The Benefits of Medical Group Construction for Healthcare Professionals: A Survey of Six Tightly Knit Pilot Urban Medical Groups
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. Sampling and Recruitment
2.3. Quality Control
2.4. Statistical Analysis
3. Results
3.1. Medical Consortium Construction and Grouping
3.2. Participant Demographics
3.3. Personal Participation and Attitude
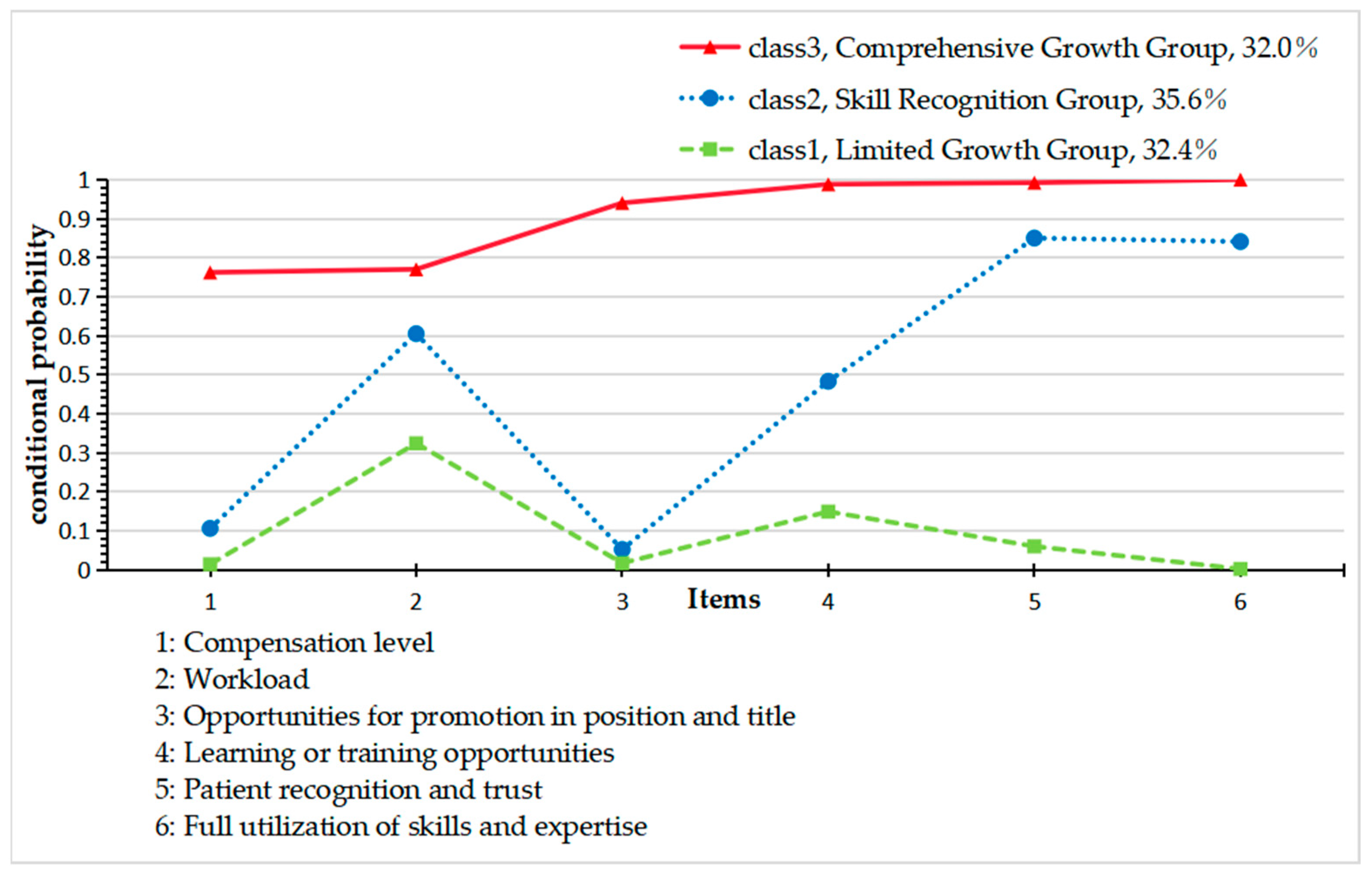
3.4. Latent Classes for Changes in Personal Development After the Construction of TKUMGs
3.5. Logistic Regression Analysis of Factors Influencing Healthcare Professionals’ Personal Development Changes After the Establishment of TKUMGs
3.5.1. Influencing Factors of Healthcare Professionals’ Personal Development Changes After the Establishment of TKUMGs in Leading Hospitals (Table 5)
- C2 Skill Recognition Group vs. C1 Limited Growth Group
- C3 Comprehensive Growth Group vs. C1 Limited Growth Group
- C3 Comprehensive Growth Group vs. C2 Skill Recognition Group
| Comparison Group | Variable/Category | β 2 | SE 2 | Wald χ2 | p-Value | OR 2 (95% CI 2) |
|---|---|---|---|---|---|---|
| C3 1 (Ref: C1 1) | Individual participation level | 0.341 | 0.034 | 101.841 | <0.001 | 1.406 (1.316–1.503) |
| Individual attitude | 1.594 | 0.261 | 37.368 | <0.001 | 4.926 (2.954–8.213) | |
| Institution department (ref: ancillary) | ||||||
| General departments | −0.922 | 0.461 | 3.993 | 0.046 | 0.398 (0.161–0.982) | |
| Other | −2.007 | 0.613 | 10.722 | 0.001 | 0.134 (0.040–0.447) | |
| C2 1 (Ref: C1 1) | Age (ref: >50 years) | |||||
| 41–50 years | −0.824 | 0.407 | 4.087 | 0.043 | 0.439 (0.197–0.957) | |
| Individual participation level | 0.228 | 0.031 | 55.934 | <0.001 | 1.257 (1.153–1.245) | |
| Individual attitude | 0.192 | 0.050 | 14.873 | <0.001 | 1.211 (1.099–1.335) | |
| TKUMG’s score 3 (ref: low) | ||||||
| High-score group | 0.411 | 0.200 | 4.222 | 0.040 | 1.508 (1.019–2.232) | |
| Institution department (ref: ancillary) | ||||||
| Others | −1.422 | 0.447 | 10.112 | 0.001 | 0.241 (0.100–0.580) | |
| C3 1 (Ref: C2 1) | Age (Ref: >50 years) | |||||
| 41–50 years | 0.807 | 0.382 | 4.459 | 0.035 | 2.241 (1.060–4.741) | |
| Individual participation level | 0.113 | 0.029 | 15.238 | <0.001 | 1.119 (1.058–1.184) | |
| Individual attitude | 1.403 | 0.259 | 29.235 | <0.001 | 4.067 (2.446–6.763) | |
| TKUMG’s score 3 (ref: low) | ||||||
| High-score group | 1.098 | 0.336 | 10.666 | 0.001 | 2.244 (1.442–3.493) | |
| Medium-score group | −0.689 | 0.192 | 12.896 | <0.001 | 0.502 (0.345–0.731) | |
| Institution department (ref: ancillary) | ||||||
| General departments | −0.855 | 0.406 | 4.444 | 0.035 | 0.425 (0.192–0.942) | |
3.5.2. Influencing Factors of Healthcare Professionals’ Personal Development Changes After the Establishment of TKUMGs in Member Institutions (Table 6)
- C2 Skill Recognition Group vs. C1-Limited Growth Group
- C3 Comprehensive Growth Group vs. C1-Limited Growth Group
- C3 Comprehensive Growth Group vs. C2 Skill Recognition Group
| Comparison Group | Variable/Category | β 2 | SE 2 | Wald χ2 | p-Value | OR 2 (95% CI 2) |
|---|---|---|---|---|---|---|
| C3 1 (Ref: C1 1) | Education (ref: postgraduate) | |||||
| College or below | 1.307 | 0.410 | 10.141 | 0.001 | 3.693 (1.653–8.254) | |
| Undergraduate | 0.815 | 0.371 | 4.831 | 0.028 | 2.260 (1.092–4.674) | |
| Individual participation level | 0.341 | 0.031 | 123.505 | <0.001 | 1.407 (1.324–1.494) | |
| Individual attitude | 0.994 | 0.164 | 36.483 | <0.001 | 2.701 (1.957–3.729) | |
| Institution department (ref: ancillary) | ||||||
| The five selected clinical departments | 1.071 | 0.422 | 6.449 | 0.011 | 2.918 (1.277–6.667) | |
| General departments | −0.920 | 0.336 | 7.495 | 0.006 | 0.399 (0.206–0.770) | |
| Other | −0.957 | 0.332 | 8.324 | 0.004 | 0.384 (0.201–0.736) | |
| C2 1 (Ref: C1 1) | Individual participation level | 0.167 | 0.025 | 43.699 | <0.001 | 1.182 (1.125–1.242) |
| Individual attitude | 0.195 | 0.035 | 31.302 | <0.001 | 1.216 (1.135–1.302) | |
| C3 1 (Ref: C2 1) | Age (ref: >50 years) | |||||
| ≤30 years | 0.654 | 0.326 | 4.017 | 0.045 | 1.923 (1.015–3.643) | |
| Individual participation level | 0.174 | 0.027 | 42.061 | <0.001 | 1.190 (1.129–1.254) | |
| Individual attitude | 0.798 | 0.164 | 23.678 | <0.001 | 2.222 (1.611–3.065) | |
| Institution department (ref: ancillary) | ||||||
| The five selected clinical departments | 0.798 | 0.349 | 5.233 | 0.022 | 2.221 (1.121–4.400) | |
| General departments | −0.802 | 0.303 | 7.001 | 0.008 | 0.448 (0.248–0.812) | |
| Other | −0.750 | 0.303 | 6.141 | 0.013 | 0.472 (0.261–0.855) | |
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| TKUMGs | Tightly knit urban medical groups |
| LCA | Latent class analysis |
Appendix A
Appendix A.1. Details of the Comprehensive Evaluation Score for the TKUMG’s Construction
| TKUMG | H1 2 | H2 2 | H3 2 | Q1 3 | Q2 3 | Q3 3 | |
|---|---|---|---|---|---|---|---|
| Item | |||||||
| 1. Dimension of Authority and Responsibility Coordination | |||||||
| 1.1. Whether to establish a management committee with the participation of relevant local government departments and the TKUMG. | ○ | ○ | ○ | ○ | ○ | ○ | |
| 1.2. Whether the autonomy of the internal institutions of the TKUMG has been implemented. | ○ | × | × | × | ○ | ○ | |
| 1.3. Whether the autonomy in the job setting for the TKUNMG has been implemented. | × | × | × | × | ○ | ○ | |
| 1.4. Whether the autonomy of the professional title appointment for the TKUMG has been implemented. | × | × | × | × | × | × | |
| 1.5. Whether the autonomy in the selection and appointment of the TKUMG has been implemented. | × | × | × | × | × | ○ | |
| 1.6. Whether the autonomy in the performance distribution within the TKUMG has been implemented. | × | × | × | ○ | ○ | ○ | |
| 2. Dimension of Resource Coordination | |||||||
| 2.1. Integrated management of staff | |||||||
| 2.1.1. Whether unified recruitment is implemented for staff within the TKUMG. | × | × | × | × | × | × | |
| 2.1.2. Whether the staff within the TKUMG are subject to unified assessment. | × | × | × | × | × | × | |
| 2.1.3. Whether the staff within the TKUMG are used in a coordinated manner. | × | × | × | × | × | ○ | |
| 2.2 Integrated financial management | |||||||
| 2.2.1. Whether to set up a financial management center. | ○ | × | × | × | ○ | × | |
| 2.2.2. Whether to coordinate the budget management of the TKUMG. | × | × | × | × | ○ | ○ | |
| 2.2.3. Whether to coordinate the asset management of the TKUMG. | × | × | × | × | × | × | |
| 2.2.4. Whether to coordinate the accounting supervision of the TKUMG. | × | × | × | ○ | ○ | × | |
| 2.3. Integrated management of materials | |||||||
| 2.3.1. Whether to unify the drug management platform. | × | × | × | × | × | × | |
| 2.3.2. Whether to unify the consumables management platform. | × | × | × | × | × | × | |
| 2.3.3. Whether to unify the large-scale equipment management platform. | × | × | × | × | × | × | |
| 2.3.4. Whether the drug formulary is integrated across institutions. | ○ | ○ | ○ | × | × | × | |
| 2.3.5. Whether the integrated distribution and payment for drug procurement have been achieved. | × | × | × | × | × | × | |
| 2.3.6. Whether the integrated distribution and payment for consumables procurement have been achieved. | × | × | × | × | × | × | |
| 2.3.7. Whether the integrated distribution and payment for large-scale equipment procurement have been achieved. | × | × | × | × | × | × | |
| 2.4. Information interconnection and interoperability as well as the joint construction and sharing of high-quality resources | |||||||
| 2.4.1. Interconnection of management information within the consortium. | ⛒ | ⛒ | ⛒ | ⛒ | ⛒ | ○ | |
| 2.4.2. Interconnection of medical records within the consortium. | ⛒ | ⛒ | ⛒ | ⛒ | ⛒ | ○ | |
| 2.4.3. Interconnection of patient information within the consortium. | ⛒ | ⛒ | ⛒ | ⛒ | ⛒ | ○ | |
| 2.4.4. Coordination in the development of shared medical laboratory centers. | ⛒ | ⛒ | ⛒ | ⛒ | ⛒ | ○ | |
| 2.4.5. Coordination in the development of shared medical imaging centers. | ⛒ | ⛒ | ⛒ | ⛒ | ○ | ○ | |
| 2.4.6. Coordination in the development of shared electrocardiogram (ECG) diagnostic centers. | ⛒ | ⛒ | × | ⛒ | ⛒ | × | |
| 2.4.7. Coordination in the development of shared pathology resource centers. | ⛒ | ⛒ | ⛒ | ⛒ | ○ | × | |
| 2.4.8. Coordination in the development of centralized disinfection and supply resource centers. | ⛒ | ⛒ | ⛒ | ⛒ | ⛒ | ○ | |
| 3. Dimension of Business Coordination | |||||||
| 3.1. Whether to unify the integrated management of medical quality and safety. | ○ | ⛒ | ⛒ | ○ | ○ | ○ | |
| 3.2. Whether to unify the integrated management of hospital infection control. | ⛒ | ⛒ | ⛒ | ○ | ○ | ○ | |
| 3.3. Whether to unify the integrated management of medical record quality. | ⛒ | ⛒ | ⛒ | ○ | ○ | ○ | |
| 3.4. Whether to unify the integrated management of prescription circulation. | ⛒ | ⛒ | ⛒ | ○ | ⛒ | ○ | |
| 3.5. Whether to unify the integrated management of disease prevention and control. | ⛒ | ⛒ | ⛒ | ○ | ⛒ | ○ | |
| 3.6. The participation of physicians from secondary and tertiary hospitals in family physician contract service teams. | ○ | ○ | ○ | ○ | ○ | ○ | |
| 3.7. Implementation of collaborative mechanisms with public health professionals. | ○ | ○ | ⛒ | ○ | ○ | ○ | |
| 3.8. Establishment of information coordination with specialized public health institutions. | ⛒ | ○ | ⛒ | ○ | ○ | ○ | |
| 3.9. Collaboration with specialized public health institutions. | ○ | ○ | ⛒ | ○ | ○ | ○ | |
| 4. Dimension of Mechanism Coordination | |||||||
| 4.1. Existence of financial support for the compact urban medical consortium. | ○ | ○ | × | ○ | ○ | ○ | |
Appendix A.2. Results of Univariate Analysis
| Variable/Category | Total (n = 2200) | Class 1 5 (n = 712) | Class 2 5 (n = 783) | Class 3 5 (n = 705) | Teat Statistic | p-Value |
|---|---|---|---|---|---|---|
| Gender, n (%) | χ2 = 1.27 | 0.53 | ||||
| Male | 642 (29.2) | 202 (28.4) | 240 (30.7) | 200 (28.4) | ||
| Female | 1558 (70.8) | 510 (71.6) | 543 (69.3) | 505 (71.6) | ||
| Age, n (%) | χ2 = 39.779 | <0.001 | ||||
| ≤30 | 321 (14.6) | 99 (13.9) a | 83 (10.6) a | 139 (19.7) b | ||
| 31–40 | 992 (45.1) | 324 (45.5) a | 337 (43.0) a | 331 (47.0) a | ||
| 41–50 | 674 (30.6) | 226 (31.7) a | 270 (34.5) a | 178 (25.2) b | ||
| >50 | 213 (9.7) | 63 (8.8) a, b | 93 (11.9) b | 57 (8.1) a | ||
| Education, n (%) | χ2 = 21.274 | <0.001 | ||||
| Junior College and Below | 398 (18.1) | 153 (21.5) a | 148 (18.9) a | 97 (13.8) b | ||
| Bachelor’s Degree | 1432 (65.1) | 462 (64.9) a | 504 (64.4) a | 466 (66.1) a | ||
| Graduate Degree and Above | 370 (16.8) | 97 (13.6) a | 131 (16.7) a, b | 142 (20.1) b | ||
| Professional Title, n (%) | χ2 = 17.682 | 0.007 | ||||
| Junior College and Below | 129 (5.9) | 49 (6.9) a | 40 (5.1) a | 40 (5.7) a | ||
| Bachelor’s Degree | 625 (28.4) | 209 (29.4) a, b | 196 (25.0) b | 220 (31.2) a | ||
| Graduate Degree and Above | 945 (43.0) | 319 (44.8) a | 349 (44.6) a | 277 (39.3) a | ||
| Junior College and Below | 501 (22.8) | 135 (19.0) a | 198 (25.3) b | 168 (23.8) a, b | ||
| TKUMG 1, n (%) (Group according to the TKUMG’s comprehensive evaluation scores 6) | χ2 = 95.745 | <0.001 | ||||
| High-Score Group (Q2 3, Q3 3) | 1225 (57.0) | 444 (62.4) a | 441 (56.3) a, b | 370 (52.5) b | ||
| Medium-Score Group (H1 2, Q1 3) | 753 (34.2) | 235 (33.0) a, b | 303 (38.7) b | 215 (30.5) a | ||
| Low-Score Group (H2 2, H3 2) | 192 (8.7) | 33 (4.6) a | 39 (5.0) a | 120 (17.0) b | ||
| Institution, n (%) | χ2 = 35.812 | <0.001 | ||||
| Leading Hospital | 942 (42.8) | 259 (36.4) a | 319 (40.7) a | 364 (51.6) b | ||
| Member Institution | 1258 (57.2) | 453 (63.6) a | 464 (59.3) a | 341 (48.4) b | ||
| Institution Department, n (%) | χ2 = 248.072 | <0.001 | ||||
| The Five Selected Clinical Departments | 781 (35.5) | 157 (22.1) a | 223 (28.5) b | 401 (56.9) c | ||
| General | 533 (24.2) | 191 (26.8) a | 230 (29.4) a | 112 (15.9) b | ||
| Ancillary | 543 (24.7) | 109 (15.3) a | 129 (16.5) a | 105 (14.9) a | ||
| Other | 343 (15.6) | 255 (35.8) a | 201 (25.7) b | 87 (12.3) c | ||
| Individual Attitude, M (Q1, Q3) 4 | 10.00 (10.00, 10.00) | 10.00 (7.50, 10.00) | 10.00 (10.00, 10.00) | 10.00 (10.00, 10.00) | Hc = 320.135 | <0.001 |
| Individual Participation Level, M (Q1, Q3) 4 | 5.00 (2.50, 8.75) | 2.50 (0.00, 5.00) | 5.00 (2.50, 7.50) | 8.75 (5.00, 10.00) | Hc = 423.853 | <0.001 |
References
- People’s Daily. Over 18,000 Medical Alliances Established Across the Country. 2024. Available online: https://paper.people.com.cn/rmrbwap/html/2024-02/29/nw.D110000renmrb_20240229_5-12.htm (accessed on 30 April 2025).
- General Office of the State Council. Guiding Opinions on Promoting the Construction and Development of Medical Consortia (Guo Ban Fa [2017] No. 32). 2017; Note: This Document Does Not Have an Official English Title. The Translation Provided Is by the Author. Available online: https://www.gov.cn/gongbao/content/2017/content_5191699.htm (accessed on 30 April 2025).
- National Health Commission; National Development and Reform Commission; Ministry of Finance; Ministry of Human Resources and Social Security; National Administration of Traditional Chinese Medicine; National Disease Control and Prevention Administration. Notice on Launching the Pilot Work for the Construction of Close knit Urban Medical Groups (Guo Wei Yi Zhen Han [2023] No. 27). 2023; Note: This Document Does Not Have an Official English Title. The Translation Provided Is by the Author. Available online: https://www.gov.cn/zhengce/zhengceku/2023-02/10/content_5740985.htm (accessed on 30 April 2025).
- Zhu, T.-D.; Yang, M.-J.; Wu, H. Exploration of policy feedback mechanism for healthcare improvement in China: A grounded theory model. Front. Med. 2025, 12, 1496836. [Google Scholar] [CrossRef]
- Piquer-Martinez, C.; Urionagüena, A.; Benrimoj, S.I.; Calvo, B.; Dineen-Griffin, S.; Garcia-Cardenas, V.; Fernandez-Llimos, F.; Martinez-Martinez, F.; Gastelurrutia, M.A. Theories, models and frameworks for health systems integration. A scoping review. Health Policy 2024, 141, 104997. [Google Scholar] [CrossRef]
- Lewis, V.A.; Tierney, K.I.; Colla, C.H.; Shortell, S.M. The new frontier of strategic alliances in health care: New partner-ships under accountable care organizations. Soc. Sci. Med. 2017, 190, 1–10. [Google Scholar] [CrossRef]
- Feng, C.; Zhu, J.; Chen, Y. The evolution and inter-sectoral interaction mechanism of China’s national medical alliance: An analysis based on complex systems theory. Int. J. Health Plan. Manag. 2022, 37, 1454–1476. [Google Scholar] [CrossRef]
- Sano, J.; Hirazawa, Y.; Komamura, K.; Okamoto, S. An overview of systems for providing integrated and comprehensive care for older people in Japan. Arch. Public. Health 2023, 81, 81. [Google Scholar] [CrossRef]
- Liljas, A.E.M.; Brattström, F.; Burström, B.; Schön, P.; Agerholm, J. Impact of Integrated Care on Patient-Related Outcomes Among Older People—A Systematic Review. Int. J. Integr. Care 2019, 19, 6. [Google Scholar] [CrossRef]
- Yu, J.; Su, L.; Feng, L.; Li, Y.; Qiao, L.; Yin, H.; Li, D.; Lei, Y.; Gao, H. Construction of Fracture Liaison Service Scheme Under Medical Alliance Framework in China: A Modified Delphi Method Study. J. Multidiscip. Healthc. 2025, 18, 2201–2213. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xiang, L.; Chen, J.; Cui, Y.; Wang, F.; Zhang, X. The downward referral experiences of stroke caregivers in the regional medical alliance in China: A phenomenological study. Medicine 2022, 101, e31151. [Google Scholar] [CrossRef] [PubMed]
- Liang, L.B.; Li, X.; Liu, X.P.; Li, C.Z.; Luo, D.; Liu, F.; Mao, T.R.; Su, Q.L. Evaluation of the star family doctors training program: An observational cohort study of a novel continuing medical education program for general practitioners within a compact medical consortium: A quantitative analysis. BMC Med. Educ. 2023, 23, 250. [Google Scholar] [CrossRef]
- Kjell, O.N.E.; Diener, E. Abbreviated Three-Item Versions of the Satisfaction with Life Scale and the Harmony in Life Scale Yield as Strong Psychometric Properties as the Original Scales. J. Pers. Assess. 2021, 103, 183–194. [Google Scholar] [CrossRef] [PubMed]
- Han, X.; Li, H.; Xiao, C.; Wang, W.; Gao, K.; Yan, S.; Niu, L. Physical activity enhances college students’ mental health through social adaptability and exercise behavior chain mediation. Sci. Rep. 2025, 15, 21127. [Google Scholar] [CrossRef]
- Sinha, P.; Calfee, C.S.; Delucchi, K.L. Practitioner’s Guide to Latent Class Analysis: Methodological Considerations and Common Pitfalls. Crit. Care Med. 2021, 49, e63–e79. [Google Scholar] [CrossRef]
- Zhonglin, W.; Jinyan, X.; Huihui, W. Principles, Procedures and Programs of Latent Class Models. J. East China Norm. Univ. (Educ. Sci.) 2023, 41, 1–15. [Google Scholar] [CrossRef]
- Zeng, W.; Tao, W.; Yang, Y.; Li, Y.; Lu, B.; Zhao, Q.; Li, Z.; Wang, M.; Shui, Z.; Wen, J. Perceived knowledge, attitudes and practices regarding the medical consortium among medical staff in Sichuan, China: A cross-sectional survey. BMC Health Serv. Res. 2023, 23, 1318. [Google Scholar] [CrossRef]
- Wang, X.; Birch, S.; Zhu, W.; Ma, H.; Embrett, M.; Meng, Q. Coordination of care in the Chinese health care systems: A gap analysis of service delivery from a provider perspective. BMC Health Serv. Res. 2016, 16, 571. [Google Scholar] [CrossRef]
- National Health Commission of China. Notice on Issuing the Measures for the Administration of Medical Consortiums (Trial Implementation) (Guo Wei YI Fa [2020] No. 13). 2020. Available online: https://www.gov.cn/zhengce/zhengceku/2020-07/18/content_5528009.htm (accessed on 30 April 2025).
- Belrhiti, Z.; Bigdeli, M.; Lakhal, A.; Kaoutar, D.; Zbiri, S.; Belabbes, S. Unravelling collaborative governance dynamics within healthcare networks: A scoping review. Health Policy Plan. 2024, 39, 412–428. [Google Scholar] [CrossRef] [PubMed]
- National People’s Congress. Civil Code of the People’s Republic of China, Article 88; Legal document; National People’s Congress: Beijing, China, 2020. (In Chinese)
- Qin, J.; Lin, C.; Zhang, Y.; Zhang, L. The status and challenges of primary health care in China. Chin. Gen. Pract. J. 2024, 1, 182–187. [Google Scholar] [CrossRef]
- Lyons, S.; Kuron, L. Generational differences in the workplace: A review of the evidence and directions for future research. Organ. Behav. 2014, 35 (Suppl. S1), S139–S157. [Google Scholar] [CrossRef]
- Super, D.E. A life-span, life-space approach to career development. J. Vocat. Behav. 1980, 16, 282–298. [Google Scholar] [CrossRef]
- Zhang, Y.M. A Model Study on the Relationship Between Job Satisfaction, Burnout, and Turnover Intention of Doctors in Urban Public Medical Institutions. Ph.D. Thesis, Fudan University, Shanghai, China, 2011. [Google Scholar]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef]
- Xu, R.H.; Zhou, L.; Li, Y.; Wang, D. Doctor’s Preference in Providing Medical Service for Patients in the Medial Alliance: A pilot Discrete Choice Experiment. Int. J. Environ. Res. Public. Health 2020, 17, 2215. [Google Scholar] [CrossRef]
- General Office of the State Council of China. Guiding Opinions of the General Office of the State Council on Promoting the Construction of a Graded Diagnosis and Treatment System (Guo Ban Fa [2015] No. 70). 2015. Available online: https://www.gov.cn/zhengce/content/2015-09/11/content_10158.htm (accessed on 30 April 2025).
| Variable | Assignment/Value |
|---|---|
| Demographics and Professional Background | |
| gender | Man = 1, Woman = 2 |
| age | ≤30 = 1, 31–40 = 2, 41–50 = 3, >50 = 4 |
| education | Junior College and Below = 1, Bachelor’s Degree = 2, Graduate Degree and Above = 3 |
| professional title | None = 1, Junior = 2, Intermediate = 3, Senior = 4 |
| affiliated TKUMG 1 | High-Score Group = 1, Medium-Score Group = 2, Low-Score Group = 3 |
| affiliated institution | Leading Hospital = 1, Member Institution = 2 |
| affiliated department | The Five Selected Clinical Departments = 1, General = 2, Ancillary = 3, Other = 4 |
| Participation and Attitudes Toward the TKUMG 1 | |
| individual attitude | 10-Point Scale |
| individual participation level | |
| Perceived Changes in Personal Development | |
| compensation level | “Decrease” = 1, “No Change” = 2, “Increase” = 3 |
| workload | |
| professional title advancement opportunities | |
| training availability | |
| patient recognition and trust | |
| utilization of one’s skills and expertise | |
| TKUMG 1 | Score in the Dimension of Authority and Responsibility Coordination | Score in the Dimension of Resource Coordination | Score in the Dimension of Business Coordination | Score in the Dimension of Mechanism Coordination | Final Comprehensive Score |
|---|---|---|---|---|---|
| H1 2 | 3.33 | 1.88 | 4.44 | 10.00 | 19.65 |
| H2 2 | 1.67 | 1.25 | 4.44 | 0.00 | 7.36 |
| H3 2 | 1.67 | 1.09 | 1.11 | 0.00 | 3.87 |
| Q1 3 | 3.33 | 2.23 | 10.00 | 0.00 | 15.56 |
| Q2 3 | 6.67 | 3.79 | 7.78 | 10.00 | 28.24 |
| Q3 3 | 8.33 | 3.69 | 10.00 | 0.00 | 22.02 |
| Variable | Leading Hospital (n = 942) | Member Institution (n = 1258) | p-Value |
|---|---|---|---|
| Male, n (%) | 276 (29.3) | 366 (29.1) | 0.916 |
| Age, n (%) | <0.001 | ||
| ≤30 | 158 (16.8) | 163 (13.0) | |
| 31–40 | 487 (51.7) | 505 (50.9) | |
| 41–50 | 232 (24.6) | 442 (35.1) | |
| >50 | 65 (6.9) | 148 (11.8) | |
| Education, n (%) | <0.001 | ||
| Junior College and Below | 62 (6.6) | 336 (26.7) | |
| Bachelor’s Degree | 594 (63.1) | 838 (66.6) | |
| Graduate Degree and Above | 286 (30.4) | 84 (6.7) | |
| Professional Title, n (%) | <0.001 | ||
| None | 36 (3.8) | 93 (7.4) | |
| Junior | 245 (26.0) | 380 (30.2) | |
| Intermediate | 408 (43.3) | 537 (42.7) | |
| Senior | 253 (26.9) | 248 (19.7) | |
| TKUMG 1, n (%) | <0.001 | ||
| H1 2 | 165 (17.5) | 263 (20.9) | |
| H2 2 | 349 (37.0) | 401 (31.9) | |
| H3 2 | 153 (16.2) | 352 (28.0) | |
| Q1 3 | 183 (19.4) | 142 (11.3) | |
| Q2 3 | 89 (9.4) | 77 (6.1) | |
| Q3 3 | 3 (0.3) | 23 (1.8) | |
| Institution Department, n (%) | <0.001 | ||
| The Five Selected Clinical Departments | 598 (63.5) | 183 (14.5) | |
| General | 60 (6.4) | 473 (37.6) | |
| Ancillary | 247 (26.2) | 96 (7.6) | |
| Other | 37 (3.9) | 506 (40.2) | |
| Individual Attitude, M (Q1, Q3) 4 | 10 (10, 10) | 10 (8.75, 10) | <0.001 |
| Individual Participation level, M (Q1, Q3) 4 | 5 (2.5, 8.75) | 3.75 (1.25, 7.5) | <0.001 |
| Number of Classes | AIC 2 | BIC 2 | aBIC 2 | Entropy | BLRT 2 | VLMR 2 | Minimum Class Population Ratio |
|---|---|---|---|---|---|---|---|
| 1 | 20,106.81 | 20,175.17 | 20,137.04 | ||||
| 2 | 16,092.21 | 16,234.62 | 16,155.19 | 0.853 | <0.001 | <0.001 | 48.3% |
| 3 1 | 15,252.99 | 15,469.45 | 15,348.71 | 0.881 | <0.001 | <0.001 | 32.0% |
| 4 | 14,772.48 | 15,062.99 | 14,900.95 | 0.898 | <0.001 | <0.001 | 3.5% |
| 5 | 14,729.71 | 15,094.27 | 14,890.93 | 0.886 | 0.0261 | 0.0251 | 1.3% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tian, C.; Deng, Y.; Gan, T.; Bai, X. The Benefits of Medical Group Construction for Healthcare Professionals: A Survey of Six Tightly Knit Pilot Urban Medical Groups. Healthcare 2025, 13, 2846. https://doi.org/10.3390/healthcare13222846
Tian C, Deng Y, Gan T, Bai X. The Benefits of Medical Group Construction for Healthcare Professionals: A Survey of Six Tightly Knit Pilot Urban Medical Groups. Healthcare. 2025; 13(22):2846. https://doi.org/10.3390/healthcare13222846
Chicago/Turabian StyleTian, Chong, Yiyang Deng, Tian Gan, and Xue Bai. 2025. "The Benefits of Medical Group Construction for Healthcare Professionals: A Survey of Six Tightly Knit Pilot Urban Medical Groups" Healthcare 13, no. 22: 2846. https://doi.org/10.3390/healthcare13222846
APA StyleTian, C., Deng, Y., Gan, T., & Bai, X. (2025). The Benefits of Medical Group Construction for Healthcare Professionals: A Survey of Six Tightly Knit Pilot Urban Medical Groups. Healthcare, 13(22), 2846. https://doi.org/10.3390/healthcare13222846






