Accelerating Recovery: A Case Report on Telerehabilitation for a Triathlete’s Post-Meniscus Surgery Comeback
Abstract
1. Introduction
Objective
2. Case Presentation
2.1. Patient Information
2.2. Preoperative Status
2.3. Intervention
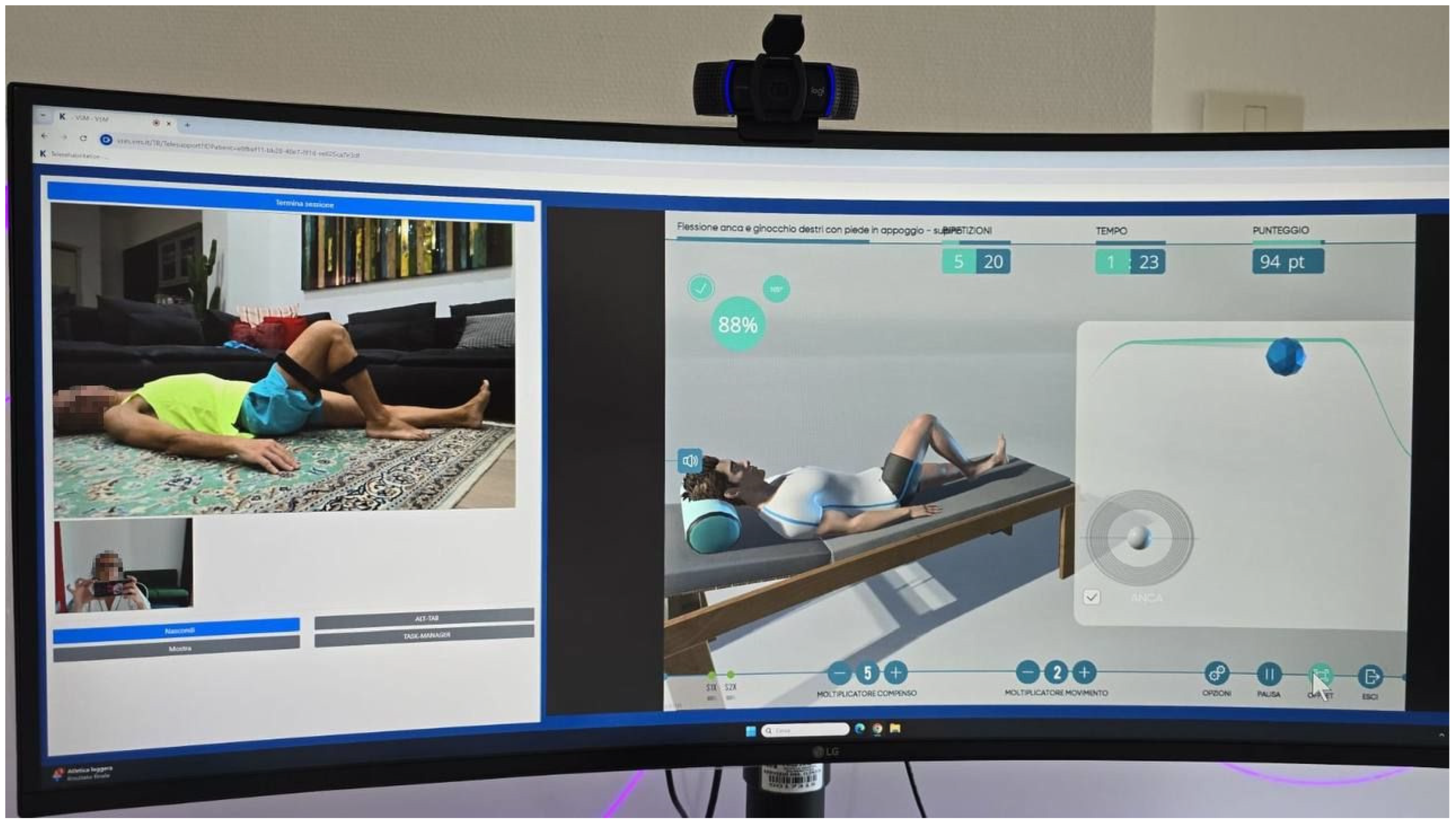
3. Telerehabilitation Program Details
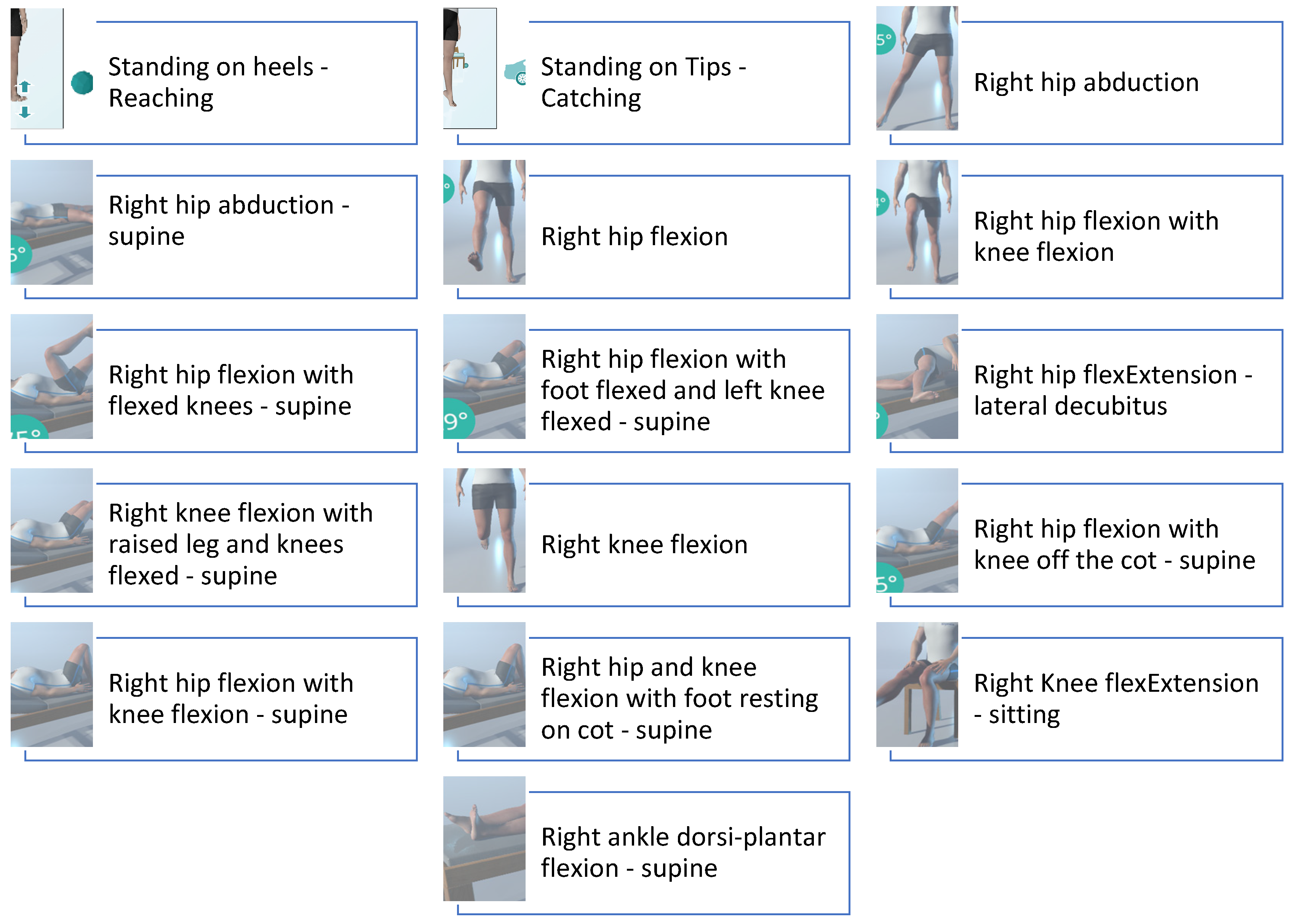
3.1. Phase 1 (Weeks 1–2)
Physiotherapy Assessment
3.2. Phase 2 (Weeks 3–6)
Physiotherapy Assessment
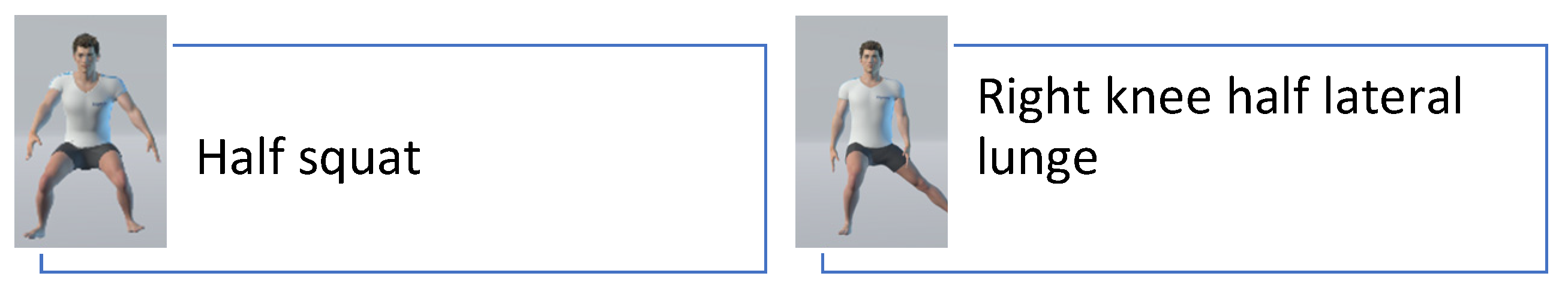
3.3. Phase 3 (Weeks 7–12)
3.3.1. Physiotherapy Assessment
3.3.2. Outcomes
4. Discussion
4.1. Interpretation of Results
- Full ROM in knee extension and flexion by the end of the third phase.
- Restoration of muscle strength, with the vastus medialis scoring 5/5 on the MRC scale.
- Pain-free static and dynamic conditions, with no adverse events reported.
- Successful resumption of triathlon-specific training sessions, including swimming, cycling, and running.
4.2. Role of Data Transmission with Wearable Devices
4.3. Comparison with Traditional In-Person Rehabilitation
5. Conclusions and Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Harput, G.; Guney-Deniz, H.; Nyland, J.; Kocabey, Y. Postoperative rehabilitation and outcomes following arthroscopic isolated meniscus repairs: A systematic review. Phys. Ther. Sport 2020, 45, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Lind, M.; Nielsen, T.; Faunø, P.; Lund, B.; Christiansen, S.E. Free rehabilitation is safe after isolated meniscus repair: A prospective randomized trial comparing free with restricted rehabilitation regimens. Am. J. Sports Med. 2013, 41, 2753–2758. [Google Scholar] [CrossRef] [PubMed]
- Cavanaugh, J.T.; Killian, S.E. Rehabilitation following meniscal repair. Curr. Rev. Musculoskelet. Med. 2012, 5, 46–58. [Google Scholar] [CrossRef] [PubMed]
- Kocabey, Y.; Nyland, J.; Isbell, W.M.; Caborn, D.N. Patient outcomes following T-Fix meniscal repair and a modifiable, progressive rehabilitation program, a retrospective study. Arch. Orthop. Trauma Surg. 2004, 124, 592–596. [Google Scholar] [CrossRef]
- Spang Iii, R.C.; Nasr, M.C.; Mohamadi, A.; DeAngelis, J.P.; Nazarian, A.; Ramappa, A.J. Rehabilitation following meniscal repair: A systematic review. BMJ Open Sport Exerc. Med. 2018, 4, e000212. [Google Scholar] [CrossRef]
- Lal, H.; Mohanta, S.; Kumar, J.; Patralekh, M.K.; Lall, L.; Katariya, H.; Arya, R.K. Telemedicine-Rehabilitation and Virtual Reality in Orthopaedics and Sports Medicine. Indian J. Orthop. 2023, 57, 7–19. [Google Scholar] [CrossRef]
- Bramanti, A.; Ciurleo, R.; Vecchione, C.; Turolla, A.; Piramide, N.; Ciccarelli, M.; Piramide, E.; Garofano, M.; Senatore, M.; Calabrese, M. Telerehabilitation: A Solution for Patients After Hip Fracture? Transl. Med. UniSa 2024, 26, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Gosling, C.M.; Gabbe, B.J.; Forbes, A.B. Triathlon related musculoskeletal injuries: The status of injury prevention knowledge. J. Sci. Med. Sport 2008, 11, 396–406. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.D.; Taylor, J.; Almqvist, K.F.; Erggelet, C.; Knutsen, G.; Garcia Portabella, M.; Smith, T.; Richardson, J.B. Arthroscopic assessment of cartilage repair: A validation study of 2 scoring systems. Arthroscopy 2005, 21, 1462–1467. [Google Scholar] [CrossRef] [PubMed]
- Noyes, F.R.; Barber-Westin, S.D. Arthroscopic repair of meniscus tears extending into the avascular zone with or without anterior cruciate ligament reconstruction in patients 40 years of age and older. Arthroscopy 2000, 16, 822–829. [Google Scholar] [CrossRef] [PubMed]
- Barber, F.A. Accelerated rehabilitation for meniscus repairs. Arthroscopy 1994, 10, 206–210. [Google Scholar] [CrossRef]
- Quesnot, A.; Mouchel, S.; Salah, S.B.; Baranes, I.; Martinez, L.; Billuart, F. Randomized controlled trial of compressive cryotherapy versus standard cryotherapy after total knee arthroplasty: Pain, swelling, range of motion and functional recovery. BMC Musculoskelet. Disord. 2024, 25, 182. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Lu, S.; Sun, J.; Zhou, W.; Liu, H. Thromboprophylactic Efficacy and Safety of Anticoagulants After Arthroscopic Knee Surgery: A Systematic Review and Meta-Analysis. Clin. Appl. Thromb. Hemost. 2019, 25, 1076029619881409. [Google Scholar] [CrossRef] [PubMed]
- Alemanno, F.; Houdayer, E.; Emedoli, D.; Locatelli, M.; Mortini, P.; Mandelli, C.; Raggi, A.; Iannaccone, S. Efficacy of virtual reality to reduce chronic low back pain: Proof-of-concept of a non-pharmacological approach on pain, quality of life, neuropsychological and functional outcome. PLoS ONE 2019, 14, e0216858. [Google Scholar] [CrossRef] [PubMed]
- Contrada, M.; Arcuri, F.; Tonin, P.; Pignolo, L.; Mazza, T.; Nudo, G.; Pignataro, M.L.; Quintieri, M.; Iozzi, A.; Cerasa, A. Stroke Telerehabilitation in Calabria: A Health Technology Assessment. Front. Neurol. 2021, 12, 777608. [Google Scholar] [CrossRef]
- Macchitella, L.; Amendola, S.; Barraco, G.; Scoditti, S.; Gallo, I.; Oliva, M.C.; Trabacca, A. A narrative review of the use of a cutting-edge virtual reality rehabilitation technology in neurological and neuropsychological rehabilitation. NeuroRehabilitation 2023, 53, 439–457. [Google Scholar] [CrossRef]
- Azhar, G.; Wei, J.Y.; Schutzler, S.E.; Coker, K.; Gibson, R.V.; Kirby, M.F.; Ferrando, A.A.; Wolfe, R.R. Daily Consumption of a Specially Formulated Essential Amino Acid-Based Dietary Supplement Improves Physical Performance in Older Adults with Low Physical Functioning. J. Gerontol. Ser. A 2021, 76, 1184–1191. [Google Scholar] [CrossRef] [PubMed]
- Hulmi, J.J.; Lockwood, C.M.; Stout, J.R. Effect of protein/essential amino acids and resistance training on skeletal muscle hypertrophy: A case for whey protein. Nutr. Metab. 2010, 7, 51. [Google Scholar] [CrossRef] [PubMed]
- Howard, E.E.; Pasiakos, S.M.; Fussell, M.A.; Rodriguez, N.R. Skeletal Muscle Disuse Atrophy and the Rehabilitative Role of Protein in Recovery from Musculoskeletal Injury. Adv. Nutr. 2020, 11, 989–1001. [Google Scholar] [CrossRef] [PubMed]
- Smith-Ryan, A.E.; Hirsch, K.R.; Saylor, H.E.; Gould, L.M.; Blue, M.N.M. Nutritional Considerations and Strategies to Facilitate Injury Recovery and Rehabilitation. J. Athl. Train. 2020, 55, 918–930. [Google Scholar] [CrossRef] [PubMed]
- Tipton, K.D. Nutritional Support for Exercise-Induced Injuries. Sports Med. 2015, 45 (Suppl. S1), S93–S104. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, K.R.; Wolfe, R.R.; Ferrando, A.A. Pre- and Post-Surgical Nutrition for Preservation of Muscle Mass, Strength, and Functionality Following Orthopedic Surgery. Nutrients 2021, 13, 1675. [Google Scholar] [CrossRef] [PubMed]
- Burgess, L.C.; Phillips, S.M.; Wainwright, T.W. What Is the Role of Nutritional Supplements in Support of Total Hip Replacement and Total Knee Replacement Surgeries? A Systematic Review. Nutrients 2018, 10, 820. [Google Scholar] [CrossRef] [PubMed]
- Koch, M.; Memmel, C.; Zeman, F.; Pfeifer, C.G.; Zellner, J.; Angele, P.; Weber-Spickschen, S.; Alt, V.; Krutsch, W. Early Functional Rehabilitation after Meniscus Surgery: Are Currently Used Orthopedic Rehabilitation Standards Up to Date? Rehabil. Res. Pract. 2020, 2020, 3989535. [Google Scholar] [CrossRef] [PubMed]
- Marco, C.A.; Marco, A.P.; Plewa, M.C.; Buderer, N.; Bowles, J.; Lee, J. The verbal numeric pain scale: Effects of patient education on self-reports of pain. Acad. Emerg. Med. 2006, 13, 853–859. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McCaffery, M. Teaching your patient to use a pain rating scale. Nursing 2002, 32, 17. [Google Scholar] [CrossRef] [PubMed]
- Marcano-Fernández, F.; Prada, C.; Johal, H. Physical outcome measures: The role of strength and range of motion in orthopaedic research. Injury 2020, 51 (Suppl. S2), S106–S110. [Google Scholar] [CrossRef] [PubMed]
- Berzosa, C.; Comeras-Chueca, C.; Bascuas, P.J.; Gutiérrez, H.; Bataller-Cervero, A.V. Assessing Trail Running Biomechanics: A Comparative Analysis of the Reliability of Stryd(TM) and GARMIN(RP) Wearable Devices. Sensors 2024, 24, 3570. [Google Scholar] [CrossRef] [PubMed]
- Viteckova, S.; Kutilek, P.; Svoboda, Z.; Krupicka, R.; Kauler, J.; Szabo, Z. Gait symmetry measures: A review of current and prospective methods. Biomed. Signal Process. Control 2018, 42, 89–100. [Google Scholar] [CrossRef]
- Henriksen, A.; Haugen Mikalsen, M.; Woldaregay, A.Z.; Muzny, M.; Hartvigsen, G.; Hopstock, L.A.; Grimsgaard, S. Using Fitness Trackers and Smartwatches to Measure Physical Activity in Research: Analysis of Consumer Wrist-Worn Wearables. J. Med. Internet Res. 2018, 20, e110. [Google Scholar] [CrossRef]
- Brooke, S.M.; An, H.S.; Kang, S.K.; Noble, J.M.; Berg, K.E.; Lee, J.M. Concurrent Validity of Wearable Activity Trackers Under Free-Living Conditions. J. Strength Cond. Res. 2017, 31, 1097–1106. [Google Scholar] [CrossRef] [PubMed]
- Claes, J.; Buys, R.; Avila, A.; Finlay, D.; Kennedy, A.; Guldenring, D.; Budts, W.; Cornelissen, V. Validity of heart rate measurements by the Garmin Forerunner 225 at different walking intensities. J. Med. Eng. Technol. 2017, 41, 480–485. [Google Scholar] [CrossRef] [PubMed]
- Gillinov, S.; Etiwy, M.; Wang, R.; Blackburn, G.; Phelan, D.; Gillinov, A.M.; Houghtaling, P.; Javadikasgari, H.; Desai, M.Y. Variable Accuracy of Wearable Heart Rate Monitors during Aerobic Exercise. Med. Sci. Sports Exerc. 2017, 49, 1697–1703. [Google Scholar] [CrossRef]
- Mooney, R.; Quinlan, L.R.; Corley, G.; Godfrey, A.; Osborough, C.; ÓLaighin, G. Evaluation of the Finis Swimsense® and the Garmin Swim™ activity monitors for swimming performance and stroke kinematics analysis. PLoS ONE 2017, 12, e0170902. [Google Scholar] [CrossRef] [PubMed]
- Nimmerichter, A.; Schnitzer, L.; Prinz, B.; Simon, D.; Wirth, K. Validity and Reliability of the Garmin Vector Power Meter in Laboratory and Field Cycling. Int. J. Sports Med. 2017, 38, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Heyken, M.; Horstmann, H.; Kerling, A.; Albrecht, K.; Kedia, G.; Kück, M.; Tegtbur, U.; Hanke, A. Comparison of wearables for self-monitoring of heart rate in coronary rehabilitation patients. Georgian Med. News 2021, 315, 78–85. [Google Scholar]
- Evenson, K.R.; Spade, C.L. Review of Validity and Reliability of Garmin Activity Trackers. J. Meas. Phys. Behav. 2020, 3, 170–185. [Google Scholar] [CrossRef] [PubMed]


| Phase | Time Period | ROM | Pain Intensity (VAS) | Muscle Strength Left (MRC Scale) | Muscle Strength Right (MRC Scale) | Biomechanical Data (Ground Contact Time Distribution) |
|---|---|---|---|---|---|---|
| Preoperative | Before surgery | Knee flexion: 110°, Knee extension: −10° | 3 (walking), 0 (at rest) | Hip flexors: 5/5 Hip extensors: 5/5 Hip abductors: 5/5 Hip adductors: 5/5 Hip external rotators: 5/5 Hip internal rotators: 5/5 Knee extensors: (vastus medialis: 5) Knee flexors: 5/5 Ankle dorsiflexion: 5/5 Ankle plantarflexion: 5/5 | Hip flexors: 5/5 Hip extensors: 5/5 Hip abductors: 5/5 Hip adductors: 5/5 Hip external rotators: 5/5 Hip internal rotators: 5/5 Knee extensors: (vastus medialis: 4) Knee flexors: 5/5 Ankle dorsiflexion:/5 Ankle plantarflexion:/5 | 51.5% left/48.5% right |
| Phase 1 | Weeks 1–2 | Knee flexion: 90°, Knee extension: −5° | 2 (walking), 0 (at rest) | Hip flexors: 5/5 Hip extensors: 5/5 Hip abductors: 4/5 Hip adductors: 5/5 Hip external rotators: 5/5 Hip internal rotators:/5 Knee extensors: 5 (vastus medialis: 5) Knee flexors: 5/5 Ankle dorsiflexion: 5/5 Ankle plantarflexion: 5/5 | Hip flexors: 5/5 Hip extensors: 5/5 Hip abductors: 4/5 Hip adductors: 5/5 Hip external rotators: 5/5 Hip internal rotators: 5/5 Knee extensors: 4 (vastus medialis: 4-) Knee flexors: 5/5 Ankle dorsiflexion: 5/5 Ankle plantarflexion: 5/5 | 51.9% left/48.1% right |
| Phase 2 | Weeks 3–6 | Knee flexion: 110°, Knee extension: 0° | 1 (walking), 0 (at rest) | Hip flexors: 5/5 Hip extensors: 5/5 Hip abductors: 5/5 Hip adductors: 5/5 Hip external rotators: 5/5 Hip internal rotators: 5/5 Knee extensors: 5/5 (vastus medialis: 5) Knee flexors: 5/5 Ankle dorsiflexion: 5/5 Ankle plantarflexion: 5/5 | Hip flexors: 5/5 Hip extensors: 5/5 Hip abductors: 4/5 Hip adductors: 5/5 Hip external rotators: 5/5 Hip internal rotators: 5/5 Knee extensors: 5- (vastus medialis: 4) Knee flexors: 5/5 Ankle dorsiflexion: 5/5 Ankle plantarflexion: 5/5 | 51.7% left/48.3% right |
| Phase 3 | Weeks 7–12 | Knee flexion: 120°, Knee extension: 0° | 0 (walking), 0 (at rest) | Hip flexors: 5/5 Hip extensors: 5/5 Hip abductors: 5/5 Hip adductors: 5/5 Hip external rotators: 5/5 Hip internal rotators: 5/5 Knee extensors: 5/5 (vastus medialis: 5) Knee flexors: 5/5 Ankle dorsiflexion: 5/5 Ankle plantarflexion: 5/5 | Hip flexors: 5/5 Hip extensors: 5/5 Hip abductors: 5/5 Hip adductors: 5/5 Hip external rotators: 5/5 Hip internal rotators: 5/5 Knee extensors: (vastus medialis: 5) Knee flexors: 5/5 Ankle dorsiflexion: 5/5 Ankle plantarflexion: 5/5 | 51.4% left/48.6% right |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galasso, O.; Calabrese, M.; Scanniello, G.; Garofano, M.; Pepe, L.; Budaci, L.; Ungaro, G.; Fimiani, G.; Bramanti, P.; Schiavo, L.; et al. Accelerating Recovery: A Case Report on Telerehabilitation for a Triathlete’s Post-Meniscus Surgery Comeback. Healthcare 2025, 13, 406. https://doi.org/10.3390/healthcare13040406
Galasso O, Calabrese M, Scanniello G, Garofano M, Pepe L, Budaci L, Ungaro G, Fimiani G, Bramanti P, Schiavo L, et al. Accelerating Recovery: A Case Report on Telerehabilitation for a Triathlete’s Post-Meniscus Surgery Comeback. Healthcare. 2025; 13(4):406. https://doi.org/10.3390/healthcare13040406
Chicago/Turabian StyleGalasso, Olimpio, Mariaconsiglia Calabrese, Giuseppe Scanniello, Marina Garofano, Lucia Pepe, Luana Budaci, Gaetano Ungaro, Gianluca Fimiani, Placido Bramanti, Luigi Schiavo, and et al. 2025. "Accelerating Recovery: A Case Report on Telerehabilitation for a Triathlete’s Post-Meniscus Surgery Comeback" Healthcare 13, no. 4: 406. https://doi.org/10.3390/healthcare13040406
APA StyleGalasso, O., Calabrese, M., Scanniello, G., Garofano, M., Pepe, L., Budaci, L., Ungaro, G., Fimiani, G., Bramanti, P., Schiavo, L., Corallo, F., Pagano, M., Cappadona, I., Crinisio, A., & Bramanti, A. (2025). Accelerating Recovery: A Case Report on Telerehabilitation for a Triathlete’s Post-Meniscus Surgery Comeback. Healthcare, 13(4), 406. https://doi.org/10.3390/healthcare13040406






