Assessment of Oral Hygiene Practices, Adjunctive Cleaning Methods, and Their Impact on Plaque and Gingival Indices Among Young Adults in Urban and Rural Settings in Romania
Abstract
1. Introduction
2. Materials and Methods
2.1. Procedure Methodology
- Between the ages of 20 and 41;
- Live in either the city or the country in Arad County;
- In excellent health overall, with no heart disease, diabetes, or other diseases that could affect oral health;
- With at least 20 natural teeth and no extensive prosthetic rehabilitation, to ensure reliable and comparable plaque and gingival index assessment;
- Have received no orthodontic or periodontal therapy within the past 12 months, as recent treatment may alter gingival indices and plaque accumulation [16];
- Willing to follow study instructions, including using their self-reported habitual toothpaste formulation during the supervised brushing session and applying the standard Bass toothbrushing technique;
- Provide written consent before taking part.
- People who have known allergies or are very sensitive to any of the natural toothpaste ingredients that were tested (sodium bicarbonate, activated charcoal, lemon) or the plaque-revealing agent that was used in the clinical study;
- Individuals who have used antibiotics, anti-inflammatories, or antibacterial mouthwashes within the last four weeks were excluded, as such agents can transiently alter the oral microbiota and gingival inflammation [17];
- Women who are pregnant or breastfeeding, because hormones can change the health of the gums;
- People who are currently getting braces, removable prostheses, or extensive fixed prosthetic restorations that could make it challenging to examine for plaque;
- People who have had craniofacial abnormalities, cleft lip/palate, or maxillofacial surgical interventions (other than minor oral surgery like extractions);
- People who have active cavities that need urgent restorative treatment or acute oral infections at the time of the examination;
- Individuals who were unable or unwilling to undergo both pre- and post-brushing evaluations were excluded.
Statistical Analysis
3. Results
4. Discussion
5. Study Limitations and Future Perspectives
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hannig, C.; Attin, T.; Hannig, M.; Henze, E.; Brinkmann, K.; Zech, R. Immobilisation and activity of human α-amylase in the acquired enamel pellicle. Arch. Oral Biol. 2004, 49, 469–475. [Google Scholar] [CrossRef]
- Oppenheim, F.; Troxler, R. Human salivary mucin MG1 selectively forms heterotypic complexes with amylase, proline-rich proteins, statherin, and histatins. J. Dent. Res. 1997, 76, 734–743. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, G.V.O.; Mosley, G.A.; Ross, W.; Dagher, A.; Martins, B.G.d.S.; Fernandes, J.C.H. Revisiting Socransky’s Complexes: A Review Suggesting Updated New Bacterial Clusters (GF-MoR Complexes) for Periodontal and Peri-Implant Diseases and Conditions. Microorganisms 2024, 12, 2214. [Google Scholar] [CrossRef] [PubMed]
- Marsh, P.D. Dental Plaque as a Biofilm and a Microbial Community—Implications for Health and Disease. BMC Oral Health 2006, 6 (Suppl. 1), S14. [Google Scholar] [CrossRef] [PubMed]
- Marsh, P.D. Dental Plaque as a Microbial Biofilm. Caries Res. 2004, 38, 204–211. [Google Scholar] [CrossRef]
- Kolenbrander, P.E.; Andersen, R.N.; Kazmerzak, K.M.; Palmer, R.J., Jr. Coaggregation and coadhesion in oral biofilms. In Community Structure and Co-Operation in Biofilms; Allison, D.G., Gilbert, P., Lappin-Scott, H.M., Wilson, M., Eds.; Society for General Microbiology Symposium 59; Cambridge University Press: Cambridge, UK, 2000; pp. 65–85. [Google Scholar]
- Hasty, D.L.; Ofek, I.; Courtney, H.S.; Doyle, R.J. Multiple Adhesins of Streptococci. Infect. Immun. 1992, 60, 2147–2152. [Google Scholar] [CrossRef]
- Zhang, Y.; Lei, Y.; Nobbs, A.; Khammanivong, A.; Herzberg, M.C. Inactivation of Streptococcus gordonii SspAB Alters Expression of Multiple Adhesin Genes. Infect. Immun. 2005, 73, 3351–3357. [Google Scholar] [CrossRef]
- Savarkar, S.; Sankar, J.; Furtado, M.A. Efficacy Study of Whitening Toothpaste Containing Lemon (Citrus limon) and Salt (Sodium Carbonate). J. Dent. Oral Health 2019, 2, 1–4. [Google Scholar] [CrossRef]
- Bosma, M.L.; Milleman, K.R.; Akwagyiram, I.; Milleman, J.L.; McKeown, P.; Gar-cia-Godoy, F. A Randomised Controlled Trial to Evaluate the Plaque Removal Efficacy of Sodium Bicarbonate Dentifrices in a Single Brushing Clinical Model. BDJ Open 2018, 4, 17037. [Google Scholar] [CrossRef]
- Activated Charcoal in Toothpaste: Systematic Review Looks at Whitening and Abrasive Effects. Today’s RDH, 14 July 2023. Available online: https://www.todaysrdh.com/activated-charcoal-in-toothpaste-systematic-review-looks-at-whitening-and-abrasive-effects/ (accessed on 29 October 2025).
- Anand, L.; Shenoy, R.P.; Yelleti, G. Effect of polyherbal toothpaste on dental plaque, gingivitis, and salivary antioxidant levels: A single-blind randomized controlled trial. Int. J. Clin. Pediatr. Dent. 2025, 18, 533–538. [Google Scholar] [CrossRef]
- Inchingolo, A.M.; Marinelli, G.; Colonna, V.; Pennacchio, B.F.P.; Giorgio, R.V.; Inchingolo, F.; Di Venere, D.; Palermo, A.; Minervini, G.; Inchingolo, A.D.; et al. Efficacy and Safety of Natural Versus Conventional Toothpastes and Mouthwashes in Gingivitis Management: A Systematic Review. Hygiene 2025, 5, 38. [Google Scholar] [CrossRef]
- Weik, U.; Shankar-Subramanian, S.; Sämann, T.; Wöstmann, B.; Margraf-Stiksrud, J.; Deinzer, R. “You should brush your teeth better”: A randomized controlled trial comparing best-possible versus as-usual toothbrushing. BMC Oral Health 2023, 23, 456. [Google Scholar] [CrossRef] [PubMed]
- Hosadurga, R.; Boloor, V.A.; Rao, S.N.; MeghRani, N. Effectiveness of two different herbal toothpaste formulations in the reduction of plaque and gingival inflammation in patients with established gingivitis—A randomized controlled trial. J. Tradit. Complement. Med. 2018, 8, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Vivek, B.; Ramesh, K.S.; Gautami, P.S.; Sruthima, G.N.; Dwarakanath, C.; Anudeep, M. Effect of Periodontal Treatment on Oral Health-Related Quality of Life—A Randomised Controlled Trial. J. Taibah Univ. Med. Sci. 2021, 16, 856–863. [Google Scholar] [CrossRef] [PubMed]
- Bescos, R.; Ashworth, A.; Cutler, C.; Brookes, Z.L.; Belfield, L.A.; Rodiles, A.; Casas-Agustench, P.; Farnham, G.; Liddle, L.; Burleigh, M.; et al. Effects of Chlorhexidine Mouthwash on the Oral Microbiome. Sci. Rep. 2020, 10, 5254. [Google Scholar] [CrossRef]
- Bass, C.C. An effective method of personal oral hygiene. J. La. State Med. Soc. 1954, 106, 57–73. [Google Scholar]
- Mehta, D.S.; Kishore, A.; Sharma, K.S.; Agrawal, N.; Singh, M.; Agrawal, S. Toothbrushes and Tooth Brushing Methods: A Periodontal Review. J. Clin. Stud. Med. Case Rep. 2022, 9, 129. [Google Scholar]
- Silness, J.; Löe, H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol. Scand. 1964, 22, 121–135. [Google Scholar] [CrossRef]
- Lobene, R.R.; Weatherford, T.; Ross, N.M.; Lamm, R.A.; Menaker, L. A modified gingival index for use in clinical trials. Clin. Prev. Dent. 1986, 8, 3–6. [Google Scholar]
- Lile, I.E.; Hajaj, T.; Veja, I.; Hosszu, T.; Vaida, L.L.; Todor, L.; Stana, O.; Popovici, R.-A.; Marian, D. Comparative Evaluation of Natural Mouthrinses and Chlorhexidine in Dental Plaque Management: A Pilot Randomized Clinical Trial. Healthcare 2025, 13, 1181. [Google Scholar] [CrossRef]
- Worthington, H.V.; MacDonald, L.; Poklepovic Pericic, T.; Sambunjak, D.; Johnson, T.M.; Imai, P.; Clarkson, J.E. Home use of interdental cleaning devices, in addition to toothbrushing, for preventing and controlling gum diseases and dental plaque. Cochrane Database Syst. Rev. 2019, 4, CD012018. [Google Scholar] [PubMed]
- Seuntjens, M.T.; Schlueter, N.; van der Weijden, F.; Slot, D.E. Plaque scores after one or two minutes of toothbrushing: A systematic review and meta-analysis. Int. J. Dent. Hyg. 2025, 23, 614–624. [Google Scholar] [CrossRef] [PubMed]
- Valkenburg, C.; Slot, D.E.; Bakker, E.W.; Van der Weijden, F.A. The effect of sodium bicarbonate toothpaste on plaque and gingival health: A systematic review. Int. J. Dent. Hyg. 2019, 17, 99–116. [Google Scholar] [CrossRef] [PubMed]
- Brooks, J.K.; Bashirelahi, N.; Reynolds, M.A. Charcoal and charcoal-based dentifrices: A literature review. J. Am. Dent. Assoc. 2017, 148, 661–670. [Google Scholar] [CrossRef]
- Marian, D.; Popovici, R.A.; Olariu, I.; Pitic (Cot), D.E.; Marta, M.-M.; Veja (Ilyes), I. Patterns and Practices in the Use of Endodontic Materials: Insights from Romanian Dental Practices. Appl. Sci. 2025, 15, 1272. [Google Scholar] [CrossRef]
- World Health Organization, Regional Office for Europe. WHO/Europe Calls for Urgent Action on Oral Disease as Highest Rates Globally Are Recorded in European Region. Media Release, 20 April 2023. Available online: https://www.who.int/europe/news/item/20-04-2023-who-europe-calls-for-urgent-action-on-oral-disease-as-highest-rates-globally-are-recorded-in-european-region (accessed on 20 September 2025).
- World Health Organization. Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030; WHO: Geneva, Switzerland, 2022; Available online: https://www.who.int/publications/i/item/9789240061484 (accessed on 20 September 2025).
- American Dental Association. Toothpastes. 2025. Available online: https://www.ada.org/resources/ada-library/oral-health-topics/toothpastes (accessed on 20 September 2025).
- Osmanaj, N.; Petersen, S.; Eisenburger, M.; Greuling, A. Abrasion Behavior of Different Charcoal Toothpastes on Human Dentin When Using Electric Toothbrushes. Dent. J. 2022, 10, 46. [Google Scholar] [CrossRef]
- Balhaddad, A.A.; Almalki, F.; Altayyar, R.; Alzahrani, R.; Alotaibi, S.; Al Dehailan, L.; Ibrahim, M.S. The Interplay between Toothbrush Stiffness and Charcoal-Containing Dentifrice on the Development of Enamel Topography Changes. BMC Oral Health 2024, 24, 1394. [Google Scholar] [CrossRef]
- Tomás, D.B.M.; Pecci-Lloret, M.P.; Guerrero-Gironés, J. Effectiveness and Abrasiveness of Activated Charcoal as a Whitening Agent: A Systematic Review of In Vitro Studies. Ann. Anat. 2023, 245, 151998. [Google Scholar] [CrossRef]
- Vertuan, M.; da Silva, J.F.; de Oliveira, A.C.M.; da Silva, T.T.; Justo, A.P.; Zordan, F.L.S.; Magalhães, A.C. The In Vitro Effect of Dentifrices with Activated Charcoal on Eroded Teeth. Int. Dent. J. 2023, 73, 518–523. [Google Scholar] [CrossRef]
- Lee, M.K.; Chen, I.H.; Hsu, I.L.; Tsai, W.H.; Lee, T.Y.; Jhong, J.H.; Wu, J.H. The Impact of Lacticaseibacillus paracasei GMNL-143 Toothpaste on Gingivitis and Oral Microbiota in Adults: A Randomized, Double-Blind, Crossover, Placebo-Controlled Trial. BMC Oral Health 2024, 24, 477. [Google Scholar] [CrossRef]
- Paqué, P.N.; Schmidlin, P.R.; Wiedemeier, D.B.; Wegehaupt, F.J.; Burrer, P.D.; Körner, P.; Attin, T. Toothpastes with Enzymes Support Gum Health and Reduce Plaque Formation. Int. J. Environ. Res. Public Health 2021, 18, 835. [Google Scholar] [CrossRef]
- Rădulescu, V.; Boariu, M.; Rusu, D.; Boldeanu, C.; Christodorescu, R.; Roman, A.; Surlin, P.; Didilescu, A.C.; Vela, O.; Kardaras, G.; et al. Is the Diagnosis of Generalized Stage IV (Severe) Periodontitis Compatible with the Survival of Extended Stabilizing Prosthetic Restorations? A Medium-Term Retrospective Study. Diagnostics 2022, 12, 3053. [Google Scholar] [CrossRef] [PubMed]
- Ilyes, I.; Rusu, D.; Rădulescu, V.; Vela, O.; Boariu, M.I.; Roman, A.; Surlin, P.; Kardaras, G.; Boia, S.; Chinnici, S.; et al. A Placebo-Controlled Trial to Evaluate Two Locally Delivered Antibiotic Gels (Piperacillin Plus Tazobactam vs. Doxycycline) in Stage III–IV Periodontitis Patients. Medicina 2023, 59, 303. [Google Scholar] [CrossRef] [PubMed]
- Ilyes, I.; Boariu, M.; Rusu, D.; Iorio-Siciliano, V.; Vela, O.; Boia, S.; Kardaras, G.; Șurlin, P.; Calniceanu, H.; Jentsch, H.; et al. A Single Dose of Piperacillin Plus Tazobactam Gel as an Adjunct to Professional Mechanical Plaque Removal (PMPR) in Patients with Peri-Implant Mucositis: A 6-Month Double-Blind Randomized Clinical Trial. Antibiotics 2024, 13, 269. [Google Scholar] [CrossRef] [PubMed]
- Ilyes, I.; Boariu, M.; Rusu, D.; Iorio-Siciliano, V.; Vela, O.; Boia, S.; Radulescu, V.; Șurlin, P.; Jentsch, H.; Lodin, A.; et al. Comparative Study of Systemic vs. Local Antibiotics with Subgingival Instrumentation in Stage III–IV Periodontitis: A Retrospective Analysis. Antibiotics 2024, 13, 430. [Google Scholar] [CrossRef]
- Vela, O.C.; Boariu, M.; Rusu, D.; Iorio-Siciliano, V.; Ramaglia, L.; Boia, S.; Radulescu, V.; Ilyes, I.; Stratul, S.-I. Healing of Periodontal Suprabony Defects following Treatment with Open Flap Debridement with or without Hyaluronic Acid (HA) Application. Medicina 2024, 60, 829. [Google Scholar] [CrossRef]
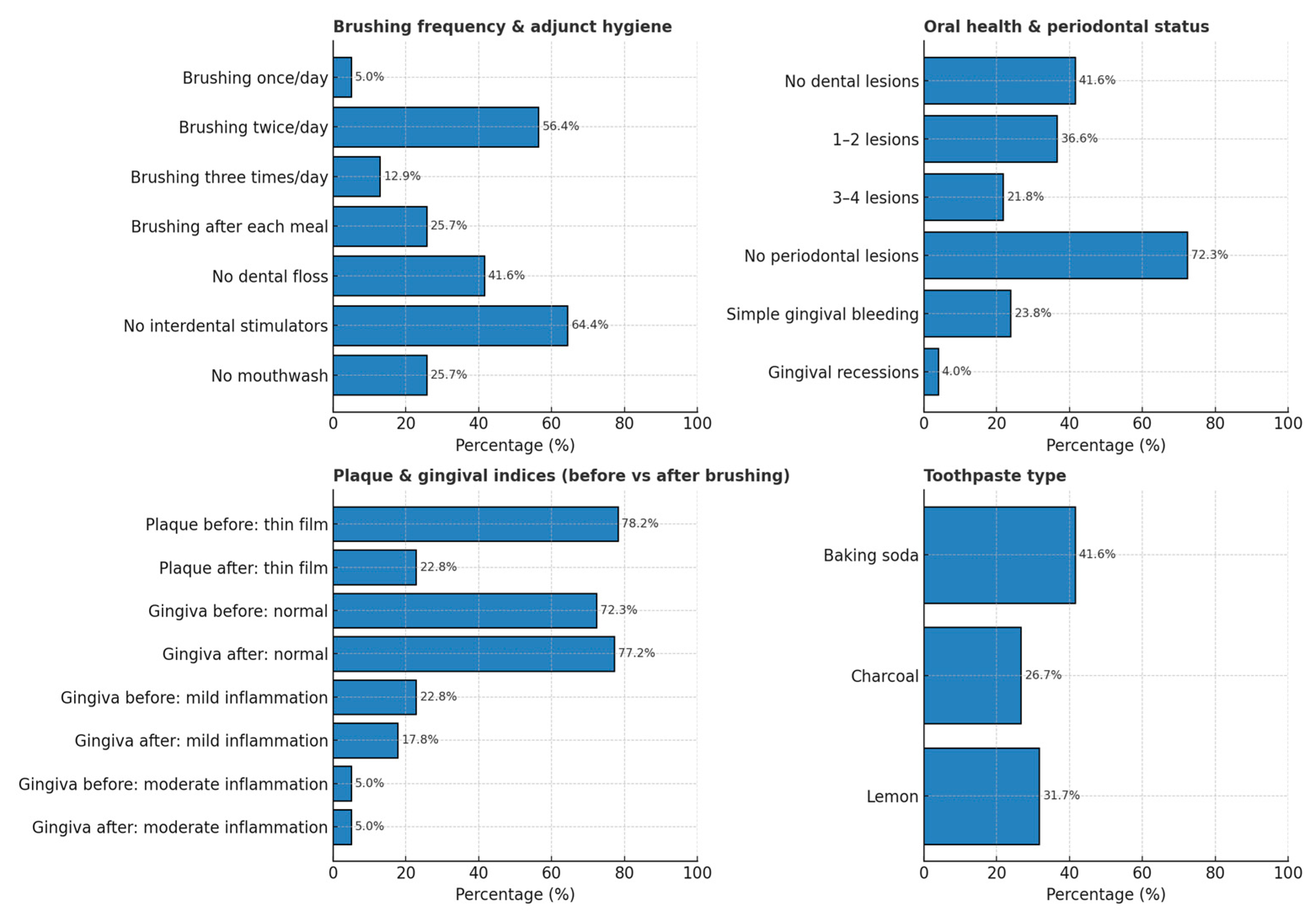
| Variable | Category | n (%)/Mean (SD) |
|---|---|---|
| Sample size | 101 | |
| Age (years) | Mean (SD) | 23.32 (5.26) |
| Environment | Urban | 70 (69.3) |
| Daily brushing frequency | Once a day | 5 (5.0) |
| Twice a day | 57 (56.4) | |
| Three times a day | 13 (12.9) | |
| After each meal | 26 (25.7) | |
| Use of dental floss | No | 42 (41.6) |
| Use of interdental stimulators | No | 65 (64.4) |
| Use of mouthwash | No | 26 (25.7) |
| Presence of carious lesions/fillings | No | 42 (41.6) |
| Number of carious lesions/fillings | 1–2 | 37 (36.6) |
| 3–4 | 22 (21.8) | |
| None | 42 (41.6) | |
| Presence of signs of gingival inflammation | None | 73 (72.3) |
| Gingival recessions | 4 (4.0) | |
| Simple (gingival bleeding) | 24 (23.8) | |
| Silness-Loe plaque index before brushing | Grade 1 = thin film adherent at gingival margin and adjacent tooth surfaces, detectable with probe | 79 (78.2) |
| Loe & Silness gingival index modified by Lobene before brushing | Normal gingiva | 73 (72.3) |
| Mild inflammation | 23 (22.8) | |
| Moderate inflammation | 5 (5.0) | |
| Toothpaste used | Baking soda | 42 (41.6) |
| Charcoal | 27 (26.7) | |
| Lemon | 32 (31.7) | |
| Loe & Silness gingival index modified by Lobene after brushing | Normal gingiva | 78 (77.2) |
| Mild inflammation | 18 (17.8) | |
| Moderate inflammation | 5 (5.0) | |
| Silness-Loe plaque index after brushing | Thin film adherent at gingival margin and adjacent tooth surfaces, detectable with probe | 23 (22.8) |
| Variable | Category | Rural (N = 31) | Urban (N = 70) | Total (N = 101) | p-Value |
|---|---|---|---|---|---|
| Age (years) | Mean (SD) | 23.9 (6.9) | 23.0 (4.4) | 23.3 (5.3) | 0.434 1 |
| Range | 20.0–41.0 | 20.0–36.0 | 20.0–41.0 | ||
| Daily brushing frequency | Once a day | 5 (16.1%) | 0 (0.0%) | 5 (5.0%) | <0.001 2 |
| Twice a day | 9 (29.0%) | 48 (68.6%) | 57 (56.4%) | ||
| Three times a day | 4 (12.9%) | 9 (12.9%) | 13 (12.9%) | ||
| After each meal | 13 (41.9%) | 13 (18.6%) | 26 (25.7%) | ||
| Use of dental floss | Yes | 21 (67.7%) | 38 (54.3%) | 59 (58.4%) | 0.206 2 |
| No | 10 (32.3%) | 32 (45.7%) | 42 (41.6%) | ||
| Use of interdental stimulators | Yes | 13 (41.9%) | 23 (32.9%) | 36 (35.6%) | 0.380 2 |
| No | 18 (58.1%) | 47 (67.1%) | 65 (64.4%) | ||
| Use of mouthwash | Yes | 22 (71.0%) | 53 (75.7%) | 75 (74.3%) | 0.615 2 |
| No | 9 (29.0%) | 17 (24.3%) | 26 (25.7%) | ||
| Presence of carious lesions/fillings | Yes | 17 (54.8%) | 42 (60.0%) | 59 (58.4%) | 0.627 2 |
| No | 14 (45.2%) | 28 (40.0%) | 42 (41.6%) | ||
| Number of carious lesions/fillings | 1–2 | 8 (25.8%) | 29 (41.4%) | 37 (36.6%) | 0.266 2 |
| 3–4 | 9 (29.0%) | 13 (18.6%) | 22 (21.8%) | ||
| None | 14 (45.2%) | 28 (40.0%) | 42 (41.6%) | ||
| Presence of signs of gingival inflammation | None | 17 (54.8%) | 56 (80.0%) | 73 (72.3%) | 0.002 2 |
| Gingival recessions | 0 (0.0%) | 4 (5.7%) | 4 (4.0%) | ||
| Simple (gingival bleeding) | 14 (45.2%) | 10 (14.3%) | 24 (23.8%) | ||
| Silness–Loe plaque index before brushing | No plaque | 5 (16.1%) | 17 (24.3%) | 22 (21.8%) | 0.360 2 |
| Thin film adherent at gingival margin and adjacent surfaces | 26 (83.9%) | 53 (75.7%) | 79 (78.2%) | ||
| Loe & Silness gingival index (modified by Lobene) before brushing | Normal gingiva | 18 (58.1%) | 55 (78.6%) | 73 (72.3%) | 0.002 2 |
| Mild inflammation | 8 (25.8%) | 15 (21.4%) | 23 (22.8%) | ||
| Moderate inflammation | 5 (16.1%) | 0 (0.0%) | 5 (5.0%) | ||
| Toothpaste used | Baking soda | 8 (25.8%) | 34 (48.6%) | 42 (41.6%) | <0.001 2 |
| Charcoal | 18 (58.1%) | 9 (12.9%) | 27 (26.7%) | ||
| Lemon | 5 (16.1%) | 27 (38.6%) | 32 (31.7%) | ||
| Loe & Silness gingival index (modified by Lobene) after brushing | Normal gingiva | 18 (58.1%) | 60 (85.7%) | 78 (77.2%) | <0.001 2 |
| Mild inflammation | 8 (25.8%) | 10 (14.3%) | 18 (17.8%) | ||
| Moderate inflammation | 5 (16.1%) | 0 (0.0%) | 5 (5.0%) | ||
| Silness–Loe plaque index after brushing | No plaque | 22 (71.0%) | 56 (80.0%) | 78 (77.2%) | 0.318 2 |
| Thin film adherent at gingival margin and adjacent surfaces | 9 (29.0%) | 14 (20.0%) | 23 (22.8%) |
| Domain/Variable | Category | Absence of Plaque (N = 78) | Baseline Silness–Löe Plaque Index (N = 23) | Total (N = 101) | p Value | Test |
|---|---|---|---|---|---|---|
| Löe & Silness gingival index (Lobene)—after brushing | normal gingiva | 74 (94.9%) | 4 (17.4%) | 78 (77.2%) | <0.001 | Pearson’s χ2 |
| mild inflammation | 4 (5.1%) | 14 (60.9%) | 18 (17.8%) | |||
| moderate inflammation | 0 (0.0%) | 5 (21.7%) | 5 (5.0%) | |||
| Toothpaste used | Bicarbonate | 34 (43.6%) | 8 (34.8%) | 42 (41.6%) | <0.001 | Pearson’s χ2 |
| Charcoal | 27 (34.6%) | 0 (0.0%) | 27 (26.7%) | |||
| Lemon | 17 (21.8%) | 15 (65.2%) | 32 (31.7%) | |||
| Löe & Silness gingival index (Lobene)—before brushing | normal gingiva | 69 (88.5%) | 4 (17.4%) | 73 (72.3%) | <0.001 | Pearson’s χ2 |
| mild inflammation | 9 (11.5%) | 14 (60.9%) | 23 (22.8%) | |||
| moderate inflammation | 0 (0.0%) | 5 (21.7%) | 5 (5.0%) | |||
| Silness–Löe plaque index—before brushing | absence of plaque | 22 (28.2%) | 0 (0.0%) | 22 (21.8%) | 0.004 | Pearson’s χ2 |
| adherent pellicle | 56 (71.8%) | 23 (100.0%) | 79 (78.2%) | |||
| Presence of signs of gingival inflammation | None | 59 (75.6%) | 14 (60.9%) | 73 (72.3%) | 0.097 | Pearson’s χ2 |
| Gingival recessions | 4 (5.1%) | 0 (0.0%) | 4 (4.0%) | |||
| Simple (gingival bleeding) | 15 (19.2%) | 9 (39.1%) | 24 (23.8%) | |||
| Carious lesions/restorations (categories) | 1–2 | 24 (30.8%) | 13 (56.5%) | 37 (36.6%) | <0.001 | Pearson’s χ2 |
| 3–4 | 12 (15.4%) | 10 (43.5%) | 22 (21.8%) | |||
| None | 42 (53.8%) | 0 (0.0%) | 42 (41.6%) | |||
| Any carious lesions/restoration | Yes | 36 (46.2%) | 23 (100.0%) | 59 (58.4%) | <0.001 | Pearson’s χ2 |
| No | 42 (53.8%) | 0 (0.0%) | 42 (41.6%) | |||
| Mouthwash use | Yes | 61 (78.2%) | 14 (60.9%) | 75 (74.3%) | 0.095 | Pearson’s χ2 |
| No | 17 (21.8%) | 9 (39.1%) | 26 (25.7%) | |||
| Interdental stimulators use | Yes | 26 (33.3%) | 10 (43.5%) | 36 (35.6%) | 0.372 | Pearson’s χ2 |
| No | 52 (66.7%) | 13 (56.5%) | 65 (64.4%) | |||
| Dental floss use | Yes | 50 (64.1%) | 9 (39.1%) | 59 (58.4%) | 0.033 | Pearson’s χ2 |
| No | 28 (35.9%) | 14 (60.9%) | 42 (41.6%) | |||
| Brushing frequency (per day) | Once | 0 (0.0%) | 5 (21.7%) | 5 (5.0%) | <0.001 | Pearson’s χ2 |
| Twice | 44 (56.4%) | 13 (56.5%) | 57 (56.4%) | |||
| Three times | 13 (16.7%) | 0 (0.0%) | 13 (12.9%) | |||
| After each meal | 21 (26.9%) | 5 (21.7%) | 26 (25.7%) | |||
| Residence | Rural | 22 (28.2%) | 9 (39.1%) | 31 (30.7%) | 0.318 | Pearson’s χ2 |
| Urban | 56 (71.8%) | 14 (60.9%) | 70 (69.3%) | |||
| Age | Mean (SD) | 23.1 (4.9) | 24.0 (6.5) | 23.3 (5.3) | 0.454 | Linear model ANOVA |
| Range | 20.0–41.0 | 20.0–36.0 | 20.0–41.0 |
| Measure | Category (Score/Definition) | Bicarbonate (Before) | Bicarbonate (After) | Charcoal (Before) | Charcoal (After) | Lemon (Before) | Lemon (After) | Total (Before) | Total (After) | p (Before) | p (After) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Silness–Löe Plaque Index | Absence of plaque | 17 (40.5%) | 34 (81.0%) | 5 (18.5%) | 27 (100.0%) | 0 (0.0%) | 17 (53.1%) | 22 (21.8%) | 78 (77.2%) | <0.001 | <0.001 |
| Grade I | 25 (59.5%) | 8 (19.0%) | 22 (81.5%) | 0 (0.0%) | 32 (100.0%) | 15 (46.9%) | 79 (78.2%) | 23 (22.8%) | |||
| Löe & Silness Gingival Index (modified) | Normal gingiva | 29 (69.0%) | 34 (81.0%) | 27 (100.0%) | 27 (100.0%) | 17 (53.1%) | 17 (53.1%) | 73 (72.3%) | 78 (77.2%) | <0.001 | <0.001 |
| Mild inflammation | 13 (31.0%) | 8 (19.0%) | 0 (0.0%) | 0 (0.0%) | 10 (31.2%) | 10 (31.2%) | 23 (22.8%) | 18 (17.8%) | |||
| Moderate inflammation | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 5 (15.6%) | 5 (15.6%) | 5 (5.0%) | 5 (5.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lile, I.E.; Talpoș-Niculescu, Ș.; Marian, D.; Stana, O.; Stăncioiu, A.-A.; Motofelea, A.C.; Constantin, G.-D. Assessment of Oral Hygiene Practices, Adjunctive Cleaning Methods, and Their Impact on Plaque and Gingival Indices Among Young Adults in Urban and Rural Settings in Romania. Healthcare 2025, 13, 2970. https://doi.org/10.3390/healthcare13222970
Lile IE, Talpoș-Niculescu Ș, Marian D, Stana O, Stăncioiu A-A, Motofelea AC, Constantin G-D. Assessment of Oral Hygiene Practices, Adjunctive Cleaning Methods, and Their Impact on Plaque and Gingival Indices Among Young Adults in Urban and Rural Settings in Romania. Healthcare. 2025; 13(22):2970. https://doi.org/10.3390/healthcare13222970
Chicago/Turabian StyleLile, Ioana Elena, Șerban Talpoș-Niculescu, Diana Marian, Otilia Stana, Andra-Alexandra Stăncioiu, Alexandru Cătălin Motofelea, and George-Dumitru Constantin. 2025. "Assessment of Oral Hygiene Practices, Adjunctive Cleaning Methods, and Their Impact on Plaque and Gingival Indices Among Young Adults in Urban and Rural Settings in Romania" Healthcare 13, no. 22: 2970. https://doi.org/10.3390/healthcare13222970
APA StyleLile, I. E., Talpoș-Niculescu, Ș., Marian, D., Stana, O., Stăncioiu, A.-A., Motofelea, A. C., & Constantin, G.-D. (2025). Assessment of Oral Hygiene Practices, Adjunctive Cleaning Methods, and Their Impact on Plaque and Gingival Indices Among Young Adults in Urban and Rural Settings in Romania. Healthcare, 13(22), 2970. https://doi.org/10.3390/healthcare13222970









