Effectiveness of Mobile-Based Learning for Nasogastric Tube Intubation Among Medical Students: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Study Procedures
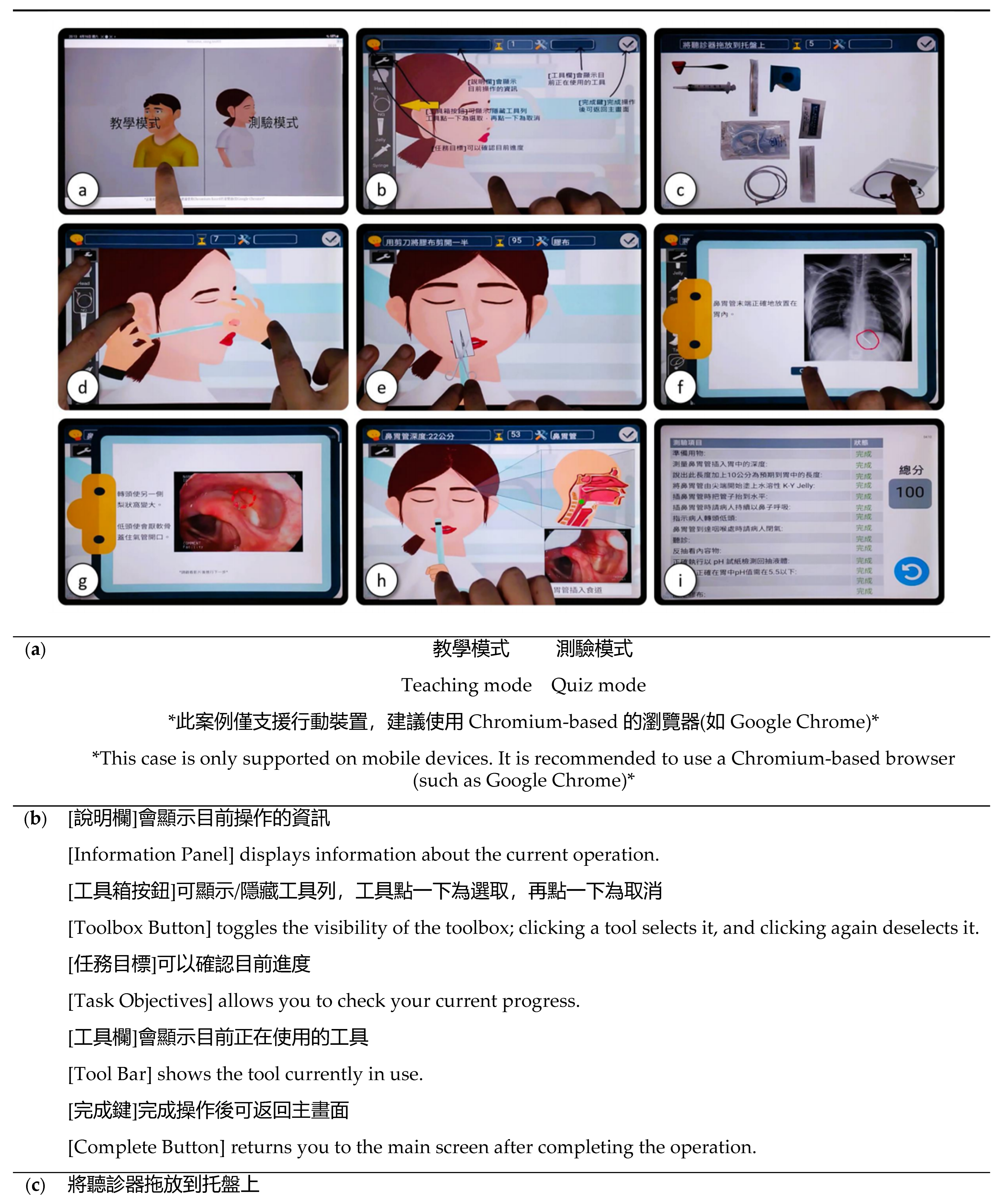
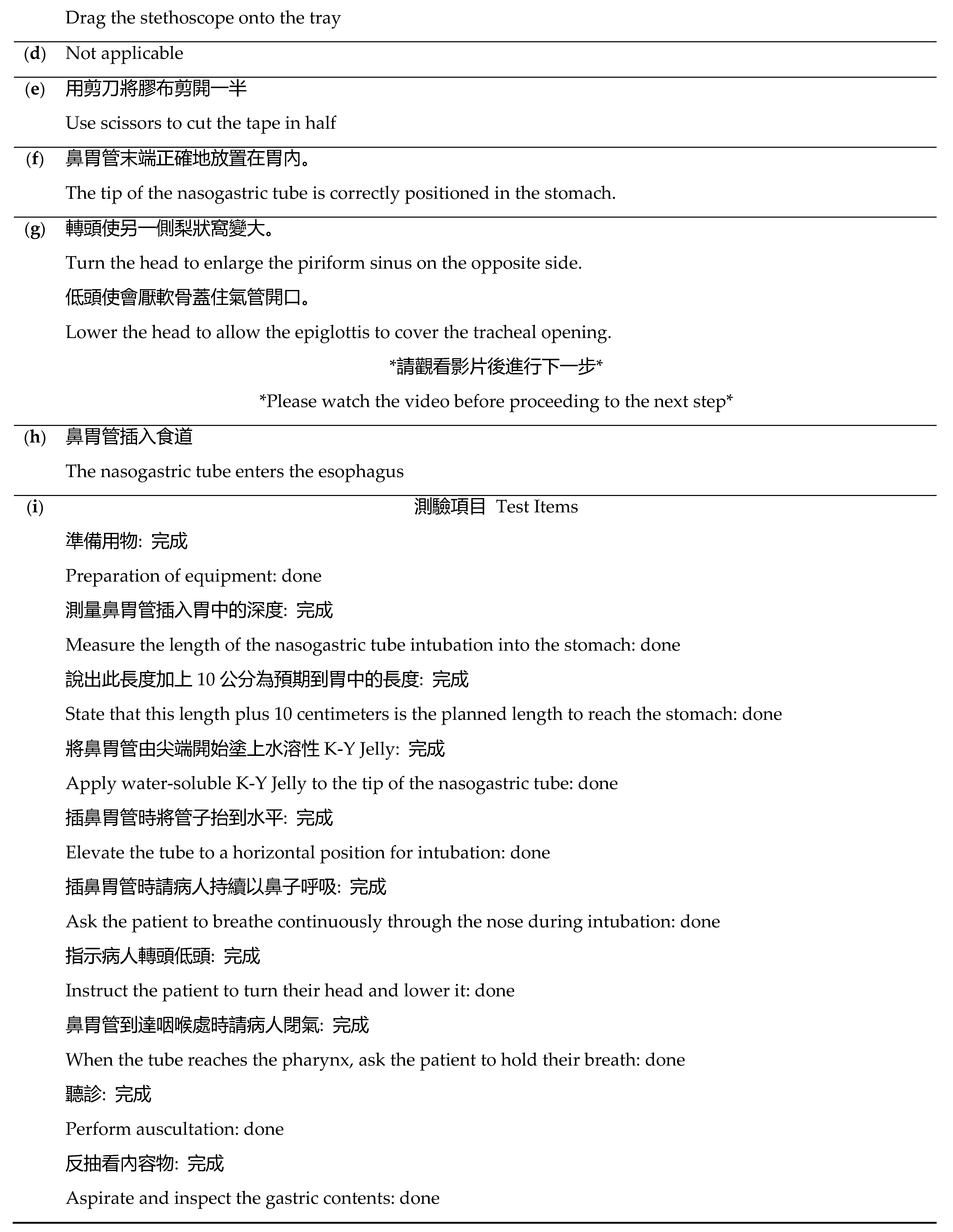
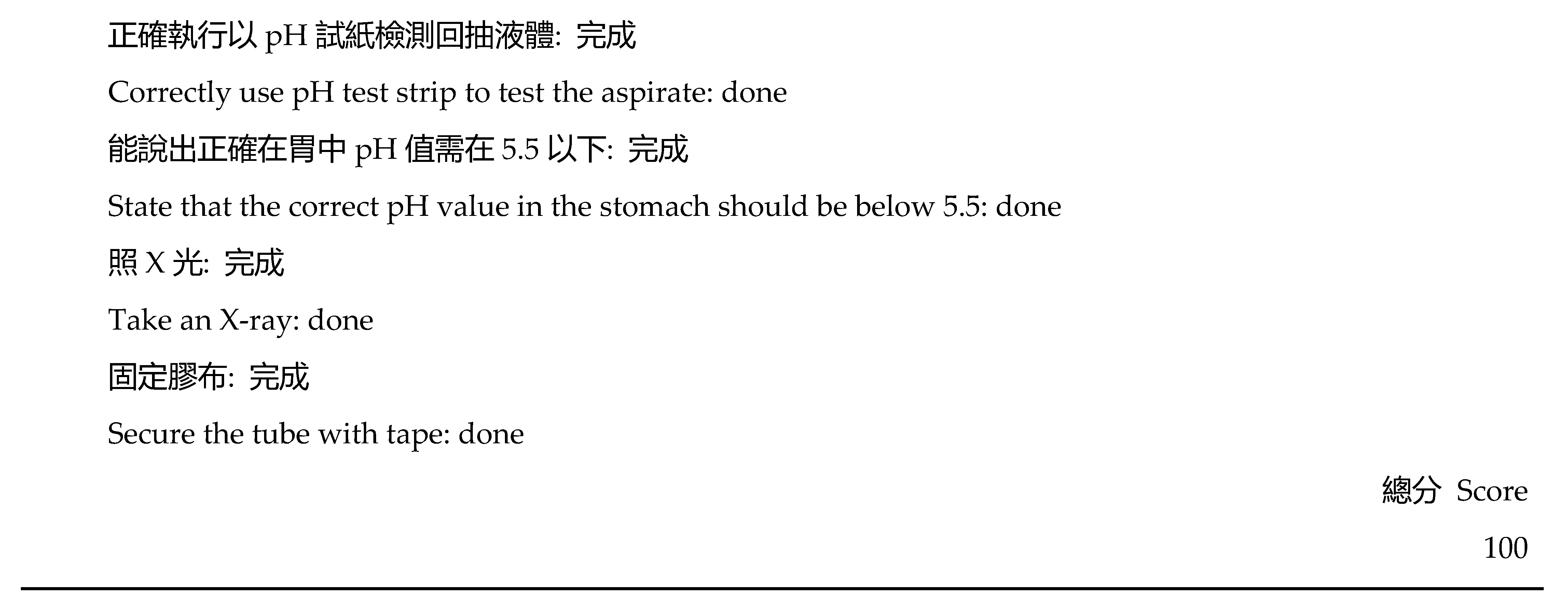
2.3. Mobile-Based Hands-On Learning System for Nasogastric Tube Intubation (MoHoNGT)
2.4. Data Collection and Measurements
2.4.1. The 10-Item Evaluation Questionnaire on NGT Intubation Knowledge
2.4.2. The Confidence Scale
2.4.3. The Objective Structured Clinical Examination (OSCE)
2.5. Statistical Analyses
3. Results
3.1. Participants
3.2. Capability for NGT Intubation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NGT | nasogastric tube |
| MoHoNGT | Mobile-based Hands-on Learning System for Nasogastric Tube Intubation |
| OSCE | objective structured clinical examination |
| SD | standard deviation |
| XR | augmented, virtual, or mixed reality |
| DOPS | direct observation of procedural skills |
References
- Appukutty, J.; Shroff, P.P. Nasogastric Tube Insertion Using Different Techniques in Anesthetized Patients: A Prospective, Randomized Study. Anesth. Analg. 2009, 109, 832–835. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.F.; Luo, C.F.; Illias, A.; Lin, C.C.; Yu, H.P. Nasogastric Tube Insertion in Anesthetized and Intubated Patients: A New and Reliable Method. BMC Gastroenterol. 2012, 12, 99. [Google Scholar] [CrossRef]
- Jonnavithula, N.; Padhy, S.; Ravula, R.; Alekhya, G. Comparison of Ease of Insertion of Nasogastric Tube in Standard Sniffing Position and in Additional Flexion of the Neck: A Randomized Control Trial. Trends Anaesth. Crit. Care 2019, 26–27, 48–51. [Google Scholar] [CrossRef]
- Honda, Y.; Momosaki, R.; Ogata, N. Nasogastric Tube Feeding versus Total Parenteral Nutrition in Older Dysphagic Patients with Pneumonia: Retrospective Cohort Study. J. Nutr. Health Aging 2020, 24, 883–887. [Google Scholar] [CrossRef] [PubMed]
- Taylor, B.E.; McClave, S.A.; Martindale, R.G.; Warren, M.M.; Johnson, D.R.; Braunschweig, C.; McCarthy, M.S.; Davanos, E.; Rice, T.W.; Cresci, G.A.; et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). Crit. Care Med. 2016, 44, 390–438. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.M. Simulation in Undergraduate Mental Health Nursing Education: A Literature Review. Clin. Simul. Nurs. 2015, 11, 445–449. [Google Scholar] [CrossRef]
- Herrmann-Werner, A.; Nikendei, C.; Keifenheim, K.; Bosse, H.M.; Lund, F.; Wagner, R.; Celebi, N.; Zipfel, S.; Weyrich, P. “best Practice” Skills Lab Training vs. a “See One, Do One” Approach in Undergraduate Medical Education: An RCT on Students’ Long-Term Ability to Perform Procedural Clinical Skills. PLoS ONE 2013, 8, e76354. [Google Scholar] [CrossRef]
- Snyder, C.W.; Vandromme, M.J.; Tyra, S.L.; Hawn, M.T. Retention of Colonoscopy Skills after Virtual Reality Simulator Training by Independent and Proctored Methods. Am. Surg. 2010, 76, 743–746. [Google Scholar] [CrossRef]
- Nagayo, Y.; Saito, T.; Oyama, H. A Novel Suture Training System for Open Surgery Replicating Procedures Performed by Experts Using Augmented Reality. J. Med. Syst. 2021, 45, 60. [Google Scholar] [CrossRef]
- Nagayo, Y.; Saito, T.; Oyama, H. Augmented Reality Self-Training System for Suturing in Open Surgery: A Randomized Controlled Trial. Int. J. Surg. 2022, 102, 106650. [Google Scholar] [CrossRef]
- Crompton, H. A Historical Overview of M-Learning: Toward Learner-Centered Education. In Handbook of Mobile Learning; Routledge: London, UK, 2013; ISBN 978-0-203-11876-4. [Google Scholar]
- Yamada, T.; Suda, H.; Yoshitake, A.; Shimizu, H. Development of an Automated Smartphone-Based Suture Evaluation System. J. Surg. Educ. 2022, 79, 802–808. [Google Scholar] [CrossRef] [PubMed]
- Castillo-Segura, P.; Fernández-Panadero, C.; Alario-Hoyos, C.; Muñoz-Merino, P.J.; Delgado Kloos, C. A Cost-Effective IoT Learning Environment for the Training and Assessment of Surgical Technical Skills with Visual Learning Analytics. J. Biomed. Inform. 2021, 124, 103952. [Google Scholar] [CrossRef] [PubMed]
- Lytras, M.; Sarirete, A.; Damiani, E. Technology-Enhanced Learning Research in Higher Education: A Transformative Education Primer. Comput. Hum. Behav. 2020, 109, 106350. [Google Scholar] [CrossRef]
- Yilar Erkek, Z.; Öztürk Altinayak, S. The Effect of Simulation Teaching Technique on the Improvement of Episiotomy Performance Skills and State Anxiety of Midwifery Students in Turkey: RCT. Clin. Simul. Nurs. 2021, 54, 62–69. [Google Scholar] [CrossRef]
- Harris, S.E. Silicone Skin Trays: An Innovative Simulation Approach to Nurse Practitioner Skills Training. Clin. Simul. Nurs. 2020, 49, 28–31. [Google Scholar] [CrossRef]
- Su, J.M.; Wu, C.Y.; Hong, W.T.; Chen, P.S.; Hung, K.S.; Wang, C.J. Application of Mobile-Based Web App to Enhance Simple Suturing Skills of Nurse Practitioners. Nurse Educ. Today 2023, 131, 105959. [Google Scholar] [CrossRef]
- Su, J.M.; Huang, W.L.; Huang, H.C.; Tseng, Y.L.; Li, M.J. A Scenario-Based Web App to Facilitate Patient Education in Lung Tumor Patients Undergoing Video-Assisted Thoracoscopic Surgery: Development and Usability Testing. Digit. Health 2024, 10, 20552076241239244. [Google Scholar] [CrossRef]
- Kim, H.; Suh, E.E. The Effects of an Interactive Nursing Skills Mobile Application on Nursing Students’ Knowledge, Self-Efficacy, and Skills Performance: A Randomized Controlled Trial. Asian Nurs. Res. 2018, 12, 17–25. [Google Scholar] [CrossRef]
- Floren, L.C.; Mandal, J.; Dall’Era, M.; Shin, J.; Irby, D.M.; Cate, O.T.; O’Brien, B.C. A Mobile Learning Module to Support Interprofessional Knowledge Construction in the Health Professions. Am. J. Pharm. Educ. 2020, 84, 847519. [Google Scholar] [CrossRef]
- Talan, T. The Effect of Mobile Learning on Learning Performance: A Meta-Analysis Study. Educ. Sci. Theory Pract. 2020, 20, 79–103. [Google Scholar] [CrossRef]
- Su, J.M. Deeply Interactive Virtual Environment (DIVE). Available online: https://dive.nutn.edu.tw (accessed on 2 July 2024).
- Chen, C.J.; Hung, D.S.Y.; Wu, M.H.; Lee, H.F.; Chen, N.C.; Yang, H.C.; Hung, Y.H. Effectiveness of Positioning in Unconscious Adults during Nasogastric Intubation on Correct Placement and Intubation Time: A Systematic Review and Meta-Analysis. Gastroenterol. Nurs. 2022, 45, 395–406. [Google Scholar] [CrossRef]
- Levin, A.S.; Haq, I.U.; LaPorte, D.M. Pre-Course Cognitive Training Using a Smartphone Application in Orthopaedic Intern Surgical Skills “Boot Camps”. J. Orthop. 2018, 15, 506–508. [Google Scholar] [CrossRef] [PubMed]
- Adams, N.E. Bloom’s Taxonomy of Cognitive Learning Objectives. J. Med. Libr. Assoc. JMLA 2015, 103, 152–153. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.N.; Merkebu, J. The Kirkpatrick Model: A Tool for Evaluating Educational Research. Fam. Med. 2024, 56, 403. [Google Scholar] [CrossRef]
- Grundy, S.E. The Confidence Scale: Development and Psychometric Characteristics. Nurse Educ. 1993, 18, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Shorey, S.; Ang, E.; Baridwan, Ns.S.; Bonito, S.R.; Dones, L.B.P.; Flores, J.L.A.; Freedman-Doan, R.; Fukahori, H.; Hirooka, K.; Koy, V.; et al. Salutogenesis and COVID-19 Pandemic Impacting Nursing Education across SEANERN Affiliated Universities: A Multi-National Study. Nurse Educ. Today 2022, 110, 105277. [Google Scholar] [CrossRef]
- Ribeiro, L.M.C.; Moura, A.S. ‘Hands-on’ Ideas to Provide Student-Targeted Clinical Reasoning Educational Interventions. Med. Educ. 2020, 54, 680–682. [Google Scholar] [CrossRef]
- Richmond, A.; Cooper, N.; Gay, S.; Atiomo, W.; Patel, R. The Student Is Key: A Realist Review of Educational Interventions to Develop Analytical and Non-Analytical Clinical Reasoning Ability. Med. Educ. 2020, 54, 709–719. [Google Scholar] [CrossRef]
- Hoopes, S.; Pham, T.; Lindo, F.M.; Antosh, D.D. Home Surgical Skill Training Resources for Obstetrics and Gynecology Trainees during a Pandemic. Obstet. Gynecol. 2020, 136, 56–64. [Google Scholar] [CrossRef]
- Yari, S.S.; Jandhyala, C.K.; Sharareh, B.; Athiviraham, A.; Shybut, T.B. Efficacy of a Virtual Arthroscopic Simulator for Orthopaedic Surgery Residents by Year in Training. Orthop. J. Sports Med. 2018, 6, 2325967118810176. [Google Scholar] [CrossRef]
- Sadeghi, A.H.; Mathari, S.E.; Abjigitova, D.; Maat, A.P.W.M.; Taverne, Y.J.H.J.; Bogers, A.J.J.C.; Mahtab, E.A.F. Current and Future Applications of Virtual, Augmented, and Mixed Reality in Cardiothoracic Surgery. Ann. Thorac. Surg. 2022, 113, 681–691. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.E.; Kimble, L.P.; Gunby, S.S.; Davis, A.H. Using Deliberate Practice and Simulation for Psychomotor Skill Competency Acquisition and Retention: A Mixed-Methods Study. Nurse Educ. 2020, 45, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Masili, G. No-Code Development Platforms: Breaking the Boundaries between IT and Business Experts. Int. J. Econ. Behav. (IJEB) 2023, 13, 33–49. [Google Scholar] [CrossRef]
- Woo, M. The Rise of No/Low Code Software Development—No Experience Needed? Engineering 2020, 6, 960–961. [Google Scholar] [CrossRef]
- Yoon, C.; Lim, D. An Empirical Study on Factors Affecting Customers’ Acceptance of Internet-Only Banks in Korea. Cogent Bus. Manag. 2020, 7, 1792259. [Google Scholar] [CrossRef]
- Al-Emran, M.; Mezhuyev, V.; Kamaludin, A. Technology Acceptance Model in M-Learning Context: A Systematic Review. Comput. Educ. 2018, 125, 389–412. [Google Scholar] [CrossRef]
- Massoth, C.; Röder, H.; Ohlenburg, H.; Hessler, M.; Zarbock, A.; Pöpping, D.M.; Wenk, M. High-Fidelity Is Not Superior to Low-Fidelity Simulation but Leads to Overconfidence in Medical Students. BMC Med. Educ. 2019, 19, 29. [Google Scholar] [CrossRef]

| Total (n = 73) | MoHoNGT Group (n = 32) | Control Group (n = 41) | p | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Gender | 0.21 | ||||||
| Male | 48 | 65.8 | 24 | 75 | 24 | 58.5 | |
| Female | 25 | 34.2 | 8 | 25 | 17 | 41.5 | |
| Smartphone usage | 0.15 | ||||||
| <3 h/day | 25 | 34.2 | 14 | 43.8 | 11 | 26.8 | |
| ≥3 h/day | 48 | 65.8 | 18 | 56.3 | 30 | 73.2 | |
| Previous e-learning experience in NGT intubation | 0.28 | ||||||
| Yes | 9 | 12.3 | 2 | 6.3 | 7 | 17.1 | |
| No | 64 | 87.7 | 30 | 93.7 | 34 | 82.9 | |
| MoHoNGT Group (n = 32) | Control Group (n = 41) | p | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| NGT intubation knowledge | |||||
| Pre-study | 30.31 | 11.21 | 27.56 | 11.35 | 0.31 |
| Post-study | 69.06 | 15.32 | 49.02 | 14.80 | <0.001 * |
| Within-group differences (t) | 13.04 * | 8.32 * | |||
| Improvement a | 38.75 | 16.8 | 21.46 | 16.52 | <0.001 * |
| The confidence scale | |||||
| Pre-study | 9.44 | 6.14 | 11.49 | 5.86 | 0.15 |
| Post-study | 17.94 | 4.06 | 16.66 | 5.35 | 0.65 |
| Within-group differences (t) | 6.39 * | 5.76 * | |||
| Improvement a | 8.50 | 7.53 | 5.17 | 5.75 | 0.04 * |
| OSCE | |||||
| Post-study | 98.81 | 5.39 | 91.18 | 14.93 | 0.003 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, M.-H.; Chen, C.-J.; Lee, H.-F. Effectiveness of Mobile-Based Learning for Nasogastric Tube Intubation Among Medical Students: A Randomized Controlled Trial. Healthcare 2025, 13, 546. https://doi.org/10.3390/healthcare13050546
Wu M-H, Chen C-J, Lee H-F. Effectiveness of Mobile-Based Learning for Nasogastric Tube Intubation Among Medical Students: A Randomized Controlled Trial. Healthcare. 2025; 13(5):546. https://doi.org/10.3390/healthcare13050546
Chicago/Turabian StyleWu, Ming-Hsuan, Chen-Ju Chen, and Huan-Fang Lee. 2025. "Effectiveness of Mobile-Based Learning for Nasogastric Tube Intubation Among Medical Students: A Randomized Controlled Trial" Healthcare 13, no. 5: 546. https://doi.org/10.3390/healthcare13050546
APA StyleWu, M.-H., Chen, C.-J., & Lee, H.-F. (2025). Effectiveness of Mobile-Based Learning for Nasogastric Tube Intubation Among Medical Students: A Randomized Controlled Trial. Healthcare, 13(5), 546. https://doi.org/10.3390/healthcare13050546






