Motor Control Exercises and Their Design for Short-Term Pain Modulation in Patients with Pelvic Girdle Pain: A Narrative Review
Abstract
1. Introduction
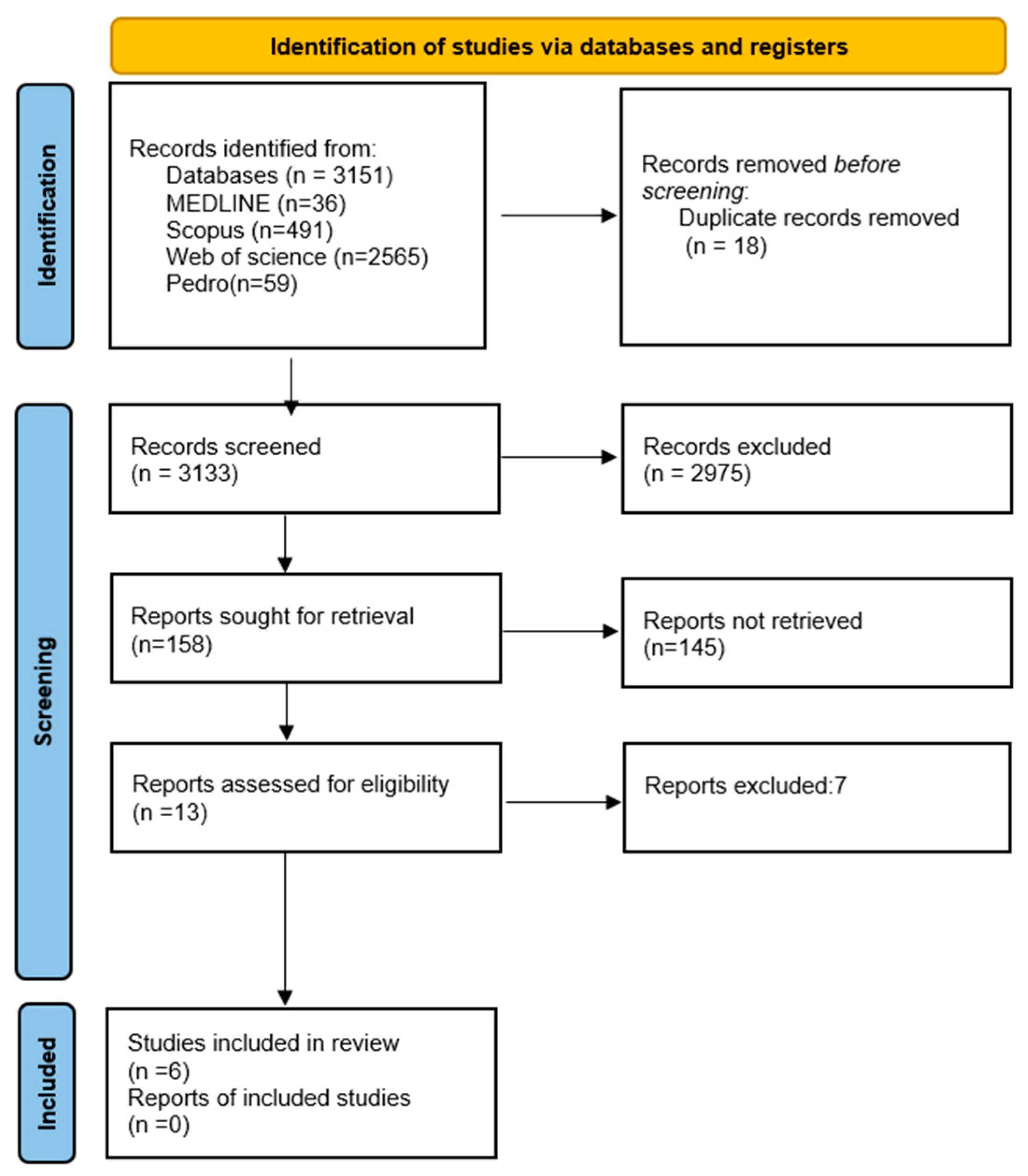
2. Materials and Methods
Data Extracion
3. Results
Results of Studies Selected
4. Discussion
4.1. Limits
4.2. Clinical Implication and Future Study Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stuge, B. Evidence of Stabilizing Exercises for Low Back- and Pelvic Girdle Pain—A Critical Review. Braz. J. Phys. Ther. 2019, 23, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Vleeming, A.; Albert, H.B.; Östgaard, H.C.; Sturesson, B.; Stuge, B. European Guidelines for the Diagnosis and Treatment of Pelvic Girdle Pain. Eur. Spine J. 2008, 17, 794–819. [Google Scholar] [CrossRef]
- Weis, C.A.; Pohlman, K.; Draper, C.; daSilva-Oolup, S.; Stuber, K.; Hawk, C. Chiropractic Care for Adults With Pregnancy-Related Low Back, Pelvic Girdle Pain, or Combination Pain: A Systematic Review. J. Manip. Physiol. Ther. 2020, 43, 714–731. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, D.J.; Engel, A.; Kreiner, D.S.; Nampiaparampil, D.; Duszynski, B.; MacVicar, J. Fluoroscopically Guided Diagnostic and Therapeutic Intra-Articular Sacroiliac Joint Injections: A Systematic Review. Pain Med. 2015, 16, 1500–1518. [Google Scholar] [CrossRef]
- Wiezer, M.; Hage-Fransen, M.A.H.; Otto, A.; Wieffer-Platvoet, M.S.; Slotman, M.H.; Nijhuis-van Der Sanden, M.W.G.; Pool-Goudzwaard, A.L. Risk Factors for Pelvic Girdle Pain Postpartum and Pregnancy Related Low Back Pain Postpartum; a Systematic Review and Meta-Analysis. Musculoskelet. Sci. Pract. 2020, 48, 102154. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, P.B.; Beales, D.J. Diagnosis and Classification of Pelvic Girdle Pain Disorders—Part 1: A Mechanism Based Approach within a Biopsychosocial Framework. Man. Ther. 2007, 12, 86–97. [Google Scholar] [CrossRef]
- Maselli, F.; Palladino, M.; Barbari, V.; Storari, L.; Rossettini, G.; Testa, M. The Diagnostic Value of Red Flags in Thoracolumbar Pain: A Systematic Review. Disabil. Rehabil. 2022, 44, 1190–1206. [Google Scholar] [CrossRef]
- Todd, N.V. Guidelines for Cauda Equina Syndrome. Red Flags and White Flags. Systematic Review and Implications for Triage. Br. J. Neurosurg. 2017, 31, 336–339. [Google Scholar] [CrossRef]
- Wuytack, F.; Begley, C.; Daly, D. Risk Factors for Pregnancy-Related Pelvic Girdle Pain: A Scoping Review. BMC Pregnancy Childbirth 2020, 20, 739. [Google Scholar] [CrossRef]
- Starkey, S.C.; Lenton, G.; Saxby, D.J.; Hinman, R.S.; Bennell, K.L.; Metcalf, B.R.; Hall, M. Effect of Functional Weightbearing Versus Non-Weightbearing Quadriceps Strengthening Exercise on Contact Force in Varus-Malaligned Medial Knee Osteoarthritis: A Secondary Analysis of a Randomized Controlled Trial; Hall, M., Ed.; Centre for Health Exercise and Sports Medicine, Department of Physiotherapy, The University of Melbourne: Victoria, Australia, 2022; Volume 39, ISBN 0968-0160. [Google Scholar]
- Desgagnés, A.; Patricio, P.; Bérubé, N.; Bernard, S.; Lamothe, M.; Massé-Alarie, H. Motor Control of the Spine in Pregnancy-Related Lumbopelvic Pain: A Systematic Review. Clin. Biomech. 2022, 98, 105716. [Google Scholar] [CrossRef]
- Levin, M.F.; Piscitelli, D. Motor Control: A Conceptual Framework for Rehabilitation. Mot. Control 2022, 26, 497–517. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Woollacott, M.H. Motor Control: Translating Research into Clinical Practice, 5th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2017; ISBN 978-1-4963-0263-2. [Google Scholar]
- Ganesh, G.S.; Kaur, P.; Meena, S. Systematic Reviews Evaluating the Effectiveness of Motor Control Exercises in Patients with Non-Specific Low Back Pain Do Not Consider Its Principles—A Review. J. Bodyw. Mov. Ther. 2021, 26, 374–393. [Google Scholar] [CrossRef] [PubMed]
- Cano-de-la-Cuerda, R.; Molero-Sánchez, A.; Carratalá-Tejada, M.; Alguacil-Diego, I.M.; Molina-Rueda, F.; Miangolarra-Page, J.C.; Torricelli, D. Theories and Control Models and Motor Learning: Clinical Applications in Neurorehabilitation. Neurol. Engl. Ed. 2015, 30, 32–41. [Google Scholar] [CrossRef]
- Wulf, G.; Shea, C.; Lewthwaite, R. Motor Skill Learning and Performance: A Review of Influential Factors: Motor Skill Learning and Performance. Med. Educ. 2010, 44, 75–84. [Google Scholar] [CrossRef]
- Kleim, J.A.; Jones, T.A. Principles of Experience-Dependent Neural Plasticity: Implications for Rehabilitation After Brain Damage. J. Speech Lang. Hear. Res. 2008, 51, S225–S239. [Google Scholar] [CrossRef]
- Mapinduzi, J.; Ndacayisaba, G.; Mahaudens, P.; Hidalgo, B. Effectiveness of Motor Control Exercises versus Other Musculoskeletal Therapies in Patients with Pelvic Girdle Pain of Sacroiliac Joint Origin: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. BMR 2022, 35, 713–728. [Google Scholar] [CrossRef]
- Gasparyan, A.Y.; Ayvazyan, L.; Blackmore, H.; Kitas, G.D. Writing a Narrative Biomedical Review: Considerations for Authors, Peer Reviewers, and Editors. Rheumatol. Int. 2011, 31, 1409–1417. [Google Scholar] [CrossRef]
- Page, M.J. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Kamali, F.; Zamanlou, M.; Ghanbari, A.; Alipour, A.; Bervis, S. Comparison of Manipulation and Stabilization Exercises in Patients with Sacroiliac Joint Dysfunction Patients: A Randomized Clinical Trial. J. Bodyw. Mov. Ther. 2019, 23, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Nejati, P. Effectiveness of Exercise Therapy andManipulation on Sacroiliac Joint Dysfunction:A Randomized Controlled Trial. Pain Phys. 2019, 1, 53–61. [Google Scholar] [CrossRef]
- Almousa, S.; Lamprianidou, E.; Kitsoulis, G. The Effectiveness of Stabilising Exercises in Pelvic Girdle Pain during Pregnancy and after Delivery: A Systematic Review. Physiother. Res. Int. 2018, 23, e1699. [Google Scholar] [CrossRef]
- Kokic, I.; Ivanisevic, M.; Uremovic, M.; Kokic, T.; Pisot, R.; Simunic, B. Effect of Therapeutic Exercises on Pregnancy-Related Low Back Pain and Pelvic Girdle Pain: Secondary Analysis of a Randomized Controlled Trial. J. Rehabil. Med. 2017, 49, 251–257. [Google Scholar] [CrossRef] [PubMed]
- ElDeeb, A.M.; Abd-Ghafar, K.S.; Ayad, W.A.; Sabbour, A.A. Effect of Segmental Stabilizing Exercises Augmented by Pelvic Floor Muscles Training on Women with Postpartum Pelvic Girdle Pain: A Randomized Controlled Trial. BMR 2019, 32, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Tseng, P.-C.; Puthussery, S.; Pappas, Y.; Gau, M.-L. A Systematic Review of Randomised Controlled Trials on the Effectiveness of Exercise Programs on Lumbo Pelvic Pain among Postnatal Women. BMC Pregnancy Childbirth 2015, 15, 316. [Google Scholar] [CrossRef] [PubMed]
- Newman, D.P.; Soto, A.T. Sacroiliac Joint Dysfunction: Diagnosis and Treatment. Am. Fam. Physician 2022, 105, 239–245. [Google Scholar]
- Piccoli, A.; Rossettini, G.; Cecchetto, S.; Viceconti, A.; Ristori, D.; Turolla, A.; Maselli, F.; Testa, M. Effect of Attentional Focus Instructions on Motor Learning and Performance of Patients with Central Nervous System and Musculoskeletal Disorders: A Systematic Review. J. Funct. Morphol. Kinesiol. 2018, 3, 40. [Google Scholar] [CrossRef]
- Aiken, C.A.; Becker, K.A. Utilising an Internal Focus of Attention during Preparation and an External Focus during Execution May Facilitate Motor Learning. Eur. J. Sports Sci. 2023, 23, 259–266. [Google Scholar] [CrossRef]
- Kantak, S.S.; Johnson, T.; Zarzycki, R. Linking Pain and Motor Control: Conceptualization of Movement Deficits in Patients With Painful Conditions. Phys. Ther. 2022, 102, pzab289. [Google Scholar] [CrossRef]
- Meier, M.L.; Vrana, A.; Schweinhardt, P. Low Back Pain: The Potential Contribution of Supraspinal Motor Control and Proprioception. Neuroscientist 2019, 25, 583–596. [Google Scholar] [CrossRef]
- Hodges, P.W. Pain and Motor Control: From the Laboratory to Rehabilitation. J. Electromyogr. Kinesiol. 2011, 21, 220–228. [Google Scholar] [CrossRef]
- Levin, M.F.; Demers, M. Motor Learning in Neurological Rehabilitation. Disabil. Rehabil. 2021, 43, 3445–3453. [Google Scholar] [CrossRef] [PubMed]
- Low, M. A Time to Reflect on Motor Control in Musculoskeletal Physical Therapy. J. Orthop. Sports Phys. Ther. 2018, 48, 833–836. [Google Scholar] [CrossRef] [PubMed]
| Motor Control Theory | Clinical Rationale |
|---|---|
Reflex Theory | Motor control recovery adjusts reflex effects during tasks. The Bobath concept is partially based on this theory. |
Hierarchical theory | Reflex analysis helps assess motor control in neurological patients, gauge neural maturity, and predict function. |
Motor programming theory | Focuses on relearning movement patterns, restoring key functional actions, and using alternative effectors if needed. |
Systems theory | Assessment and treatment should address both specific motor control deficits and broader system interactions, including musculoskeletal deficiencies. |
Dynamic action theory | Motor behavior changes follow physical principles rather than just neural structures, guiding therapy through body dynamics. |
Theory of parallel distributed processing | Brain systems are redundant, allowing function despite damage. This model helps predict how nervous system lesions affect performance. |
Activity-oriented theory | It states that MC recovery should focus on essential functional activities. |
Ecological theory | Describes the subject as an active explorer of their environment, where exploration enables the development of multiple ways to perform a task. |
| Author (Year) | Study Design | Group Characteristics | Rehabilitation Intervention | Outcome Measures | Conclusions |
|---|---|---|---|---|---|
| Almousa et al. (2017) [23] | SR | 719 female individuals with PGP pregnancy related and post-partum. | IG: exercises for activation of the multifidus and transversus abdominis. Performed 3 times a week for 12 weeks. CG: no exercises. | Pain and disability. | There is limited evidence for the clinician to conclude on the effectiveness of stabilizing exercises in treating PGP during pregnancy and the postpartum periods. |
| ElDeeb et al. (2019) [25] | RCT | 40 female individuals with PGP during pregnancy or within the first 3 months postpartum. IG: n = 20 patients. CG: n = 20 patients. | IG: exercises to activate the multifidus and transversus abdominis. Performed 3 times a week for 12 weeks. CG: exercises for strengthening pelvic floor muscle. Performed 3 times a week for 12 weeks. | Pain. | This study did not demonstrate significant improvements in the group performing isolated stabilization exercises compared to the group performing pelvic floor exercises. |
| Kamali et al.(2019) [21] | RCT | 30 individuals with subacute or chronic sacroiliac joint dysfunction. IG: n = 10 F patients, 5 M. patients. CG: n = 11 F patients, 4 M patients | IG: stabilization exercise (control of neutral spine alignment, co-contraction of the local muscles transverse abdominis and deep fibers of multifidus with normal, etc.). Patients performed for 20 min 3 times a week, for 4 weeks. CG: in each session, the therapist performed a manipulation technique on the side with positive SIJ test results. Patients were treated individually 3 times a week for 2 weeks by a physiotherapist expert in manual therapy. | Pain and disability. | Despite the improvements seen after both manipulation and stabilization exercise therapies in patients with sacroiliac joint dysfunction, there was no significant between-group difference in the treatment effects. |
| Nejati et al.(2018) [22] | RCT | 51 individuals (sex not specified) with lower back or buttock pain. EG: n = 19 MTG: n = 18 EMTG: n = 19 | All groups performed exercises at home daily for 12 weeks. EG: group received posterior innominate self-mobilization, sacroiliac joint stretching, and spinal stabilization exercises. MG: spinal stabilization exercises EMTG: manual therapy plus stretch and self-mobilization exercises. | Pain and disability | Exercise only and manipulation plus exercise therapy appear to be effective in reducing pain and disability in patients with sacroiliac joint dysfunction. |
| Kokic et al. (2017) [24] | RCT | 45 female individuals with PGP by the 30th week of pregnancy. | IG: aerobic activity and resistance exercises. Activation of the lumbopelvic musculature, pelvic floor exercises, and final stretching. The exercise program commenced within 1 week following inclusion into the trial and continued throughout the duration of the pregnancy. CG: received only standard antenatalcare, but were not discouraged from exercising on their own. | Pain and disability | The exercise program had a beneficial effect on the severity of lumbopelvic pain in pregnancy, reducing the intensity of pain and the level of disability experienced as a result. |
| Tseng et al. (2015) [26] | SR | 251 female individuals with PGP during pregnancy or within the first three months postpartum. | IG: stabilization exercises for the lumbopelvic muscles specifically the multifidus, abdominal muscles, and transversus abdominis. CG: manual therapy, mobilizations, manipulation, and massage. | Pain | There is some evidence to indicate the effectiveness of exercise for relieving lumbopelvic pain, further good quality trials are needed to ascertain the most effective elements of postnatal exercise programs suited for LPP treatment. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zitti, M.; Mantia, A.; Garzonio, F.; Raffaele, G.; Storari, L.; Paciotti, R.; Fiorentino, F.; Andreutto, R.; Maselli, F. Motor Control Exercises and Their Design for Short-Term Pain Modulation in Patients with Pelvic Girdle Pain: A Narrative Review. Healthcare 2025, 13, 572. https://doi.org/10.3390/healthcare13050572
Zitti M, Mantia A, Garzonio F, Raffaele G, Storari L, Paciotti R, Fiorentino F, Andreutto R, Maselli F. Motor Control Exercises and Their Design for Short-Term Pain Modulation in Patients with Pelvic Girdle Pain: A Narrative Review. Healthcare. 2025; 13(5):572. https://doi.org/10.3390/healthcare13050572
Chicago/Turabian StyleZitti, Mirko, Alessandro Mantia, Fabiola Garzonio, Graziano Raffaele, Lorenzo Storari, Rachele Paciotti, Fabio Fiorentino, Rebecca Andreutto, and Filippo Maselli. 2025. "Motor Control Exercises and Their Design for Short-Term Pain Modulation in Patients with Pelvic Girdle Pain: A Narrative Review" Healthcare 13, no. 5: 572. https://doi.org/10.3390/healthcare13050572
APA StyleZitti, M., Mantia, A., Garzonio, F., Raffaele, G., Storari, L., Paciotti, R., Fiorentino, F., Andreutto, R., & Maselli, F. (2025). Motor Control Exercises and Their Design for Short-Term Pain Modulation in Patients with Pelvic Girdle Pain: A Narrative Review. Healthcare, 13(5), 572. https://doi.org/10.3390/healthcare13050572







