Effects of Online Supervised Slow-Movement Bodyweight Resistance Training Followed by Self-Directed Exercise on Physical Function in Older Adults: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Design
2.3. Online Exercise Class
2.3.1. OEC Implementation Mode and Flow
2.3.2. Training Program
2.4. Self-Directed Exercise (SDE)
2.5. Measurements
2.5.1. Physical Function
2.5.2. Questionnaires
2.5.3. Training Recording Sheet to Assess Training Status
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OEC | Online exercise class |
| SBRT | Slow movement bodyweight-based resistance training |
| SDE | Self-directed exercise |
| CS-30 | 30-second chair stand test |
| ICT | Information and communication technology |
| SQ | Squat |
| SSQ | Split squat |
| SP | Shoulder press |
| CSAC | Chair-seated abdominal curl |
| KCL | Kihon Checklist |
| GLFS-25 | 25-question geriatric locomotive function scale |
References
- Chen, L.-K. Community-Powered Actions Building a Healthier Future for Aging Populations. Arch. Gerontol. Geriatr. 2025, 128, 105652. [Google Scholar] [CrossRef]
- Olshansky, S.J. From Lifespan to Healthspan. JAMA 2018, 320, 1323–1324. [Google Scholar] [CrossRef]
- Lai, X.; Zhu, H.; Wu, Z.; Chen, B.; Jiang, Q.; Du, H.; Huo, X. Dose–Response Effects of Resistance Training on Physical Function in Frail Older Chinese Adults: A Randomized Controlled Trial. J. Cachexia Sarcopenia Muscle 2023, 14, 2824–2834. [Google Scholar] [CrossRef]
- Sun, R.; Wan, J.; Tang, J.; Deng, Y.; Zhang, M.; Liu, C.; Li, J.; Zhang, Q. Effectiveness of Resistance Training on Body Composition, Muscle Strength, and Biomarker in Sarcopenic Older Adults: A Meta-Analysis of Randomized Controlled Trials. Arch. Gerontol. Geriatr. 2025, 128, 105595. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Hashizume, H.; Oka, H.; Okada, M.; Takakura, R.; Hisari, A.; Yoshida, M.; Utsunomiya, H. Physical Performance Measures Associated with Locomotive Syndrome in Middle-Aged and Older Japanese Women. J. Geriatr. Phys. Ther. 2015, 38, 202–207. [Google Scholar] [CrossRef]
- Chao, D.; Foy, C.G.; Farmer, D. Exercise Adherence among Older Adults: Challenges and Strategies. Control Clin. Trials 2000, 21, 212S–217S. [Google Scholar] [CrossRef] [PubMed]
- Schutzer, K.A.; Graves, B.S. Barriers and Motivations to Exercise in Older Adults. Prev. Med. 2004, 39, 1056–1061. [Google Scholar] [CrossRef]
- Tison, G.H.; Avram, R.; Kuhar, P.; Abreau, S.; Marcus, G.M.; Pletcher, M.J.; Olgin, J.E. Worldwide Effect of COVID-19 on Physical Activity: A Descriptive Study. Ann. Intern. Med. 2020, 173, 767–770. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, G.J.; Malani, P.N.; Solway, E.; Kirch, M.; Singer, D.C.; Kullgren, J.T. Changes in Activity Levels, Physical Functioning, and Fall Risk during the COVID-19 Pandemic. J. Am. Geriatr. Soc. 2022, 70, 49–59. [Google Scholar] [CrossRef]
- Kirwan, R.; McCullough, D.; Butler, T.; Perez de Heredia, F.; Davies, I.G.; Stewart, C. Sarcopenia during COVID-19 Lockdown Restrictions: Long-Term Health Effects of Short-Term Muscle Loss. Geroscience 2020, 42, 1547–1578. [Google Scholar] [CrossRef]
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Suzuki, M.; Koyama, S.; Kikuchi, T.; Kusumi, H.; Arai, H. Effect of the COVID-19 Epidemic on Physical Activity in Community-Dwelling Older Adults in Japan: A Cross-Sectional Online Survey. J. Nutr. Health Aging 2020, 24, 948–950. [Google Scholar] [CrossRef]
- Chaabene, H.; Prieske, O.; Herz, M.; Moran, J.; Höhne, J.; Kliegl, R.; Ramirez-Campillo, R.; Behm, D.G.; Hortobágyi, T.; Granacher, U. Home-Based Exercise Programmes Improve Physical Fitness of Healthy Older Adults: A PRISMA-Compliant Systematic Review and Meta-Analysis with Relevance for COVID-19. Ageing Res. Rev. 2021, 67, 101265. [Google Scholar] [CrossRef]
- Thiebaud, R.S.; Funk, M.D.; Abe, T. Home-Based Resistance Training for Older Adults: A Systematic Review. Geriatr. Gerontol. Int. 2014, 14, 750–757. [Google Scholar] [CrossRef]
- Geraedts, H.; Zijlstra, A.; Bulstra, S.K.; Stevens, M.; Zijlstra, W. Effects of Remote Feedback in Home-Based Physical Activity Interventions for Older Adults: A Systematic Review. Patient Educ. Couns. 2013, 91, 14–24. [Google Scholar] [CrossRef] [PubMed]
- Hyodo, K.; Kidokoro, T.; Yamaguchi, D.; Iida, M.; Watanabe, Y.; Ueno, A.; Noda, T.; Kawahara, K.; Nishida, S.; Kai, Y.; et al. Feasibility, Safety, Enjoyment, and System Usability of Web-Based Aerobic Dance Exercise Program in Older Adults: Single-Arm Pilot Study. JMIR Aging 2023, 6, e39898. [Google Scholar] [CrossRef] [PubMed]
- Fyfe, J.J.; Dalla Via, J.; Jansons, P.; Scott, D.; Daly, R.M. Feasibility and Acceptability of a Remotely Delivered, Home-Based, Pragmatic Resistance ‘Exercise Snacking’ Intervention in Community-Dwelling Older Adults: A Pilot Randomised Controlled Trial. BMC Geriatr. 2022, 22, 521. [Google Scholar] [CrossRef]
- Hong, J.; Kim, J.; Kim, S.W.; Kong, H.-J. Effects of Home-Based Tele-Exercise on Sarcopenia among Community-Dwelling Elderly Adults: Body Composition and Functional Fitness. Exp. Gerontol. 2017, 87, 33–39. [Google Scholar] [CrossRef]
- Chang, S.-H.; Wang, L.-T.; Chueh, T.-Y.; Hsueh, M.-C.; Hung, T.-M.; Wang, Y.-W. Effectiveness of Facebook Remote Live-Streaming-Guided Exercise for Improving the Functional Fitness of Community-Dwelling Older Adults. Front. Med. 2021, 8, 734812. [Google Scholar] [CrossRef] [PubMed]
- Edna Mayela, D.L.V.-C.; Miriam, L.-T.; Ana Isabel, G.-G.; Oscar, R.-C.; Alejandra, C.-A. Effectiveness of an Online Multicomponent Physical Exercise Intervention on the Physical Performance of Community-Dwelling Older Adults: A Randomized Controlled Trial. Geriatr. Nurs. 2023, 54, 83–93. [Google Scholar] [CrossRef]
- Granet, J.; Peyrusqué, E.; Ruiz, F.; Buckinx, F.; Abdelkader, L.B.; Dang-Vu, T.T.; Sirois, M.J.; Gouin, J.P.; Pageaux, B.; Aubertin-Leheudre, M. Online Physical Exercise Intervention in Older Adults during Lockdown: Can We Improve the Recipe? Aging Clin. Exp. Res. 2023, 35, 551–560. [Google Scholar] [CrossRef]
- Hong, J.; Kong, H.-J.; Yoon, H.-J. Web-Based Telepresence Exercise Program for Community-Dwelling Elderly Women with a High Risk of Falling: Randomized Controlled Trial. JMIR mHealth uHealth 2018, 6, e132. [Google Scholar] [CrossRef] [PubMed]
- Kuldavletova, O.; Pasquier, F.; Bigot, L.; Langeard, A.; Gauthier, A.; Quarck, G. Videoconference-Based Adapted Physical Exercise Training Is a Good and Safe Option for Seniors. Int. J. Environ. Res. Public. Health 2021, 18, 9439. [Google Scholar] [CrossRef] [PubMed]
- Poon, E.T.-C.; Sun, F.; Tse, A.C.-Y.; Tsang, J.H.; Chung, A.Y.-H.; Lai, Y.Y.-Y.; Wong, S.W.-S. Effectiveness of Tele-Exercise Training on Physical Fitness, Functional Capacity, and Health-Related Quality of Life in Non-Hospitalized Individuals with COVID-19: The COFIT-HK Study. J. Exerc. Sci. Fit. 2024, 22, 134–139. [Google Scholar] [CrossRef]
- Ozaki, H.; Sawada, S.; Osawa, T.; Natsume, T.; Yoshihara, T.; Deng, P.; Machida, S.; Naito, H. Muscle Size and Strength of the Lower Body in Supervised and in Combined Supervised and Unsupervised Low-Load Resistance Training. J. Sports Sci. Med. 2020, 19, 721–726. [Google Scholar]
- Jones, C.J.; Rikli Roberta, E.; Beam, W.C. A 30-s Chair-Stand Test as a Measure of Lower Body Strength in Community-Residing Older Adults. Res. Q. Exerc. Sport 1999, 70, 113–119. [Google Scholar] [CrossRef]
- Sawada, S.; Ozaki, H.; Natsume, T.; Deng, P.; Yoshihara, T.; Nakagata, T.; Osawa, T.; Ishihara, Y.; Kitada, T.; Kimura, K.; et al. The 30-s Chair Stand Test Can Be a Useful Tool for Screening Sarcopenia in Elderly Japanese Participants. BMC Musculoskelet. Disord. 2021, 22, 639. [Google Scholar] [CrossRef]
- McCain, A.; McGibbon, C.; Carroll, M.; MacKenzie, E.; Sénéchal, M.; Bouchard, D. Validity of Common Physical Function Tests Performed Online for Older Adults. Arch. Gerontol. Geriatr. 2023, 114, 105104. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Sawada, S.; Deng, P.; Naito, H.; Machida, S. Continued Benefits of Online Supervised Bodyweight Training for Lower-Limb Function in Older Adults: A Single-arm Pilot Study. Aging Med. Healthc. 2025, accepted. [Google Scholar]
- Satake, S.; Senda, K.; Hong, Y.-J.; Miura, H.; Endo, H.; Sakurai, T.; Kondo, I.; Toba, K. Validity of the Kihon Checklist for Assessing Frailty Status. Geriatr. Gerontol. Int. 2016, 16, 709–715. [Google Scholar] [CrossRef]
- Seichi, A.; Hoshino, Y.; Doi, T.; Akai, M.; Tobimatsu, Y.; Iwaya, T. Development of a Screening Tool for Risk of Locomotive Syndrome in the Elderly: The 25-Question Geriatric Locomotive Function Scale. J. Orthop. Sci. 2012, 17, 163–172. [Google Scholar] [CrossRef]
- Yoshiko, A.; Ogawa, M.; Shimizu, K.; Radaelli, R.; Neske, R.; Maeda, H.; Maeda, K.; Teodoro, J.; Tanaka, N.; Pinto, R.S.; et al. Chair Sit-to-Stand Performance Is Associated with Diagnostic Features of Sarcopenia in Older Men and Women. Arch. Gerontol. Geriatr. 2021, 96, 104463. [Google Scholar] [CrossRef] [PubMed]
- Orange, S.T.; Marshall, P.; Madden, L.A.; Vince, R.V. Short-Term Training and Detraining Effects of Supervised vs. Unsupervised Resistance Exercise in Aging Adults. J. Strength. Cond. Res. 2019, 33, 2733–2742. [Google Scholar] [CrossRef] [PubMed]
- Kalapotharakos, V.I.; Diamantopoulos, K.; Tokmakidis, S.P. Effects of Resistance Training and Detraining on Muscle Strength and Functional Performance of Older Adults Aged 80 to 88 Years. Aging Clin. Exp. Res. 2010, 22, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Van Roie, E.; Bautmans, I.; Coudyzer, W.; Boen, F.; Delecluse, C. Low- and High-Resistance Exercise: Long-Term Adherence and Motivation among Older Adults. Gerontology 2015, 61, 551–560. [Google Scholar] [CrossRef]
- Kim, H.-R.; Woo, S.-H.; Seo, J.-P.; So, W.-Y.; Bae, J.-S. Satisfaction with the Exercise Program and Successful Aging Among Older Adults Who Exercise Regularly: The Multiple Mediation of Physical Self-Efficacy and Exercise Adherence. Healthcare 2024, 12, 2054. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Martin, A.D.; Taunton, J.E.; Rhodes, E.C.; Donnelly, M.; Elliot, J. Factors Associated with Exercise Adherence among Older Adults. An Individual Perspective. Sports Med. 1999, 28, 397–411. [Google Scholar] [CrossRef]
| Lesson | Exercise | Repetition | CON-ECC | Set | Interval |
|---|---|---|---|---|---|
| 3 | SQ | 8 | 3–3 | 2 | 60 |
| 4 | SQ, SP | 8 | 3–3 | 2 | 60 |
| 5 | SQ, SP | 10 | 3–3 | 2 | 60 |
| 6 | SQ, SP, CSAC | 10 | 3–3 | 2 | 60 |
| 7 | SSQ, SQ, SP, CSAC | 10 | 3–3 | 2 | 45 |
| 8 | SSQ, SQ, SP, CSAC | 10 | 3–3 | 3 | 45 |
| 9 | SSQ, SQ, SP, CSAC | 10 | 3–3 | 3 | 45 |
| 10 | SSQ, SQ, SP, CSAC | 15 | 3–3 | 3 | 45 |
| 11 | SSQ, SQ, SP, CSAC | 15 | 3–3 | 3 | 45 |
| 12 | SSQ, SQ, SP, CSAC | 15 | 3–3 | 3 | 30 |
| 13 | SSQ, SQ, SP, CSAC | 15 | 3–3 | 3 | 30 |
| 14 | SSQ, SQ, SP, CSAC | 15 | 3–3 | 3 | 30 |
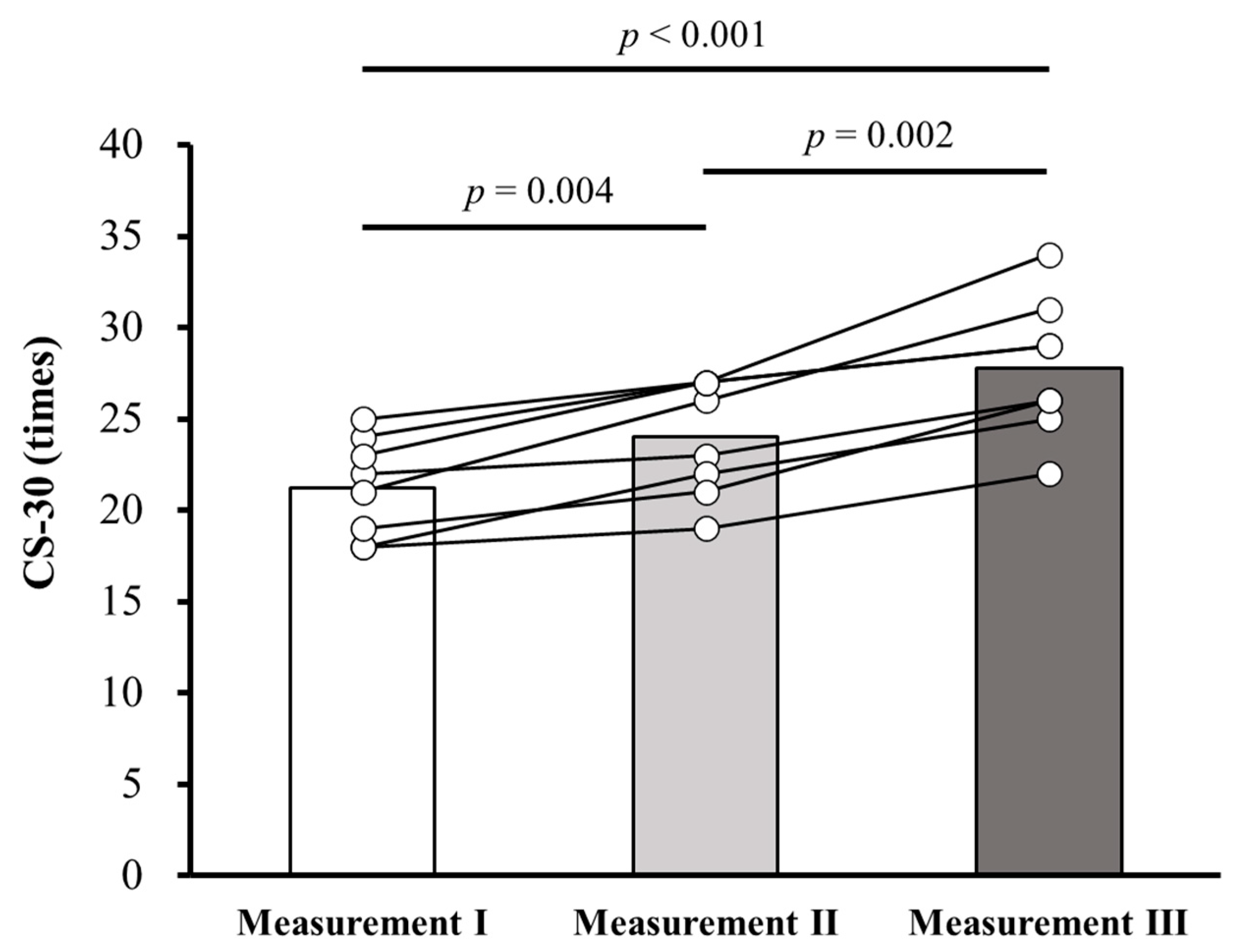
| Outcome | Measurement 1 | Measurement 2 | Measurement 3 | Main Effect of Time * |
|---|---|---|---|---|
| CS-30 (times) | 21.3 ± 2.7 21.5 [18.3, 23.8] | 24.0 ± 3.2 24.5 [21.3, 27.0] | 27.8 ± 3.8 27.5 [25.3, 30.5] | p < 0.001 |
| KCL (points) | 5.0 ± 2.3 5.0 [2.5, 7.5] | 3.6 ± 0.9 4.0 [3.0, 4.0] | 3.9 ± 2.0 3.5 [3.0, 4.8] | p = 0.112 |
| GLFS-25 (points) | 9.8 ± 5.6 9.5 [6.3, 10.8] | 8.8 ± 4.3 7.0 [6.3, 9.5] | 9.8 ± 3.8 9.5 [7.3, 10.8] | p = 0.542 |
| Outcome | OEC Period Measurements 1–2 | SDE Period Measurements 2–3 | p-Value |
|---|---|---|---|
| Days of training (days) | 17.5 ± 8.7 14.0 [12.0, 22.5] | 15.0 ± 6.9 17.5 [9.0, 19.8] | 0.916 a |
| Days of training/week | 2.5 ± 1.2 2.0 [1.7, 3.2] | 2.1 ± 1.0 2.5 [1.3, 2.9] | 0.916 a |
| Performed repetitions of SQ (reps) | 528.4 ± 134.7 558.0 [382.5, 655.3] | 462.0 ± 242.8 550.5 [270.0, 581.3] | 0.510 b |
| Performed repetitions of SSQ (one side) (reps) | 392.4 ± 135.5 342.5 [305.0, 447.3] | 479.6 ± 220.7 523.5 [315.0, 573.8] | 0.247 a |
| Performed repetitions of total lower limb training (reps) | 1313.1 ± 376.4 1302.5 [992.5, 1520.0] | 1421.3 ± 673.2 1552.5 [922.5, 1728.8] | 0.698 b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Z.; Sawada, S.; Naito, H.; Machida, S. Effects of Online Supervised Slow-Movement Bodyweight Resistance Training Followed by Self-Directed Exercise on Physical Function in Older Adults: A Pilot Study. Healthcare 2025, 13, 3091. https://doi.org/10.3390/healthcare13233091
Liu Z, Sawada S, Naito H, Machida S. Effects of Online Supervised Slow-Movement Bodyweight Resistance Training Followed by Self-Directed Exercise on Physical Function in Older Adults: A Pilot Study. Healthcare. 2025; 13(23):3091. https://doi.org/10.3390/healthcare13233091
Chicago/Turabian StyleLiu, Zhenyue, Shuji Sawada, Hisashi Naito, and Shuichi Machida. 2025. "Effects of Online Supervised Slow-Movement Bodyweight Resistance Training Followed by Self-Directed Exercise on Physical Function in Older Adults: A Pilot Study" Healthcare 13, no. 23: 3091. https://doi.org/10.3390/healthcare13233091
APA StyleLiu, Z., Sawada, S., Naito, H., & Machida, S. (2025). Effects of Online Supervised Slow-Movement Bodyweight Resistance Training Followed by Self-Directed Exercise on Physical Function in Older Adults: A Pilot Study. Healthcare, 13(23), 3091. https://doi.org/10.3390/healthcare13233091







