-5D: A simple alternative for measuring health-related quality of life in primary care]. Aten. Primaria 2001, 28, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Cabrera, D.; Menéndez, A.; Fernández, A.; Acebal, V.; García, J.V.; Díaz, E.; García, A.S. Evaluación de la fiabilidad y validez de una escala de valoración social en el anciano. Aten. Primaria 1999, 23, 434–440. [Google Scholar]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.-M.; Sundararajan, V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2009, 95, 103208. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Nowell, L.S.; Norris, J.M.; White, D.E.; Moules, N.J. Thematic analysis: Striving to meet the trustworthiness criteria. Int. J. Qual. Methods 2017, 16, 1–13. [Google Scholar] [CrossRef]
- European Commission. Communication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions. EUR-Lex 2022. Available online: https://eur-lex.europa.eu/legal-content/EN/ALL/?uri=CELEX%3A52012DC0673 (accessed on 31 May 2024).
- Scheibe, S.; Timpel, P.; Mäder, M.; Heinrich, R.; Kugler, J.; Schönfelder, T. Effektivität digitaler Pflegeanwendungen bei Pflegebedürftigen im häuslichen Umfeld [The effectiveness of digital care applications in people with need of home care: A systematic review]. Pflege 2024, 38, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Van Dort, B.A.; Zheng, W.Y.; Sundar, V.; Baysari, M.T. Optimizing clinical decision support alerts in electronic medical records: A systematic review of reported strategies adopted by hospitals. J. Am. Med. Inform. Assoc. 2021, 28, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Sutton, R.T.; Pincock, D.; Baumgart, D.C.; Sadowski, D.C.; Fedorak, R.N.; Kroeker, K.I. An overview of clinical decision support systems: Benefits, risks, and strategies for success. NPJ Digit. Med. 2020, 3, 17. [Google Scholar] [CrossRef]
- Gani, I.; Litchfield, I.; Shukla, D.; Delanerolle, G.; Cockburn, N.; Pathmanathan, A. Understanding “Alert Fatigue” in Primary Care: Qualitative Systematic Review of General Practitioners Attitudes and Experiences of Clinical Alerts, Prompts, and Reminders. J. Med. Internet Res. 2025, 27, e62763. [Google Scholar] [CrossRef]
- Shahriari, M.; Nia, D.H.; Kalij, F.; Hashemi, M.S. Challenges of home care: A qualitative study. BMC Nurs. 2024, 23, 215. [Google Scholar] [CrossRef]
- Departament de Salut. Generalitat de Catalunya. Seguretat dels Pacients. Generalitat de Catalunya, 2017. Available online: https://seguretatdelspacients.gencat.cat/ca/HCP/projectes_de_seguretat_dels_pacients/plataforma-de-seguretat-dels-pacients-de-catalunya/sistema-de-notificacio/ (accessed on 17 February 2023).
- Departament de Salut. Generalitat de Catalunya. Seguretat dels Pacients. Generalitat de Catalunya, 2022. Available online: https://seguretatdelspacients.gencat.cat/ca/detalls/article/app-proscat (accessed on 12 June 2023).
- Paatela, S.; Kyytsönen, M.; Saranto, K.; Kinnunen, U.M.; Vehko, T. Experiences of Electronic Health Records’ and Client Information Systems’ Use on a Mobile Device and Factors Associated With Work Time Savings Among Practical Nurses: Cross-Sectional Study. J. Med. Internet Res. 2024, 26, e46954. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernández-Vidal, N.; Pujol-Vidal, M.; Mengíbar-García, Y.; Ayala-Villuendas, D.; Contel-Segura, J.-C.; Martínez-Torres, S.; Bordas, A.; Oriol-Colominas, E.; Martín-Vergara, N.; Martín-Lujan, F.; et al. Design, Implementation, and Evaluation of Healthcare Visual Map Tool for Health Workers to Improve Quality of Life of Home Care Patients: Study Protocol. Healthcare 2025, 13, 626. https://doi.org/10.3390/healthcare13060626
Hernández-Vidal N, Pujol-Vidal M, Mengíbar-García Y, Ayala-Villuendas D, Contel-Segura J-C, Martínez-Torres S, Bordas A, Oriol-Colominas E, Martín-Vergara N, Martín-Lujan F, et al. Design, Implementation, and Evaluation of Healthcare Visual Map Tool for Health Workers to Improve Quality of Life of Home Care Patients: Study Protocol. Healthcare. 2025; 13(6):626. https://doi.org/10.3390/healthcare13060626
Chicago/Turabian StyleHernández-Vidal, Núria, Marta Pujol-Vidal, Yolanda Mengíbar-García, David Ayala-Villuendas, Joan-Carlos Contel-Segura, Sara Martínez-Torres, Anna Bordas, Eulalia Oriol-Colominas, Nuria Martín-Vergara, Francisco Martín-Lujan, and et al. 2025. "Design, Implementation, and Evaluation of Healthcare Visual Map Tool for Health Workers to Improve Quality of Life of Home Care Patients: Study Protocol" Healthcare 13, no. 6: 626. https://doi.org/10.3390/healthcare13060626
APA StyleHernández-Vidal, N., Pujol-Vidal, M., Mengíbar-García, Y., Ayala-Villuendas, D., Contel-Segura, J.-C., Martínez-Torres, S., Bordas, A., Oriol-Colominas, E., Martín-Vergara, N., Martín-Lujan, F., Astier-Peña, M.-P., & Gens-Barberà, M. (2025). Design, Implementation, and Evaluation of Healthcare Visual Map Tool for Health Workers to Improve Quality of Life of Home Care Patients: Study Protocol. Healthcare, 13(6), 626. https://doi.org/10.3390/healthcare13060626






