Autonomic Balance Differences Through Heart Rate Variability Between Adults with and Without Chronic Low Back Pain
Abstract
1. Introduction
2. Materials and Methods
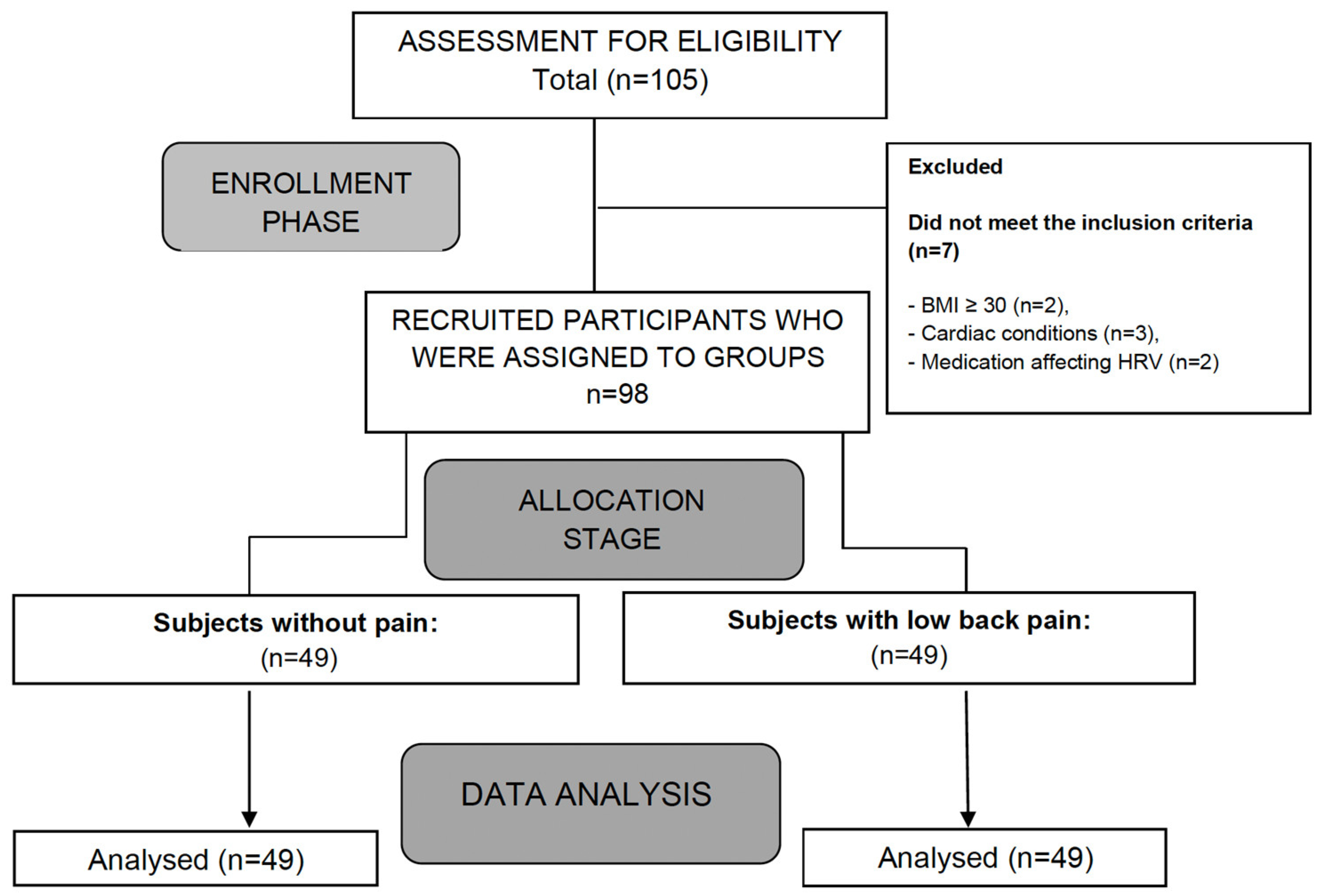
2.1. Study Design
2.2. Participants
2.3. Outcome Measures
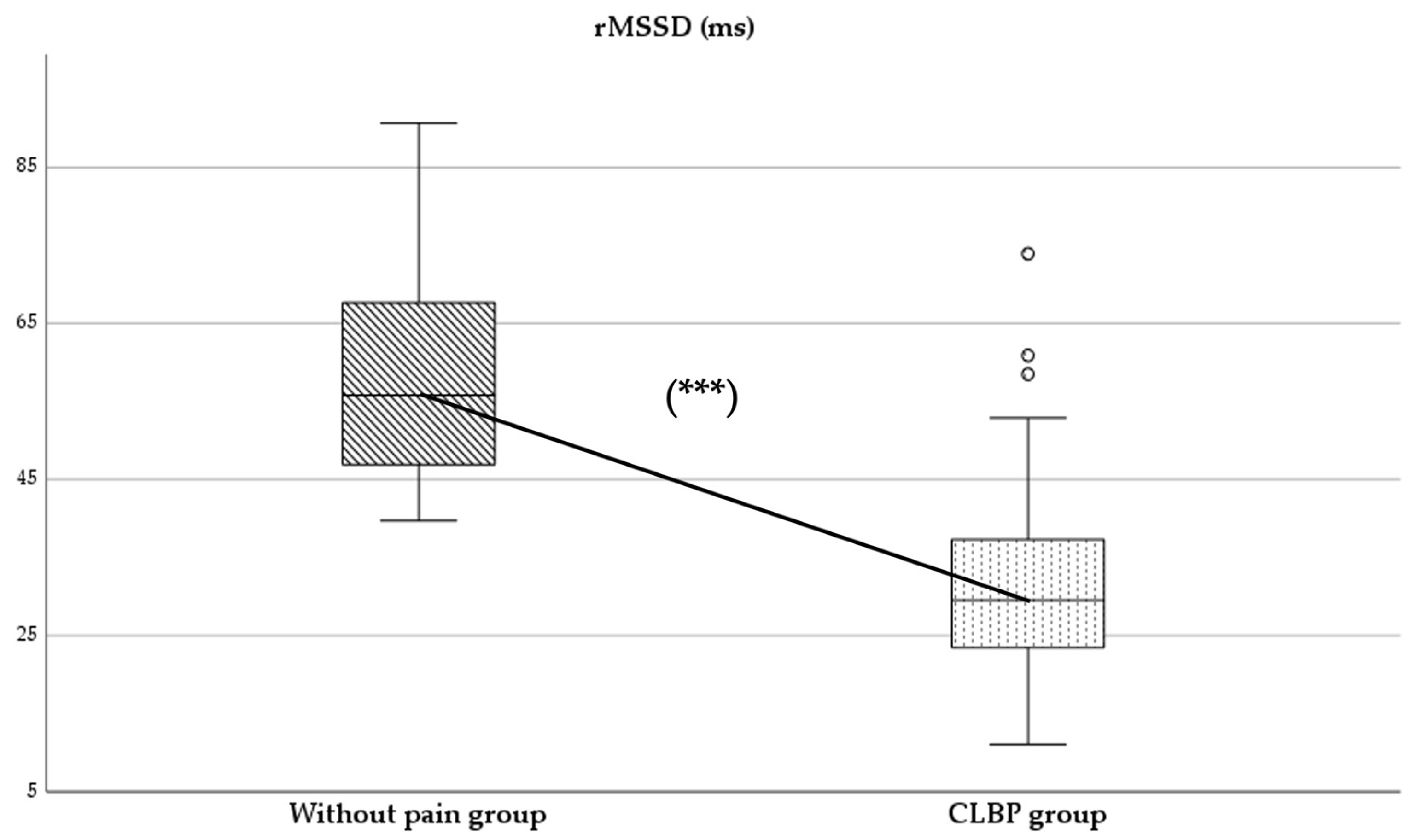
- rMSSD (root mean square of successive differences) (ms): This parameter represents the square root of the average of the sum of the squared differences between normal adjacent RR intervals. It reflects short-term variability and is directly associated with parasympathetic nervous system (PNS) activity. Higher rMSSD values indicate greater parasympathetic modulation [10,23].
- Sympathetic/parasympathetic ratio (S:PS): This ratio, also described by Naranjo-Orellana et al. [25], is calculated as the quotient of SS and SD1. It reflects the balance between sympathetic and parasympathetic activity, with higher values indicating a predominance of sympathetic activity.
2.4. Sample Size
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Clinical Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Otero-Ketterer, E.; Peñacoba-Puente, C.; Pinheiro-Araujo, C.F.; Valera-Calero, J.A.; Ortega-Santiago, R. Biopsychosocial factors for chronicity in individuals with non-specific low back pain: An umbrella review. Int. J. Environ. Res. Public Health 2022, 19, 10145. [Google Scholar] [CrossRef]
- Tracy, L.M.; Ioannou, L.; Baker, K.S.; Gibson, S.J.; Georgiou-Karistianis, N.; Giummarra, M.J. Meta-analytic evidence for decreased heart rate variability in chronic pain implicating parasympathetic nervous system dysregulation. Pain 2016, 157, 7–29. [Google Scholar] [CrossRef] [PubMed]
- Hashmi, J.A.; Baliki, M.N.; Huang, L.; Baria, A.T.; Torbey, S.; Hermann, K.M.; Schnitzer, T.J.; Apkarian, A.V. Shape shifting pain: Chronification of back pain shifts brain representation from nociceptive to emotional circuits. Brain 2013, 136, 2751–2768. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.W.; Massé, N.; Kimmerly, D.S.; Menon, R.S.; Shoemaker, J.K. Ventral medial prefrontal cortex and cardiovagal control in conscious humans. Neuroimage 2007, 35, 698–708. [Google Scholar] [CrossRef] [PubMed]
- Koenig, J.; Loerbroks, A.; Jarczok, M.N.; Fischer, J.E.; Thayer, J.F. Chronic pain and heart rate variability in a cross-sectional occupational sample: Evidence for impaired vagal control. Clin. J. Pain 2016, 32, 218–225. [Google Scholar] [CrossRef]
- Bandeira, P.M.; Reis, F.J.; Sequeira, V.C.; Chaves, A.C.; Fernandes, O.; Arruda-Sanchez, T. Heart rate variability in patients with low back pain: A systematic review. Scand. J. Pain 2021, 21, 426–433. [Google Scholar] [CrossRef]
- Telles, S.; Sharma, S.K.; Gupta, R.K.; Bhardwaj, A.K.; Balkrishna, A. Heart rate variability in chronic low back pain patients randomized to yoga or standard care. BMC Complement Altern. Med. 2016, 16, 279. [Google Scholar] [CrossRef] [PubMed]
- Catai, A.M.; Pastre, C.M.; de Godoy, M.F.; da Silva, E.; Takahashi, A.C.d.M.; Vanderlei, L.C.M. Heart rate variability: Are you using it properly? Standardisation checklist of procedures. Braz. J. Phys. Ther. 2020, 24, 91–102. [Google Scholar] [CrossRef] [PubMed]
- Camm, A.J. Heart rate variability. Standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur. Heart J. 1996, 17, 354–381. [Google Scholar]
- Hoshi, R.A.; Pastre, C.M.; Vanderlei, L.C.M.; Godoy, M.F. Poincaré plot indexes of heart rate variability: Relationships with other nonlinear variables. Auton. Neurosci. 2013, 177, 197–201. [Google Scholar] [CrossRef]
- Tousignant-Laflamme, Y.; Marchand, S. Sex differences in cardiac and autonomic response to clinical and experimental pain in LBP patients. Eur. J. Pain 2006, 10, 603–614. [Google Scholar] [CrossRef]
- Billet, B.; Goudman, L.; Rigoard, P.; Billot, M.; Roulaud, M.; Verstraete, S.; Nagels, W.; Moens, M. Effect of neuromodulation for chronic pain on the autonomic nervous system: A systematic review. BJA Open. 2024, 11, 100305. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Morales, C.; Espejo-Antúnez, L.; Clemente-Suárez, V.J.; Tabla-Hinojosa, F.B.; Albornoz-Cabello, M. Analysis of heart rate variability during emergency flight simulator missions in fighter pilots. BMJ Mil. Health 2024, 170, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Morales, C.; Espejo-Antúnez, L.; Cardero-Durán, M.d.L.Á.; Falla, D.; Moreno-Vázquez, J.M.; Albornoz-Cabello, M. Psychophysiological responses to a multimodal physiotherapy program in fighter pilots with flight-related neck pain: A pilot trial. PLoS ONE 2024, 19, e0306708. [Google Scholar] [CrossRef] [PubMed]
- Espejo-Antúnez, L.; Fernández-Morales, C.; Cardero-Durán, M.Á.; Toledo-Marhuenda, J.V.; Díaz-Mancha, J.A.; Albornoz-Cabello, M. Detection of changes on parameters related to heart rate variability after applying current interferential therapy in subjects with non-specific low back pain. Diagnostics 2021, 11, 2175. [Google Scholar] [CrossRef]
- Main, C.; Sullivan, M.; Watson, P. Pain Management: Practical Applications of the Biopsychosocial Perspective in Clinical and Occupational Settings, 2nd ed.; Churchill Livingstone: London, UK, 2008; ISBN 9780443100697. [Google Scholar]
- Berry, M.E.; Chapple, I.T.; Ginsberg, J.P.; Gleichauf, K.J.; Meyer, J.A.; Nagpal, M.L. Non-pharmacological intervention for chronic pain in veterans: A pilot study of heart rate variability biofeedback. Glob. Adv. Health Med. 2014, 3, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Echeita, J.A.; Preuper, H.R.S.; Dekker, R.; Stuive, I.; Timmerman, H.; Wolff, A.P.; Reneman, M.F. Central sensitisation and functioning in patients with chronic low back pain: Protocol for a cross-sectional and cohort study. BMJ Open 2020, 10, e031592. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Alsufiany, M.B.; Lohman, E.B.; Daher, N.S.; Gang, G.R.; Shallan, A.I.; Jaber, H.M. Non-specific chronic low back pain and physical activity: A comparison of postural control and hip muscle isometric strength: A cross-sectional study. Medicine 2020, 99, e18544. [Google Scholar] [CrossRef] [PubMed]
- Amundsen, P.A.; Evans, D.W.; Rajendran, D.; Bright, P.; Bjørkli, T.; Eldridge, S.; Buchbinder, R.; Underwood, M.; Froud, R. Inclusion and exclusion criteria used in non-specific low back pain trials: A review of randomised controlled trials published between 2006 and 2012. BMC Musculoskelet Disord. 2018, 19, 113. [Google Scholar] [CrossRef]
- Espejo-Antúnez, L.; Fernández-Morales, C.; Hernández-Sánchez, S.; Cardero-Durán, M.d.L.Á.; Toledo-Marhuenda, J.V.; Albornoz-Cabello, M. The impact on the stress-associated autonomic response of physiotherapy students receiving interferential current in an electrotherapy training session. Int. J. Environ. Res. Public Health 2022, 19, 13348. [Google Scholar] [CrossRef]
- Mourot, L.; Bouhaddi, M.; Perrey, S.; Rouillon, J.-D.; Regnard, J. Quantitative Poincaré plot analysis of heart rate variability: Effect of endurance training. Eur. J. Appl. Physiol. 2004, 91, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Brennan, M.; Palaniswami, M.; Kamen, P. Do existing measures of Poincaré plot geometry reflect nonlinear features of heart rate variability? IEEE Trans. Biomed. Eng. 2001, 48, 1342–1347. [Google Scholar] [CrossRef]
- Naranjo-Orellana, J.; De la Cruz-Torres, B.; Sarabia-Cachadiña, E.; De Hoyo, M.; Domínguez-Cobo, S. Two new indexes for the assessment of autonomic balance in elite soccer players. Int. J. Sports Physiol. Perform. 2015, 10, 452–457. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge Academic: New York, NY, USA, 1988. [Google Scholar]
- Sherriff, B.; Clark, C.; Killingback, C.; Newell, D. Impact of contextual factors on patient outcomes following conservative low back pain treatment: Systematic review. Chiropr. Man. Ther. 2022, 30, 1–29. [Google Scholar] [CrossRef] [PubMed]
- Rossettini, G.; Carlino, E.; Testa, M. Clinical relevance of contextual factors as triggers of placebo and nocebo effects in musculoskeletal pain. BMC Musculoskelet. Disord. 2018, 19, 1–15. [Google Scholar] [CrossRef]
- Nunan, D.; Sandercock, G.R.H.; Brodie, D.A. A quantitative systematic review of normal values for short-term heart rate variability in healthy adults. Pacing Clin. Electrophysiol. 2010, 33, 1407–1417. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, N.; Reece, J.; Polus, B.I. Effects of body position on autonomic regulation of cardiovascular function in young, healthy adults. Chiropr. Osteopat. 2007, 15, 19. [Google Scholar] [CrossRef]
- Terkelsen, A.J.; Molgaard, H.; Hansen, J.; Finnerup, N.B.; Kroner, K.; Jensen, T.S. Heart Rate Variability in Complex Regional Pain Syndrome during Rest and Mental and Orthostatic Stress. J. Am. Soc. Anesthesiol. 2012, 116, 133–146. [Google Scholar] [CrossRef]
- Bigand, T.; Wilson, M.; Bindler, R.; Daratha, K. Examining risk for persistent pain among adults with overweight status. Pain Manag. Nurs. 2018, 19, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Miranda, C.M.; de Lima Campos, M.; Leite-Almeida, H. Diet, body weight and pain susceptibility—A systematic review of preclinical studies. Neurobiol. Pain 2021, 10, 100066. [Google Scholar] [CrossRef] [PubMed]
- Amaro-Díaz, L.; Montoro, C.I.; Fischer-Jbali, L.R.; Galvez-Sánchez, C.M. Chronic pain and emotional Stroop: A systematic review. J. Clin. Med. 2022, 11, 3259. [Google Scholar] [CrossRef]
- Lin, I.-M.; Fan, S.-Y.; Yen, C.-F.; Yeh, Y.-C.; Tang, T.-C.; Huang, M.-F.; Liu, T.-L.; Wang, P.-W.; Lin, H.-C.; Tsai, H.-Y.; et al. Heart rate variability biofeedback increased autonomic activation and improved symptoms of depression and insomnia among patients with major depression disorder. Clin. Psychopharmacol. Neurosci. 2019, 17, 222–232. [Google Scholar] [CrossRef]
| Variable | Total Sample (n = 98) | Without-Pain Group (n = 49) | CLBP Group (n = 49) | p-Value * | d |
|---|---|---|---|---|---|
| Age (years) | 38.41 ± 15.18 | 37.71 ± 14.85 | 39.10 ± 15.63 | 0.653 | - |
| Height (cm) | 178.06 ± 6.66 | 178.92 ± 7.10 | 177.49 ± 5.96 | 0.283 | - |
| Weight (kg) | 75.15 ± 12.77 | 73.19 ± 8.61 | 82.30 ± 14.52 | <0.001 ** | 0.8 |
| BMI (kg/m2) | 23.52 ± 2.73 | 22.85 ± 1.86 | 25.27 ± 2.95 | <0.001 ** | 0.9 |
| Min HR (bpm) | 63.07 ± 11.15 | 61.26 ± 8.45 | 66.14 ± 12.87 | 0.029 * | 0.4 |
| Max HR (bpm) | 82.53 ± 12.70 | 100.35 ± 16.54 | 88.90 ± 15.27 | 0.001 * | 0.7 |
| Mean HR (bpm) | 74.52 ± 12.21 | 74.25 ± 11.51 | 75.01 ± 13.05 | 0.763 | - |
| rMSSD (ms) | 45.27 ± 19.53 | 58.98 ± 14.75 | 31.57 ± 13.04 | <0.001 ** | 2 |
| SD1 (ms) | 32.03 ± 14.81 | 40.53 ± 7.92 | 32.57 ± 24.02 | 0.030 * | 0.4 |
| SD2 (ms) | 72.75 ± 26.88 | 90.67 ± 24.27 | 54.84 ± 13.61 | <0.001 ** | 1.8 |
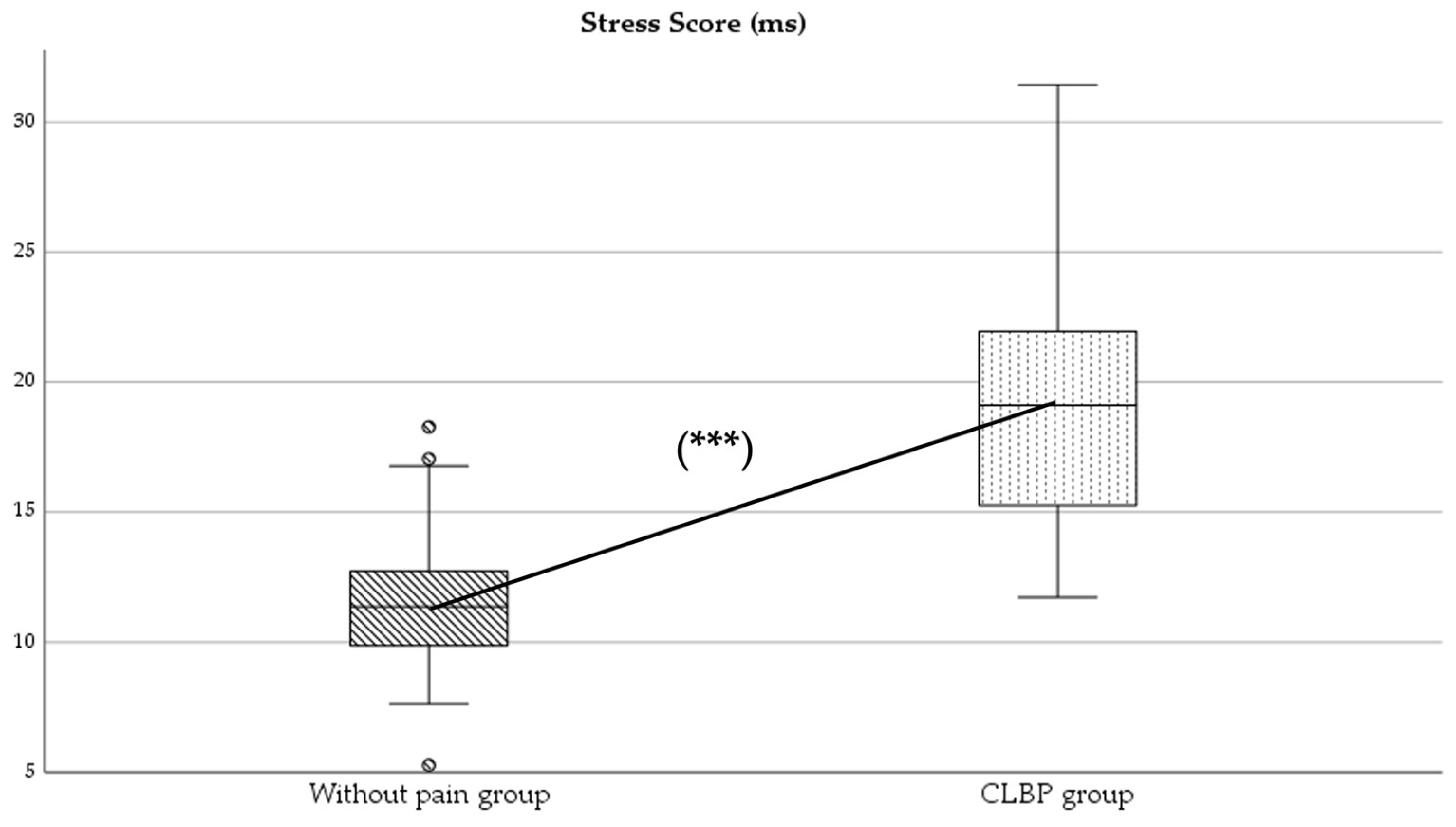
| SS (ms) | 15.78 ± 5.72 | 12.10 ± 3.92 | 19.46 ± 5.27 | <0.001 ** | 1.6 |
| S:PS ratio | 0.61 ± 0.53 | 0.30 ± 0.14 | 0.92 ± 0.60 | <0.001 ** | 1.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-Morales, C.; Espejo-Antúnez, L.; Albornoz-Cabello, M.; Yáñez-Álvarez, Á.R.; Cardero-Durán, M.d.l.Á. Autonomic Balance Differences Through Heart Rate Variability Between Adults with and Without Chronic Low Back Pain. Healthcare 2025, 13, 509. https://doi.org/10.3390/healthcare13050509
Fernández-Morales C, Espejo-Antúnez L, Albornoz-Cabello M, Yáñez-Álvarez ÁR, Cardero-Durán MdlÁ. Autonomic Balance Differences Through Heart Rate Variability Between Adults with and Without Chronic Low Back Pain. Healthcare. 2025; 13(5):509. https://doi.org/10.3390/healthcare13050509
Chicago/Turabian StyleFernández-Morales, Carlos, Luis Espejo-Antúnez, Manuel Albornoz-Cabello, Ángel Rufino Yáñez-Álvarez, and María de los Ángeles Cardero-Durán. 2025. "Autonomic Balance Differences Through Heart Rate Variability Between Adults with and Without Chronic Low Back Pain" Healthcare 13, no. 5: 509. https://doi.org/10.3390/healthcare13050509
APA StyleFernández-Morales, C., Espejo-Antúnez, L., Albornoz-Cabello, M., Yáñez-Álvarez, Á. R., & Cardero-Durán, M. d. l. Á. (2025). Autonomic Balance Differences Through Heart Rate Variability Between Adults with and Without Chronic Low Back Pain. Healthcare, 13(5), 509. https://doi.org/10.3390/healthcare13050509







