Thirdhand Smoke and Neonatal/Pediatric Health: A Scoping Review on Nursing Implications
Abstract
1. Introduction
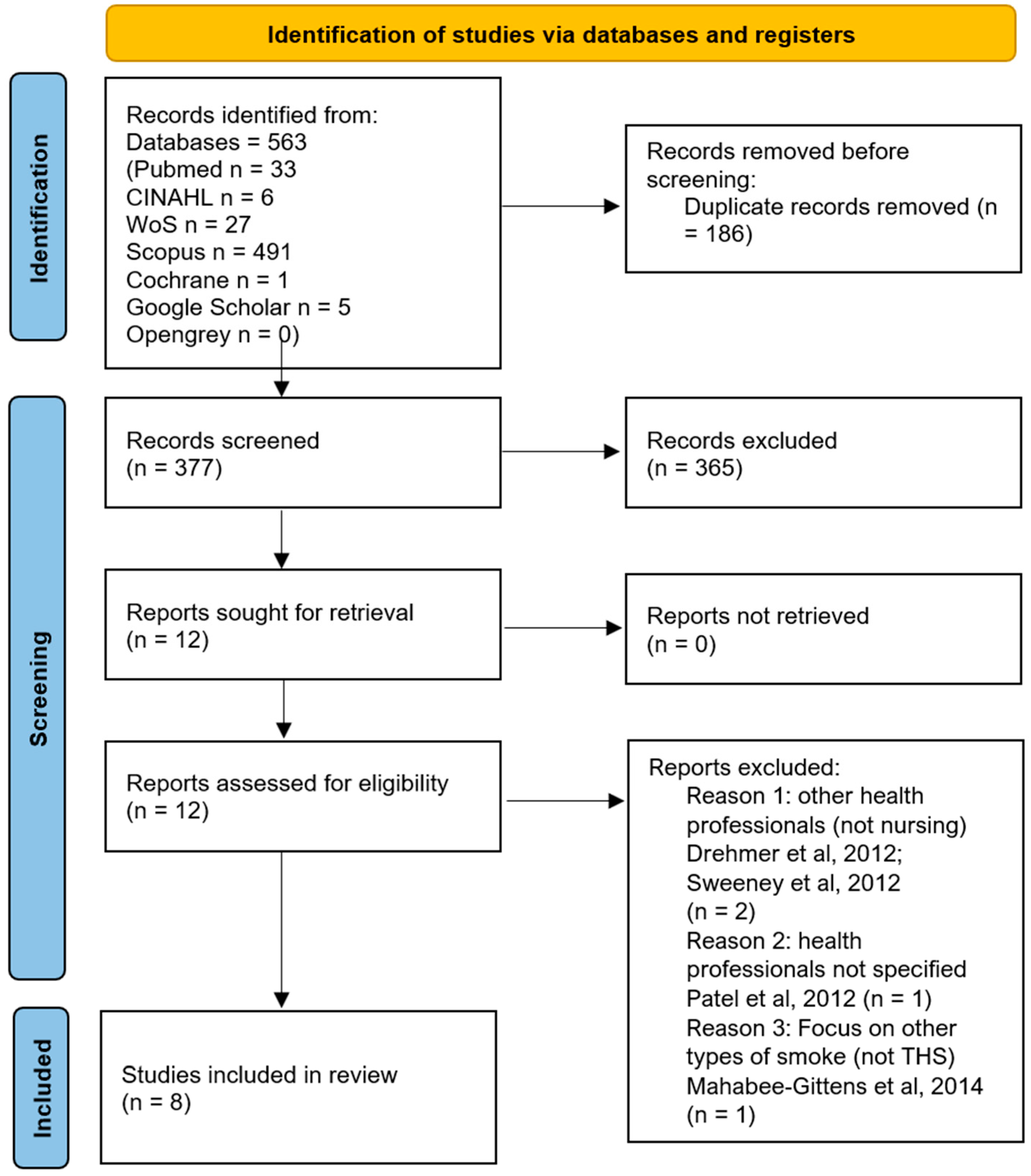
2. Materials and Methods
3. Results
3.1. First Sub-Question
3.2. Second Sub-Question
3.3. Third Sub-Question
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Adams, K.K.; Beem, A.; Diener, E.; Merritt, T.A. Protecting the vulnerable: The importance of effective parental tobacco-dependence treatment during prenatal and newborn care. Pediatr. Allergy Immunol. Pulmonol. 2012, 25, 3–10. [Google Scholar] [CrossRef]
- Parks, J.; McLean, K.E.; McCandless, L.; de Souza, R.J.; Brook, J.R.; Scott, J.; Turvey, S.E.; Mandhane, P.J.; Becker, A.B.; Azad, M.B.; et al. Assessing secondhand and thirdhand tobacco smoke exposure in Canadian infants using questionnaires, biomarkers, and machine learning. J. Expo. Sci. Environ. Epidemiol. 2022, 32, 112–123. [Google Scholar] [CrossRef] [PubMed]
- Vanzi, V.; Marti, F.; Cattaruzza, M.S. Thirdhand smoke knowledge, beliefs and behaviors among parents and families: A systematic review. Healthcare 2023, 11, 2403. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). WHO Global Report on Trends in Prevalence of Tobacco Use 2000–2030; World Health Organization: Geneva, Switzerland, 2024. [Google Scholar]
- World Health Organization (WHO). WHO Report on the Global Tobacco Epidemic 2013: Enforcing Bans on Tobacco Advertising, Promotion and Sponsorship; World Health Organization Tobacco Free Initiative: Geneva, Switzerland, 2013. [Google Scholar]
- Oberg, M.; Jaakkola, M.S.; Woodward, A.; Peruga, A.; Prüss-Ustün, A. Worldwide burden of disease from exposure to second-hand smoke: A retrospective analysis of data from 192 countries. Lancet 2011, 377, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Mahabee-Gittens, M.E.; Matt, G.E.; Lopez-Galvez, N.; Hoh, E.; Quintana, P.J.E.; Dodder, N.G.; Jandarov, R.A.; Stone, L.; Wullenweber, C.A.; Ahluwalia, J.S.; et al. Assessment, detection, and validation of clinical associations of thirdhand smoke exposure (ADVOCATE) study protocol. Pediatr. Res. 2025, 98, 864–870. [Google Scholar] [CrossRef]
- Hein, H.O.; Suadicani, P.; Skov, P.; Gyntelberg, F. Indoor dust exposure: An unnoticed aspect of involuntary smoking. Arch. Environ. Health 1991, 46, 98–101. [Google Scholar] [CrossRef]
- Almassi, A.A.; Oliver, B.G.G.; Smith, S.M. Analysis of assessment methods for detecting nicotine residue and its impact on humans: A systematic review. Int. J. Environ. Res. Public Health 2025, 22, 621. [Google Scholar] [CrossRef]
- Acuff, L.; Fristoe, K.; Hamblen, J.; Smith, M.; Chen, J. Third-hand smoke: Old smoke, new concerns. J. Community Health 2016, 41, 680–687. [Google Scholar] [CrossRef]
- Alotaibi, E.A.; Alrasheed, M.K.; Almutairi, I.H.; Almoutairi, K.M.; Aladdad, A.A.; Alharbi, A.A.; Albaibi, S.A.; Alsadun, A.H.; Alharthi, M.H. Awareness of third-hand smoke: A cross-sectional study among medical students at Qassim University. J. Fam. Med. Prim. Care 2025, 14, 1865–1870. [Google Scholar] [CrossRef]
- Samet, J.M.; Chanson, D.; Wipfli, H. The challenges of limiting exposure to THS in vulnerable populations. Curr. Environ. Health Rep. 2015, 2, 215–225. [Google Scholar] [CrossRef]
- Northrup, T.F.; Matt, G.E.; Hovell, M.F.; Khan, A.M.; Stotts, A.L. Thirdhand smoke in the homes of medically fragile children: Assessing the impact of indoor smoking levels and smoking bans. Nicotine Tob. Res. 2016, 18, 1290–1298. [Google Scholar] [CrossRef] [PubMed]
- Matt, G.E.; Quintana, P.J.; Destaillats, H.; Gundel, L.A.; Sleiman, M.; Singer, B.C.; Jacob, P.; Benowitz, N.; Winickoff, J.P.; Rehan, V.; et al. Thirdhand tobacco smoke: Emerging evidence and arguments for a multidisciplinary research agenda. Environ. Health Perspect. 2011, 119, 1218–1226. [Google Scholar] [CrossRef] [PubMed]
- Jacob, P., 3rd; Benowitz, N.L.; Destaillats, H.; Gundel, L.; Hang, B.; Martins-Green, M.; Matt, G.E.; Quintana, P.J.; Samet, J.M.; Schick, S.F.; et al. Thirdhand smoke: New evidence, challenges, and future directions. Chem. Res. Toxicol. 2017, 30, 270–294. [Google Scholar] [CrossRef] [PubMed]
- Sleiman, M.; Logue, J.M.; Luo, W.; Pankow, J.F.; Gundel, L.A.; Destaillats, H. Inhalable constituents of thirdhand tobacco smoke: Chemical characterization and health impact considerations. Environ. Sci. Technol. 2014, 48, 13093–13101. [Google Scholar] [CrossRef]
- Kuo, H.-W.; Rees, V.W. Third-hand smoke (THS): What is it and what should we do about it? J. Formos. Med. Assoc. 2019, 118, 1478–1479. [Google Scholar] [CrossRef]
- Thomas, J.L.; Guo, H.; Carmella, S.G.; Balbo, S.; Han, S.; Davis, A.; Yoder, A.; Murphy, S.E.; An, L.C.; Ahluwalia, J.S.; et al. Metabolites of a tobacco-specific lung carcinogen in children exposed to secondhand or thirdhand tobacco smoke in their homes. Cancer Epidemiol. Biomark. Prev. 2011, 20, 1213–1221. [Google Scholar] [CrossRef]
- Hang, B.; Sarker, A.H.; Havel, C.; Saha, S.; Hazra, T.K.; Schick, S.; Jacob, P.; Rehan, V.K.; Chenna, A.; Sharan, D.; et al. Thirdhand smoke causes DNA damage in human cells. Mutagenesis 2013, 28, 381–391. [Google Scholar] [CrossRef]
- Díez-Izquierdo, A.; Cassanello-Peñarroya, P.; Lidón-Moyano, C.; Matilla-Santander, N.; Balaguer, A.; Martínez-Sánchez, J.M. Update on thirdhand smoke: A comprehensive systematic review. Environ. Res. 2018, 167, 341–371. [Google Scholar] [CrossRef]
- McGrath-Morrow, S.A.; Gorzkowski, J.; Groner, J.A.; Rule, A.M.; Wilson, K.; Tanski, S.E.; Collaco, J.M.; Klein, J.D. The effects of nicotine on development. Pediatrics 2020, 145, e20191346. [Google Scholar] [CrossRef]
- Castro, E.M.; Lotfipour, S.; Leslie, F.M. Nicotine on the developing brain. Pharmacol. Res. 2023, 190, 106716. [Google Scholar] [CrossRef]
- Tang, X.; Benowitz, N.; Gundel, L.; Hang, B.; Havel, C.M.; Hoh, E.; Jacob, P.; Mao, J.-H.; Martins-Green, M.; Matt, G.E.; et al. Thirdhand exposures to tobacco-specific nitrosamines through inhalation, dust ingestion, dermal uptake, and epidermal chemistry. Environ. Sci. Technol. 2022, 56, 12506–12516. [Google Scholar] [CrossRef]
- Kharazmi, E.; Bordbar, N.; Bordbar, S. Distribution of nursing workforce in the world using Gini coefficient. BMC Nurs. 2023, 22, 151. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Vanzi, V.; Lommi, M.; Stievano, A.; Rocco, G.; Zega, M.; Caggianelli, G. Third-Hand Smoke and neonatal-pediatric health: A scoping review on nursing implications. 4 November 2025. [Google Scholar] [CrossRef]
- Drehmer, J.E.; Ossip, D.J.; Rigotti, N.A.; Nabi-Burza, E.; Woo, H.; Wasserman, R.C.; Chang, Y.; Winickoff, J.P. Pediatrician interventions and thirdhand smoke beliefs of parents. Am. J. Prev. Med. 2012, 43, 533–536. [Google Scholar] [CrossRef]
- Patel, S.; Hendry, P.; Kalynych, C.; Butterfield, R.; Lott, M.; Lukens-Bull, K. The impact of third-hand smoke education in a pediatric emergency department on caregiver smoking policies and quit status: A pilot study. Int. J. Disabil. Hum. Dev. 2012, 11, 335–342. [Google Scholar] [CrossRef]
- Sweeney, L.; Taylor, L.; Peurifoy, J.; Kauffman, K.; Napolitano, N. Success of a Tobacco Cessation Program for Parents at a Children’s Hospital. Respir. Care 2020, 65, 407–412. [Google Scholar] [CrossRef]
- Mahabee-Gittens, E.M.; Dixon, C.A.; Vaughn, L.M.; Duma, E.M.; Gordon, J.S. Parental tobacco screening and counseling in the pediatric emergency department: Practitioners’ attitudes, perceived barriers, and suggestions for implementation and maintenance. J. Emerg. Nurs. 2014, 40, 336–345. [Google Scholar] [CrossRef]
- Yildirim-Ozturk, E.N.; Uyar, M.; Ozturk, M. Determining the prevalence of people’s knowledge that third-hand smoke is harmful to health: A meta-analysis study. Public Health Nurs. 2024, 41, 836–844. [Google Scholar] [CrossRef] [PubMed]
- Darlow, S.D.; Heckman, C.J.; Munshi, T.; Collins, B.N. Thirdhand smoke beliefs and behaviors among healthcare professionals. Psychol. Health Med. 2017, 22, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Quispe-Cristóbal, B.; Lidón-Moyano, C.; Martín-Sánchez, J.C.; Pérez-Martín, H.; Cartanyà-Hueso, À.; Cabriada-Sáez, Í.; de Paz-Cantos, S.; Martínez-Sánchez, J.M.; González-Marrón, A. Knowledge and opinions of healthcare professionals about thirdhand smoke: A multi-national, cross-sectional study. Healthcare 2022, 10, 945. [Google Scholar] [CrossRef] [PubMed]
- Akdeniz, E.; Ahi, S. Yaşamımızda gizli tehlike olan üçüncü el sigara dumanı konusunda hemşirelerin farkındalık düzeyleri: Kesitsel çalışma. Turk. Klin. J. Nurs. Sci. 2025, 17, 477–484. [Google Scholar] [CrossRef]
- Dickinson, B.J.; Thompson, E.D.; Gracely, E.J.; Wilson, K.M.; Pediatric Research in Inpatient Settings (Pris) NetworK. Smoking cessation counseling in the inpatient unit: A survey of pediatric hospitalists. Hosp. Pediatr. 2021, 11, 30–35. [Google Scholar] [CrossRef]
- Northrup, T.F.; Stotts, A.L.; Suchting, R.; Khan, A.M.; Green, C.; Quintana, P.J.E.; Hoh, E.; Hovell, M.F.; Matt, G.E. Medical staff contributions to thirdhand smoke contamination in a neonatal intensive care unit. Tob. Induc. Dis. 2019, 17, 37. [Google Scholar] [CrossRef]
- Daly, J.B.; Mackenzie, L.J.; Freund, M.; Wolfenden, L.; Roseby, R.; Wiggers, J.H. Interventions by health care professionals who provide routine child health care to reduce tobacco smoke exposure in children: A review and meta-analysis. JAMA Pediatr. 2016, 170, 138–145. [Google Scholar] [CrossRef]
- Merianos, A.L.; Fiser, K.A.; Mahabee-Gittens, E.M.; Lyons, M.S.; Gordon, J.S. Barriers to implementation of pediatric emergency department interventions for parental tobacco use and dependence: A qualitative study using the theoretical domains framework. Implement. Sci. Commun. 2022, 3, 3. [Google Scholar] [CrossRef]
- Ferguson, K.; Krishnan, S.; Sullivan, E.; Bhela, S.; Dozor, A.J.; Welter, J.J. Counseling tobacco smoke exposure reduction measures in pediatrics: A quality improvement project. Pediatr. Qual. Saf. 2022, 7, e588. [Google Scholar] [CrossRef]
- Ahialey, J.K.; Lee, Y.; Park, M.-B.; Huh, J. Trends in academic research on thirdhand smoke using bibliometric analysis. Tob. Induc. Dis. 2025, 23, 45. [Google Scholar] [CrossRef]
- Çoşğun, İ.G.; Çilekar, Ş.; Balcı, A.; Köymen, B.N.; Moral, S.; Nur, B.; Yetim, B. The beliefs of medical faculty students about thirdhand smoke. Tob. Induc. Dis. 2023, 21, 17. [Google Scholar] [CrossRef] [PubMed]
- Aras, A.; Bayraktar, M. Third-hand smoke perception and awareness among medical students: A survey study. Sci. Rep. 2024, 14, 13355. [Google Scholar] [CrossRef] [PubMed]
- Sagar, S.; Bhattarai, D.; Ghimire, S.; Bhattarai, A.; Wagle, A.; Subedi, K. Tobacco use, secondhand exposure and knowledge of secondhand and third-hand smoke among medical college students in Western Nepal: A cross-sectional study. BMJ Open 2024, 14, e086266. [Google Scholar] [CrossRef] [PubMed]
- Deckter, L.; Mahabee-Gittens, E.M.; Gordon, J.S. Are pediatric ED nurses delivering tobacco cessation advice to parents? J. Emerg. Nurs. 2009, 35, 402–405. [Google Scholar] [CrossRef]
- Northrup, T.F.; Stotts, A.L.; Suchting, R.; Khan, A.M.; Green, C.; Klawans, M.R.; Quintana, P.J.E.; Hoh, E.; Hovell, M.F.; Matt, G.E. Thirdhand smoke contamination and infant nicotine exposure in a neonatal intensive care unit: An observational study. Nicotine Tob. Res. 2021, 23, 373–382. [Google Scholar] [CrossRef]
- Northrup, T.F.; Stotts, A.L.; Suchting, R.; Matt, G.E.; Quintana, P.J.E.; Khan, A.M.; Green, C.; Klawans, M.R.; Johnson, M.; Benowitz, N.; et al. Thirdhand smoke associations with the gut microbiomes of infants admitted to a neonatal intensive care unit: An observational study. Environ. Res. 2021, 197, 111180. [Google Scholar] [CrossRef]
- Kelley, S.T.; Liu, W.; Quintana, P.J.E.; Hoh, E.; Dodder, N.G.; Mahabee-Gittens, E.M.; Padilla, S.; Ogden, S.; Frenzel, S.; Sisk-Hackworth, L.; et al. Altered microbiomes in thirdhand smoke-exposed children and their home environments. Pediatr. Res. 2021, 90, 1153–1160. [Google Scholar] [CrossRef]
- Northrup, T.F.; Khan, A.M.; Jacob, P., 3rd; Benowitz, N.L.; Hoh, E.; Hovell, M.F.; Matt, G.E.; Stotts, A.L. Thirdhand smoke contamination in hospital settings: Assessing exposure risk for vulnerable paediatric patients. Tob. Control 2016, 25, 619–623. [Google Scholar] [CrossRef]
- Northrup, T.F.; Stotts, A.L.; Suchting, R.; Khan, A.M.; Klawans, M.R.; Green, C.; Hoh, E.; Hovell, M.F.; Matt, G.E.; Quintana, P.J.E. Handwashing results in incomplete nicotine removal from fingers of individuals who smoke: A randomized controlled experiment. Am. J. Perinatol. 2022, 39, 1634–1642. [Google Scholar] [CrossRef]
- Roberts, C.; Wagler, G.; Carr, M.M. Environmental tobacco smoke: Public perception of risks of exposing children to second- and third-hand tobacco smoke. J. Pediatr. Health Care 2017, 31, e7–e13. [Google Scholar] [CrossRef]
- Schuler, B.R.; Collins, B.N.; Scheuermann, T.S.; Baishya, M.; Kilby, L.; Lepore, S.J. Translating pediatric primary care best practice guidelines for addressing tobacco in the WIC system. Transl. Behav. Med. 2023, 13, 57–63. [Google Scholar] [CrossRef]
- Jiang, Y.; Zhao, Y.; Tang, P.; Wang, X.; Guo, Y.; Tang, L. The role of nurses in smoking cessation interventions for patients: A scoping review. BMC Nurs. 2024, 23, 803. [Google Scholar] [CrossRef] [PubMed]
| Authors, Year | Country | Study Design | Aim of the Study | Nursing Focus | Main Findings | Scoping Review’s Sub-Question |
|---|---|---|---|---|---|---|
| Daly et al., 2016 [39] | Australia | Meta-analysis | To determine the effectiveness of interventions delivered by healthcare professionals who provide routine child health care in reducing TSE in children (primary outcome) | Eleven of the sixteen trials in this meta-synthesis included nurses in the educational intervention/model provided | Interventions delivered by HCPs who provide routine child healthcare may be effective in preventing maternal smoking relapse. Further research is required to improve the effectiveness of such interventions in reducing child TSE and increasing parental smoking cessation. | Education/counseling |
| Darlow et al., 2017 [34] | USA | Cross-sectional study | To assess beliefs and behaviors regarding THS among healthcare professionals | Multiprofessional survey: the sample included 204 HCPs and around half of them were nurses (n. 113; 55.7%) | A little more than one third (35%) of the sample had heard of THS before completing the survey, and more than two thirds (69%) of the sample believed that THS issues do not receive enough attention. | Awareness/knowledge |
| Northrup et al., 2019 [38] | USA | Observational cross-sectional study | To explore contamination routes by characterizing nicotine levels (THS proxy) found on the fingers of NICU medical staff and to assess finger-nicotine correlates | Multiprofessional-based study: the final sample size was 246: the majority of participants were nursing staff (n = 170; 65.6%), the most numerous NICU specialty, and nurse practitioners (n = 12; 4.6%) | Almost four in five NICU staff had measurable finger nicotine, with finger surface area and frequency of reported exposure to tobacco smoke in friends’/family members’ homes emerging as important correlates. | Environment contribution |
| Ferguson et al., 2022 [41] | USA | Quality improvement project | To increase the rates of TSE screening and provider counseling regarding TSE reduction using an evidence-based approach | Multiprofessional project: role reconfiguration with nurse-led TSE screening | By integrating TSE screening into established nursing vital-signs records, the practice achieved sustained child TSE screening, with rates rising to 85%, surpassing the pre-specified 80% benchmark. | Education/counseling |
| Merianos et al., 2022 [40] | USA | Qualitative study | To use the theoretical domains framework (TDF) to identify current screening and counseling behaviors of PED/UC professionals related to parental tobacco use and child TSE, and determine barriers and enablers that influence these behaviors | Multiprofessional-based study: semi-structured interviews were conducted with 29 actively practicing PED/UC clinical staff; 51% were nurses | Most PED/UC professionals did not currently follow the guidelines, but perceived addressing parental tobacco use as part of their role. This study’s findings support the need to develop and implement an intervention to support PED/UC professionals in their tobacco prevention and control practices. | Education/counseling |
| Quispe-Cristóbal et al., 2022 [35] | Spain | Cross-sectional study | To explore the knowledge and opinions of healthcare professionals about THS | Multiprofessional survey: the final sample consisted of 233 participants and 67.4% were nurses | Almost two out of three HCPs who participated in the study did not know what THS was. Educational activities on this topic should be implemented. | Awareness/knowledge |
| Yildirim-Ozturk et al., 2024 [33] | Turkey | Meta-analysis | To determine the prevalence of people’s knowledge that THS is harmful for children and adults. | Of the twelve articles in this meta-synthesis, three targeted HCPs, but only one included nurses among the participants | For HCPs, the prevalence of people’s knowledge that THS is harmful to children was 89.8%, the highest prevalence value calculated in the meta-analysis | Awareness/knowledge |
| Akdeniz et al., 2025 [36] | Turkey | Cross-sectional study | To determine the awareness of THS among nurses | Nurse-based study: 219 nurses were included as participants | The study found that while the participants’ THSA was high, only a small proportion (23.7%) had heard of the concept. It is recommended to provide educational programs to inform nurses about THS. | Awareness/knowledge |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vanzi, V.; Lommi, M.; Stievano, A.; Rocco, G.; Zega, M.; Caggianelli, G. Thirdhand Smoke and Neonatal/Pediatric Health: A Scoping Review on Nursing Implications. Healthcare 2025, 13, 3289. https://doi.org/10.3390/healthcare13243289
Vanzi V, Lommi M, Stievano A, Rocco G, Zega M, Caggianelli G. Thirdhand Smoke and Neonatal/Pediatric Health: A Scoping Review on Nursing Implications. Healthcare. 2025; 13(24):3289. https://doi.org/10.3390/healthcare13243289
Chicago/Turabian StyleVanzi, Valentina, Marzia Lommi, Alessandro Stievano, Gennaro Rocco, Maurizio Zega, and Gabriele Caggianelli. 2025. "Thirdhand Smoke and Neonatal/Pediatric Health: A Scoping Review on Nursing Implications" Healthcare 13, no. 24: 3289. https://doi.org/10.3390/healthcare13243289
APA StyleVanzi, V., Lommi, M., Stievano, A., Rocco, G., Zega, M., & Caggianelli, G. (2025). Thirdhand Smoke and Neonatal/Pediatric Health: A Scoping Review on Nursing Implications. Healthcare, 13(24), 3289. https://doi.org/10.3390/healthcare13243289