Longitudinal Changes in the Adjusted Body Mass Index (BMI) Percentile Among Children in Riyadh, Saudi Arabia, During and After the COVID-19 Lockdown
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Study Population and Covariates
- Cohort 1 (N = 934): Children who had anthropometric measurements recorded in both before and during the COVID-19 lockdown. This sample was used to evaluate the longitudinal adjusted BMI percentile change during the COVID-19 pandemic lockdown.
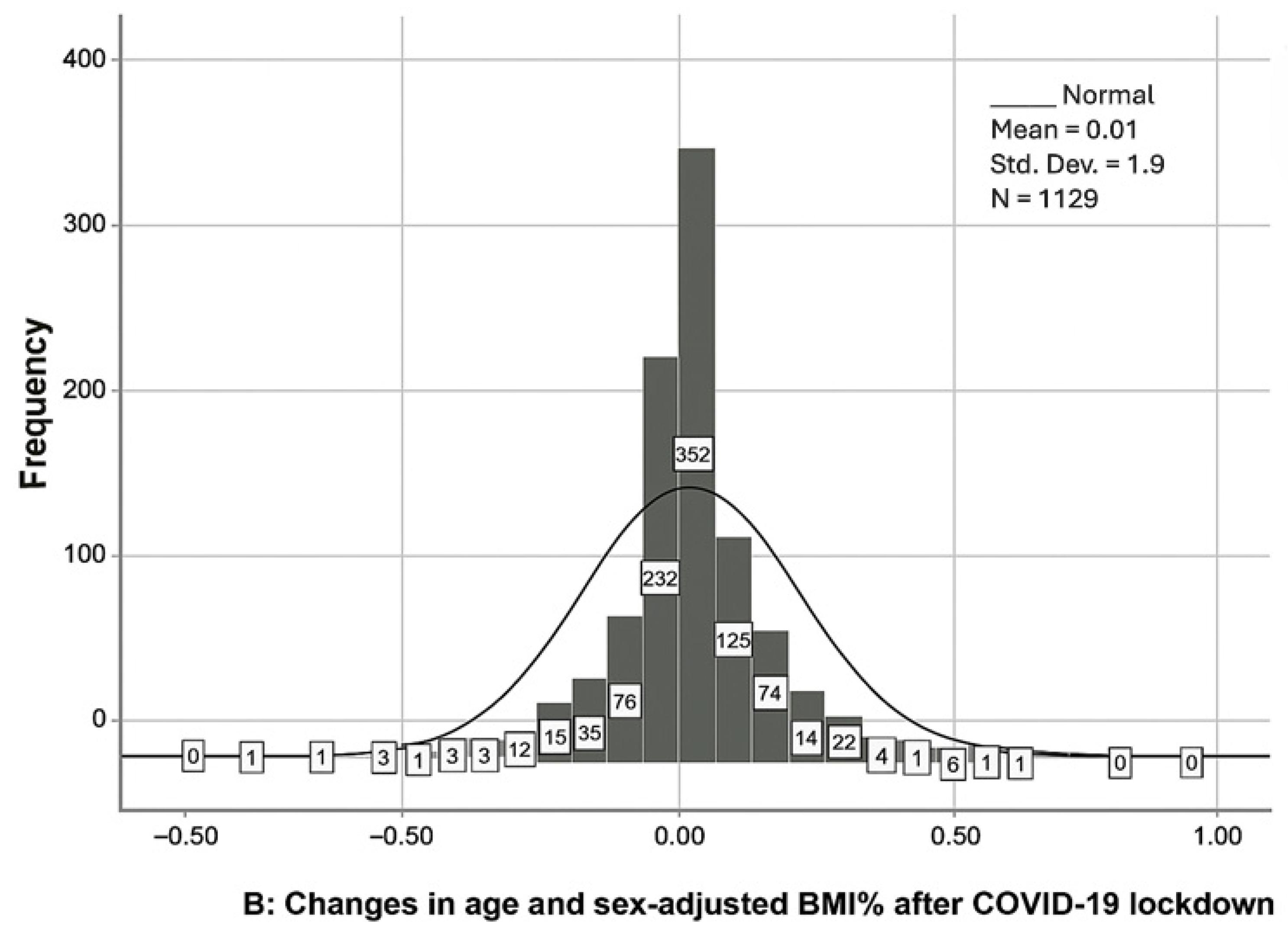
- Cohort 2 (N = 1129): Children with anthropometric measurements recorded during the COVID-19 pandemic lockdown and following the lockdown. This sample was used to evaluate longitudinal age- and sex-adjusted BMI percentile changes within individuals from during to after the lockdown.
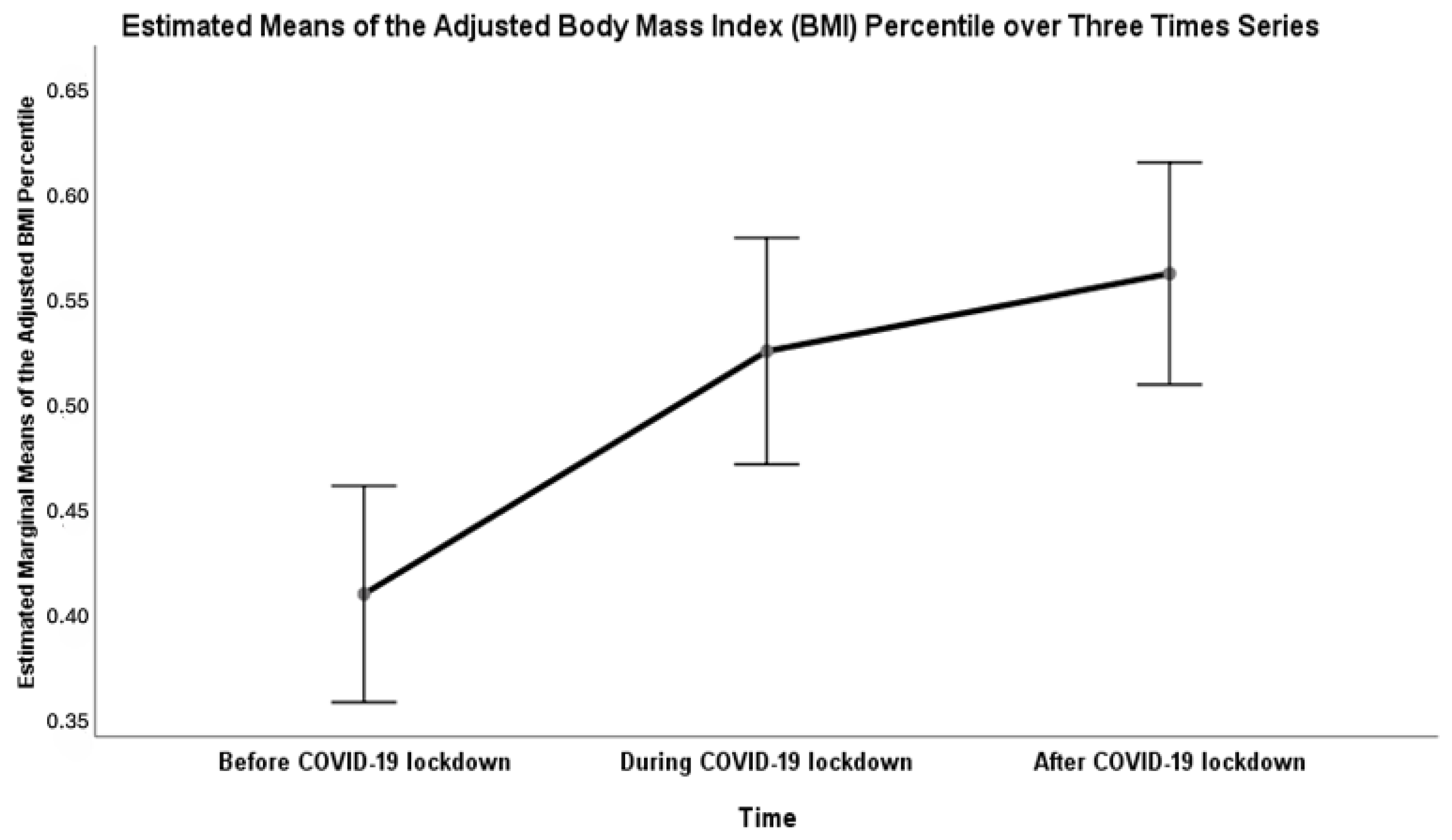
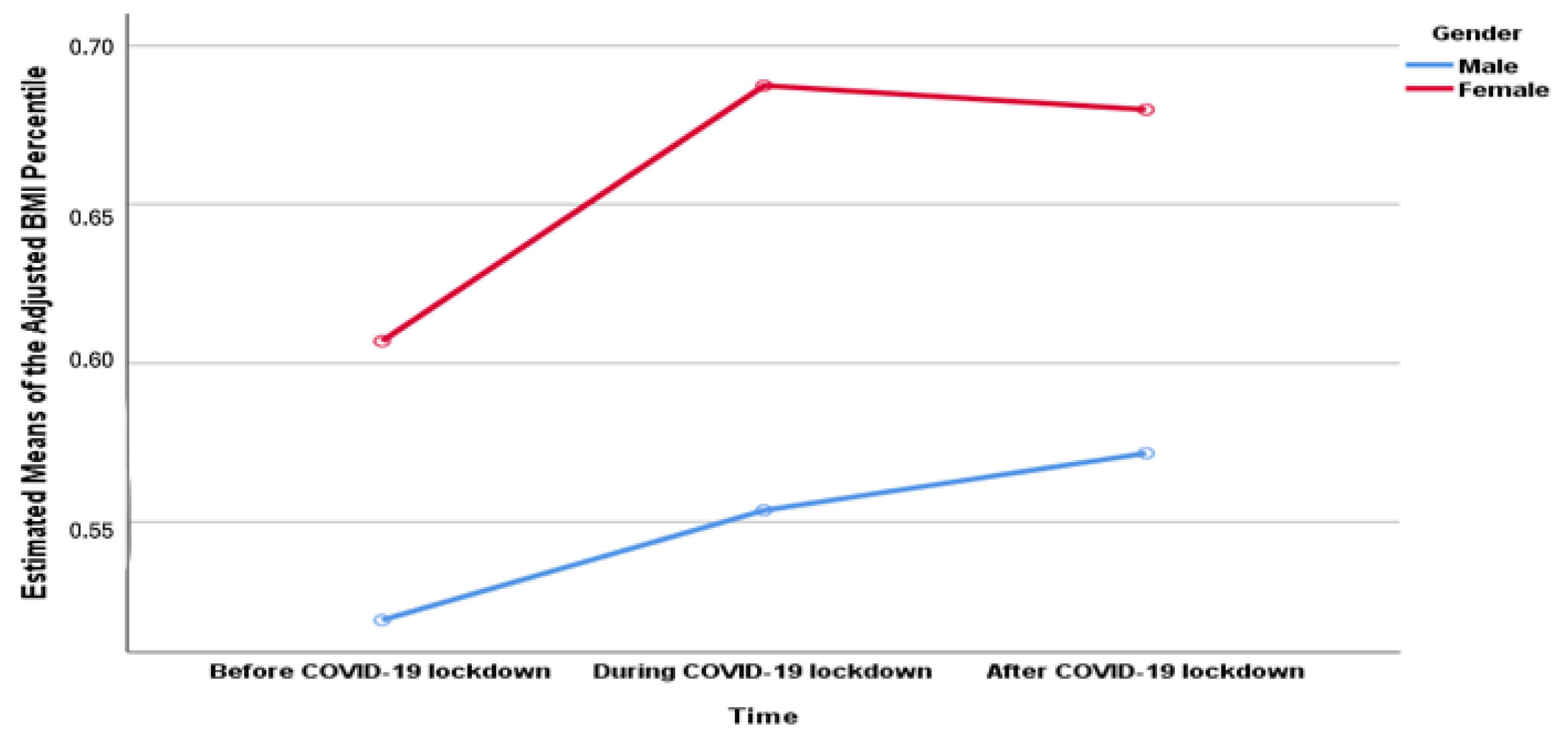
- Cohort 3 (N = 203): Children with anthropometric measurements recorded in all three periods: pre-COVID-19 pandemic, during the lockdown, and after the lockdown. This sample was used to evaluate within-subject changes across the entire pandemic timeline.
2.3. Sample Size
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Asselah, T.; Durantel, D.; Pasmant, E.; Lau, G.; Schinazi, R.F. COVID-19: Discovery, diagnostics and drug development. J. Hepatol. 2021, 74, 168–184. [Google Scholar] [CrossRef]
- WHO. Coronavirus Disease (COVID-19): Situation Report, 181. Available online: https://apps.who.int/iris/handle/10665/333566 (accessed on 1 January 2023).
- Perra, N. Non-pharmaceutical interventions during the COVID-19 pandemic: A review. Phys. Rep. 2021, 913, 1–52. [Google Scholar] [CrossRef]
- Alrashed, S.; Min-Allah, N.; Saxena, A.; Ali, I.; Mehmood, R. Impact of lockdowns on the spread of COVID-19 in Saudi Arabia. Inform. Med. Unlocked 2020, 20, 100420. [Google Scholar] [CrossRef]
- Bhargava, M.; Kandpal, S.D.; Aggarwal, P. Physical activity correlates of overweight and obesity in school-going children of Dehradun, Uttarakhand. J. Fam. Med. Prim. Care 2016, 5, 564–568. [Google Scholar] [CrossRef] [PubMed]
- Hart, C.N.; Raynor, H.A.; Osterholt, K.M.; Jelalian, E.; Wing, R.R. Eating and activity habits of overweight children on weekdays and weekends. Int. J. Pediatr. Obes. IJPO 2011, 6, 467–472. [Google Scholar] [CrossRef]
- Whooten, R.C.; Perkins, M.E.; Gerber, M.W.; Taveras, E.M. Effects of Before-School Physical Activity on Obesity Prevention and Wellness. Am. J. Prev. Med. 2018, 54, 510–518. [Google Scholar] [CrossRef]
- Weaver, R.G.; Armstrong, B.; Hunt, E.; Beets, M.W.; Brazendale, K.; Dugger, R.; Turner-McGrievy, G.; Pate, R.R.; Maydeu-Olivares, A.; Saelens, B.; et al. The impact of summer vacation on children’s obesogenic behaviors and body mass index: A natural experiment. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 153. [Google Scholar] [CrossRef] [PubMed]
- Panchal, U.; Salazar de Pablo, G.; Franco, M.; Moreno, C.; Parellada, M.; Arango, C.; Fusar-Poli, P. The impact of COVID-19 lockdown on child and adolescent mental health: Systematic review. Eur. Child Adolesc. Psychiatry 2023, 32, 1151–1177. [Google Scholar] [CrossRef] [PubMed]
- Luijten, M.A.J.; van Muilekom, M.M.; Teela, L.; Polderman, T.J.C.; Terwee, C.B.; Zijlmans, J.; Klaufus, L.; Popma, A.; Oostrom, K.J.; van Oers, H.A.; et al. The impact of lockdown during the COVID-19 pandemic on mental and social health of children and adolescents. Qual. Life Res. 2021, 30, 2795–2804. [Google Scholar] [CrossRef]
- Chang, T.-H.; Chen, Y.-C.; Chen, W.-Y.; Chen, C.-Y.; Hsu, W.-Y.; Chou, Y.; Chang, Y.-H. Weight Gain Associated with COVID-19 Lockdown in Children and Adolescents: A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 3668. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity 2020, 28, 1382–1385. [Google Scholar] [CrossRef]
- Štveráková, T.; Jačisko, J.; Busch, A.; Šafářová, M.; Kolář, P.; Kobesová, A. The impact of COVID-19 on Physical Activity of Czech children. PLoS ONE 2021, 16, e0254244. [Google Scholar] [CrossRef]
- Lange, S.J.; Kompaniyets, L.; Freedman, D.S.; Kraus, E.M.; Porter, R.; Blanck, H.M.; Goodman, A.B. Longitudinal Trends in Body Mass Index Before and During the COVID-19 Pandemic Among Persons Aged 2–19 Years—United States, 2018–2020. MMWR. Morb. Mortal. Wkly. Rep. 2021, 70, 1278–1283. [Google Scholar] [CrossRef]
- Weaver, R.G.; Hunt, E.T.; Armstrong, B.; Beets, M.W.; Brazendale, K.; Turner-McGrievy, G.; Pate, R.R.; Youngstedt, S.D.; Dugger, R.; Parker, H.; et al. COVID-19 Leads to Accelerated Increases in Children’s BMI z-Score Gain: An Interrupted Time-Series Study. Am. J. Prev. Med. 2021, 61, e161–e169. [Google Scholar] [CrossRef]
- Salman, H.; İssi Irlayici, F.; Akçam, M. The COVID-19 Pandemic and the Prevalence of Childhood Obesity in Turkiye. J. Pediatr. Gastroenterol. Nutr. 2023, 76, e15–e19. [Google Scholar] [CrossRef]
- Yang, Y.; Zhang, M.; Yu, J.; Pei, Z.; Sun, C.; He, J.; Qian, T.; Luo, F.; Zhang, S.; Xu, Z. Nationwide Trends of Pediatric Obesity and BMI z-Score From 2017–2021 in China: Comparable Findings From Real-World Mobile- and Hospital-Based Data. Front. Endocrinol. 2022, 13, 859245. [Google Scholar] [CrossRef]
- Brooks, C.G.; Spencer, J.R.; Sprafka, J.M.; Roehl, K.A.; Ma, J.; Londhe, A.A.; He, F.; Cheng, A.; Brown, C.A.; Page, J. Pediatric BMI changes during COVID-19 pandemic: An electronic health record-based retrospective cohort study. eClinicalMedicine 2021, 38, 101026. [Google Scholar] [CrossRef] [PubMed]
- Florea, M.; Lucia, L.; Puia, I.; Stănescu, A.; Simionescu, A.A.; CORNEAN, R. The challenges of COVID-19-related weight gain in children. Rom. J. Med. Pract. 2021, 16, 66–71. [Google Scholar] [CrossRef]
- Cena, H.; Fiechtner, L.; Vincenti, A.; Magenes, V.C.; De Giuseppe, R.; Manuelli, M.; Zuccotti, G.V.; Calcaterra, V. COVID-19 Pandemic as Risk Factors for Excessive Weight Gain in Pediatrics: The Role of Changes in Nutrition Behavior. A Narrative Review. Nutrients 2021, 13, 4255. [Google Scholar] [CrossRef] [PubMed]
- Irschik, S.; Brandt, J.B.; Eisenkölbl, J. COVID-19 pandemic-related weight gain in the pediatric population declined after restrictions ended, except among obese patients. Front. Public Health 2023, 11, 1260269. [Google Scholar] [CrossRef]
- Moore, K.; Do, B.; Wang, S.; McAlister, K.; Chapman, T.; Belcher, B.; Dunton, G. Long-term effects of the COVID-19 Pandemic on Children’s Physical Activity and Sedentary Behavior. Obes. Sci. Pract. 2023, 10, e710. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Child Growth Standards. Available online: https://www.who.int/tools/child-growth-standards (accessed on 1 January 2023).
- Centers for Disease Control and Prevention. Defining Child BMI Categories. Available online: https://www.cdc.gov/bmi/child-teen-calculator/bmi-categories.html?CDC_AAref_Val=https://www.cdc.gov/obesity/basics/childhood-defining.html (accessed on 1 January 2023).
- Albaker, W.; Saklawi, R.; Bah, S.; Motawei, K.; Futa, B.; Al-Hariri, M. What is the current status of childhood obesity in Saudi Arabia?: Evidence from 20,000 cases in the Eastern Province: A cross-sectional study. Medicine 2022, 101, e29800. [Google Scholar] [CrossRef] [PubMed]
- Ge, W.; Hu, J.; Xiao, Y.; Liang, F.; Yi, L.; Zhu, R.; Yin, J. COVID-19–related childhood BMI increases in China: A health surveillance–based ambispective cohort analysis. Am. J. Prev. Med. 2022, 63, 647–655. [Google Scholar] [CrossRef]
- Woolford, S.J.; Sidell, M.; Li, X.; Else, V.; Young, D.R.; Resnicow, K.; Koebnick, C. Changes in Body Mass Index Among Children and Adolescents During the COVID-19 Pandemic. JAMA 2021, 326, 1434–1436. [Google Scholar] [CrossRef]
- Ochoa-Moreno, I.; Taheem, R.; Woods-Townsend, K.; Chase, D.; Godfrey, K.M.; Modi, N.; Hanson, M. Projected health and economic effects of the increase in childhood obesity during the COVID-19 pandemic in England: The potential cost of inaction. PLoS ONE 2024, 19, e0296013. [Google Scholar] [CrossRef] [PubMed]
- Iacopetta, D.; Catalano, A.; Ceramella, J.; Pellegrino, M.; Marra, M.; Scali, E.; Sinicropi, M.S.; Aquaro, S. The Ongoing Impact of COVID-19 on Pediatric Obesity. Pediatr. Rep. 2024, 16, 135–150. [Google Scholar] [CrossRef]
- Ferentinou, E.; Koutelekos, I.; Pappa, D.; Manthou, P.; Dafogianni, C. The Impact of the COVID-19 Pandemic on Childhood Obesity: A Review. Cureus 2023, 15, e45470. [Google Scholar] [CrossRef]
- Valenzise, M.; D’Amico, F.; Cucinotta, U.; Lugarà, C.; Zirilli, G.; Zema, A.; Wasniewska, M.; Pajno, G.B. The lockdown effects on a pediatric obese population in the COVID-19 era. Ital. J. Pediatr. 2021, 47, 209. [Google Scholar] [CrossRef]
- Knapp, E.A.; Dong, Y.; Dunlop, A.L.; Aschner, J.L.; Stanford, J.B.; Hartert, T.; Teitelbaum, S.L.; Hudak, M.L.; Carroll, K.; O’Connor, T.G.; et al. Changes in BMI During the COVID-19 Pandemic. Pediatrics 2022, 150, e2022056552. [Google Scholar] [CrossRef]
- Moore, S.A.; Faulkner, G.; Rhodes, R.E.; Brussoni, M.; Chulak-Bozzer, T.; Ferguson, L.J.; Mitra, R.; O’Reilly, N.; Spence, J.C.; Vanderloo, L.M.; et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: A national survey. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 85. [Google Scholar] [CrossRef] [PubMed]
- Bond, D.M.; Seimon, R.; Schneuer, F.J.; Baur, L.A.; Craig, M.; Alexander, S.; Garnett, S.P.; Henderson, J.; Nassar, N. Impact and recovery of the COVID-19 pandemic on weight status of children and adolescents. Clin. Obes. 2023, 13, e12579. [Google Scholar] [CrossRef] [PubMed]
- Azrak, M.Á.; Fasano, M.V.; Avico, A.J.; Sala, M.; Casado, C.; Padula, M.; Kruger, A.L.; Malpeli, A.; Andreoli, M.F. Prolonged body weight gain, lifestyle changes and health-related quality of life in children during the COVID-19 pandemic lockdown: A follow-up study. Eur. J. Clin. Nutr. 2023, 77, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Dunford, L.J.; Langley-Evans, S.C.; McMullen, S. Childhood obesity and adult cardiovascular disease risk: A systematic review. Int. J. Obes. 2010, 34, 18–28. [Google Scholar] [CrossRef] [PubMed]
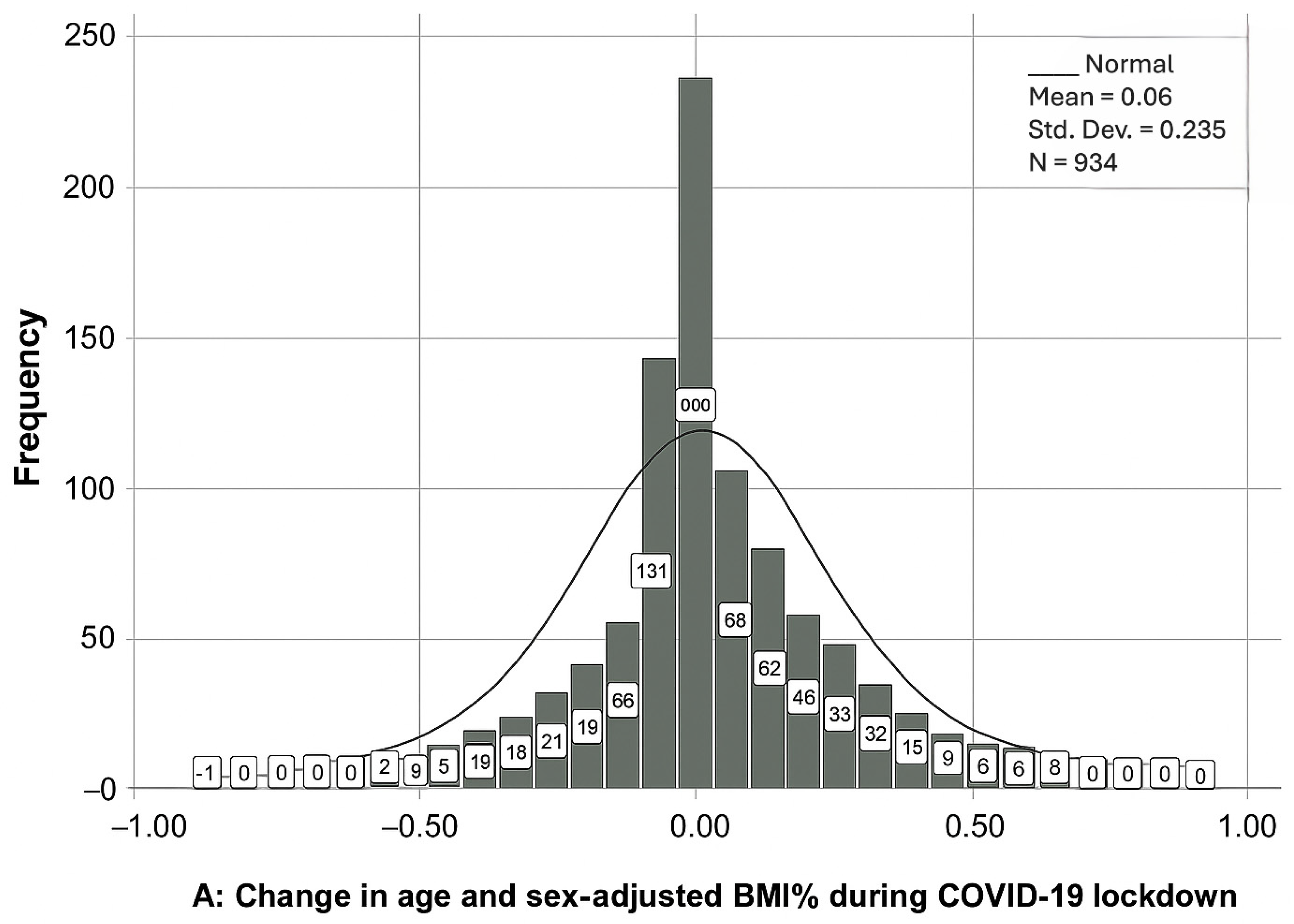
| Variable | N (%) | Change in the Adjusted BMI Percentile | |||
|---|---|---|---|---|---|
| Mean ± SD | p-Value | Effect Size | |||
| Total | 934 (100) | 0.06 ± 0.24 | |||
| Gender | 0.704 a | −0.025 | |||
| Male | 508 (54.4) | 0.06 ± 0.24 | |||
| Female | 426 (45.6) | 0.06 ± 0.22 | |||
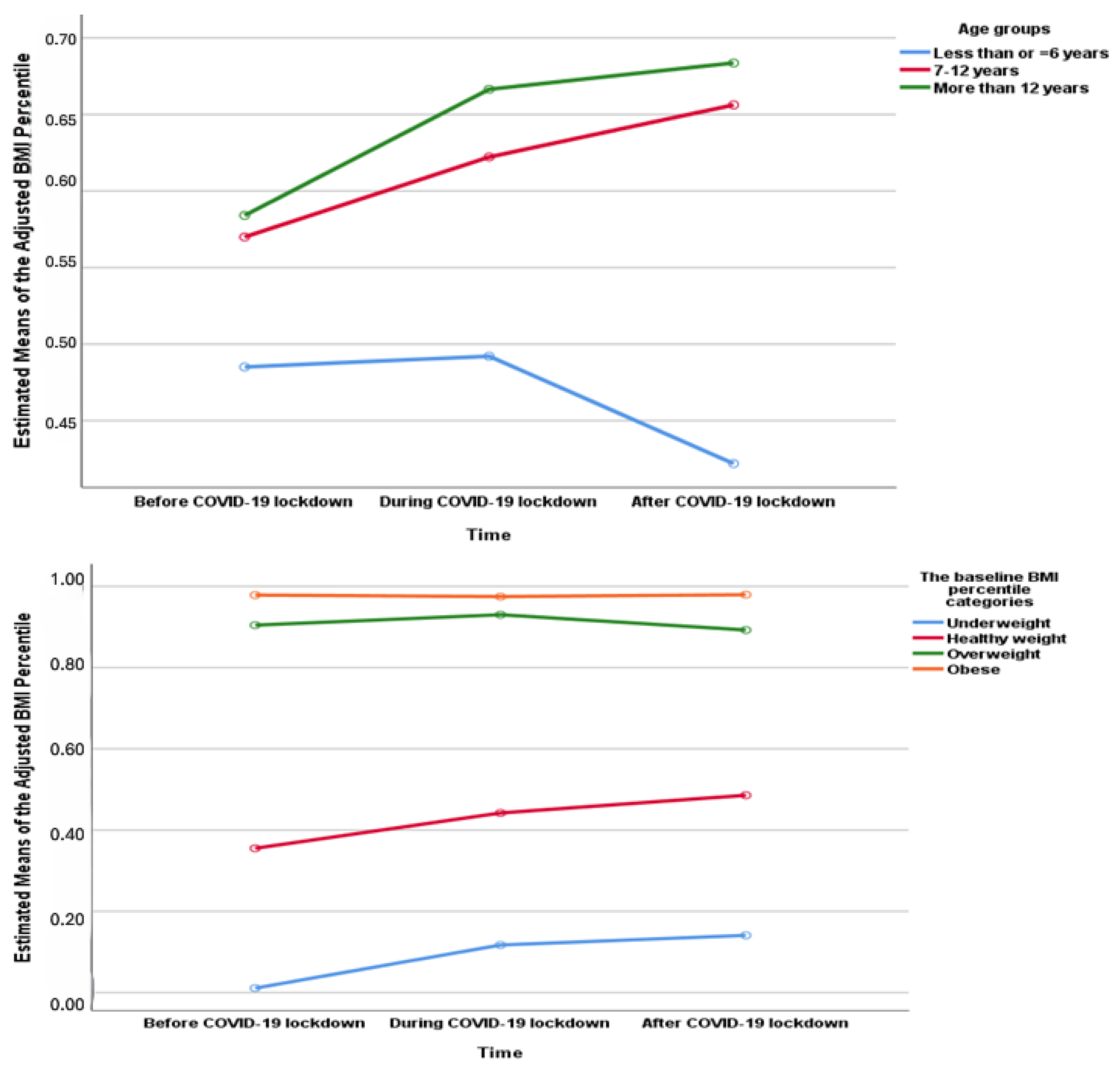
| Age groups | <0.001 b | 0.032 | |||
| Less than or equal to 6 years | 44 (4.7) | −0.13 ± 0.31 | |||
| 7–12 years | 469 (50.2) | 0.08 ± 0.26 | |||
| More than 12 years | 421 (45.1) | 0.05 ± 0.18 | |||
| The baseline weight status | <0.001 b | 0.060 | |||
| Underweight | 166 (17.8) | 0.13 ± 0.21 | |||
| Healthy weight | 559 (59.9) | 0.08 ± 0.25 | |||
| Overweight | 98 (10.5) | −0.05 ± 0.19 | |||
| Obese | 111 (11.9) | −0.04 ± 0.13 | |||
| Variable | N (%) | Change in the Adjusted BMI Percentile | |||
|---|---|---|---|---|---|
| Mean ± SD | p-Value | Effect Size | |||
| Total | 1129 (100) | 0.01 ± 0.19 | |||
| Gender | 0.887 a | 0.008 | |||
| Male | 583 (51.6) | 0.01 ± 0.20 | |||
| Female | 546 (48.4) | 0.01 ± 0.18 | |||
| Age groups | <0.001 b | 0.015 | |||
| Less than or equals to 6 years | 457 (40.5) | −0.02 ± 0.25 | |||
| 7–12 years | 441 (39.1) | 0.03 ± 0.13 | |||
| More than 12 years | 231 (20.5) | 0.02 ±0.13 | |||
| The baseline Body Mass Index Categories | <0.001 b | 0.039 | |||
| Underweight | 151 (13.4) | 0.08 ± 0.18 | |||
| Healthy weight | 652 (56.8) | 0.02 ± 0.21 | |||
| Overweight | 136 (12.0) | −0.05 ± 0.15 | |||
| Obese | 190 (16.8) | −0.04 ± 0.15 | |||
| Variable | N (%) | The Mean of the Adjusted BMI Percentile ± SD | |||||
|---|---|---|---|---|---|---|---|
| Before COVID-19 Lockdown | During COVID-19 Lockdown | After COVID-19 Lockdown | df | p-Value | |||
| Total | 203 (100) | 0.4 ± 0.36 | 0.53 ± 0.37 | 0.56 ± 0.37 | 2 | <0.001 * | |
| Gender | 1 | 0.04 * | |||||
| Male | 110 (54.2) | 0.44 ± 0.36 | 0.54 ± 0.38 | 0.57 ± 0.38 | |||
| Female | 93 (45.8) | 0.39 ± 0.36 | 0.51 ± 0.37 | 0.55 ± 0.36 | |||
| Age groups | 2 | 0.247 * | |||||
| Less than or equals to 6 years | 5 (2.5) | 0.56 ± 0.45 | 0.59 ± 0.54 | 0.48 ± 0.49 | |||
| 7–12 years | 123 (60.6) | 0.39 ± 0.33 | 0.51 ± 0.54 | 0.55 ± 0.36 | |||
| More than 12 years | 75 (36.9) | 0.43 ± 0.39 | 0.56 ± 0.38 | 0.59 ± 0.38 | |||
| The baseline Body Mass Index Categories | 3 | <0.001 * | |||||
| Underweight | 47 (23.2) | 0.01 ± 0.01 | 0.15 ± 0.22 | 0.18 ± 0.25 | |||
| Healthy weight | 117 (57.6) | 0.40 ± 0.26 | 0.54 ± 0.32 | 0.59 ± 0.31 | |||
| Overweight | 22 (10.8) | 0.90 ± 0.03 | 0.89 ± 0.23 | 0.88 ± 0.21 | |||
| Obese | 17 (8.4) | 0.98 ± 0.02 | 0.98 ± 0.02 | 0.98 ± 0.02 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhakami, A.; Alenzi, E.O.; Algariri, N.A.; Assiri, R.A.; Alqahtani, H.M. Longitudinal Changes in the Adjusted Body Mass Index (BMI) Percentile Among Children in Riyadh, Saudi Arabia, During and After the COVID-19 Lockdown. Healthcare 2025, 13, 2875. https://doi.org/10.3390/healthcare13222875
Alhakami A, Alenzi EO, Algariri NA, Assiri RA, Alqahtani HM. Longitudinal Changes in the Adjusted Body Mass Index (BMI) Percentile Among Children in Riyadh, Saudi Arabia, During and After the COVID-19 Lockdown. Healthcare. 2025; 13(22):2875. https://doi.org/10.3390/healthcare13222875
Chicago/Turabian StyleAlhakami, Amal, Ebtihag O. Alenzi, Najla Ali Algariri, Rawan Abdulaziz Assiri, and Hala Muidh Alqahtani. 2025. "Longitudinal Changes in the Adjusted Body Mass Index (BMI) Percentile Among Children in Riyadh, Saudi Arabia, During and After the COVID-19 Lockdown" Healthcare 13, no. 22: 2875. https://doi.org/10.3390/healthcare13222875
APA StyleAlhakami, A., Alenzi, E. O., Algariri, N. A., Assiri, R. A., & Alqahtani, H. M. (2025). Longitudinal Changes in the Adjusted Body Mass Index (BMI) Percentile Among Children in Riyadh, Saudi Arabia, During and After the COVID-19 Lockdown. Healthcare, 13(22), 2875. https://doi.org/10.3390/healthcare13222875






