Trajectories of Mental Distress and Resilience During the COVID-19 Pandemic Among Healthcare Workers
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Sample Characteristics
2.3. Measures
2.3.1. Depressive and Anxiety Symptoms (PHQ-4)
2.3.2. Resilience (RS-5)
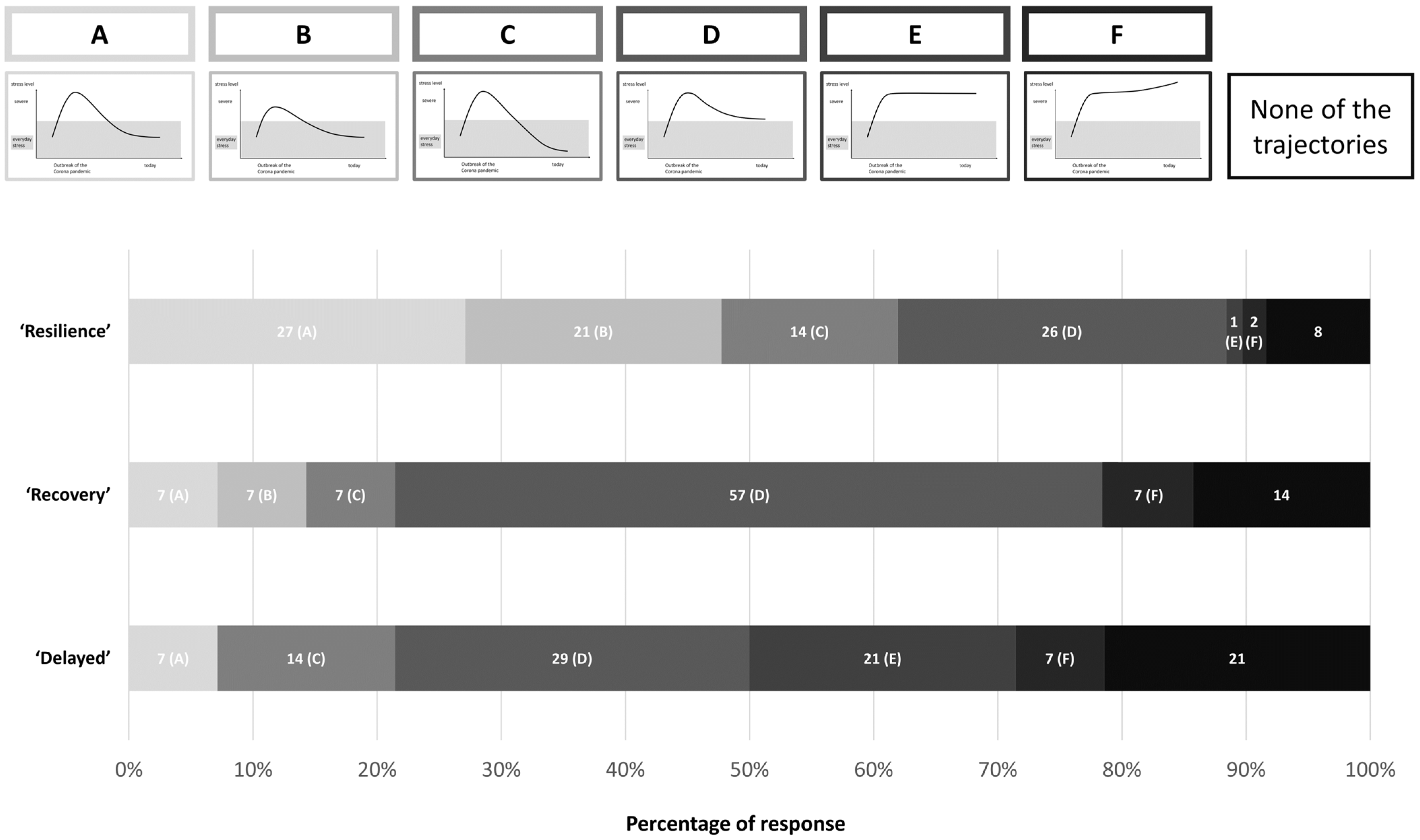
2.3.3. Self-Reported Trajectories of Resilience
2.4. Statistical Analysis
3. Results
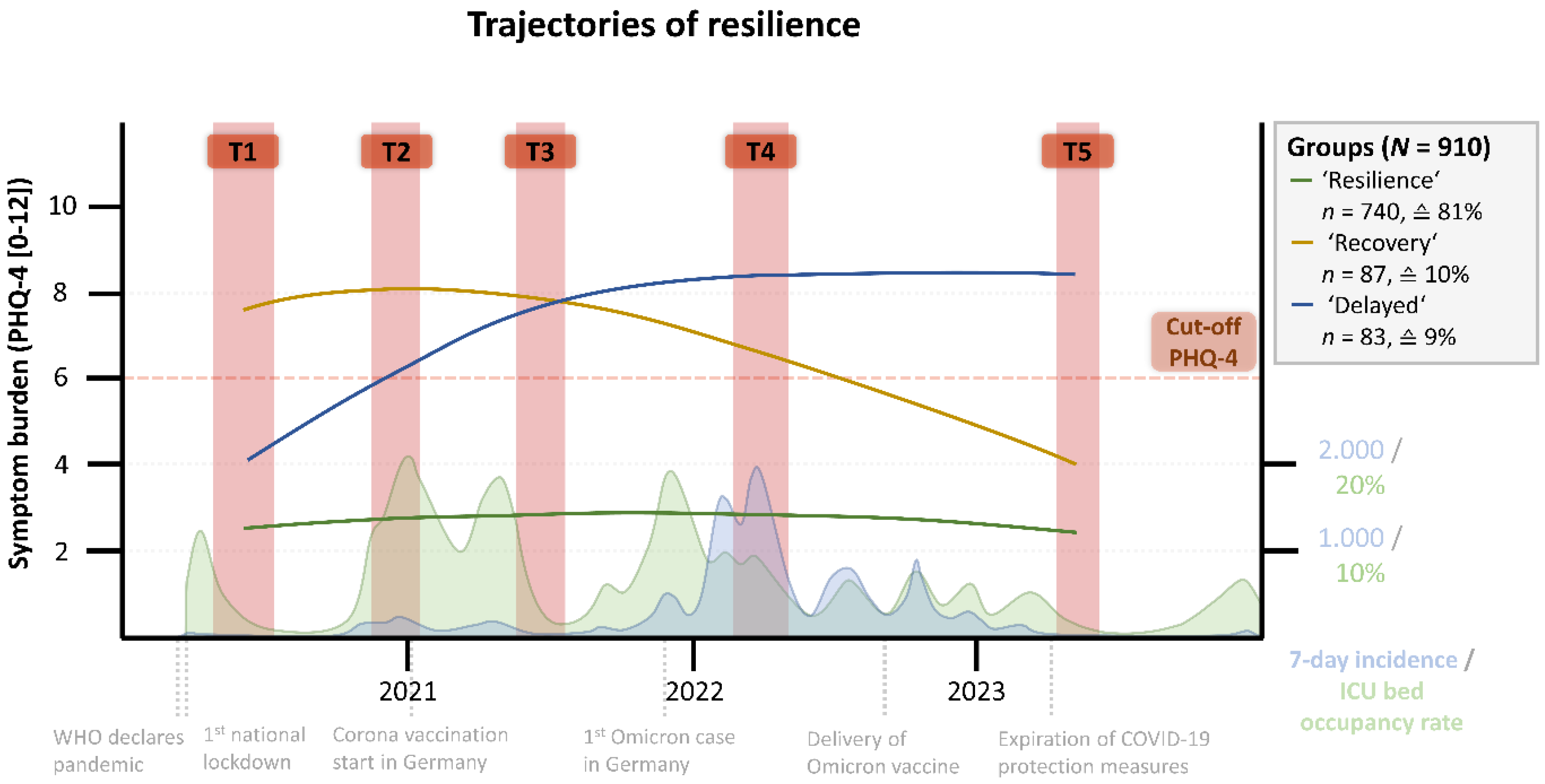
3.1. Trajectories of Resilience
3.2. Cohort Characteristics
3.3. Symptom Burden and Resilience
3.4. Comparison of Self-Reported and Data-Based Stress Trajectories
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bhattacharjee, B.; Acharya, T. The COVID-19 Pandemic and Its Effect on Mental Health in USA—A Review with Some Coping Strategies. Psychiatr. Q. 2020, 91, 1135–1145. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.J.; Pusica, Y.; Sohaei, D.; Prassas, I.; Diamandis, E.P. An Overview of Mental Health during the COVID-19 Pandemic. Diagnosis 2021, 8, 403–412. [Google Scholar] [CrossRef] [PubMed]
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental Health before and during the COVID-19 Pandemic: A Longitudinal Probability Sample Survey of the UK Population. Lancet Psychiatry 2020, 7, 883–892. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Wu, Y.; Fan, S.; Dal Santo, T.; Li, L.; Jiang, X.; Li, K.; Wang, Y.; Tasleem, A.; Krishnan, A.; et al. Comparison of Mental Health Symptoms before and during the Covid-19 Pandemic: Evidence from a Systematic Review and Meta-Analysis of 134 Cohorts. BMJ 2023, 380, e074224. [Google Scholar] [CrossRef]
- Patzina, A.; Collischon, M.; Hoffmann, R.; Obrizan, M. Mental Health in Germany before, during and after the COVID-19 Pandemic. PLoS ONE 2025, 20, e0313689. [Google Scholar] [CrossRef]
- Du, J.; Mayer, G.; Hummel, S.; Oetjen, N.; Gronewold, N.; Zafar, A.; Schultz, J.H. Mental Health Burden in Different Professions during the Final Stage of the COVID-19 Lockdown in China: Cross-Sectional Survey Study. J. Med. Internet Res. 2020, 22, e24240. [Google Scholar] [CrossRef]
- Aymerich, C.; Pedruzo, B.; Pérez, J.L.; Laborda, M.; Herrero, J.; Blanco, J.; Mancebo, G.; Andrés, L.; Estévez, O.; Fernandez, M.; et al. COVID-19 Pandemic Effects on Health Worker’s Mental Health: Systematic Review and Meta-Analysis. Eur. Psychiatry 2022, 65, e10. [Google Scholar] [CrossRef]
- Qi, G.; Yuan, P.; Qi, M.; Hu, X.; Shi, S.; Shi, X. Influencing Factors of High PTSD among Medical Staff during COVID-19: Evidences from Both Meta-Analysis and Subgroup Analysis. Saf. Health Work 2022, 13, 269–278. [Google Scholar] [CrossRef]
- Lowry, D.; Hevey, D.; Wilson, C.; Doherty, V.O.; Sullivan, S.O.; Finnerty, C.; Pender, N.; D’Alton, P.; Mulhern, S. Wellbeing and Mental Health Outcomes amongst Hospital Healthcare Workers during COVID-19. Ir. J. Psychol. Med. 2023, 40, 402–410. [Google Scholar] [CrossRef]
- Alhouri, A.; Abu Shokor, M.; Marwa, K.; Sharabi, A.; Mohammad Nazir Arrouk, D.; Al Houri, F.N.; Al Houri, H. COVID-19 and Its Impact on Healthcare Workers: Understanding Stigma, Tress, and Quality of Life. Cureus 2023, 15, e37846. [Google Scholar] [CrossRef]
- Havnen, A.; Anyan, F.; Hjemdal, O.; Solem, S.; Riksfjord, M.G.; Hagen, K. Resilience Moderates Negative Outcome from Stress during the COVID-19 Pandemic: A Moderated-Mediation Approach. Int. J. Environ. Res. Public Health 2020, 17, 6461. [Google Scholar] [CrossRef] [PubMed]
- Polizzi, C.P.; McDonald, C.W.; Sleight, F.G.; Lynn, S.J. Resilience, Coping, and the COVID-19 Pandemic across the Globe—An Update: What Have We Learned? Clin. Neuropsychiatry 2023, 20, 316–326. [Google Scholar] [CrossRef] [PubMed]
- Carr, E.; Oetzmann, C.; Davis, K.; Bergin-Cartwright, G.; Dorrington, S.; Lavelle, G.; Leightley, D.; Polling, C.; Stevelink, S.A.M.; Wickersham, A.; et al. Trajectories of Mental Health among UK University Staff and Postgraduate Students during the Pandemic. Occup. Environ. Med. 2022, 79, 514–520. [Google Scholar] [CrossRef] [PubMed]
- Wackerhagen, C.; Veer, I.M.; van Leeuwen, J.M.C.; Reppmann, Z.; Riepenhausen, A.; Bögemann, S.A.; Mor, N.; Puhlmann, L.M.C.; Uściko, A.; Zerban, M.; et al. Dynamic Modelling of Mental Resilience in Young Adults: Protocol for a Longitudinal Observational Study (DynaM-OBS). JMIR Res. Protoc. 2023, 12, e39817. [Google Scholar] [CrossRef]
- Galatzer-Levy, I.R.; Huang, S.H.; Bonanno, G.A. Trajectories of Resilience and Dysfunction Following Potential Trauma: A Review and Statistical Evaluation. Clin. Psychol. Rev. 2018, 63, 41–55. [Google Scholar] [CrossRef]
- Schäfer, S.K.; Kunzler, A.M.; Kalisch, R.; Tüscher, O.; Lieb, K. Trajectories of Resilience and Mental Distress to Global Major Disruptions. Trends Cogn. Sci. 2022, 26, 1171–1189. [Google Scholar] [CrossRef]
- Neuberger, F.; Grgic, M.; Buchholz, U.; Maly-Motta, H.L.; Fackler, S.; Lehfeld, A.-S.; Haas, W.; Kalicki, B.; Kuger, S. Delta and Omicron: Protective Measures and SARS-CoV-2 Infections in Day Care Centres in Germany in the 4th and 5th Wave of the Pandemic 2021/2022. BMC Public Health 2022, 22, 2106. [Google Scholar] [CrossRef]
- Löwe, B.; Wahl, I.; Rose, M.; Spitzer, C.; Glaesmer, H.; Wingenfeld, K.; Schneider, A.; Brähler, E. A 4-Item Measure of Depression and Anxiety: Validation and Standardization of the Patient Health Questionnaire-4 (PHQ-4) in the General Population. J. Affect. Disord. 2010, 122, 86–95. [Google Scholar] [CrossRef]
- Christodoulaki, A.; Baralou, V.; Konstantakopoulos, G.; Touloumi, G. Validation of the Patient Health Questionnaire-4 (PHQ-4) to Screen for Depression and Anxiety in the Greek General Population. J. Psychosom. Res. 2022, 160, 110970. [Google Scholar] [CrossRef]
- von Eisenhart Rothe, A.; Zenger, M.; Lacruz, M.E.; Emeny, R.; Baumert, J.; Haefner, S.; Ladwig, K.-H. Validation and Development of a Shorter Version of the Resilience Scale RS-11: Results from the Population-Based KORA–Age Study. BMC Psychol. 2013, 1, 25. [Google Scholar] [CrossRef]
- Wagnild, G.M.; Young, H.M. Development and Psychometric Evaluation of the Resilience Scale. J. Nurs. Meas. 1993, 1, 165–178. [Google Scholar] [PubMed]
- Wickrama, K.A.S.; Lee, T.K.; O’Neal, C.W.; Lorenz, F.O. Higher-Order Growth Curves and Mixture Modeling with Mplus: A Practical Guide; Routledge: New York, NY, USA, 2016; ISBN 9780367711269. [Google Scholar]
- Sclove, S.L. Application of Model-Selection Criteria to Some Problems in Multivariate Analysis. Psychometrika 1987, 52, 333–343. [Google Scholar] [CrossRef]
- Lo, Y.; Mendell, N.R.; Rubin, D.B. Testing the Number of Components in a Normal Mixture. Biometrika 2001, 88, 767–778. [Google Scholar] [CrossRef]
- Nylund, K.L.; Asparouhov, T.; Muthén, B.O. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct. Equ. Model. 2007, 14, 535–569. [Google Scholar] [CrossRef]
- Jung, T.; Wickrama, K.A.S. An Introduction to Latent Class Growth Analysis and Growth Mixture Modeling. Soc. Personal. Psychol. Compass 2008, 2, 302–317. [Google Scholar] [CrossRef]
- Seery, M.D.; Holman, E.A.; Silver, R.C. Whatever Does Not Kill Us: Cumulative Lifetime Adversity, Vulnerability, and Resilience. J. Personal. Soc. Psychol. 2010, 99, 1025–1041. [Google Scholar] [CrossRef]
- Beschoner, P.; Jerg-Bretzke, L.; Erim, Y.; Geiser, F.; Baranowski, A.M.; Weidner, K.; Albus, C.; Schug, C.; Limbrecht-Ecklundt, K.; Weimer, K.; et al. The Prevalence of Effort-Reward Imbalance and Its Associations with Working Conditions, Psychosocial Resources and Burden among Health Care Workers during the COVID-19 Pandemic: Results of the EgePan-Voice Study. PLoS ONE 2023, 18, e0287509. [Google Scholar] [CrossRef]
- Morawa, E.; Schug, C.; Geiser, F.; Beschoner, P.; Jerg-Bretzke, L.; Albus, C.; Weidner, K.; Hiebel, N.; Borho, A.; Erim, Y. Psychosocial Burden and Working Conditions during the COVID-19 Pandemic in Germany: The VOICE Survey among 3678 Health Care Workers in Hospitals. J. Psychosom. Res. 2021, 144, 110415. [Google Scholar] [CrossRef]
- Hobbs, C.; Lewis, G.; Dowrick, C.; Kounali, D.; Peters, T.J.; Lewis, G. Comparison between Self-Administered Depression Questionnaires and Patients’ Own Views of Changes in Their Mood: A Prospective Cohort Study in Primary Care. Psychol. Med. 2021, 51, 853–860. [Google Scholar] [CrossRef]
- Bonanno, G.A. Loss, Trauma, and Human Resilience: Have We Underestimated the Human Capacity to Thrive after Extremely Aversive Events? Am. Psychol. 2004, 59, 20–28. [Google Scholar] [CrossRef]
- Hiebel, N.; Rabe, M.; Maus, K.; Peusquens, F.; Radbruch, L.; Geiser, F. Resilience in Adult Health Science Revisited—A Narrative Review Synthesis of Process-Oriented Approaches. Front. Psychol. 2021, 12, 659395. [Google Scholar] [CrossRef] [PubMed]
- Southwick, S.M.; Sippel, L.; Krystal, J.; Charney, D.; Mayes, L.; Pietrzak, R.H. Why Are Some Individuals More Resilient than Others: The Role of Social Support. World Psychiatry 2016, 15, 77–79. [Google Scholar] [CrossRef] [PubMed]
- Windle, G. What Is Resilience? A Review and Concept Analysis. Rev. Clin. Gerontol. 2011, 21, 152–169. [Google Scholar] [CrossRef]
- Röhrig, B.; Schleußner, C.; Brix, C.; Strauß, B. Die Resilienzskala (RS): Ein Statistischer Vergleich Der Kurz- Und Langform Anhand Einer Onkologischen Patientenstichprobe [The Resilience Scale (RS): A Statistical Comparison of the Short and Long Form Using an Oncology Patient Sample]. PPmP Psychother. Psychosom. Med. Psychol. 2006, 56, 285–290. [Google Scholar] [CrossRef]
- Fisher, D.M.; Law, R.D. How to Choose a Measure of Resilience: An Organizing Framework for Resilience Measurement. Appl. Psychol. 2021, 70, 643–673. [Google Scholar] [CrossRef]
- Morawa, E.; Adler, W.; Schug, C.; Geiser, F.; Beschoner, P.; Jerg-Bretzke, L.; Albus, C.; Weidner, K.; Baranowski, A.M.; Erim, Y. Depressive and Anxiety Symptoms in the Course of the COVID-19 Pandemic among Physicians in Hospitals: Results of the Longitudinal, Multicenter VOICE-EgePan Survey over Two Years. BMC Psychol. 2023, 11, 327. [Google Scholar] [CrossRef]

| Total | Resilience | Recovery | Delayed | |
|---|---|---|---|---|
| Gender, n (%) | ||||
| Female | 701 | 569 (81.17%) | 71 (10.13%) | 61 (8.70%) |
| Male | 224 | 184 (82.14%) | 17 (7.59%) | 23 (10.27%) |
| Diverse | 5 | 2 (40.00%) | 1 (20.00%) | 2 (40.00%) |
| Age, n (%) | ||||
| 18–30 | 170 | 125 (73.53%) | 23 (13.53%) | 22 (12.94%) |
| 31–40 | 268 | 208 (77.61%) | 31 (11.57%) | 28 (10.45%) |
| 41–50 | 256 | 211 (82.42%) | 19 (7.42%) | 26 (10.16%) |
| 51–60 | 325 | 280 (86.15%) | 23 (7.08%) | 22 (6.77%) |
| 61–70 | 69 | 62 (89.86%) | 3 (4.35%) | 4 (5.80%) |
| 70+ | 2 | 2 (100.00%) | 0 (0.00%) | 0 (0.00%) |
| Profession, n (%) | ||||
| Physicians | 168 | 148 (88.10%) | 8 (4.76%) * | 12 (7.14%) |
| Nurses | 231 | 184 (79.65%) | 25 (10.82%) | 21 (9.09%) |
| Medical Technical Assistants (MTAs) | 156 | 112 (71.79%) | 25 (16.03%) *** | 18 (11.54%) |
| Psychologists | 50 | 46 (92.00%) | 3 (6.00%) | 2 (4.00%) |
| Pastoral care workers | 58 | 56 (96.55%) | 1 (1.72%) | 1 (1.72%) |
| Others | 407 | 323 (79.36%) | 40 (9.83%) | 44 (10.81%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baranowski, A.M.; Tüttenberg, S.C.; Culmann, A.C.; Matthias, J.-K.; Maus, K.; Blank, R.; Erim, Y.; Morawa, E.; Beschoner, P.; Jerg-Bretzke, L.; et al. Trajectories of Mental Distress and Resilience During the COVID-19 Pandemic Among Healthcare Workers. Healthcare 2025, 13, 574. https://doi.org/10.3390/healthcare13050574
Baranowski AM, Tüttenberg SC, Culmann AC, Matthias J-K, Maus K, Blank R, Erim Y, Morawa E, Beschoner P, Jerg-Bretzke L, et al. Trajectories of Mental Distress and Resilience During the COVID-19 Pandemic Among Healthcare Workers. Healthcare. 2025; 13(5):574. https://doi.org/10.3390/healthcare13050574
Chicago/Turabian StyleBaranowski, Andreas M., Simone C. Tüttenberg, Anna C. Culmann, Julia-K. Matthias, Katja Maus, Rebecca Blank, Yesim Erim, Eva Morawa, Petra Beschoner, Lucia Jerg-Bretzke, and et al. 2025. "Trajectories of Mental Distress and Resilience During the COVID-19 Pandemic Among Healthcare Workers" Healthcare 13, no. 5: 574. https://doi.org/10.3390/healthcare13050574
APA StyleBaranowski, A. M., Tüttenberg, S. C., Culmann, A. C., Matthias, J.-K., Maus, K., Blank, R., Erim, Y., Morawa, E., Beschoner, P., Jerg-Bretzke, L., Albus, C., Weidner, K., Radbruch, L., Richter, C., & Geiser, F. (2025). Trajectories of Mental Distress and Resilience During the COVID-19 Pandemic Among Healthcare Workers. Healthcare, 13(5), 574. https://doi.org/10.3390/healthcare13050574






