Metabolic Indicators and Emotional Distress Symptoms Related to Overweight in Youth: A Brief Network Analysis
Abstract
1. Introduction
1.1. Depression Associated with Overweight and Obesity
1.2. Stress and Anxiety Associated with Overweight and Obesity
1.3. Positive Emotions Associated with Overweight and Obesity
2. Current Study
3. Method
3.1. Design Research
3.2. Measurements
3.2.1. Biochemical Evaluations
- Glucose: Analyses were stratified according to risk levels based on reference values established by the American Diabetes Association et al. [42], as follows: (a) Normal or Risk Level 1 (less than 100 mg/dL), (b) Prediabetes or Risk Level 2 (between 100 and 125 mg/dL), and (c) Diabetes or Risk Level 3 (greater than 126 mg/dL).
- Cholesterol: Analyses were categorized into different risk levels based on reference values established by the Mexican Social Security Institute et al. [43], as follows: (a) Desirable or Risk Level 1 (less than 200 mg/dL), (b) Borderline High or Risk Level 2 (between 200 and 239 mg/dL), and (c) High or Risk Level 3 (greater than 240 mg/dL).
- Triglycerides: Data were organized according to risk level, using the reference criteria from the Mexican Social Security Institute et al. [43], as follows: (a) Normal or Risk Level 1 (less than 150 mg/dL), (b) Borderline High or Risk Level 2 (between 150 and 199 mg/dL), (c) High or Risk Level 3 (between 200 and 499 mg/dL), and (d) Very High or Risk Level 4 (greater than 500 mg/dL).
3.2.2. Anthropometric Measurements
- Body Mass Index (BMI): Classified according to the Centers for Disease Control and Prevention et al. [44], as follows: (a) Underweight or Risk Level 1 (below 18.5), (b) Normal weight or Risk Level 2 (between 18.5 and 24.9), (c) Overweight or Risk Level 3 (25.0–29.0), and (d) Obesity or Risk Level 4 (30.0 or higher).
- Waist-to-hip Ratio (WHR): Categorized according to risk level based on the criteria established by Rosas et al. [45], as follows: (a) Low health risk or Risk Level 1 (<0.95 in men and <0.80 in women), (b) Moderate risk or Risk Level 2 (81–85 in women and 96–100 in men), and (c) High risk or Risk Level 3 (>86 in women and >100 in men).
3.2.3. Patient Health Questionnaire-9 for Depression (PHQ-9)
3.2.4. Self-Assessment of Happiness
3.2.5. GAD-7 (Generalized Anxiety Disorder 7-Item)
3.2.6. Emotional Exhaustion Scale (EES)
4. Procedure
5. Statistics Analysis
6. Results
6.1. Descriptive Statistics of the Study Variables
6.2. Correlation Analysis
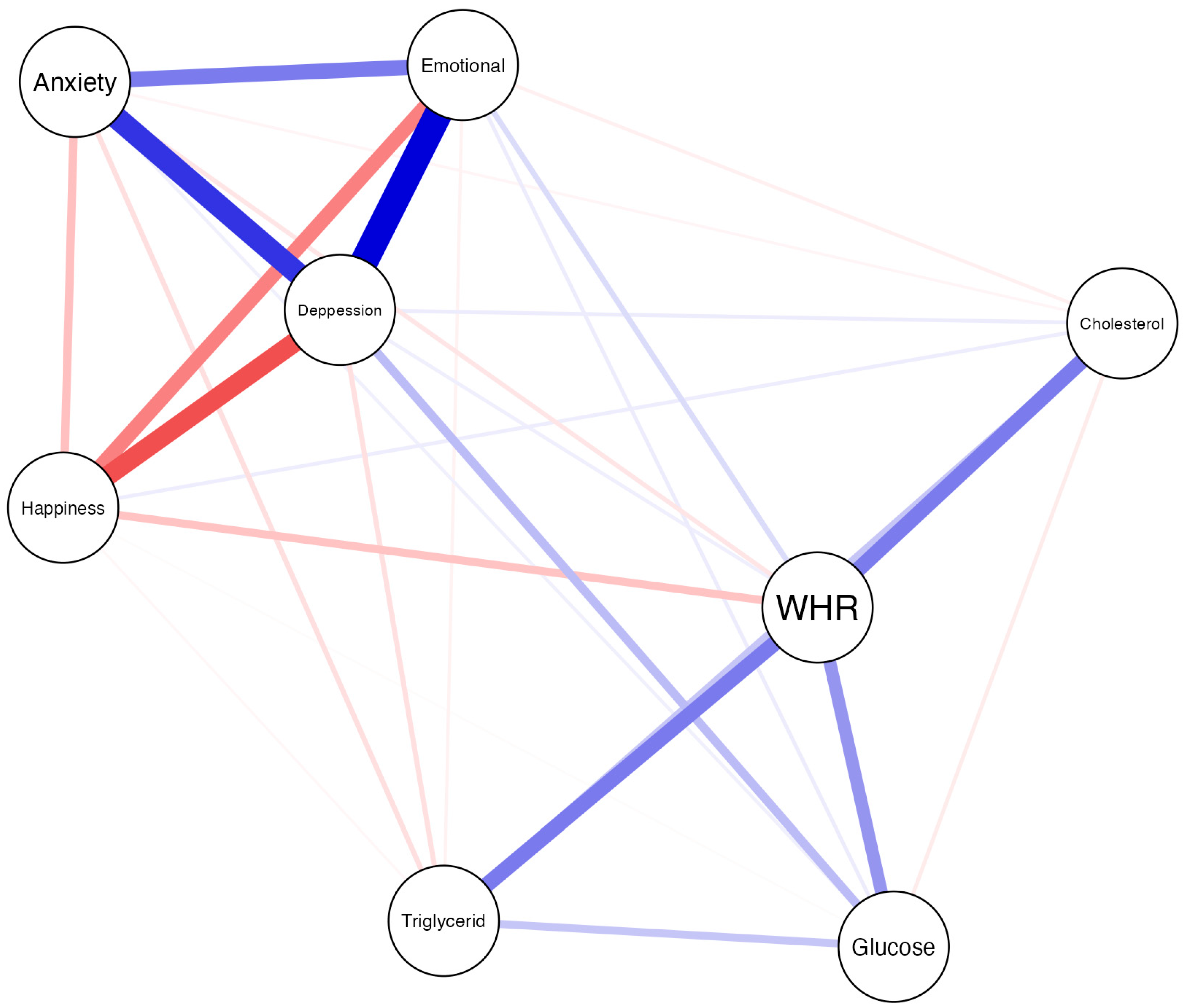
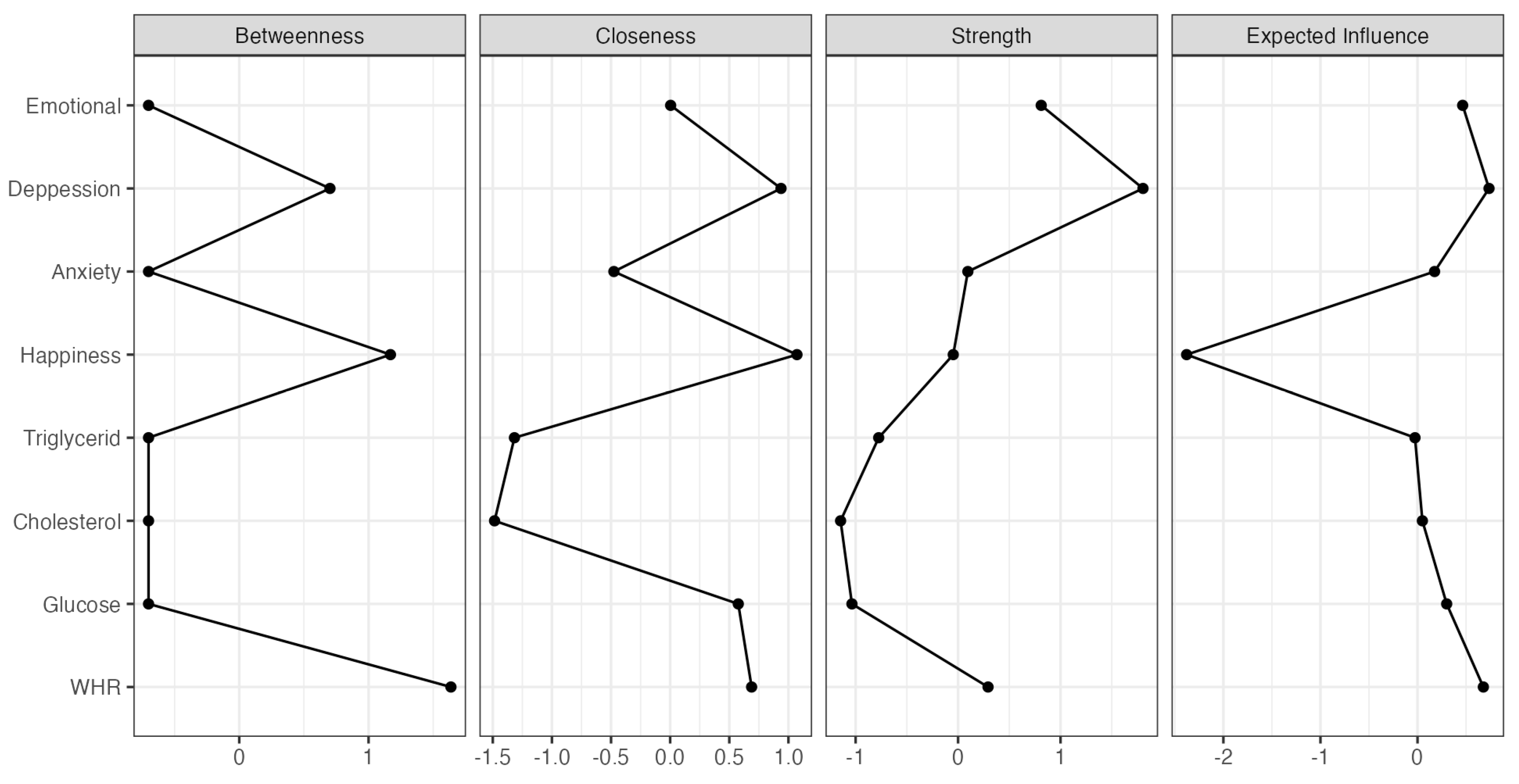
6.3. Neural Network Structure
7. Discussion
7.1. Practical Implications
7.2. Limitations and Suggestions
7.3. Implications for Future Research
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Campos-Nonato, I.; Galván-Valencia, O.; Hernández-Barrera, L.; Oviedo-Solís, C.; Barquera, S. Prevalencia de obesidad y factores de riesgo asociados en adultos mexicanos: Resultados de la ENSANUT 2022. Salud Publica Mex. 2023, 65, s238–s247. [Google Scholar] [CrossRef]
- Secretaría de Salud. Norma Oficial Mexicana NOM-037-SSA2-2012, Para la Prevención, Tratamiento y Control de las Dislipidemias; Secretaría de Salud: México City, México, 2012.
- Organización Mundial de la Salud. Obesidad y Sobrepeso; OMS: Ginebra, Switzerland, 2024; Available online: https://www.who.int/es/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 17 March 2025).
- Organización para la Cooperación y el Desarrollo Económicos (OCDE). The Heavy Burden of Obesity: The Economics of Prevention; OECD Publishing: París, France, 2019. [Google Scholar] [CrossRef]
- Çeltikçi, B.; Gülensoy, E. The biochemical effect correlated with pulmonary dysfunction and complications in obese patients. Acta Medica 2024, 55, 85–92. [Google Scholar] [CrossRef]
- Monserrat-Mesquida, M.; Quetglas-Llabrés, M.; Bouzas, C.; Capó, X.; Mateos, D.; Ugarriza, L.; Tur, J.A.; Sureda, A. Peripheral blood mononuclear cells oxidative stress and plasma inflammatory biomarkers in adults with normal weight, overweight and obesity. Antioxidants 2021, 10, 813. [Google Scholar] [CrossRef]
- Mata-Cases, M.; Artola, S.; Escalada, J.; Ezkurra-Loyola, P.; Ferrer-García, J.C.; Fornos, J.A.; Girbés, J.; Rica, I. Consenso sobre la detección y el manejo de la prediabetes. Aten. Primaria 2015, 47, 456–468. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, A.M. Highlighting diabetes mellitus: The epidemic continues. Arterioscler. Thromb. Vasc. Biol. 2018, 38, e1–e8. [Google Scholar] [CrossRef]
- Smith, J.; Rodríguez, P.; Gómez, L. Evaluación antropométrica y bioquímica en el diagnóstico de obesidad y riesgo metabólico. Rev. Cienc. Salud 2020, 15, 45–60. [Google Scholar]
- Lampignano, L.; Zupo, R.; Donghia, R.; Guerra, V.; Castellana, F.; Murro, I.; Di Noia, C.; Sardone, R.; Giannelli, G.; De Pergola, G.; et al. Cross-sectional relationship among different anthropometric parameters and cardio-metabolic risk factors in a cohort of patients with overweight or obesity. PLoS ONE 2020, 15, e0241841. [Google Scholar] [CrossRef]
- Noboa Pullaguari, K.D. Asociación entre la circunferencia abdominal y el riesgo de enfermedades cardiovasculares [Association between abdominal circumference and risk of cardiovascular disease]. Latam Rev. Latinoam. Cienc. Soc. Humanidades 2023, 4, 4699. [Google Scholar] [CrossRef]
- Dakanalis, A.; Mentzelou, M.; Papadopoulou, S.K.; Papandreou, D.; Spanoudaki, M.; Vasios, G.K.; Pavlidou, E.; Mantzorou, M.; Giaginis, C. The association of emotional eating with overweight/obesity, depression, anxiety/stress, and dietary patterns: A review of the current clinical evidence. Nutrients 2023, 15, 1173. [Google Scholar] [CrossRef]
- Miguel-Soca, P.E. Alteraciones metabólicas durante la obesidad. Salud Publica Mex. 2014, 56, 657–658. [Google Scholar]
- Martí-Nicolovius, M. Efectos del sobrepeso y la obesidad en las funciones cognitivas de niños y adolescentes [Effects of overweight and obesity on cognitive functions of children and adolescents]. Rev. Neurol. 2022, 75, 59–65. [Google Scholar] [CrossRef]
- Frank, P.; Jokela, M.; Batty, G.; Lassale, C.; Steptoe, A.; Kivimäki, M. Overweight, obesity, and individual symptoms of depression: A multicohort study with replication in UK Biobank. Brain Behav. Immun. 2022, 105, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Blaine, B. Does Depression Cause Obesity? J. Health Psychol. 2008, 13, 1190–1197. [Google Scholar] [CrossRef] [PubMed]
- Luppino, F.S.; De Wit, L.M.; Vliet, V.J. Overweight, obesity, and depression. Arch. Gen. Psychiatry 2010, 67, 220–227. [Google Scholar] [CrossRef]
- Palomino-Pérez, A.M. Rol de la emoción en la conducta alimentaria. Rev. Chil. Nutr. 2020, 47, 286–291. [Google Scholar] [CrossRef]
- Jantaratnotai, N.; Mosikanon, K.; Lee, Y.; McIntyre, R.S. The interface of depression and obesity. Obes. Res. Clin. Pract. 2017, 11, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Tomiyama, J. Stress and Obesity. Annu. Rev. Psychol. 2019, 70, 703–718. [Google Scholar] [CrossRef]
- Metz, U.; Welke, J.; Esch, T.; Renneberg, B.; Braun, V.; Heintze, C. Perception of stress and quality of life in overweight and obese people—Implications for preventive consultancies in primary care. Med. Sci. Monit. 2008, 15, PH1–PH6. [Google Scholar]
- Urriza-Trejo, S.; Hurtazo, H.; Palacios, J.; Cruz-Soto, M. The Association of Insomnia and Stress on Cardiovascular Risk Factors during COVID-19 Confinement in the Mexican Population. Int. J. Environ. Res. Public Health 2023, 20, 7135. [Google Scholar] [CrossRef]
- Gay Patiño, J.V.; Jiménez Tlatenchi, D.E.; García González, J.E.; Zempoalteca Morales, A. Asociación entre ansiedad, sobrepeso y obesidad en población adulta adscrita a una unidad de medicina familiar. Atención Fam. 2020, 27, 131–134. [Google Scholar] [CrossRef]
- Guillén Riebeling, R.S. El estrés como factor de riesgo en el sobrepeso y la obesidad. Psic-Obesidad 2023, 12, 8–13. [Google Scholar] [CrossRef]
- Pompa Guajardo, E.G.; Meza Peña, C. Ansiedad, estrés y obesidad en una muestra de adolescentes de México. Univ. Psychol. 2017, 16, 199–209. [Google Scholar] [CrossRef]
- Andrei, F.; Nuccitelli, C.; Mancini, G.; Reggiani, G.; Trombini, E. Emotional intelligence, emotion regulation and affectivity in adults seeking treatment for obesity. Psychiatry Res. 2018, 269, 191–198. [Google Scholar] [CrossRef]
- Saxena, V.; Pandey, N.; Sarraf, R.R. Correlation Between Obesity, Self Esteem, & Happiness in Young Adults. Int. J. Indian. Psychol. 2024, 12, 1247–1255. [Google Scholar]
- Katsaiti, M. Obesity and happiness. Appl. Econ. 2012, 44, 4101–4111. [Google Scholar] [CrossRef]
- Diener, E.; Seligman, M.E.P. Very happy people. Psychol. Sci. 2002, 13, 81–84. [Google Scholar] [CrossRef]
- Kok, B.E.; Coffey, K.A.; Cohn, M.A.; Catalino, L.I.; Vacharkulksemsuk, T.; Algoe, S.B.; Brantley, M.; Fredrickson, B.L. How positive emotions build physical health: Perceived positive social connections account for the upward spiral between positive emotions and vagal tone. Psychol. Sci. 2013, 24, 1123–1132. [Google Scholar] [CrossRef]
- Ong, A.D.; Uchino, B.N.; Wethington, E. Loneliness and health in older adults: A mini-review and synthesis. Gerontology 2016, 62, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Toker, S.; Shirom, A.; Melamed, S. Depression and the metabolic syndrome: Gender-dependent associations in the Israeli CORDIS study. J. Psychosom. Res. 2005, 59, 265–273. [Google Scholar] [CrossRef]
- Steptoe, A.; Wardle, J.; Marmot, M. Positive affect and health-related neuroendocrine, cardiovascular, and inflammatory processes. Proc. Natl. Acad. Sci. USA 2005, 102, 6508–6512. [Google Scholar] [CrossRef]
- González-Carrillo, L.; Rodríguez-Ramírez, S. Obesidad y salud mental en adultos mexicanos: Una revisión sistemática. Rev. Salud Publica 2020, 22, 215–223. [Google Scholar]
- Carfora, V.; Morandi, M.; Catellani, P. The influence of message framing on consumers’ selection of local food. Foods 2022, 11, 1268. [Google Scholar] [CrossRef]
- Avitia, G.C.; Portillo Reyes, V.; Reyes Leal, G.; Loya Méndez, Y. Relación del índice de masa corporal con felicidad, autoestima y depresión en adultos jóvenes. Nóesis. Rev. Cienc. Soc. Humanidades 2022, 27, 51–63. [Google Scholar] [CrossRef]
- Zheng, H.; García, L.; Yao, J. The bidirectional association between depression and obesity in adults: A systematic review and meta-analysis of longitudinal studies. Obes. Rev. 2021, 22, e13128. [Google Scholar] [CrossRef]
- Sultson, H.; Akkermann, K. Investigating phenotypes of emotional eating based on weight categories: A latent profile analysis. Int. J. Eat. Disord. 2019, 52, 1024–1034. [Google Scholar] [CrossRef]
- Borsboom, D.; Cramer, A.O. Network analysis: An integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [CrossRef] [PubMed]
- Magallares, A.; Benito de Valle, P.; Irles, J.A.; Bolaños-Ríos, P.; Jáuregui-Lobera, I. Psychological well-being in a sample of obese patients compared with a control group. Nutr. Hosp. 2014, 30, 32–36. [Google Scholar] [CrossRef]
- Calderón, C.; Forns, M.; Varea, V. Obesidad infantil: Ansiedad y síntomas cognitivos y conductuales propios de los trastornos de alimentación. An. Pediatr. 2009, 71, 489–494. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. Standards of Medical Care in Diabetes—2025. Available online: https://professional.diabetes.org/standards-of-care (accessed on 28 August 2024).
- Instituto Mexicano del Seguro Social. Diagnóstico y Tratamiento de Dislipidemias (Hipercolesterolemia) en el Adulto (Guía de Práctica Clínica IMSS-233-09). 2016. Available online: https://www.imss.gob.mx/sites/all/statics/guiasclinicas/233GER.pdf (accessed on 20 March 2025).
- Centros para el Control y la Prevención de Enfermedades. Acerca del Índice de Masa Corporal Para Adultos; CDC: Atlanta, GA, USA, 2022. Available online: https://www.cdc.gov/healthyweight/spanish/assessing/bmi/adult_bmi/index.html (accessed on 21 March 2025).
- Rosas, M.; Calles, J.; Friege, L. Índice cintura-cadera como predictor de riesgo cardiovascular en adultos. Rev. Mex. Cardiol. 2009, 20, 123–129. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Huarcaya-Victoria, J.; De-Lama-Morán, R.; Quiros, M.; Bazán, J.; López, K.; Lora, D. Propiedades psicométricas del Patient Health Questionnaire (PHQ-9) en estudiantes de medicina en Lima, Perú. Rev. Neuropsiquiatr. 2020, 83, 72–78. [Google Scholar] [CrossRef]
- Cassiani-Miranda, C.A.; Cuadros-Cruz, A.K.; Torres-Pinzón, H.; Scoppetta, O.; Pinzón-Tarrazona, J.H.; López-Fuentes, W.Y.; Paez, A.; Cabanzo-Arenas, D.F.; Ribero-Marulanda, S.; Llanes-Amaya, E.R. Validez del cuestionario de salud del paciente-9 (PHQ-9) para cribado de depresión en adultos usuarios de Atención Primaria en Bucaramanga, Colombia. Rev. Colomb. Psiquiatr. 2021, 50, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Khalek, A.M. Measuring happiness with a single-item scale. Soc. Behav. Personal. 2006, 34, 139–150. [Google Scholar] [CrossRef]
- Palacios-Delgado, J.; Ambriz-Flores, M.; Cruz-Vargas, D.J. The effectiveness of kindness intervention for promoting positive emotions and reducing depressive symptoms in Mexican adults. Soc. Sci. 2025, 14, 61. [Google Scholar] [CrossRef]
- Gaitán-Rossi, P.; Pérez-Hernández, V.; Vilar-Compte, M.; Teruel-Belismelis, G. Prevalencia mensual de trastorno de ansiedad generalizada durante la pandemia por COVID-19 en México. Salud Publica Mex. 2021, 63, 478–485. [Google Scholar] [CrossRef]
- García-Campayo, J.; Zamorano, E.; Ruiz, M.A.; Pardo, A.; Perez-Paramo, M.; Lopez-Gomez, V.; Freire, O.; Rejas, J. Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual. Life Outcomes 2010, 8, 8. [Google Scholar] [CrossRef]
- González Ramírez, M.T.; Landero Hernández, R. Escala de cansancio emocional (ECE) para estudiantes universitarios: Propiedades psicométricas en una muestra de México. An. Psicol. 2007, 23, 253–257. Available online: https://revistas.um.es/analesps/article/view/22321 (accessed on 14 January 2024).
- Hevey, D. Network analysis: A brief overview and tutorial. Health Psychol. Behav. Med. 2018, 6, 301–328. [Google Scholar] [CrossRef]
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef]
- Flegal, K.M. Assessing the effects of obesity on health outcomes. Med. Clin. N. Am. 2010, 94, 1047–1060. [Google Scholar] [CrossRef]
- Du, J.Y.; Hallford, D.J.; Busby Grant, J. Characteristics of episodic future thinking in anxiety: A systematic review and meta-analysis. Clin. Psychol. Rev. 2022, 95, 102162. [Google Scholar] [CrossRef] [PubMed]
- Bucio Palma, L.J.; Palacios Delgado, J.R. Saborea la vida para sentirte mejor. ExpresionES UVM 2025, 13, 18–21. Available online: https://expresionesuvm.com/ojs-3.3.0-8/index.php/expresionesuvm/article/view/478/259 (accessed on 20 July 2025).
| Mean | SD | Range | Category | |
|---|---|---|---|---|
| Metabolic indicators | ||||
| Glucose | 93.7 | 11.7 | 74–141 | low * |
| Cholesterol | 181 | 27.7 | 149–297 | low * |
| Triglycerides | 220 | 106 | 84–538 | high limit |
| Anthropometric measures | ||||
| Weight | 66.0 | 15.0 | 39.6–108 | - |
| BMI | 24.6 | 4.96 | 17.2–37.2 | healthy * |
| Waist | 78.3 | 11.1 | 58.9–82.0 | normal |
| Hip | 98 | 9.49 | 82–127 | low * |
| Emotional factors | ||||
| Happiness | 7.24 | 2.12 | 1–10 | low |
| Depression | 7.36 | 5.66 | 0–25 | low |
| Anxiety | 6.91 | 4.8 | 0–21 | moderate |
| Emotional exhaustion | 28.2 | 8.87 | 11–48 | moderate |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bucio-Palma, L.; García-Mier, L.; Cruz-Soto, M.; Vargas-Rodríguez, A.; Palacios-Delgado, J. Metabolic Indicators and Emotional Distress Symptoms Related to Overweight in Youth: A Brief Network Analysis. Healthcare 2025, 13, 3096. https://doi.org/10.3390/healthcare13233096
Bucio-Palma L, García-Mier L, Cruz-Soto M, Vargas-Rodríguez A, Palacios-Delgado J. Metabolic Indicators and Emotional Distress Symptoms Related to Overweight in Youth: A Brief Network Analysis. Healthcare. 2025; 13(23):3096. https://doi.org/10.3390/healthcare13233096
Chicago/Turabian StyleBucio-Palma, Lesly, Lina García-Mier, Martha Cruz-Soto, Angela Vargas-Rodríguez, and Jorge Palacios-Delgado. 2025. "Metabolic Indicators and Emotional Distress Symptoms Related to Overweight in Youth: A Brief Network Analysis" Healthcare 13, no. 23: 3096. https://doi.org/10.3390/healthcare13233096
APA StyleBucio-Palma, L., García-Mier, L., Cruz-Soto, M., Vargas-Rodríguez, A., & Palacios-Delgado, J. (2025). Metabolic Indicators and Emotional Distress Symptoms Related to Overweight in Youth: A Brief Network Analysis. Healthcare, 13(23), 3096. https://doi.org/10.3390/healthcare13233096






