Oral Health-Related Quality of Life After Allogeneic Bone Marrow Transplant—A Cross-Sectional Study †
Abstract
1. Introduction
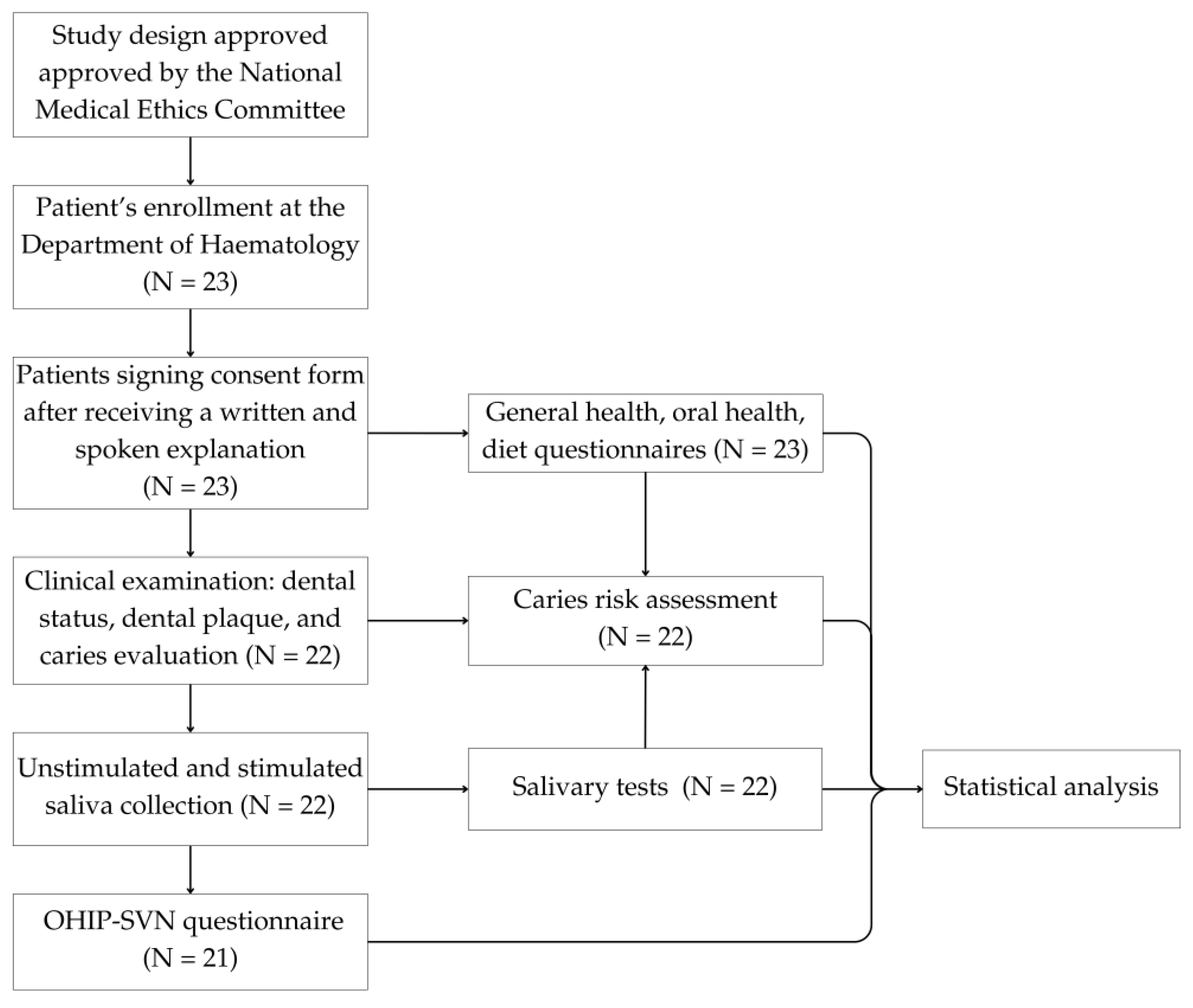
2. Materials and Methods
3. Results
3.1. Results of the Clinical and Demographic Data and the OHIP-SVN Questionnaire
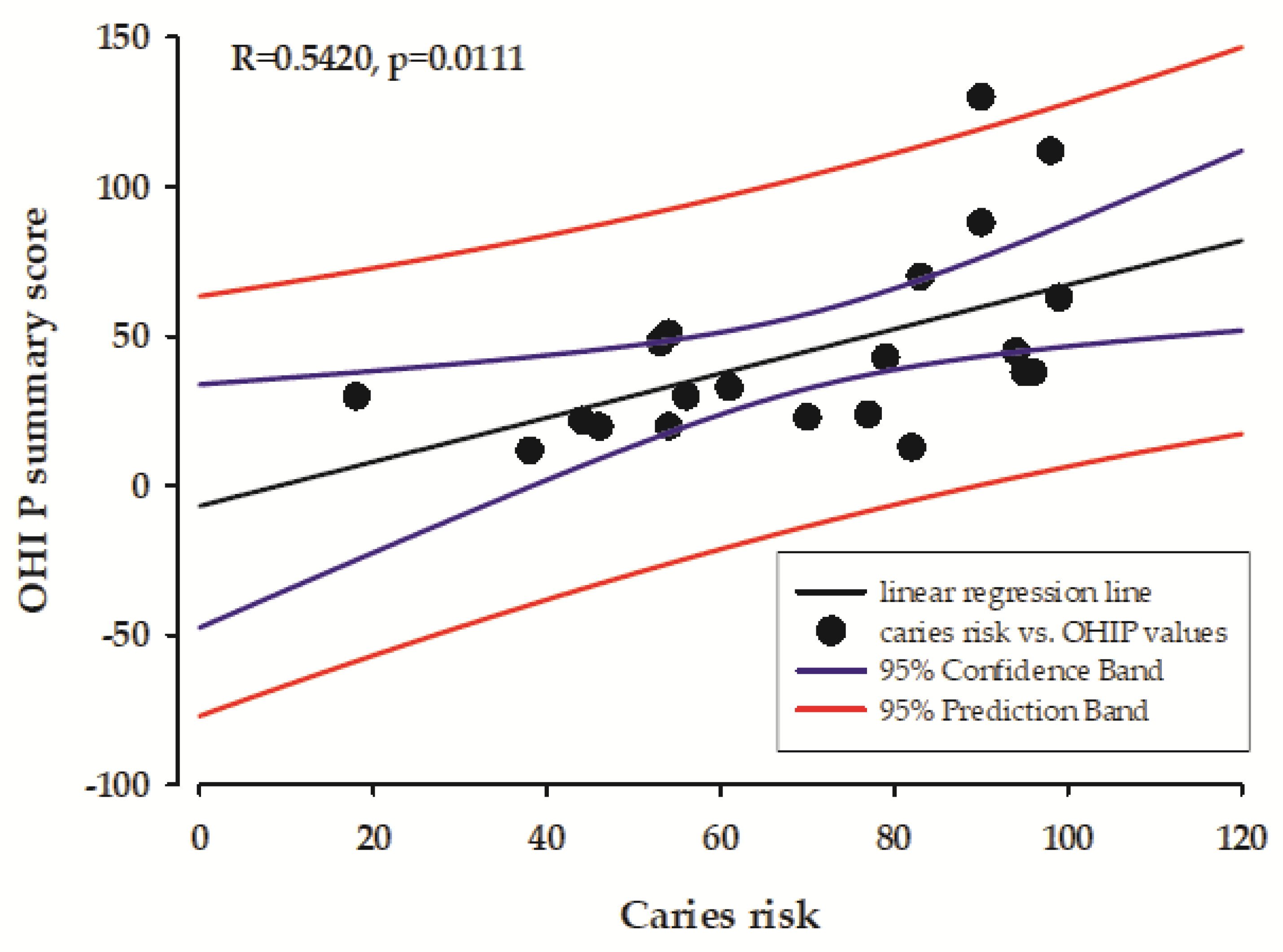
3.2. The Relationship Between the Measured Parameters and the Results of the OHIP-SVN Questionnaire
3.3. Differences Between cGVHD Patients and the Healthy Population
4. Discussion
4.1. General Findings
4.2. Strengths, Limitations, and Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baird, K.; Pavletic, S.Z. Chronic graft versus host disease. Curr. Opin. Hematol. 2006, 13, 426–435. [Google Scholar] [CrossRef] [PubMed]
- Grube, M.; Holler, E.; Weber, D.; Holler, B.; Herr, W.; Wolff, D. Risk Factors and Outcome of Chronic Graft-versus-Host Disease after Allogeneic Stem Cell Transplantation—Results from a Single-Center Observational Study. Biol. Blood Marrow Transplant. 2016, 22, 1781–1791. [Google Scholar] [CrossRef] [PubMed]
- Arai, S.; Arora, M.; Wang, T.; Spellman, S.R.; He, W.; Couriel, D.R.; Urbano-Ispizua, A.; Cutler, C.S.; Bacigalupo, A.A.; Battiwalla, M.; et al. Increasing Incidence of Chronic Graft-versus-Host Disease in Allogeneic Transplantation—A Report from CIBMTR. Biol. Blood Marrow Transplant. 2015, 21, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Baird, K.; Cooke, K.; Schultz, K.R. Chronic Graft-Versus-Host Disease (GVHD) in children. Pediatr. Clin. N. Am. 2010, 57, 297–322. [Google Scholar] [CrossRef]
- Filipovich, A.H.; Weisdorf, D.; Pavletic, S.; Socie, G.; Wingard, J.R.; Lee, S.J.; Martin, P.; Chien, J.; Przepiorka, D.; Couriel, D.; et al. National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: I. diagnosis and staging working group report. Biol. Blood Marrow Transplant. 2005, 11, 945–956. [Google Scholar] [CrossRef]
- Cooke, K.R.; Luznik, L.; Sarantopoulos, S.; Hakim, F.; Jagasia, M.; Fowler, D.; van den Brink, M.R.M.; Hansen, J.A. The Biology of Chronic Graft-versus-Host Disease: A Task Force Report from the National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-Versus-Host Disease. Biol. Blood Marrow Transplant. 2017, 23, 211–234. [Google Scholar] [CrossRef]
- Vadakkel, G.; Eng, S.; Proli, A.; Ponce, D.M. Updates in chronic graft-versus-host disease: Novel treatments and best practices in the current era. Bone Marrow Transplant. 2024, 59, 1360–1368. [Google Scholar] [CrossRef]
- Jagasia, M.H.; Greinix, H.T.; Arora, M.; Williams, K.M.; Wolff, D.; Cowen, E.W.; Palmer, J. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: I. The 2014 Diagnosis and Staging Working Group Report. Biol. Blood Marrow Transplant. 2015, 21, 389–401. [Google Scholar] [CrossRef]
- Meier, J.K.H.; Wolff, D.; Pavletic, S.; Greinix, H.; Gosau, M.; Bertz, H.; Lee, S.J.; Lawitschka, Á.; Elad, S. Oral chronic graft-versus-host disease: Report from the International Consensus Conference on clinical practice in cGVHD. Clin. Oral Investig. 2011, 15, 127–139. [Google Scholar] [CrossRef]
- Lee, S.J.; Vogelsang, G.; Flowers, M.E.D. Chronic graft-versus-host disease. Biol. Blood Marrow Transplant. 2003, 9, 215–233. [Google Scholar] [CrossRef]
- Imanguli, M.M.; Atkinson, J.C.; Mitchell, S.A.; Avila, D.N.; Bishop, R.J.; Cowen, E.W.; Datiles, M.B.; Hakim, F.T.; Kleiner, D.E.; Krumlauf, M.C.; et al. Salivary Gland Involvement in Chronic Graft-Versus-Host Disease: Prevalence, Clinical Significance, and Recommendations for Evaluation. Biol. Blood Marrow Transplant. 2010, 16, 1362–1369. [Google Scholar] [CrossRef] [PubMed]
- Treister, N.; Duncan, C.; Cutler, C.; Lehmann, L. How we treat oral chronic graft-versus-host disease. Blood 2012, 120, 3407–3418. [Google Scholar] [CrossRef] [PubMed]
- Featherstone, J.D.B. The science and practice of caries prevention. J. Am. Dent. Assoc. 2000, 131, 887–899. [Google Scholar] [CrossRef] [PubMed]
- Pretty, I.A.; Ekstrand, K.R. Detection and monitoring of early caries lesions: A review. Eur. Arch. Paediatr. Dent. 2016, 17, 13–25. [Google Scholar] [CrossRef]
- Nyvad, B.; Fejerskov, O. Assessing the stage of caries lesion activity on the basis of clinical and microbiological examination. Community Dent. Oral Epidemiol. 1997, 25, 69–75. [Google Scholar] [CrossRef]
- Humphrey, S.P.; Williamson, R.T. A review of saliva: Normal composition, flow, and function. J. Prosthet. Dent. 2001, 85, 162–169. [Google Scholar] [CrossRef]
- Scully, C.; Felix, D.H. Oral Medicine—Update for the dental practitioner. Dry mouth and disorders of salivation. Br. Dent. J. 2005, 199, 423–427. [Google Scholar] [CrossRef]
- Marsh, P.D. Dental plaque as a biofilm and a microbial community—Implications for health and disease. BMC Oral Health 2006, 6, S14. [Google Scholar] [CrossRef]
- Rodrigues, J.A.; Lussi, A.; Seemann, R.; Neuhaus, K.W. Prevention of crown and root caries in adults. Periodontol. 2000 2011, 55, 231–249. [Google Scholar] [CrossRef]
- Seneviratne, C.J.; Zhang, C.F.; Samaranayake, L.P. Dental plaque biofilm in oral health and disease. Chinese J. Dent. Res. 2011, 14, 87–94. [Google Scholar]
- Struzycka, I. The Oral Microbiome in Dental Caries. Polish J. Microbiol. 2014, 63, 127–135. [Google Scholar] [CrossRef]
- Tanzer, J.M.; Livingston, J.; Thompson, A.M. The Microbiology of Primary Dental Caries in Humans. J. Dent. Educ. 2001, 65, 1028–1037. [Google Scholar] [CrossRef]
- Wiriyasatiankun, P.; Sakoolnamarka, R.; Thanyasrisung, P. The impact of an alkasite restorative material on the pH of Streptococcus mutans biofilm and dentin remineralization: An in vitro study. BMC Oral Health 2022, 22, 334. [Google Scholar] [CrossRef] [PubMed]
- Toz Ertop, M.; Cicek, O.; Erener, H.; Ozkalayci, N.; Demir Cicek, B.; Comert, F. Evaluation of the Demineralization Development around Different Types of Orthodontic Brackets. Materials 2023, 16, 984. [Google Scholar] [CrossRef] [PubMed]
- Lingstrom, P.; Birkhed, D.; Ruben, J.; Arends, J. Effect of Frequent Consumption of Starchy Food Items on Enamel and Dentin Demineralization and on Plaque pH in situ. J. Dent. Res. 1994, 73, 652–660. [Google Scholar] [CrossRef]
- Rugg-Gunn, A. Dental caries: Strategies to control this preventable disease. Acta Med. Acad. 2013, 42, 117–130. [Google Scholar] [CrossRef]
- Featherstone, J.D.B. The continuum of dental caries—Evidence for a dynamic disease process. J. Dent. Res. 2004, 83, C39–C42. [Google Scholar] [CrossRef]
- Cury, J.A.; Tenuta, L.M. How to maintain a cariostatic fluoride concentration in the oral environment. Adv. Dent. Res. 2008, 20, 13–16. [Google Scholar] [CrossRef]
- Pitts, N. “ICDAS”—An international system for caries detection and assessment being developed to facilitate caries epidemiology, research and appropriate clinical management. Community Dent. Health 2004, 21, 193–198. [Google Scholar]
- Kidd, E.A.M. Clinical threshold for carious tissue removal. Dent. Clin. North Am. 2010, 54, 541–549. [Google Scholar] [CrossRef]
- Bratthall, D.; Petersson, G.H. Cariogram—A multifactorial risk assessment model for a multifactorial disease. Community Dent. Oral Epidemiol. 2005, 33, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Rener-Sitar, K.; Celebić, A.; Petricević, N.; Papić, M.; Sapundzhiev, D.; Kansky, A.; Marion, L.; Kopac, I.; Zaletel-Kragelj, L. The Slovenian version of the Oral Health Impact Profile Questionnaire (OHIP-SVN): Translation and psychometric properties. Coll. Antropol. 2009, 33, 1177–1183. [Google Scholar]
- Marquezan, P.K.; Comim, L.D.; de Oliveira Racki, D.N.; Dalla Nora, Á.; Alves, L.S.; Zennker, J.E.d.A. Association between underlying dentin shadows (ICDAS 4) and OHRQoL among adolescents from southern Brazil. Braz. Oral Res. 2024, 38, e046. [Google Scholar] [CrossRef] [PubMed]
- Azher, S.; McGrath, R.; Kamalabadi, Y.M.; Tsakos, G.; Sim, F.; Singh, A. Impact of rehabilitation with dental implants on the quality of life of patients undergoing maxillofacial reconstruction: A systematic review. Qual. Life Res. 2024, 34, 113–130. [Google Scholar] [CrossRef] [PubMed]
- Bulthuis, M.S.; Jan Jager, D.H.; Brand, H.S. Relationship among perceived stress, xerostomia, and salivary flow rate in patients visiting a saliva clinic. Clin. Oral Investig. 2018, 22, 3121–3127. [Google Scholar] [CrossRef]
- Allen, P.F.; O’Sullivan, M.; Locker, D. Determining the minimally important difference for the Oral Health Impact Profile-20. Eur. J. Oral Sci. 2009, 117, 129–134. [Google Scholar] [CrossRef]
- Zucoloto, M.L.; Maroco, J.; Campos, J.A.D.B. Impact of oral health on health-related quality of life: A cross-sectional study. BMC Oral Health 2016, 16, 2–7. [Google Scholar] [CrossRef]
- de Oliveira Júnior, A.G.; Montagna, E.; Zaia, V.; Barbosa, C.P.; Bianco, B. Oral health-related quality of life in patients aged 8 to 19 years with cleft lip and palate: A systematic review and meta-analysis. BMC Oral Health 2023, 23, 670. [Google Scholar] [CrossRef]
- Qamar, Z.; Alghamdi, A.M.S.; Haydarah, N.K.B.; Balateef, A.A.; Alamoudi, A.A.; Abumismar, M.A.; Shivakumar, S.; Cicciù, M.; Minervini, G. Impact of temporomandibular disorders on oral health-related quality of life: A systematic review and meta-analysis. J. Oral Rehabil. 2023, 50, 706–714. [Google Scholar] [CrossRef]
- Rener-Sitar, K.; Celebić, A.; Mehulić, K.; Petricević, N. Factors related to oral health related quality of life in TMD patients. Coll. Antropol. 2013, 37, 407–413. [Google Scholar]
- Serrano, J.; López-Pintor, R.M.; Fernández-Castro, M.; Ramírez, L.; Sanz, M.; López, J.; Blázquez, M.Á.; González, J.J.; Hernández, G. Usefulness of implementing the OHIP-14 questionnaire to assess the impact of xerostomia and hyposalivation on quality of life in patients with primary Sjögren’s syndrome. J. Oral Pathol. Med. 2022, 51, 810–817. [Google Scholar] [CrossRef] [PubMed]
- Santos, P.S.d.S.; Granzotto, F.C.N.; Antunes, H.S.; de Lima, E.M.; Varanda, R.d.F.; Maccari, K.; Bezinelli, L.M.; Melo, W.R.; Junior, L.A.V.S.; De Macedo, L.D.; et al. Dentistry consensus on HSCT—Part III: Special topics—Dentistry on HSCT. Hematol. Transfus. Cell Ther. 2023, 45, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Stolze, J.; Boor, M.; Hazenberg, M.D.; Brand, H.S.; Raber-Durlacher, J.E.; Laheij, A.M.G.A. Oral health–related quality of life of patients with oral chronic graft-versus-host disease. Support. Care Cancer 2021, 29, 6353–6360. [Google Scholar] [CrossRef] [PubMed]
- Baker, K.S.; Fraser, C.J. Quality of life and recovery after graft-versus-host disease. Best Pract. Res. Clin. Haematol. 2008, 21, 333–341. [Google Scholar] [CrossRef]
- DePaloa, J.; Chaib, X.; Leeb, S.J.; Cutlerc, C.S.; Treister, N. Assessing the relationship between oral chronic graft-versus- host disease and global measures of quality of life. Oral Oncol. 2015, 51, 944–949. [Google Scholar] [CrossRef]
- Fall-Dickson, J.; Mitchell, S.; Marden, S.; Ramsay, E.; Guadagnini, J.; Wu, T.; St John, L.; Pavletic, S. Oral Symptom Intensity, Health-Related Quality of Life, and Correlative Salivary Cytokines in Adult Survivors of Hematopoietic Stem Cell Transplantation with Oral Chronic Graft-Versus-Host Disease. Physiol. Behav. 2010, 16, 948–956. [Google Scholar] [CrossRef]
- Bardellini, E.; Amadori, F.; Conti, G.; Veneri, F.; Majorana, A. Effectiveness of a spray containing 1% malic acid in patients with xerostomia induced by graft-versus-host disease. Med. Oral Patol. Oral Cir. Bucal 2019, 24, e190–e194. [Google Scholar] [CrossRef]
- Bassim, C.W.; Fassil, H.; Mays, J.W.; Edwards, D.; Baird, K.; Steinberg, S.M.; Cowen, E.W.; Naik, H.; Datiles, M.; Stratton, P.; et al. Oral disease profiles in chronic graft versus host disease. J. Dent. Res. 2015, 94, 547–554. [Google Scholar] [CrossRef]
- Castellarin, P.; Stevenson, K.; Biasotto, M.; Yuan, A.; Woo, S.B.; Treister, N.S. Extensive Dental Caries in Patients with Oral Chronic Graft-versus-Host Disease. Biol. Blood Marrow Transplant. 2012, 18, 1573–1579. [Google Scholar] [CrossRef]
- The STROBE Guidelines. Available online: https://www.strobe-statement.org/ (accessed on 16 February 2025).
- Caceda, J.H.; Jiang, S.; Calderon, V.; Villavicencio-Caparo, E. Sensitivity and specificity of the ICDAS II system and bitewing radiographs for detecting occlusal caries using the SpectraTM caries detection system as the reference test in children. BMC Oral Health 2023, 23, 896. [Google Scholar] [CrossRef]
- Christian, B.; Amezdroz, E.; Calache, H.; Gussy, M.; Sore, R.; Waters, E. Examiner calibration in caries detection for populations and settings where in vivo calibration is not practical. Community Dent. Health 2017, 34, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.; Eggertsson, H.; Powell, B.; Mandelaris, J.; Ntragatakis, M.; Richardson, T.; Ferretti, G. Dental examiners consistency in applying the ICDAS criteria for a caries prevention community trial. Community Dent. Health 2011, 28, 238–242. [Google Scholar] [PubMed]
- Rener-Sitar, K.; Petričević, N.; Čelebić, A.; Marion, L. Psychometric Properties of Croatian and Slovenian Short Form of Oral Health Impact Profile Questionnaires. Croat. Med. J. 2008, 49, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Rener-Sitar, K.; Čelebić, A.; Stipetić, J.; Marion, L.; Petričević, N.; Zaletel-Kragelj, L. Oral health related quality of life in Slovenian patients with craniomandibular disorders. Coll. Antropol. 2008, 32, 513–517. [Google Scholar]
- Bergdahl, M. Salivary flow and oral complaints in adult dental patients. Community Dent Oral. Epidemiol. 2000, 28, 59–66. [Google Scholar] [CrossRef]
- Levy, S.; Nagler, A.; Okon, S.; Marmary, Y. Parotid salivary gland dysfunction in chronic graft-versus-host disease (cGVHD): A longitudinal study in a mouse model. Bone Marrow Transplant. 2000, 25, 1073–1078. [Google Scholar] [CrossRef]
- Daikeler, T.; Mauramo, M.; Rovó, A.; Stern, M.; Halter, J.; Buser, A.; Tyndall, A.; Häusermann, P.; Gratwohl, A.; Tichelli, A.; et al. Sicca symptoms and their impact on quality of life among very long-term survivors after hematopoietic SCT. Bone Marrow Transplant. 2013, 48, 988–993. [Google Scholar] [CrossRef]
- Rødseth, S.C.; Høvik, H.; Bjertness, E.; Skudutyte-Rysstad, R. Is Poor Self-Rated Health Associated with Higher Caries Experience in Adults? The HUNT4 Oral Health Study. Caries Res. 2024; online ahead of print. [Google Scholar] [CrossRef]
- Silva, M.P.; Vettore, M.V.; Rebelo, M.A.B.; Rebelo Vieira, J.M.; Herkrath, A.P.C.D.Q.; De Queiroz, A.C.; Herkrath, F.J.; Pereira, J.V. Clinical Consequences of Untreated Dental Caries, Individual Characteristics, and Environmental Factors on Self-Reported Oral Health Measures in Adolescents: A Follow-Up Prevalence Study. Caries Res. 2020, 54, 176–184. [Google Scholar] [CrossRef]
- Leal, S.C.; Bronkhorst, E.M.; Fan, M.; Frencken, J.E. Untreated cavitated dentine lesions: Impact on children’s quality of life. Caries Res. 2012, 46, 102–106. [Google Scholar] [CrossRef]
- Alanzi, A.; Husain, F.; Husain, H.; Hanif, A.; Baskaradoss, J. Does the severity of untreated dental caries of preschool children influence the oral health-related quality of life? BMC Oral Health 2023, 23, 552. [Google Scholar] [CrossRef]
- Lee, S.J.; Kim, H.T.; Ho, V.T.; Cutler, C.; Alyea, E.P.; Soiffer, R.J.; Antin, J.H. Quality of life associated with acute and chronic graft-versus-host disease. Bone Marrow Transplant. 2006, 38, 305–310. [Google Scholar] [CrossRef]
- Janicsák, H.; Ungvari, G.S.; Gazdag, G. Psychosocial aspects of hematopoietic stem cell transplantation. World J. Transplant. 2021, 11, 263–276. [Google Scholar] [CrossRef] [PubMed]
- Epstein, J.B.; Scully, C. The role of saliva in oral health and the causes and effects of xerostomia. J. Can. Dent. Assoc. 1992, 58, 217–221. [Google Scholar] [PubMed]
- Santos-Silva, A.R.; Feio, P.d.S.Q.; Vargas, P.A.; Correa, M.E.P.; Lopes, M.A. cGVHD-related caries and its shared features with other ‘dry-mouth’-related caries. Braz. Dent. J. 2015, 26, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Bishop, M.M. Psychosocial Sequelae of Hematopoietic Cell Transplantation in Survivors and Caregivers. Biol. Blood Marrow Transplant. 2009, 15, 29–32. [Google Scholar] [CrossRef]
- Syrjala, K.L.; Langer, S.L.; Abrams, J.R.; Storer, B.; Sanders, J.E.; Flowers, M.E.D.; Martin, P.J. Recovery and long-term function after hematopoietic cell transplantation for leukemia or lymphoma. JAMA 2004, 291, 2335–2343. [Google Scholar] [CrossRef]
- Wong, F.L.; Francisco, L.; Togawa, K.; Bosworth, A.; Gonzales, M.; Hanby, C.; Sabado, M.; Grant, M.; Forman, S.J.; Bhatia, S. Long-term recovery after hematopoietic cell transplantation: Predictors of quality-of-life concerns. Blood 2010, 115, 2508–2519. [Google Scholar] [CrossRef]
- Wingard, J.R.; Huang, I.C.; Sobocinski, K.A.; Andrykowski, M.A.; Cella, D.; Rizzo, J.D.; Brady, M.; Horowitz, M.M.; Bishop, M.M. Factors Associated with Self-Reported Physical and Mental Health after Hematopoietic Cell Transplantation. Biol. Blood Marrow Transplant. 2010, 16, 1682–1692. [Google Scholar] [CrossRef]
- Mosher, C.E.; Duhamel, K.N.; Rini, C.M.; Li, Y.; Isola, L.; Labay, L.; Rowley, S.; Papadopoulos, E.; Moskowitz, C.; Scigliano, E.; et al. Barriers to mental health service use among hematopoietic SCT survivors. Bone Marrow Transplant. 2010, 45, 570–579. [Google Scholar] [CrossRef]
- Vovk, N.; Urek, M.; Cankar, K.; Nemeth, L. Oral health-related quality of life in patients with chronic graft-versus- host disease. In Proceedings of the 71st International Congress of the Organisation for Caries Research (ORCA), Heraklion, Crete, Greece, 3−6 July 2024. [Google Scholar]

| Frequency (N) | % | Mean (SD) | Median (25%, 75% Percentiles) | |
|---|---|---|---|---|
| Age | 22 | 45.05 (14.66) | 47.5 (25% 29.75, 75% 58.25) | |
| Gender | ||||
| Male | 10 | 45.45 | ||
| Female | 12 | 54.55 | ||
| BMI | 22 | 22.86 (4.13) | 22.5 (25% 20.05, 75% 25.63) | |
| Race | ||||
| Caucasian | 22 | |||
| Smoking | ||||
| Yes | 0 | 0 | ||
| No | 22 | 100 | ||
| Diagnosis | ||||
| Acute myeloid leukaemia | 14 | 63.64 | ||
| Acute lymphoblastic leukaemia | 6 | 27.27 | ||
| Mielodysplastic syndrome | 1 | 4.55 | ||
| Non-Hodkin lymphoma | 1 | 4.55 | ||
| Time since transplant (months) | 22 | 27.55 (48.87) | ||
| NIH cGVHD Global Rating | ||||
| Mild | 15 | 68.18 | ||
| Moderate | 5 | 22.73 | ||
| Severe | 2 | 0.09 |
| Domain Score | Mean (SD) | Median (25%, 75% Percentiles) |
|---|---|---|
| Self-reported oral health | 2.21 (0.9) | 3 (25% 2, 75% 3) |
| Self-reported oral aesthetic | 2.09 (0.86) | 2 (25% 2, 75% 3) |
| Functional limitation | 10.50 (7) | 9 (25% 6, 75% 15) |
| Physical pain | 6.95 (4.69) | 5 (25% 4.5, 75% 11.5) |
| Psychological discomfort | 7.09 (5.33) | 5 (25% 4, 75% 10.5) |
| Physical disability | 7.01 (6.93) | 5 (25% 0.5, 75% 11.5) |
| Psychological disability | 3.23 (4) | 2 (25% 0.5, 75% 4.5) |
| Social disability | 1.32 (2.17) | 0 (25% 0, 75% 1.5) |
| Handicap | 2.91 (4.15) | 1 (25% 0, 75% 4) |
| OHIP summary score | 40.81 (31.83) | 23 (25% 8, 75% 46.5) |
| N = 21 | pH of Unstimulated Saliva (N = 21) | Unstimulated Salivary Flow Rate (N = 21) | pH of Stimulated Saliva (N = 21) | Stimulated Salivary Flow Rate (N = 21) | Caries Risk (N = 21) |
|---|---|---|---|---|---|
| Self-reported oral health | NS | NS | NS | NS | −0.512 (0.0177) |
| Self-reported oral aesthetic | NS | NS | NS | NS | NS |
| Functional limitation | NS | NS | NS | NS | 0.499 (0.0214) |
| Physical pain | NS | NS | −0.516 (0.0198) | NS | 0.439 (0.0466) |
| Psychological discomfort | NS | −0.442 (0.0447) | −0.495 (0.0266) | NS | 0.622 (0.0026) |
| Physical disability | NS | NS | NS | NS | 0.469 (0.0322) |
| Psychological disability | NS | NS | −0.453 (0.0448) | NS | 0.475 (0.0296) |
| Social disability | NS | NS | NS | NS | NS |
| Handicap | NS | NS | NS | NS | NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vovk, N.; Urek, M.; Cankar, K.; Nemeth, L. Oral Health-Related Quality of Life After Allogeneic Bone Marrow Transplant—A Cross-Sectional Study. Healthcare 2025, 13, 561. https://doi.org/10.3390/healthcare13050561
Vovk N, Urek M, Cankar K, Nemeth L. Oral Health-Related Quality of Life After Allogeneic Bone Marrow Transplant—A Cross-Sectional Study. Healthcare. 2025; 13(5):561. https://doi.org/10.3390/healthcare13050561
Chicago/Turabian StyleVovk, Nina, Manca Urek, Ksenija Cankar, and Lidija Nemeth. 2025. "Oral Health-Related Quality of Life After Allogeneic Bone Marrow Transplant—A Cross-Sectional Study" Healthcare 13, no. 5: 561. https://doi.org/10.3390/healthcare13050561
APA StyleVovk, N., Urek, M., Cankar, K., & Nemeth, L. (2025). Oral Health-Related Quality of Life After Allogeneic Bone Marrow Transplant—A Cross-Sectional Study. Healthcare, 13(5), 561. https://doi.org/10.3390/healthcare13050561







