Abstract
Although the COVID-19 pandemic negatively affected the health and quality of life of older people (OP), it provided an opportunity for the implementation of telehealth in the areas of Gerontology and Geriatrics, globally and in the countries of Latin America and the Caribbean, which enabled the continuity of healthcare interventions. Therefore, this literature review aimed to (a) conceptualize telehealth in OP through the lens of Gerontology and Geriatrics; (b) analyze the implementation, facilitators, and barriers of telehealth for OP during the COVID-19 pandemic at both global and Latin American and Caribbean regional levels; (c) identify lessons learned and considerations for improving implementation and reducing barriers to telehealth for OP; and (d) discuss challenges related to the integration of telehealth for OP in the region. The databases consulted were PubMed, Scopus, and Scielo; scientific articles in both English and Spanish were considered, including research conducted globally and in Latin American and Caribbean countries that contributed to the objectives of the literature review; the search was conducted from the year 2020 onwards. In addition, government documents and non-governmental technical guidelines from countries in the region were included, whether they focused specifically on older populations or the general population; the search was not limited to a specific time period. Initially, in our search strategy, 1631 scientific articles and 20 governmental and non-governmental documents were identified for the literature review. After eliminating duplicate and applying the inclusion and exclusion criteria, 84 documents were selected for the literature review (46 analyzed the implementation, barriers, and facilitators of telehealth during the COVID-19 pandemic). This literature review presents a conceptual analysis of the implementation and facilitators of, as well as barriers to, telehealth among OP during the COVID-19 pandemic from the perspective of healthcare providers and OP themselves. The paper synthesizes a number of international and Latin American experiences and proposes several recommendations for the implementation of telehealth for OP in the Latin American and Caribbean region. Despite the ongoing challenges regarding telehealth research and training, this review describes telehealth for OP as an intervention approach that improves the provision of holistic care, favoring OP autonomy, functionality, and overall quality of life. This review also proposes telehealth as a regular intervention approach to clinical practice in Gerontology and Geriatrics in the region. Collaborative endeavors are needed to further regulate and promote public policy on telehealth, telemedicine and telerehabilitation for OP.
1. Introduction
Worldwide, the population aged 60 and over will increase from 900 million to more than 1.4 billion people between 2015 and 2030. This represents a 64% increase in just 15 years, making it the fastest-growing age group [1]. Although the situation varies significantly across regions, the Latin America and the Caribbean region is on the verge of an unprecedented shift in its history, with projections indicating an increase from 76 million older persons (OP) today to 147 million by 2037 [1]. Although the region as a whole has entered a stage of accelerated aging, in half of the countries (some of which are among the least developed), the process is still incipient and moderate, with the most significant changes expected to occur between now and 2030 [1].
Although the Coronavirus SARS-CoV-2 (COVID-19) pandemic was a global public health emergency between 2020 and 2023, its health consequences remain a priority for the region [2]. Quarantines, isolation measures, and mobility restrictions were public health strategies implemented during the pandemic. Among OP, longer quarantine periods were observed, overlooking their heterogeneity, health and illness history, life trajectories, and the diverse ways in which people age. This approach disregarded their role as agents of change and full-rights citizens [3], shifting from physical distancing to a form of social exclusion. This distancing had a negative impact on the overall health of OP, defined as a geriatric emergency [3] associated with physical inactivity [4,5], increased susceptibility to chronic diseases and geriatric syndromes [3], and related mental health issues [6,7].
Specifically, various bio-psycho-social challenges were identified among OP during the COVID-19 pandemic. For example, low levels of physical activity (PA) were associated with immunosenescence, increased risk of chronic diseases, frailty, cognitive decline, and mortality [8]; a decrease in muscle mass, muscle strength, and the number of steps per day [4]; sleep problems, insomnia, and daytime sleepiness [3,9]; worsening of pre-existing conditions, such as diabetes, hypertension, angina pectoris, cardiac events, and psychiatric conditions [10]. Poor appetite control was also described (including possible excessive consumption of ultra-processed foods, risk of malnutrition, weight gain or loss), along with reduced exposure to sunlight and vitamin D [9]. The loss of daily routines and the reduction in physical and social contact led to a sense of isolation from the rest of the world, boredom, frustration, uncertainty about the future, and fear of infection [11,12], resulting in stress, distress, and agitation. The situation was further aggravated by the inability to carry out Activities of Daily Living (ADLs) [11,12]. This was accompanied by limited participation in community activities, formal physical activity, and adherence to medical regimens, and public health recommendations [13]. Additionally, the discontinuation of participation in cognitive stimulation activities, workshops, social gatherings, group therapies, and/or volunteer work contributed to increased cognitive decline and depressive symptoms, resulting in reduced social contact and heightened feelings of loneliness [3]. A complex and bidirectional relationship was even described between mental health problems and social disconnection [10], leading to the emergence of social frailty among OP [13]. All these bio-psycho-social challenges affected the resilience that OP had developed throughout their aging process prior to the pandemic.
This global health situation also affected the implementation and continuity of government-led programs for OP, due to lack of access [14]. Likewise, it disrupted in-person research with OP, forcing projects to either suspend operations or implement remote, contactless methods [15,16]. In this context, and as alternatives to help OP maintain their ADLs, the World Health Organization (WHO) encouraged continued social engagement through virtual means and regular physical activity at home [17]. In doing so, the pandemic accelerated innovation in telecommunications and normalized the use of previously underutilized services and products, such as telehealth [15,18], understood as, a modality that utilizes Information and Communication Technologies (ICTs) to pro-vide health services, medical care, and information regardless of distance [19]. This led to an earlier-than-expected implementation of telehealth globally, across various contexts, programs, and services, and for different health conditions, chronic diseases, and geriatric syndromes [20,21,22,23,24,25,26,27,28,29,30,31,32]. In turn, telehealth maintained and/or improved health outcomes by increasing access to care for OP with limited resources, those living in remote geographic areas, individuals with cognitive and/or physical disabilities, or with limited access to transportation; it also enhanced follow-up and quality of care, reduced costs, and facilitated the collection of collateral information during the pandemic [20,33,34,35,36,37,38]. Additionally, it led to the establishment of new models of care [39]. In this context, at the beginning of the pandemic, a scoping review describing the implementation of telehealth for OP, showed a greater experience of telehealth in high-income countries in the Northern Hemisphere. It also indicated a lack of consistency in the concepts associated with telehealth for OP [40], that is, for the field of action of Gerontology and Geriatrics.
Despite a growing body of literature describing the implementation of telehealth in the health systems of some Latin American countries, some countries stand out as having pushed more than others to adopt telemedicine in their health systems, as Argentina, Brazil, Chile, Colombia and Mexico [41], as well as some of the main facilitators and barriers to telehealth in the region [42], these studies have not focused specifically on OP. Therefore, this literature review aimed to (a) conceptualize telehealth in OP through the lens of Gerontology and Geriatrics; (b) analyze the implementation, facilitators, and barriers of telehealth for OP during the COVID-19 pandemic at both global and Latin American and Caribbean regional levels; (c) identify lessons learned and considerations for improving implementation and reducing barriers to telehealth for OP; and (d) discuss challenges related to the integration of telehealth for OP in the region.
2. Materials and Methods
Search Strategy
A literature review was chosen as the methodological approach, as it allows for a broader and more diverse identification of the available literature, as well as a more flexible and context-sensitive exploration [43]. To achieve the objectives of this literature review [43], a bibliographic search was conducted to answer the question: How was telehealth implemented for older people during the COVID-19 pandemic at the global level and in Latin America and the Caribbean region? The keywords and search terms (MeSH/DeCS), in both English and Spanish, were as follows: older adult, older person, older people, old age, aging, aged, elderly, telehealth, telemedicine, telerehabilitation, Covid, Pandemic, SARS-CoV-2, Coronavirus, implement, facilitator, and barrier. The search strategy is described in Appendix A, Table A1.
The databases consulted were PubMed, Scopus, and Scielo. Scientific articles in both English and Spanish were considered, including research conducted globally and in Latin American and Caribbean countries that contributed to the objectives of the literature review. The search was conducted from the year 2020 onwards.
In addition, government documents and non-governmental technical guidelines from countries in the region were included, whether they focused specifically on older populations or the general population. To do this, the research team, made up of members from different countries (Mexico, Costa Rica, Panama, Venezuela, Colombia, Brazil, Ecuador, Argentina, and Chile), reviewed the websites of the health ministries, professional associations, and other non-governmental organizations from countries in the region. The documents included addressed the implementation of telehealth in the countries of the region. The search was not limited to a specific time period.
Conference abstracts, scientific conference reports, dissertations, research reports, theses, case studies, protocols, letters to the editor, and editorials were excluded. The inclusion and exclusion criteria are described in Appendix A, Table A2.
The literature review process followed the steps outlined in references [44,45], depending on the type of document. In the case of scientific articles, the steps included were: search strategy, article identification, removal of duplicates, title and abstract screening, full-text review, selection, data compilation into tables, analysis, interpretation of results and discussion, and referencing. For governmental and non-governmental documents, the steps were: search, identification, full-text review focused on the implementation of telehealth for both OP and the general population in countries of the region, selection, data compilation into tables, analysis, interpretation of results and discussion, and referencing. A reference librarian, part of the research team, contributed to the various stages of the literature review process. This professional contributed to the process by helping with defining keywords, formulating the search strategy, identifying articles, removing duplicates, retrieving the full text of articles for review (from the university’s institutional databases), proposing tables for organizing the results, and compiling the bibliography.
Initially, 1631 scientific articles and 20 governmental and non-governmental documents were identified for the literature review. A total of 254 duplicates were found and removed. After applying the inclusion and exclusion criteria, 84 documents were selected for the literature review (76 scientific articles, 4 governmental documents, and 4 non-governmental documents). Figure 1 presents a flowchart of the article selection process for the literature review.
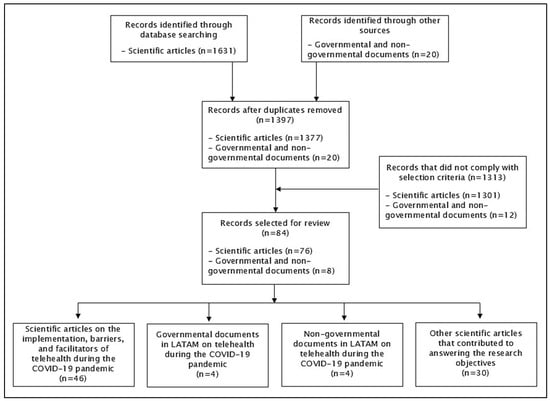
Figure 1.
Flowchart of the article selection process for the literature review, classified by type of document. Abbreviation: LATAM: Latin America.
3. Results
3.1. Conceptualization of Telehealth in Gerontology and Geriatrics
Guidelines from various international, governmental, and non-governmental organizations, both prior to and during the COVID-19 pandemic, they were identified, and thus, established conceptual frameworks related to telehealth [19,46,47,48,49,50]. Consequently, telehealth is understood as a modality that utilizes Information and Communication Technologies (ICTs) to provide health services, medical care, and information regardless of distance [19]. Telehealth is also a tool for disseminating information on the care and prevention of chronic diseases, as well as epidemics [19]. Telehealth is also part of AgeTech, understood as the use of advanced technologies for OP, including both existing devices (such as eyeglasses, walkers, and prosthetics) and emerging technologies (digital media, ICTs, mobile technologies, wearables, and smart home systems) [51], which experienced significant growth during the COVID-19 pandemic [51].
Three key components of telehealth are described: tele-education, telemedicine, and tele-assistance [19,47]. Specifically, telemedicine focuses on the provision of remote health services in the areas of health promotion, prevention, diagnosis, treatment, and rehabilitation. These services are delivered by healthcare professionals who use ICTs to exchange data, with the aim of facilitating access and timely delivery of services for populations facing limited healthcare availability, access barriers, or both, in their geographic area [19,46]. Telerehabilitation, in turn, focuses on the provision of rehabilitation services remotely through the application of telecommunication, remote sensing, operational, and information technologies. Its purpose is to serve individuals, professionals, and systems by minimizing barriers of distance, time, and cost [19,46,50]—a concept that was further reinforced during the COVID-19 pandemic [50]. In summary, telerehabilitation is a branch of telemedicine [50], and telemedicine is a branch of telehealth [19]. Regarding its modality, there are three ways to implement telehealth, telemedicine, and telerehabilitation: synchronous (in real time between the professional and the user); asynchronous (at different times and/or for later review); or hybrid (a combination of both) [19,46].
Telehealth has been incorporated into public health systems in some countries of the region [41]. For example, in the case of Chile, telehealth is understood as a strategy based on the Comprehensive Family and Community Health Care Model, within the context of Integrated Health Service Networks. It facilitates the provision of remote services in the areas of health promotion, prevention, diagnosis, treatment, rehabilitation, and palliative care [19], with a person-centered approach that considers the sociocultural context and life course. The aim is to maintain optimal health status and continuity of care for the population, thereby improving equity in access, rights, timeliness, and quality of care [19]. This intervention was implemented during the pandemic to ensure continuity of care for OP in primary healthcare (PHC) programs [52].
Integrating the conceptualization of telehealth (its components and branches) previously described [19] within the fields of Gerontology (the science of aging) [45,53] and Geriatrics (a branch of this science that focuses on addressing the needs, problems, and geriatric syndromes of OP across different levels of healthcare) [45,54], we propose the concept of Telegerontology, expanding on previous definitions [55]. Additionally, we expand the concept of Telegeriatrics as proposed by the Brazilian Society of Gerontology and Geriatrics [56] for broader application in the region, as summarized in Table 1 and Figure 2.

Table 1.
Concepts of TeleGerontology and TeleGeriatrics for use in the Latin America and Caribbean region.
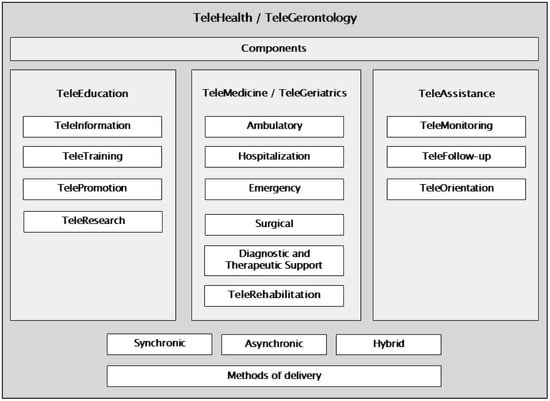
Figure 2.
Components of telehealth, their relationship with the branches of telemedicine and telerehabilitation, and their modalities of delivery; with emphasis on the care of older persons, incorporating the concepts of TeleGerontology and TeleGeriatrics. Own elaboration based on the document “National Telehealth Program in the context of Integrated Health Services Networks” [19].
These updated concepts, which reflect the regional experience of Latin America and the Caribbean, allow for a more precise understanding of the scope of Telehealth (as a care modality) in the fields of Gerontology and Geriatrics, as well as in the daily approach to OP in different contexts, programs, and services; concepts that can also be used in other regions globally (Table 1). Update and integrate these new concepts “Telegerontology” and “Telegeriatrics” into previously published concepts in the field of Telehealth [19], provides a more appropriate representation for the fields of Gerontology and Geriatrics (Figure 2).
3.2. Overview of the Implementation, Barriers, and Facilitators of Telehealth for Older People
This literature review has compiled a total of 46 scientific articles that address the implementation, barriers, and facilitators of telehealth for OP (Appendix A, Table A3). Among these, an integrative review article, published prior to the COVID-19 pandemic, has been included to provide an initial comparative perspective on the barriers and facilitators of telehealth for OP.
Several types of research have been identified: Quantitative (20), Qualitative (12) and Mixed Methods (6). Within quantitative research, primarily through cross-sectional studies. Within qualitative research, primarily through semi-structured interviews. A similar trend can be observed in research using mixed methods. This reflects the need and the resources that researchers had available at the beginning of the pandemic to address this research topic, as well as the diversity of information collected. Furthermore, there are studies that have included some type of intervention (10), primarily analyzed at the end of the intervention.
Most studies focused exclusively on OP, healthy individuals and/or those with various chronic diseases (23), followed by groups of physicians and/or healthcare professionals (7), and then both groups combined (6). In the case of studies using exclusively quantitative methods (excluding mixed methods), the sample sizes ranged from 8 to 3257 OP. For studies using exclusively qualitative methods (excluding mixed methods), the sample sizes ranged from 7 to 98 OP. This reflects the diversity of stakeholders who have reported the information. Two studies presented data on the number of consultations with the Telehealth service.
Globally, the United States is the main country of origin for these studies (15), followed by Canada (5). Specifically in Latin America and the Caribbean, eleven articles on this topic have been identified, published in Chile (5), Mexico (2), Brazil (2), and Peru (2).
Eight review articles were included, providing a broader perspective to support the objectives of this literature review. Three of these review articles specifically included information from countries in Latin America and the Caribbean.
Next, and in the following three sections, we present a narrative and detailed analysis of the research findings, with regard to implementation, barriers, and facilitators of telehealth for OP.
3.3. Implementation of Telehealth for Older People During COVID-19
Older people are the fastest-growing group of ICT users [15]. A study in 1067 OP in Italy conducted during the pandemic identified that smartphones were the most commonly used devices for internet access (59%), WhatsApp was the most frequently used app (57%), internet users were younger than non-users (63 vs. 78 years old), and they had higher educational levels [57]. Furthermore, a study conducted in Chile among 680 OP who used technology during the pandemic showed that 91% of participants considered having internet access useful in their daily lives, and 86% stated that the internet enabled them to access knowledge they would not have obtained otherwise. In addition, participants reported using social media in their everyday lives, including WhatsApp (95%), Facebook (82%), and YouTube (60%) [58].
Regarding the use of telehealth among OP, it increased from 4.6% before the COVID-19 pandemic to 21.1%, with 1 in 3 OP having used telemedicine during the pandemic [32]. Since the onset of the pandemic, there has been growing interest and acceptance of telehealth among OP, with studies indicating that active collaboration between OP and their healthcare providers has been linked to increased acceptance of remote services [40]. It was also reported that OP were more motivated and able to quickly learn new technologies in the context of the pandemic [59], enabling them to continue with their ADLs, exchange informal support with family and neighbors, rely on formal support from community organizations, and remain physically active as part of their resilience [60].
A scoping review investigating the use of telehealth in geriatrics revealed that telehealth interventions targeting OP at the onset of the pandemic focused predominantly on curative services, rather than on promotional—preventive care and rehabilitation [40]. However, these services were predominantly available in high-income countries of the Northern Hemisphere, compared to those in the Global South and middle- to low-income countries [40], such as those in the Latin American region. In addition, there was a greater focus on research about telehealth for OP based on information provided by healthcare providers, both during the beginning of the pandemic [61,62,63], and prior to it [64].
Several international experiences [13,65,66,67,68,69,70,71] demonstrated that telehealth made it possible to ensure continuity of care for OP and reduce the risk of infection during the pandemic [23,72,73]. However, at the global level, there is still a lack of studies that explore in depth issues such as the safety, usefulness, usability, scalability, cost-effectiveness, facilitators and barriers, and demand for the use of telehealth in gerontology and geriatrics. Therefore, there is a clear need for research in these areas now that the COVID-19 pandemic has ended [40], so that the lessons learned can help identify the specific needs of OP when designing and managing future telehealth interventions [65].
Potential uses of telehealth for OP include: remote monitoring of chronic diseases (e.g., vital signs, weight, blood glucose), receiving laboratory results and medical reports, access to personal medical records, and medical/professional consultations via videoconference [9]. Potential uses of telerehabilitation for OP have also been proposed, including: facilitating transitions of care between different healthcare settings (e.g., acute care hospitals, rehabilitation centers, long-term care facilities, home care), preventing falls and reducing functional decline, cognitive rehabilitation, targeted therapy for specific conditions (e.g., heart disease, osteoarthritis), addressing loneliness and social isolation, and monitoring safety in the home environment [9].
A systematic review exploring the application and implementation of telehealth services for OP during the pandemic identified the following services: triage and monitoring, remote monitoring and treatment, online follow-up for residents in healthcare facilities, and the use of online services involving various types of telehealth applications. These applications included phone calls, live videoconferencing, online programs, smartphone apps, Internet of Things (IoT), cloud computing, and social media—mostly reported in countries in the Northern Hemisphere [66]. To ensure the security and privacy of telehealth services, the U.S. Department of Health and Human Services provided a list of video communication providers that comply with the Health Insurance Portability and Accountability Act (HIPAA) [47].
Regarding the specific analysis of the implementation of telehealth with OP during the pandemic, a qualitative study conducted in 2020 through interviews with geriatricians, primary care physicians, and emergency doctors in both rural and urban settings in the United States described telehealth as a more flexible, value-based, and user-centered mode of care [61]. The authors identified several benefits of using telehealth with OP, including the reduction in delayed care and the increase in timely attention, improved efficiency of physicians, enhanced communication with caregivers and OP, reduced travel burdens for the elderly, and greater facilitation of health education and outreach [61]. The same study described several challenges, including unequal access in rural areas and the care of OP with cognitive impairments [61]. Other reported benefits have included greater time efficiency and the delivery of visual information through videoconferencing, as well as increased convenience and safety [34,74,75].
Moreover, in the context of PHC in the United States, a qualitative study conducted in 2021—including interviews with 29 OP and three focus groups with professionals—found that telemedicine contributed to continuity of care. Also, in this same country, another research mixed-method carried out in 80 OPs identified socio-emotional connection and comfort as benefits, and technological barriers and loss of the face-to-face experience as challenges [76]. It was particularly convenient when there was a pre-existing or established doctor–patient relationship or when addressing minor health concerns. It was also beneficial for individuals with reduced mobility, as it reduced their exposure to potentially high-risk environments [23].
From a telehealth management perspective, a series of strengths, weaknesses, threats, and opportunities related to telehealth for OP were synthesized at the beginning of the COVID-19 pandemic [40]. Identifying them would allow for the design and implementation of more optimal telehealth strategies for OP (in both intervention and/or research contexts), whether during a pandemic or under normal circumstances. This also highlights the need to further explore this analysis both during and after the pandemic.
Implementation of Telehealth for Older People, Before and During COVID-19 in Latin America and the Caribbean
In the Americas, in the 20 years prior to the COVID-19 pandemic, there has been an increase in resources and technical capacity, an improvement in digital education, patient empowerment in their treatment, and greater public interest in telemedicine; he formation of interdisciplinary teams, academic and professional networks, and virtual medical consultations, have been considered particularly successful [42]. During the pandemic, Chile, Brazil, Colombia, Mexico, Argentina and Peru were the countries that made the most progress in the field of telehealth in Latin America, both within their health systems and/or through legislation, increasing its use in recent years [41].
Specifically regarding OP, during the pandemic, the Chilean Ministry of Health urged the teams of the primary healthcare program “Más Adultos Mayores Autovalentes (+AMA)” to implement the intervention through telehealth modalities (synchronous, asynchronous, and/or supported by manuals), depending on local resources and training [52]. This approach incorporated local experiences and was seen as an adaptation to alternative forms of contact. Other countries in the region have also developed recommendations for implementing telehealth for OP. For instance, at the end of 2023, the Brazilian Society of Gerontology and Geriatrics published the Telegeriatrics Guide [56]. However, there are still few guidelines or recommendations on telehealth with an emphasis on gerontology and geriatrics in the region.
Additional benefits have been reported regarding the implementation of telehealth with OP from the perspective of healthcare personnel and patients. A user satisfaction survey conducted during the COVID-19 pandemic in Peru reported that, out of a total of 129 healthcare workers, more than 55% of professionals expressed satisfaction with telehealth [77]. On the other hand, approximately 77% of 377 patients (including 44 OP) reported being satisfied with telehealth services. [77].
Specifically, published experiences have been identified on the implementation of telehealth interventions focused on OP in countries of the region, such as the psychosocial teleassistance program of Peru’s Social Security, which provided 154,280 follow-ups and 36,492 teleassistance services to OP—mainly involving emotional support and social counseling [78]; the TeleCOVID-MG program in two municipalities in Brazil, which offered support to OP [79]; a multidisciplinary intervention conducted in Mexico involving 44 OP with colorectal or gastric cancer from a geriatric oncology clinic, where geriatric assessments, treatment toxicity evaluations, physical exams, and treatment prescriptions were performed using platforms such as WhatsApp or Zoom [80]; a semi-presential technological platform (mobile dental clinic combined with a digital platform) designed to support urgent and priority dental care for OP in five regions of Chile [81]; and telehealth-based evaluations, such as the use of the Phototest to identify mild cognitive impairment in OP with memory complaints from rural areas in southern Chile [82]. Additionally, there are reported experiences that have included OP (average age of 68 years), such as a multidisciplinary supportive care program for individuals with advanced cancer in Mexico. In this program, the most common interventions were psychological care (33%), pain and symptom management (25%), and nutritional counseling (13%). Half of the interventions were delivered via videoconference [83]. Also, in Chile, an online course on healthy aging was implemented for the community and health professionals, which included 20% of OP [84].
Additionally, some interventions initially delivered in person were later continued via telehealth. One example is Brazil’s Playful Living Program, aimed at delivering clown-based performances to OP with aphasia [85]. This telehealth-based intervention included not only clowning but also dance, storytelling, and cooking (safe complementary therapies), delivered through individual and group video calls. It involved the participation of professionals and undergraduate and graduate students from the fields of Speech and Language Therapy, Theater, Psychology, Dance, Culinary Arts, Psychiatry, and Public Health [85]. In addition, to facilitate access for OPs, they received donated technological devices; to improve affordability, they were provided with internet credit donations necessary to stay connected; and to support digital capacity, assistance was offered to help them use the technology [85]. Also in Chile, +AMA—the government program that began in 2015, [52], transitioned from an in-person format to an asynchronous telehealth modality, as a pilot in one of the cities where it is implemented. In its in-person format, it is a health promotion and prevention intervention within PHC, which provides physical activity, cognitive stimulation, and education to OP in the community. During the pandemic, the local team transitioned to an asynchronous telehealth modality through videos uploaded to YouTube and infographics stored on Facebook, which were shared weekly via WhatsApp with OP groups so they could carry out the activities [71]. Monthly telephone follow-ups were conducted. Additionally, during the final month of the intervention, a manual containing the same exercises/activities (including a weekly check-up schedule) was delivered in person to the OP, along with other materials. This intervention has been described in detail previously [71].
3.4. Telehealth Facilitators for Older People, Before and During COVID-19
Before the COVID-19 pandemic, an integrative review identified several facilitators that contributed to the acceptance of telehealth by OP with chronic physical conditions. These included: devices with fewer buttons, automatic information transmission, use of low-tech platforms (such as telephones or televisions), devices that provided reminders or alerts (either visual or audio-guided), and user-friendly images [64]. In addition, a systematic mixed-methods review analyzing telemedicine in OP in primary healthcare settings (mostly from studies published before the pandemic) identified the most frequently cited facilitator as location and travel time savings [86].
During the pandemic, qualitative studies involving healthcare providers described additional facilitators of telehealth use in OP [34,63,69]. The first study, conducted in 2020, interviewed 13 healthcare providers in the United States (including medical/clinical directors, program managers, clinical nurses/managers, and clinical social work managers) who provided synchronous telehealth via videoconference to medically complex OP. It identified the following facilitators: assessment of patient needs, collection of information from OP, and increased scheduling capacity [63]. The second study, conducted in the same year, interviewed 33 geriatricians and primary care physicians in the United States to explore their experiences with telemedicine and to identify strategies used to maintain continuity of care for OP [69]. This study reported that many physicians successfully bridged the digital divide by assessing OP’s technological readiness in advance, educating them about telehealth privacy and utility, being flexible with telehealth modalities, using the home or available facilities, making accommodations for disabilities, and involving caregivers [69]. The third study, conducted between 2020 and 2021, interviewed 29 geriatric care physicians in Canada and identified the presence of a caregiver and administrative support as key facilitators of telemedicine use with OP [34]. Additionally, a mixed-methods study conducted in 2020 interviewed 30 professionals—geriatricians, geriatric psychiatrists, and geriatric nurses in Canada—regarding the use of telemedicine technologies with frail OP, their families, and caregivers. The study identified several facilitators, including relative advantage, adaptability, tension for change, available resources, access to knowledge, networks and communication, compatibility, knowledge and beliefs, self-efficacy, champions, external agents, execution, and reflection and evaluation [87].
Other features of synchronous telehealth visits via videoconference have been highlighted as additional opportunities for intervention, as they allow professionals to observe the OP’s home environment [75]—something that in-clinic visits rarely offer. For example, gait assessments revealed mobility obstacles in the home that increased the risk of falls and injuries [65]. Additionally, medication reviews allowed providers to observe how medications were stored and administered [65]. Inviting professionals into the OPs home environment also enabled more direct conversations. Those OPs and caregivers who had previously participated in a video visit reported being more likely to accept a video call visit in the future [65]. At the same time, the use of audio and video equipment of adequate quality (including adaptive devices such as pocket speakers) facilitated these virtual assessments [88]. For its part, regarding asynchronous telehealth, it has been shown that the volume of follow-up, response time, and the quality-related variables involved in service delivery are critically important to ensure patient/user satisfaction, programmatic success, and the sustainability of the intervention [20]. Among the methodologies used, the use of WhatsApp has been described as reducing loneliness among OP [89], and more generally, the use of technology (in various forms) is considered a strategy to address loneliness in OP living alone [90].
A mixed-methods study conducted in the United States in 2020, involving 3 patients, 4 caregivers, 19 physicians, 5 medical assistants, and 2 programers, identified customer service support and the existence of protocols to guide patients in the use of telemedicine as key facilitators of video consultations [91]. Specifically regarding OP, a qualitative study conducted in New Zealand in 2021 aimed at identifying facilitators for the use of telehealth in underserved rural populations—through seven focus groups and thirteen individual interviews across four diverse communities—found that the term telehealth was not initially understood by many participants and required clarification [92]. Those who had used telehealth reported positive experiences—such as saving time and costs—and were likely to use it again [92]. Facilitators also included trust in telehealth technology (reliable and accessible internet access, and access to digital devices); trust in the user experience through the relationship between the consumer and healthcare provider (such as the availability of user support); and trust in the healthcare system (regarding wait times, communication and coordination, and cost) [92]. Additionally, facilitators included access to culturally appropriate healthcare services, the type of consultation (enabling access to specialized services), and the implementation of telehealth (through a fixed community center or a mobile bus unit, with support available—especially when combined with non-health services such as online banking) [92].
Telehealth Facilitators for Older People During COVID-19 in Latin America and the Caribbean
From the perspective of healthcare providers in the Latin American region, evidence on facilitators of telehealth for OP during the pandemic is limited. However, insights can be drawn from the perspective of OP telehealth users, as demonstrated in a qualitative study conducted in Chile in 2020. This study used in-depth semi-structured interviews with 26 community-dwelling self-sufficient OP (14 participated in the telehealth intervention, and 12 served as non-intervention controls) [71]. These OP participated in the government intervention program +AMA [52]. This is a multicomponent intervention (Physical Activity, Cognitive Stimulation, and Education) that, during the pandemic, was delivered through an asynchronous telehealth modality (videos, infographics, and a manual) to ensure continuity of care [52]. The OP had previously participated in the same intervention in its in-person format in earlier years. Following thematic analysis, the OP identified the following as facilitators: participating in the intervention alongside others, prior experience with the in-person modality, good digital literacy, self-motivation, commitment to the program, and the emergence of natural leaders [71]. In addition, the OP identified several positive aspects of this modality, such as the sustainability of the effects between the in-person and telehealth formats, the bio-psycho-social benefits achieved through telehealth, the fact that telehealth helped establish a routine, the guidance and instructions provided by professionals, and the flexibility to carry out the intervention at any time and place, which fostered a sense of autonomy and flexibility [71].
3.5. Telehealth Barriers for Older People, Before and During COVID-19
Prior to the pandemic, the aforementioned review [64], also described intrinsic barriers to the use of technology. These included font size, the use of unusual characters (which are difficult to read), soft graphics and poor color contrast, devices with widgets (which pose challenges for fine eye-hand motor coordination), the use of a computer mouse (difficult for individuals with hand arthritis), lack of experience using a smartphone or computer, multiple screen transitions required to complete tasks, multi-layered menu bars, inappropriate smartphone size (either too large or too small), and difficulties handling devices among many OP with reduced grip strength [64]. Delays in responses, lack of feedback, and technical problems can lead to frustration and decrease motivation for OP to continue engaging in self-care activities. Likewise, for OP who are not accustomed to using technology, telehealth can represent a significant cultural shift [64]. Moreover, in the previously mentioned mixed-methods systematic review [86], the most frequently cited barrier was user habits or preferences.
During the COVID-19 pandemic, additional barriers were described. A quantitative study involving surveys with 16 primary care physicians from a U.S.-based program serving 873 community-dwelling OP aimed to identify barriers to synchronous (video-based) telehealth. The study found that over one-third of these OP participated in video-based telehealth visits for the first time between April and June 2020. It also reported that most required assistance from a family member and/or paid caregiver to complete the visit. Among OP who had not used telehealth, 27% were unable to engage via video due to factors such as cognitive or sensory impairments, while 14% lacked access to a caregiver who could assist them with the technology [62]. Similarly, physicians were unaware of their OP patients’ internet connectivity, ability to afford mobile phone plans, or access to video-capable devices [62]. In another qualitative study conducted in 2020, involving interviews with 13 synchronous (video-based) telehealth providers in the United States who worked with medically complex OP, the reported barriers included cognitive and sensory abilities, access to technology, reliance on caregivers and aides, addressing sensitive topics, and incomplete examinations [63]. A mixed-methods study conducted in 2020 in Canada, which interviewed 30 professionals (geriatricians, geriatric psychiatrists, and geriatric nurses), identified several barriers to telemedicine for frail OP, their families, and caregivers. These included complexity, quality of design and presentation, patient needs and resources, readiness for implementation, and cultural factors [87]. More recently, a qualitative study conducted between 2020 and 2021 with 29 geriatric care physicians in Canada identified several barriers to telemedicine, including difficulties using technology, patients’ sensory impairments, lack of hospital support, and a high volume of pre-existing patients [34].
In the previously mentioned 2020 study conducted in the United States with 33 participants (including 3 patients, caregivers, physicians, medical assistants, and programers), the identified barriers to video consultations included difficulties navigating technology, concerns about privacy, and lack of technical support [91]. Additionally, a quantitative study conducted in 2021 in Canada, involving surveys with 39 healthcare providers, 40 patients with multiple comorbidities, and 22 caregivers from outpatient clinics at a tertiary hospital—who had received phone visits—expressed interest in future telehealth visits. They identified similar barriers: lack of access to technology and skills, the perception that telehealth may be inferior to in-person visits, lack of administrative support, limited technological skills among both healthcare professionals and patients, and limited access to infrastructure and internet [93].
Also, in a qualitative study conducted in 2021 in the United States involving 29 OP from primary care, participants expressed concerns about the lack of eye contact, which they felt led healthcare professionals to overlook essential details. They also identified issues related to poor communication due to language or hearing barriers [23]. Similarly, in a qualitative study conducted in 2021 with 20 OP in Canada, identified barriers to telehealth included the need for physical examination and touch, lack of nonverbal communication, difficulties using technology, and systemic barriers to access [74]. Furthermore, in a qualitative study conducted with 14 OP in Israel, they expressed concern about the potential for poorer quality of telemedicine sessions compared to in-person sessions, and they also expressed a lack of trust in telemedicine services and frustration with the lack of face-to-face interaction and communication [94]. Additionally, in a mixed-methods study conducted in 2021 in the United States with 249 OP residing in independent living facilities in the community, the main barriers to video visits included not knowing how to connect to the platform, lack of familiarity with technology and the internet, difficulty hearing, limited English proficiency, and lack of interest in seeing providers outside the clinic setting [95]. In addition to the above, in a qualitative study of 78 OP in Singapore, they preferred in-person consultations due to a perceived lack of human interaction and diagnostic accuracy, low digital literacy, and a lack of access to telehealth-compatible devices [96].
Telehealth Barriers for Older People During COVID-19 in Latin America and the Caribbean
In the Latin American region, while there is limited evidence on telehealth barriers for OP during the pandemic from the perspective of providers, there is information from the perspective of OP users. A quantitative study, which surveyed 237 OP in Brazil participating in the TeleCOVID-MG program, identified certain personal barriers such as being over 80 years old, having lower educational levels, and experiencing hearing and visual impairments—all of which were associated with the need for support during teleconsultations. This need for support was also associated with hospitalization and mortality [79]. Also, in a quantitative study conducted in 2020 in Chile surveying 34 OP, participants received physical exercise and pain education videos over a 4-week period to be performed independently at home (asynchronous telehealth) [97]. The average adherence was 2 days per week over 2.5 weeks, with the main barrier identified as a lack of willingness to perform the activities. This reluctance was more common among individuals who had engaged in group physical exercise before the pandemic [97]. Additionally, in the previously described 2020 study [71], OP who participated in the asynchronous telehealth intervention reported pain during physical activity and the complexity of the cognitive exercises as barriers [71]. Additionally, those who did not participate in the intervention (controls) reported low digital literacy and lack of support from others as barriers. They also cited lack of motivation, lack of time, low digital literacy, limited knowledge of how to use social media, and poor internet connection, as reasons for not engaging in telehealth [71].
Recognizing the various benefits, facilitators, and barriers that telehealth presented for OP during the COVID-19 pandemic—summarized in Table 2—will be essential when designing and implementing future interventions.

Table 2.
Summary of telehealth benefits, facilitators, and barriers among older people during the COVID-19 pandemic: Global and Latin America and Caribbean perspectives.
4. Discussion
4.1. Lessons Learned and Considerations to Improve the Implementation of Telehealth and Reduce Barriers for Older People
Recent studies have identified a trend and preference among OP and professionals for using telehealth in combination with in-person interventions, rather than relying solely on telehealth [23,71,74,76,94,96]. This includes starting with initial in-person appointments, followed by telehealth and/or additional in-person visits [75].
In general, the three principles for delivering telehealth to OP proposed by The Collaborative for Telehealth and Aging (C4TA) from the United States—a group composed of providers, geriatric experts, telehealth specialists, and advocates—can be followed [98]. First, care must be person-centered; therefore, telehealth programs should be designed to meet the needs and preferences of OP by considering their goals, family and caregivers, language characteristics, and their readiness and ability to use technology [98]. Second, care must be equitable and accessible; thus, telehealth programs should address both individual and systemic barriers to care for OP by taking into account issues of equity and access [98]. Third, care must be integrated and coordinated across systems and individuals [98]. In addition, we present more specific considerations below to reduce telehealth barriers for OP. These recommendations are presented for application in various countries worldwide, including those in Latin America and the Caribbean, based on the findings identified in this literature review.
4.1.1. Intrinsic and Extrinsic Factors
A review of OP’s perceptions of technology showed that a one-size-fits-all approach does not work, and that technologies must be adapted to individual needs [99]. It should also not be assumed that all OP face difficulties accessing virtual care. [88]. Therefore, it is important to identify OP’s perceptions of ICTs in order to encourage their use, considering intrinsic factors, such as control-oriented attitudes, independence, and the need or requirement for safety; and extrinsic factors, such as usability, feedback, and costs [99].
Active listening should be encouraged, as well as discussing both the advantages and disadvantages of telehealth, considering existing recommendations in these areas [23]. It is important to emphasize the positive benefits that promote autonomy [99], adapt to OP’s lifestyles and expectations, and offer personalized interventions that take into account individual preferences and capabilities [5]. Also, the option to choose between a phone or videoconference assessment should be offered [88], all with the aim of preventing rejection or dropout. Therefore, technologies must be perceived as reliable and effective, if long-term use is to be achieved [99].
4.1.2. Digital Health Literacy
It has been reported that older age, low educational level, low income, depressive symptoms, low cognitive functioning, disability, limited support networks, complex application interfaces, and lack of digital health literacy are negatively associated with the use of telehealth [32,57,100,101,102,103,104]. It is important to note that when introducing new ICTs, the steep learning curve that OP may experience should be acknowledged, and support should be provided to help them become familiar with these technologies [5]. In addition, they may feel less comfortable, lack access to the necessary technology, and/or have sensory difficulties (such as impaired hearing or vision), which can hinder their use of telehealth [65]. Likewise, the “digital divide” resulting from socioeconomic status, age, geographic location, and cultural factors should also be taken into account [5].
In terms of Assessment, this could be achieved through the use of in-person or online surveys, as previously reported [73], to identify OP’s readiness for telehealth. This includes internet use, access to internet-connected devices, experiences and concerns related to this mode of intervention, and perceived barriers—ultimately enabling the development of training programs [73].
In terms of Training, a commonly expressed need among OP has been for professionals to provide educational sessions, workshops, and tutorials on how to use remote care [94]. In this regard, a meta-analysis—where the majority of studies included were from the United States—which aimed at evaluating the effectiveness of digital health literacy interventions for OP, found that these interventions led to significant improvements in OP’s knowledge and self-efficacy [105]. Additionally, it has been reported that in-person teaching, guided by a conceptual framework and delivered over a minimum of four weeks, had a more significant effect [105]. This approach also helps to strengthen relationships and bonds, which later foster trust when using telehealth [88].
In addition, programs aimed at increasing digital health literacy and competencies should include physicians, professionals, and OP, as this is essential to ensure that all parties have the knowledge, confidence, and ability to equitably benefit from emerging innovations, such as telehealth [33]. To this end, experiences such as the one implemented in Chile—where an online course on healthy aging was offered to both the community and healthcare professionals [84]—can be followed, as well as other international initiatives, such as volunteer programs involving university students that increased access to telehealth services for OP during the pandemic [106]. Likewise, training and capacity building for the personnel who will deliver telehealth should be encouraged, provided by clinical professionals with experience in telehealth, along with updates on new digital assessment tools [75].
In terms of Intervention, it is recommended that professionals use a coaching model for OP, which increases OP’s sense of responsibility in each session and enhances relationship-centered communication skills [9]. At the same time, review techniques should be used to ensure that OP adequately understand instructions and training. It is also important to listen to both the content and the emotions expressed by OP [9].
In addition, a series of actions should be considered with the OP, their family member and/or caregiver before a telehealth appointment, that include: explaining the format and purpose of the visit, practicing with providers beforehand, reminding the OP and their support network when and how the call will take place, explaining the need for future in-person consultations, obtaining photo documentation and/or encouraging family participation—all with the aim of ensuring better preparation for subsequent telehealth sessions [75]. This presents a challenge for OP, as it increases their responsibility to report on their health status and to engage in self-examination [9]. During the telehealth appointment, it is recommended to ask the OP to repeat the information and review it again at the end of the session or to write it down, provide opportunities to ask questions during the visit, look at the camera and be more expressive to ensure the message is understood—including careful placement of the microphone to avoid blocking the mouth. If multiple people are present, it is helpful to practice participation and decide in advance who will lead the conversation. All of this aims to improve communication [75].
4.1.3. Support, Adaptations, and Complements
OP should be supported in navigating the telehealth platform as needed, and assistance should be provided to promote self-efficacy and self-management. [23]. Social support and the involvement of a caregiver or family member during telehealth increase the likelihood of use [107] and facilitate the use of technology (e.g., Zoom). During the assessment, their participation can also be helpful for obtaining collateral information and may aid in remembering appointments [88], which becomes even more relevant for OP with disabilities [103].
A commonly expressed need among OP has been to simplify telehealth infrastructure [94]. It has also been reported that when enablers are present (having a cellphone/PC/tablet, knowing how to use them, and having internet access), these factors cease to be barriers [32]. Therefore, regarding telehealth and data use, it is recommended to use lower bandwidth if the platform allows it, provide a tablet and data loan service, use high-quality headsets/microphones that do not cover the mouth [75], use adequately functioning audio and video equipment (including adaptive devices such as pocket speakers) [88], and include a chat feature during the video call [23], all of which can facilitate telehealth.
Specifically for OP in rural areas or with disabilities, telehealth interventions can be adapted with a health promotion focus, drawing on international experiences in which context was adjusted (shorter, smaller, and longer-duration activities) and equity was addressed (e.g., phone formats, automatically generated subtitles) without altering the content [108]. Specifically, and based on the authors’ experience, we present a series of recommendations to consider when implementing telehealth with OP with disabilities, in order to reduce barriers and, as a result, improve access, use, and satisfaction with telehealth in this population group (Table 3). These recommendations can help make telehealth equitable and accessible, as well as integrated and coordinated across systems and individuals [98].

Table 3.
Recommendations and strategies for implementing telehealth for older people with disabilities, aimed at reducing telehealth barriers.
It has even been suggested that in cases where telehealth cannot be implemented at all, support for OP should be provided via telephone or social media. Periodic home visits may also be carried out, delivering infographics, guidelines, and/or manuals for use and later feedback [52], following the example of rural schools where due to geographic inaccessibility, this is a common practice to facilitate interventions. In this context, it was found that using a manual as the sole intervention tool is less effective compared to videos or a combination of both (video plus manual) [71], due to a social presence effect.
A strategy that could improve manual delivery and follow-up/support was drawn from a telehealth study during the pandemic, where the manual included a calendar with scheduled dates that OP were instructed to mark [13]. In this way, the number of sessions completed was self-reported during biweekly phone calls, incorporating motivational, psychological, and practical elements, along with goal-setting and an emphasis on independence—allowing OP to choose the physical activity of their preference. This approach enhanced adherence and empowerment [13], enabling positive relationships between users and professionals, addressing questions, monitoring health and intervention progress, and fostering self-efficacy in OP.
4.1.4. Conceptual Framework for the Implementation and Presentation of Research Related to Telehealth for Older People
Implementation science encompasses a broad range of applicable methodologies to improve the dissemination, implementation, and scalability of effective interventions in behavioral, clinical, healthcare, public health, global health, and educational settings, with the aim of improving the quality of care and health outcomes, while taking into account local realities, and ensuring sustainable implementation at scale [109]. This could be an interesting conceptual framework for the implementation of telehealth in different population groups, and specifically among OP. Unlike most publication guidelines, which apply to a specific research methodology, the Standard for Reporting Implementation Studies (StaRI) and its accompanying checklist cover the wide range of study designs used in implementation research [110]; therefore, this checklist can guide and facilitate the reporting of interventions and research related to the implementation of telehealth for OP. Furthermore, when designing and implementing these interventions, researchers should consider the barriers and facilitators identified in this literature review. The need for a comprehensive description of the context, implementation strategies, and interventions, as well as the presentation of various effectiveness, process, and cost-effectiveness outcomes, poses a challenge for journals with strict word limits for research articles and may require innovative solutions and the use of online Supplementary Materials [110], as well as for researchers themselves.
4.2. Challenges for Telehealth for Older People in Latin America and the Caribbean
4.2.1. Considerations from a Perspective of Future Pandemics
It is essential that responses to this past crisis (and to similar ones in the future) identify and prioritize OP, who may be at particular risk of being left behind or excluded during the pandemic response and subsequent recovery phases [14]. This is especially important in less developed countries, which are less likely to have access to ICTs and where needs are even greater [14], as may be the case in countries in the region.
As a result, it is necessary to ensure that community-based services and support for OP are maintained despite future physical distancing measures [14]. This presents a challenge for professional teams in social and health programs—at the institutional level (hospitals, long-term care facilities), in primary healthcare, and in the community—who have traditionally worked in face-to-face modalities, and who faced both the need and the opportunity to shift to telehealth in order to ensure continuity of care during the pandemic. In this sense, telehealth for OP should become a regular component of clinical practice for professionals in Gerontology and Geriatrics. Therefore, professional teams should always design and implement their in-person interventions with the awareness that, in situations like a pandemic, they may need to rapidly transition—within days—to a telehealth model to continue providing care.
It has been reported that, during quarantine periods, preventive telehealth strategies focused on cognitive, behavioral, social, positive, and brief interventions—delivered either online or in person—can improve mental well-being, social affiliation, and support, and reduce perceived loneliness [6]. On the other hand, cognitive skills and social support networks can help OP foster meaningful connection and a sense of belonging, improving social connection and promoting healthy relationships with oneself and others [6]. The minimum components that an intervention should include to protect the psychological and mental health of OP during a pandemic are: developing problem- and emotion-focused coping strategies; strengthening social skills and family relationships; and engaging in regular physical activity [111]. In addition, religion and spirituality have been strongly associated with positive psychological well-being, as they provide support, a sense of belonging, life purpose, and helping alleviate distress in the face of adversity [13]; this will be interesting to investigate and include as part of Telesalud’s interventions with OP of the Latin American and Caribbean region, where there is a high Christian and Catholic proportion.
4.2.2. Considerations from a Management Perspective: Design, Implementation, and Evaluation
In addition, investment is needed in care and support services to ensure that they are adapted to the individual needs of OP, advancing in the design, implementation, and management of cost-effective telehealth interventions that prioritize low cost and take into account the diversity and specific needs of OP [15]. These services should be designed to be accessible and aligned with the changes associated with normal aging, considering and differentiating by sex, age, educational level, functional status, cognitive status, digital literacy, context, among other factors. This approach promotes well-being, helps maintain autonomy and independence [14], and improves quality of life. Furthermore, interventions should include OP and their families in the design, user testing, and standardization of telehealth services.
At the same time, it is necessary to support OP and their caregivers so they can access digital communication or alternative ways to stay in contact with their families and social networks, when physical movement is restricted [14]. For this reason, it is also recommended to include OP and their caregivers in learning programs, as well as to regularly improve their access to ICTs [14]. It is both a challenge and a responsibility for professionals to conduct digital health literacy workshops, thereby fostering better performance of the telehealth strategies implemented.
It would also be essential to design, translate, adapt, and/or validate tools that assess motivation, competence, usability, and/or user satisfaction with mobile devices and telehealth, given that very few tools currently exist [112] and there are still challenges and opportunities in identifying valid tools for the OP population [113], —especially in Spanish or Portuguese in the region—following some early-stage experiences in certain countries [77,97]. These tools could complement those used in the Comprehensive Gerontological Assessment (CGA) [45,114], which is the cornerstone of evaluation in this field, thereby facilitating professional training. Furthermore, there is an opportunity to digitize many scales, questionnaires, or clinical tests routinely used in CGA—either through apps or video consultations—as has already been done with cognitive assessment tools in Chile and other countries [38,82,115,116]. Questionnaires or written materials may even be provided to OP before virtual visits to improve the quality of the evaluation [88]. This entire set of tools could be used to assess telehealth in OP and their caregivers, as part of the CGA, as previously recommended [45].
4.2.3. Considerations from a Research Perspective
In parallel, it is necessary to advance qualitative, quantitative, and mixed-methods research with an interdisciplinary focus involving OP, recognizing the specificities and strengths of the region. This will help explore in greater depth how telehealth was implemented during the COVID-19 pandemic from the perspectives of physicians, professionals (in their diversity), and OP themselves, using methodological strategies already employed—such as online surveys, due to their feasibility and reach [117]. It will also be highly relevant to investigate the benefits, facilitators, and barriers—such as those documented in this article (Table 2)—as experienced by both OP and healthcare providers, as well as the effects of different telehealth modalities (synchronous, asynchronous, or hybrid) on the biopsychosocial health and quality of life of OP, considering previous research, which showed that older people were more likely to recover from negative emotions, improve their well-being, and enhance their quality of life during the COVID-19 pandemic through telehealth services [118].
4.2.4. Considerations from an Academic Training Perspective
The fact that healthcare providers themselves may possess greater knowledge about managing telehealth with OP—following a gerontological and geriatric care model, alongside other intervention modalities—will enable them to develop more appropriate interventions with OP, their families, and caregivers, from a more ethical perspective and with a focus on promoting their rights. Likewise, this new knowledge needs to be incorporated into the training and curriculum of undergraduate and postgraduate students/professionals, as well as into continuing education programs for professionals who work or will work in the health and psychosocial fields with OP.
4.2.5. Considerations from a Healthcare System and Public Policy Perspective
Finally, some countries of the region already incorporate the telehealth as part of the strategies from their health ministries, such as Argentina, Brazil, Chile and Colombia [41]. Also telehealth guidelines in OP emanating from non-governmental organizations such as the Brazilian Society of Gerontology and Geriatrics [56], which can be replicated in other geriatric societies or professional associations in the region, with a focus on OP. These and other countries in the region must demonstrate the viability, scalability, profitability, availability and sustainability throughout the health system, of the telehealth with emphasis on gerontology and geriatrics. Therefore, having greater knowledge of telehealth in gerontology and geriatrics in Latin America and the Caribbean region will generate lessons learned and experiences that can be used to improve public policies, regulations, and health systems in countries where implementation barriers still persist [41], in light of other international experiences [119].
One of the limitations of our literature review is that the methodological quality of the scientific articles was not assessed, given the diversity of designs included in this literature review. However, its strengths include an updated concept of TeleGerontology and TeleGeriatrics; a broad and exhaustive review of the global and regional literature on the implementation, barriers, and facilitators of telehealth for OP during the COVID-19 pandemic; lessons learned and considerations for improving telehealth implementation and reducing barriers for OP, both globally and regionally; and the challenges for telehealth for OP in Latin America and the Caribbean (as a present and future opportunity) in aspects related to future pandemics, management (design, implementation, and evaluation), research, academic training, and the healthcare system and public policies.
5. Conclusions
During the COVID-19 pandemic, the effectiveness of telehealth was demonstrated, as it provided continuity and access to gerontological and geriatric care services, while reducing the risk of infection among OP by minimizing the need to visit healthcare facilities. Telehealth, thus, became a new modality of intervention with OP and their support networks, accelerating its adoption by several decades.
As a result, the pandemic was an opportunity to evaluate the current systems for delivering social and healthcare services, both for the general population and for OP. This highlights the importance of assessing, designing, and implementing strategies in a telehealth modality, considering all levels of healthcare, in order to ensure the continuity of regular interventions.
The increase in population aging is one of the major challenges in the coming decades, and one in which the needs and requirements among demographic cohorts will vary considerably, in light of individuals’ life course. In this context, the documented benefits of telehealth support its role as a fundamental and routine component of gerontological and geriatric care, particularly for reaching OP who face barriers to accessing healthcare services, including those in rural and remote areas. Similarly, telehealth is an excellent alternative for ensuring continuity of specialized care in situations involving physical isolation (e.g., pandemics, natural disasters, disability, and critical care), which restrict the social and healthcare participation of those affected. In fact, during the early months of the pandemic, telehealth served as a care alternative for OP with various health conditions. A proactive approach to identifying and addressing telehealth barriers can help maximize virtual interactions for the older population and mitigate healthcare inequities.
In the future, it will be necessary to gather local experiences accumulated during the pandemic, as well as to advance research, university education, professional training, and the development of guidelines, regulations, and public policies on telehealth in the fields of gerontology and geriatrics, reflecting the specific needs and context of the region.
Finally, the recommendations emerging from this review are highly relevant for healthcare professionals who work directly with older people, as well as for decision-makers, in guiding effective intervention strategies for the implementation of healthcare services for individuals with limited access to specialized care. Telehealth should help reduce fragmentation, improve data sharing, enhance communication among stakeholders, and address the sustainability of interventions.
Author Contributions
Conceptualization, R.P.-M. and E.S.R.; methodology, R.P.-M., E.S.R. and G.R.-B.; resources, R.P.-M.; writing—original draft preparation, R.P.-M., E.S.R., H.A.B.-C., S.D.-A., S.P.-S., F.R.-W., P.A.W., S.M., V.T., S.A.-N., I.B.-C., V.C.-A., C.B., M.F.L., R.M., A.T., I.C., F.M. and G.R.-B.; writing—review and editing, R.P.-M., E.S.R., H.A.B.-C., S.D.-A., S.P.-S., F.R.-W., P.A.W., S.M., V.T., S.A.-N., I.B.-C., V.C.-A., C.B., M.F.L., R.M., A.T., I.C., F.M. and G.R.-B.; supervision, E.S.R.; project administration, R.P.-M.; funding acquisition, R.P.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the ANID Millennium Science Initiative Program (NCS2022_039).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
Search strategy.
Table A1.
Search strategy.
| Databases | Syntax Descriptors | Results |
|---|---|---|
| Pubmed | ((“older adult”[Title/Abstract] OR “older person”[Title/Abstract] OR “older people”[Title/Abstract] OR “old age”[Title/Abstract] OR aging[Title/Abstract] OR aged[Title/Abstract] OR elderly[Title/Abstract]) AND (telehealth[Title/Abstract] OR telemedicine[Title/Abstract] OR telerehabilitation[Title/Abstract]) AND (Covid*[Title/Abstract] OR Pandemic*[Title/Abstract] OR SARS-CoV-2[Title/Abstract] OR Coronavirus[Title/Abstract]) AND (implement*[Title/Abstract] OR facilitator*[Title/Abstract] OR barrier*[Title/Abstract])) Filters: English, Spanish | 313 |
| Scopus | (((“older adult” OR “older person” OR “older people” OR “old age” OR aging OR aged OR elderly) AND (telehealth OR telemedicine OR telerehabilitation) AND (covid* OR pandemic* OR sars-cov-2 OR coronavirus) AND (implement* OR facilitator* OR barrier*))) AND (LIMIT-TO (DOCTYPE, “ar”)) AND (LIMIT-TO (LANGUAGE, “English”) OR LIMIT-TO (LANGUAGE, “Spanish”)) | 1299 |
| Scielo | (ab:((older adult OR older person OR older people OR old age OR aging OR aged OR elderly) AND (telehealth OR telemedicine OR telerehabilitation))) Filtros aplicados: (Tipo de literatura: Artículo) | 19 |
| Total export | 1631 | |
| Total duplicates | 254 | |
| Total articles | 1377 | |
Date of the Exporting records 23 January 2025.

Table A2.
Inclusion and Exclusion Criteria.
Table A2.
Inclusion and Exclusion Criteria.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|

Table A3.
Description of the 46 scientific articles on the implementation, barriers, and facilitators of telehealth during the COVID-19 pandemic, included in the literature Review.
Table A3.
Description of the 46 scientific articles on the implementation, barriers, and facilitators of telehealth during the COVID-19 pandemic, included in the literature Review.
| N° | Title | Country | Year | Aim | Type of Research | Sample Size (n=) | Results |
|---|---|---|---|---|---|---|---|
| 1 | Perceived Facilitators and Barriers, From the Perspective of Users, of a Multicomponent Intervention in Older People Using an Asynchronous Telehealth Modality During the COVID-19 Pandemic: A Qualitative Research [71] | Chile | 2025 | Examine the facilitators and barriers, from the users’ perspective, of a promotional-preventive multicomponent intervention in older people using an asynchronous telehealth modality during the COVID-19 pandemic, as a continuation of the face-to-face intervention. | Qualitative. Intervention. In-depth semi-structured interviews | 26 OP | Six themes were identified: positive aspects of telehealth, telehealth facilitators, preference for face-to-face modality over telehealth modality, telehealth barriers, reasons for not performing telehealth, and coping strategies in the pandemic: specifically, as facilitators, participating in the company of others, having participated in the same intervention previously (face-to-face modality), good knowledge of digital literacy, self-motivation, commitment to the program, and the emergence of innate leaders, and as barriers, pain during physical activity, complexity of cognitive exercises included in cognitive stimulation, poor digital literacy, and not having support from others. |
| 2 | Satisfaction of healthcare workers and patients regarding telehealth service in a hospital in Peru [77] | Peru | 2022 | Evaluate the level of satisfaction of healthcare workers and patients with the telehealth service of the Hospital III Regional Honorio Delgado (HRHD), as well as the maturity level of the telehealth service implementation. | Quantitative. Cross-sectional survey | 129 (physicians and nonphysician professionals) 377 patients (44 OP) | Non-physician professionals’ satisfaction with the telehealth service was higher than that of physicians (72.5% vs. 18.3%). Of patients, 77.6% stated they were satisfied with the service. Regarding the maturity level, the HRHD telemedicine service had 32% of items in null status, 40.8% in started, 25.2% in advanced, and 2% in ready conditions. |
| 3 | Psychosocial telemonitoring and teleorientation for older adults in the Social Security (EsSalud) during the first six months of the COVID-19 pandemic in Peru [78] | Peru | 2022 | Describe the experience of implemented Psychosocial telemonitoring and teleorientation for elderly patients during COVID-19 pandemic. | Quantitative. Cross-sectional | 154,280 follow-ups and 36,492 remote care services were provided to OP | The main interventions provided were emotional support (75.5%) and social counseling (53.8%). The most recorded moods were calmness and worry. Feelings of worry, stress, sadness, and fear are higher in the reports with COVID-19 compared to those without COVID-19. |
| 4 | Understanding the Personal Barriers of Elderly Patients for Carrying out Teleconsultations During COVID-19 Pandemic: An Observational Study [79] | Brazil | 2024 | Describe the socioeconomic, clinical, and functional characteristics of elderly patients who were supported by a COVID-19 telehealth program. | Quantitative. Cross-sectional | 237 OP | Age greater than 80 years, lower educational level, hearing, and visual impairments were characteristics associated with the need for support for teleconsultations. The need for support was associated with hospitalization and mortality. |
| 5 | Providing geriatric oncology care using telemedicine for older patients with cancer during the COVID-19 pandemic in Mexico [80] | Mexico | 2023 | Describe experience using readily available telemedicine tools to deliver specialist multidisciplinary care to older adults with cancer at a Mexican medical center during the COVID-19 pandemic. | Quantitative. Intervention. Cross-sectional | 44 OP with cancer | Only 20% of patients had webcam-equipped computers, and 50% of visits were performed using a caregiver’s device. Seventy-five percent of visits took place using WhatsApp, and 23% using Zoom. The average visit lasted 23 min, with only 2% not completed due to technical issues. A geriatric assessment was successfully conducted in 81% of telemedicine visits, and chemotherapy was prescribed remotely in 32%. |
| 6 | Implementation of a Teledentistry Platform for Dental Emergencies for the Elderly in the Context of the COVID-19 Pandemic in Chile [81] | Chile | 2022 | Develop and implement a “semi-presential” technology platform to support urgent and priority dental care for the elderly in the context of the COVID-19 pandemic among the Chilean population. | Quantitative. Intervention. Cross-sectional | 135 OP | 53.3% required immediate or urgent treatment, and 24.4% were derived to specialists from whom 60.6% needed immediate or urgent treatment. 74.3% of teleconsultations were derived to an oral pathology specialist. |
| 7 | Clinical utility of Phototest via teleneuropsychology in Chilean rural older adults [82] | Chile | 2022 | Analyze the clinical utility of the Phototest, through telemedicine, to identify mild cognitive impairment in rural older adults with memory complaints, during the COVID-19 pandemic. | Quantitative. Cross-sectional Case–control | 111 (rural OP with mild cognitive impairment) 130 (healthy controls) | To identify mild cognitive impairment, using a cutoff score of 27–28 points, the Phototest showed a sensitivity of 96.6% and a specificity of 81.8%; indicators superior to those of the MMSEm. |
| 8 | Providing Supportive and Palliative Care Using Telemedicine for Patients with Advanced Cancer During the COVID-19 Pandemic in Mexico [83] | Mexico | 2021 | Describe how transformed a multidisciplinary supportive and palliative care program into a telemedicine intervention for patients with advanced cancer during the COVID-19 pandemic. | Quantitative. Intervention. Cross-sectional | 45 patients with Advanced Cancer (Median age was 68 years) | The most common interventions were psychological care (33%), pain and symptom control (25%), and nutritional counseling (13%). Half of the interventions were provided by video conferencing. The most common patient-reported barrier was limited experience using communication technology. |
| 9 | Implementation of a virtual telehealth course for Chilean older adults and health students [84] | Chile | 2023 | Assess the perception and impact of an online course about healthy aging aimed at the community and healthcare professionals. | Quantitative. Intervention. Cross-sectional survey | 386 attendants (20,46% OP) | All respondents acquired new knowledge and were willing to participate again. The frequency of interest about self-care is three times greater than about caring for another person, In an older person, the interest is 101 more times about self-care than caring for another person. Ninety five percent of respondents felt more active and 84% felt more accompanied. |
| 10 | Playing remotely in times of crisis: A program to overcome social isolation [85] | Brazil | 2022 | Examine the feasibility of an intergenerational remote intervention program designed to promote the well-being and social connection of vulnerable older adults, mainly people with aphasia and dementia during the COVID-19 pandemic in the south of Brazil. | Mixed-method. Quantitative (Cross-sectional) Qualitative (participative observation) | 34 OP with stroke-induced cognitive impairments, dementia and individuals without any neurological conditions | The initial period of the program achieved 83.7% of adherence and sustainability for additional 3 months. Preliminary results suggest feasibility and acceptability, considering formal and informal support in digital inclusion. Participatory observations describe that the structure of sessions and activities were well received. The analysis of participants’ perceptions detects the thematic saliency of feelings of social connection and a sense of having learned with the group. |
| 11 | Experience in the use of videos for the promotion of physical exercise at home in online mode in older adults in Chile during the COVID-19 pandemic [97] | Chile | 2022 | Describe the usability, actionability and understanding of videos to promote exercise at home online during the COVID-19 pandemic, analyzing the characteristics of the population, their satisfaction, adherence and barriers to physical exercise. | Quantitative. Intervention. Cross-sectional survey | 34 OP | The videos as understandable and actionable. Usability was lower in people who perceived a lower level of technological management. Average adherence was 2 days a week for 2.5 weeks. The main perceived barrier was the lack of will, which showed a greater tendency in people who performed physical exercise in a group way before the restrictions due to the COVID-19 pandemic. |
| 12 | Telemedicine in primary care of older adults: a qualitative study [23] | Canada | 2024 | Identify potential facilitators and barriers to telemedicine use in primary care for older adults and develop recommendations accordingly. | Qualitative. Semi-structured interviews and focus groups | 29 OP 15 Healthcare professionals (family physicians, nurses, social workers, and physiotherapists) | Telemedicine contributed to maintaining the continuity of care and was particularly convenient when there was an existing or established patient-physician relationship or for addressing minor health issues. Telemedicine was found to be beneficial for people with limited mobility, reducing their exposure to potentially high-risk environments. However, participants expressed concerns about the lack of visual contact, causing essential details to be overlooked. Additionally, issues related to miscommunication due to language or hearing barriers were identified. Healthcare professionals perceived that most older adults did not consider phone consultations a medical act. Participants were open to a hybrid approach, combining in-person consultations and telemedicine, based on their specific health conditions. |
| 13 | The Effect of a Tele-Health Intervention Program on Home-Dwelling Persons with Dementia or MCI and on Their Primary Caregivers during the Stay-at-Home-Order Period in the COVID-19 Pandemic Outbreak: Evidence from Taiwan [26] | Taiwan | 2022 | The results could serve as an important reference for policymakers to evaluate whether the Tele-Health intervention program is an appropriate policy instrument for delivering various supportive care services to persons with dementia or mild cognitive impairment and their primary caregivers. | Quantitative. Intervention Case–control | 8 OP dementia and mild cognitive impairment (Case) 8 OP dementia and mild cognitive impairment (control group) | The Telehealth intervention program significantly increased the well-being of the participants and their primary caregivers, but the negative correlations between the Tele-Health intervention program and family functioning were also found to be significant. |
| 14 | Telehealth Use Among Older Adults During COVID-19: Associations With Sociodemographic and Health Characteristics, Technology Device Ownership, and Technology Learning [32] | USA | 2022 | Examine rates and correlates of telehealth (video call) use among those aged 70+, and tested the significance of access to information and communication technology device ownership and knowledge of how to use the internet and devices as telehealth-enabling factors. | Quantitative. Cross-sectional survey | 3257 OP | Telehealth use increased to 21.1% from 4.6% pre-pandemic. In logistic regression models without technology-enabling factors, older age and lower income were negatively associated with telehealth use; however, when technology-enabling factors were included, they were significant while age and income were no longer significant. Insuring that older adults have ICT devices and internet access may reduce health disparities and improve telehealth care delivery. |
| 15 | Geriatric care physicians’ perspectives on providing virtual care: a reflexive thematic synthesis of their online survey responses from Ontario, Canada [34] | Canada | 2024 | Understand the perspectives of geriatric care providers on using telemedicine with older adults through telephone, videoconferencing and eConsults. | Qualitative. Cross-sectional survey (thematic analysis) | 29 Geriatric care physicians | Identified difficulty using technology, patient sensory impairment, lack of hospital support and pre-existing high patient volumes as barriers against using telemedicine, whereas the presence of a caregiver and administrative support were facilitators. Perceived benefits of telemedicine included improved time efficiency, reduced travel, and provision of visual information through videoconferencing. Ultimately, participants felt telemedicine served various purposes in geriatric care, including improving accessibility of care, providing follow-up and obtaining collateral history. Main limitations are the absence of, or incomplete physical exams and cognitive testing. |
| 16 | Digital literacy as a potential barrier to implementation of cardiology tele-visits after COVID-19 pandemic: the INFO-COVID survey [57] | Italy | 2023 | Evaluate digital literacy among cardiology outpatients. | Quantitative. Cross-sectional survey | 1067 OP | For internet access, there was a splitting between “never” (42.1%) and “every day” (41.0%). In the total population, the most used devices for internet access were smartphones (59.0%), and WhatsApp represented the most used app (57.3%). Internet users were younger compared to non-internet users (63 vs. 78 years old, respectively) and with a higher educational level. Age and educational level were associated with non-use of internet. |
| 17 | Technology Learning and the Adoption of Telehealth Among Community-Dwelling Older Adults During the COVID-19 Outbreak [59] | USA | 2022 | Examine changes in the prevalence of telehealth utilization in older adults before and during the COVID-19 outbreak, and to investigate the relationship between learning a new technology and the adoption of telehealth during the outbreak. | Quantitative. Cross-sectional survey | 1769 OP | The older adults substantially increased the utilization of telehealth during the outbreak. Additionally, learning a new technology is related to the adoption of both emails and video calls to access telehealth. The findings suggest that older adults may be motivated and able to quickly learn a new technology that is required to access telehealth during the COVID-19 outbreak. |
| 18 | Exploring Factors Enhancing Resilience Among Marginalized Older Adults During the COVID-19 Pandemic [60] | USA | 2022 | Explore daily activities of marginalized older adults and how they coped with various challenges during the COVID-19 pandemic when there was state-wide quarantine enforcement. | Qualitative. In-depth semi-structured interviews | 18 OP | COVID-19 influenced not only the physical health but also the mental health of older adults. However, they overcame adversity by using technology to continue daily activities, exchanging informal support with family and neighbors, relying on formal support from community organizations, and keeping themselves physically active in their neighborhoods. |
| 19 | Perspectives on Telehealth for older adults during the COVID-19 pandemic using the quadruple aim: interviews with 48 physicians [61] | USA | 2022 | Understand experiences of frontline physicians caring for older adults via telehealth during the COVID-19 pandemic. | Qualitative. Semi-structured interviews | 18 Geriatricians 15 Primary care physicians 15 Emergency physicians | Frontline physicians described telehealth as a more flexible, value-based, and patient-centered mode of healthcare delivery. Benefits of using telehealth to treat older adults included reducing deferred care and increasing timely care, improving efficiency for physicians, enhancing communication with caregivers and patients, reducing patient travel burdens, and facilitating health outreach and education. Challenges included unequal access for rural, older, or cognitively impaired patients. Physicians noted that payment parity with in-person visits, between video and telephone visits, and relaxation of restrictive regulations would enhance their ability to continue to offer telehealth. |
| 20 | Barriers to telehealth access among homebound older adults [62] | USA | 2021 | Identify major barriers to video-based telehealth use among homebound older adults. | Quantitative. Cross-sectional survey | 16 physicians | More than one-third (35%) of homebound patients (mean age of 82.7; 46.6% with dementia; mean of 4 comorbidities/patient) engaged in first-time video-based telehealth encounters between April and June 2020 during the first COVID-19. The majority (82%) required assistance from a family member and/or paid caregiver to complete the visit. Among patients who had not used telehealth, providers deemed 27% “unable to interact over video” for reasons including cognitive or sensory impairment and 14% lacked access to a caregiver to assist them with technology. Physicians were not knowledgeable of their patients’ internet connectivity, ability to pay for cellular plans, or video-capable device access. |
| 21 | “There Is Something Very Personal About Seeing Someone’s Face”: Provider Perceptions of Video Visits in Home-Based Primary Care During COVID-19 [63] | USA | 2021 | Examine provider perceptions of video visits during the first wave of the COVID-19 crisis in New York City. | Qualitative. Semi-structured interviews | 6 Medical/clinical director 3 Nurse/nursing coordinator 3 Social worker/social work coordinator 1 Program manager | Providers reported a combination of commercial (health system-supported) and consumer (e.g., FaceTime) technological platforms was essential. Video visit benefits included triaging patient needs, collecting patient information, and increasing scheduling capacity. Barriers included cognitive and sensory abilities, technology access, reliance on caregivers and aides, addressing sensitive topics, and incomplete exams. |
| 22 | Telehealth for the cognitively impaired older adult and their caregivers: lessons from a coordinated approach [65] | USA | 2022 | Describe the ‘Coordinated Care At Risk/Remote Elderly’ program (CCARRE) to demonstrate a unique approach to reaching culturally diverse and vulnerable population using telehealth, and share some of the lessons learned as a result of early difficulties faced. | Quantitative. Intervention. Cross-sectional | 85 OP with cognitive complaints | Recognized unique factors that could improve patient care, lessen burden and optimize access to community resources. Lessons learned from the experience are shared: the televisit approach; start on the phone & move to video; use the video visit to conduct a ‘real-time’ safety evaluation; the ‘virus’ approach; address advance care planning & goals of care; address caregiver stress & caregiver needs, including providing behavioral management techniques; address daily activities—cognitively, socially & physically. appropriate things patients can/should be doing; the multidisciplinary approach; address social determinants of health; consider cultural/racial factors & language barriers; and link with local community-based organizations to establish seamless connections. |
| 23 | Telemedicine Care of Dementia Patients During the COVID-19 Pandemic [67] | Germany | 2023 | Evaluate the potential use of telemedicine in older people with incipient cognitive deficits in the context of dementia. | Quantitative. Intervention. Cross-sectional survey | 90 OP at risk of developing dementia or with dementia disease | More than 80% of the physicians and neuropsychologists rated the technical process of video consultations as good/very good. A general assessment of the cognitive deficits by physicians and neuropsychologists correlated extremely highly with the results of the subsequent specific testing (MMST and ACE) in F2F and video consultations. Overall, could not find any significant differences in patients’ satisfaction between video consultations and classical face-to-face contact presentation. |
| 24 | Strategies to Ensure Continuity of Care Using Telemedicine with Older Adults during COVID-19: A Qualitative Study of Physicians in Primary Care and Geriatrics [69] | USA | 2022 | Understand the experiences using telemedicine during the COVID-19 pandemic to examine strategies used to maintain continuity of care with their patients, ages 65 and older. | Qualitative. Semi-structured interviews | 18 geriatricians 15 Primary care physicians | Many physicians successfully bridged the digital divide by: assessing patients’ technological readiness in advance, being flexible with telehealth modes, using available home or facility-based staff, educating patients on telehealth privacy and usefulness, making accommodations for disabilities, and involving caregivers. |
| 25 | Development and implementation of an interdisciplinary telemedicine clinic for older patients with cancer-Preliminary data [70] | USA | 2023 | Develop the Cancer and Aging Interdisciplinary Team (CAIT) clinic model to provide timely GA and treatment recommendations independent of patient’s physical location. | Quantitative. Intervention. Cross-sectional | 50 OP with cancer | 68% were 80 years of age or older (range 67–99). All the evaluations were hybrid. The median days between receiving a referral and having the appointment was 8. GA detected multiple unidentified impairments. About half of the patients (52%) went on to receive chemotherapy (24% standard dose, 28% with dose modifications). The rest received radiation (20%), immune (12%) or hormonal (4%) therapies, 2% underwent surgery, 2% chose alternative medicine, 8% were placed under observation, and 6% enrolled in hospice care. Feedback was extremely positive. |
| 26 | COVID-19 transforms health care through telemedicine: Evidence from the field [72] | USA | 2020 | Provide data on the feasibility and impact of video-enabled telemedicine use among patients and providers and its impact on urgent and nonurgent healthcare delivery from one large health system (NYU Langone Health) at the epicenter of the COVID-19 outbreak in the United States. | Quantitative. Cross-sectional | 1336 telemedicine visits | Between March 2nd and April 14th 2020, telemedicine visits increased from 102.4 daily to 801.6 daily (683% increase) in urgent care after the system-wide expansion of virtual urgent care staff in response to COVID-19. Of all virtual visits post expansion, 56.2% and 17.6% urgent and nonurgent visits, respectively, were COVID-19-related. Telemedicine usage in urgent care (21.7%, in 55 and over) and non-urgent care (40.9%, in 55 and over). |
| 27 | Telemedicine Preparedness Among Older Adults With Chronic Illness: Survey of Primary Care Patients [73] | USA | 2022 | About their telemedicine preparedness, including internet usage, internet-capable devices, telemedicine experiences and concerns, and perceived barriers. | Quantitative. Cross-sectional survey | 30 OP with chronic illness | Most participants (70%) reported having a device that could be used for telemedicine and using the internet. However, about half had only a single connected device, and messaging and video calling were the most commonly used applications. Few used email and none used online shopping or banking. Nearly all respondents recognized avoiding travel and COVID-19 exposure as telemedicine benefits. The most common concerns were loss of the doctor-patient connection and inability to be examined. |
| 28 | The Impact of COVID-19 on Older Adults’ Perceptions of Virtual Care: Qualitative Study [74] | Canada | 2022 | Understand older adults’ perspectives and experiences of virtual care during the pandemic. | Qualitative. Semi-structured interviews | 20 OP | Participants were generally satisfied with the virtual care they received during the pandemic. Participants described the benefits of virtual care (e.g., increased convenience, efficiency, and safety), the limitations of virtual care (e.g., need for physical examination and touch, lack of nonverbal communication, difficulties using technology, and systemic barriers in access), and their perspectives on the future of virtual care. Half of our participants preferred a return to in-person care after the COVID-19 pandemic, while the other half preferred a combination of in-person and virtual services. Many participants who preferred to access in-person services were not opposed to virtual care options, as needed; however, they wanted virtual care as an option alongside in-person care. Participants emphasized a need for training and support to be meaningfully implemented to support both older adults and providers in using virtual care. |
| 29 | Rapid implementation of telehealth in geriatric outpatient clinics due to COVID-19 [75] | Australia | 2021 | Evaluate the rapid implementation of telehealth in outpatient geriatric clinics at a tertiary public hospital in Victoria, in response to COVID-19. | Mixed-method. Quantitative (Cross-sectional survey) Qualitative (Semi-structured interviews) | 24 Geriatricians | Half of the appointments needed to be re-scheduled due to language barrier, poor connection, hard of hearing and inability to perform assessments. Advantages included time efficiency and ability to visualize the home. Preference for the future was initial appointments as face–face, but reviews as either telehealth or face–face. |
| 30 | Telehealth access and experiences of older adults with HIV during the COVID-19 pandemic: Lessons for the future [76] | USA | 2024 | Assess the telehealth capability and experiences of older people with HIV at an urban HIV clinic. | Mixed-method. Quantitative (Cross-sectional survey) Qualitative (Focus group) | 80 OP | One-third did not have internet access or an email address. A total of 65% had at least one telehealth-capable device but 12.5% of respondents with a device did not know how to use it. Themes were grouped into benefits (social/emotional connection and convenience) and challenges (technological barriers and missed in-person experience). |
| 31 | Understanding the Experience of Geriatric Care Professionals in Using Telemedicine to Care for Older Patients in Response to the COVID-19 Pandemic: Mixed Methods Study [87] | Canada | 2022 | Identify the benefits and challenges geriatric care professionals face when using telemedicine technologies with frail older patients, their caregivers, and their families and how to maximize the benefits of this method of providing care. | Mixed-method. Quantitative (Cross-sectional survey) Qualitative (Semi-structured interviews) | 22 geriatricians 5 geriatric psychiatrist 3 geriatric nurse practitioners | Analysis of interview data identified 5 using the Consolidated Framework for Implementation Research (CFIR) contextual barriers (complexity, design quality and packaging, patient needs and resources, readiness for implementation, and culture) and 13 CFIR contextual facilitators (relative advantage, adaptability, tension for change, available resources, access to knowledge, networks and communications, compatibility, knowledge and beliefs, self-efficacy, champions, external agents, executing, and reflecting and evaluating). |
| 32 | Barriers and facilitators to virtual care in a geriatric medicine clinic: a semi-structured interview study of patient, caregiver and healthcare provider perspectives [88] | Canada | 2022 | Describe barriers and facilitators experienced by people accessing and providing virtual care in a geriatric medicine clinic. | Qualitative. Semi-structured interviews | 7 healthcare providers 7 OP 7 caregivers | Identified eight themes: impact of the COVID-19 pandemic on virtual care uptake, complexity of virtually caring for older adults, uncertain accuracy of virtual assessments, inequity in access to virtual care, importance of caring for the patient-caregiver dyad, assimilating technology into the lives of older adults, impact of technology-related factors on virtual care uptake and impact of clinic processes on integration of virtual care into outpatient care. Further, identified knowledge, skills, belief in capabilities, and environmental context and resources as key barriers and facilitators to uptake. |
| 33 | Determining the Factors that Impede or Facilitate the Utilization of Telemedicine (Video Visits) for Geriatric Patients [91] | USA | 2022 | Evaluate the barriers and facilitators of telemedicine utilization experienced by geriatric patients at the University of Iowa Family Medicine Clinic and selected Senior Living Communities in Iowa City, to inform recommendations for improving the telemedicine delivery process for older adults. | Mixed-method. Quantitative (Cross-sectional survey) Qualitative (Semi-structured interviews) | 3 OP 4 caregivers 19 physicians 5 medical assistants 2 schedulers | Geriatric patients and their caregivers, as well as health and non-healthcare personnel experience barriers, including difficulty navigating technology, privacy concerns, and lack of technical support; and facilitators, such as customer service support and having protocols to guide patients on telemedicine use. |
| 34 | Enabling Rural Telehealth for Older Adults in Underserved Rural Communities: Focus Group Study [92] | New Zealand | 2022 | Investigate enablers for telehealth use in underserved rural populations to improve access to healthcare for rural older adults. | Qualitative. Focus group and Semi-structured interviews | 98 OP | Those who had used telehealth reported positive experiences (time and cost savings) and were likely to use telehealth again. A total of 2 main themes were identified through an equity lens. The first theme was trust, with 3 subthemes—trust in the telehealth technology, trust in the user (consumer and health provider), and trust in the health system. Having access to reliable and affordable internet connectivity and digital devices was a key enabler for telehealth use. Most rural areas had intermittent and unreliable internet connectivity. Another key enabler is easy access to user support. Trust in the health system focused on waiting times, lack of and/or delayed communication and coordination, and cost. The second theme was choice, with 3 subthemes—health service access, consultation type, and telehealth deployment. Access to health services through telehealth needs to be culturally appropriate and enable access to currently limited or absent services such as mental health and specialist services. Accessing specialist care through telehealth was extremely popular, although some participants preferred to be seen in person. A major enabler for telehealth was telehealth deployment by a fixed community hub or on a mobile bus, with support available, particularly when combined with non-health-related services such as internet banking. |
| 35 | Personalized Telehealth: Redesigning Complex Care Delivery for the 65+ During the COVID Pandemic: a Survey of Patients, Caregivers, and Health-care Providers [93] | USA | 2023 | Identify perceptions, barriers, and possible facilitators to telehealth use amongst elderly patients with comorbidities, their caregivers, and healthcare providers (HCPs). | Quantitative. Cross-sectional survey | 40 OP with multiple comorbidities 39 healthcare providers 22 Caregivers | Most patients (90%), caregivers (82%), and healthcare providers (97%) had experienced telephone visits, but few were conducted via videoconference platforms. Patients and caregivers showed interest in pursuing some future telehealth visits (68%, 86%, respectively), but felt they lacked access to technology and skills, and some felt that telehealth visits may be inferior to in-person visits. Health-care providers showed interest in incorporating telehealth visits into practice, but identified challenges in lack of administrative support, lack of Health-care providers and patient technological skills, and limited infrastructure/internet access. |
| 36 | Barriers and challenges to telemedicine usage among the elderly population in Israel in light of the COVID-19 era: A qualitative study [94] | Israel | 2024 | Investigate the challenges and barriers (if any) experienced by the elderly population when using telemedicine services in Israel. | Qualitative. Semi-structured inter-views | 14 OP | Most participants recognized the advantages of telehealth services, particularly for the elderly population during pandemics and normal times. Many participants were concerned that the quality of telemedicine sessions may not be good enough compared to in-person sessions, and expressed a lack of confidence in telemedicine services, and frustration from the absence of in-person interaction and communication. Many participants highlighted the technological challenges in the use of computers and applications in general and in the context of healthcare, in particular, in addition to physiological and literacy difficulties. Finally, the participants suggested several ways to increase the accessibility and usage of telemedicine solutions by elderly people. |
| 37 | Barriers to Telemedicine Video Visits for Older Adults in Independent Living Facilities: Mixed Methods Cross-sectional Needs Assessment [95] | USA | 2022 | Understand the barriers to telemedicine in community-dwelling older adults to improve the access to and experience of virtual visits. | Mixed-method. Quantitative (Cross-sectional survey) Qualitative (Semi-structured interviews) | 249 OP | Regarding video visits, 36.5% of all participants felt comfortable connecting with their healthcare team through video visits. Regarding top barriers, participants at site A reported not knowing how to connect to the platform, not being familiar with the technology, and having difficulty hearing, whereas for site B, the top barriers were not being able to speak English well, lack of familiarity with technology and the internet, and lack of interest in seeing providers outside of the clinic. Three key themes emerged from the follow-up interviews: the perceived limitations of video visits, the overwhelming process of learning the technology for telemedicine, and the desire for in-person or on-demand help with telemedicine. |
| 38 | Awareness and attitudes of elderly Southeast Asian adults towards telehealth during the COVID-19 pandemic: a qualitative study [96] | Singapore | 2025 | Understand the awareness and attitudes of elderly Southeast Asians towards telehealth services during the coronavirus disease 2019 (COVID-19) pandemic. | Qualitative. Semi-structured inter-views | 78 OP | Despite the advantages offered by telehealth services, participants preferred in-person consultations due to a perceived lack of human interaction and accuracy of diagnoses, poor digital literacy and a lack of access to telehealth-capable devices. |
| 39 | Persisting Barriers to the Adoption of Telemedicine in Latin America After the COVID-19 Pandemic [41] | Argentina, Brazil, Chile, Colombia, Mexico | 2023 | Gives a broad-strokes update on the development of telemedicine after the COVID pandemic in Chile, Brazil, Mexico and Colombia—the four countries that made the greatest strides in the field of telemedicine and telehealth in Latin America, identifying which barriers still persist to its full integration into the health system. | Literature Review | 12 documents were included | This gives a broad-strokes update on the development of telemedicine after the COVID pandemic in Chile, Brazil, Mexico and Colombia—the four countries that made the greatest strides in the field of telemedicine and telehealth in Latin America, identifying which barriers still persist to its full integration into the health system. |
| 40 | Implementation of telemedicine in the Americas: Barriers and facilitators [42] | Region of the Americas. | 2021 | To present an overview of the last twenty years of telemedicine, identifying its objectives, achievements, opportunities for improvement, lessons learned, and lessons learned during the COVID-19 pandemic. Academic aspects, public policy, regulations, hospital care, and knowledge networks from both the public and private sectors were covered, with a special emphasis on the Americas. | Literature Review | 21 documents were included | The past 20 years have seen an increase in the availability of resources and technical capacity, improvements in digital education, empowerment of patients regarding their treatment, and increased public interest in this area. Successes have included the use of interdisciplinary teams, academic and professional networking, and virtual medical consultations. After reviewing the state of telemedicine in the Region of the Americas, the authors recommend the urgent adoption of measures aimed at implementing national telemedicine policies and programs, including a regulatory framework and adequate funding. Implementation of the measures should be integrated and interoperable and include the support of academic networks and the collaboration of specialized institutions. The policies should generate an enabling context that ensures sustainability of the progress achieved, bearing in mind the possible barriers mentioned. |
| 41 | Telerehabilitation for Geriatrics [9] | Not specified | 2021 | This article reviews the scope, need, and implementation of telehealth and telerehabilitation in the aging population from the perspective of both clinicians, patients, and caregivers. | Literature Review | 82 articles were included | Telehealth use was accelerated by the coronavirus disease 2019 pandemic and became an essential part of the rehabilitation service. Telehealth has a great potential in alleviating social isolation as well as addressing the medical needs of older individuals. Challenges to effective and efficient implementation include willingness to adapt to the technology by older adults, reliable Internet connections, identifying the area where telehealth is most effective, and evaluating the patients and administrative outcomes of telehealth interventions. Telerehabilitation refers to rehabilitation services involving evaluation and treatment. It is an attractive option for older adults who may have multiple comorbidities. Limited access to in-person services and the concern about potential exposure to severe acute respiratory syndrome coronavirus-2 during this pandemic accelerated the implementation of telerehabilitation. |
| 42 | Asynchronous Telehealth [20] | Not specified | 2022 | Discuss the use of asynchronous telehealth in the form of e-visits and e-consults. | Literature Review | 28 articles were included | Asynchronous telehealth, which includes both e-visits and e-consults. The highest utility for e-visits is for lower acuity illness that does not require immediate evaluation and for which diagnosis does not require a physical examination. The potential benefits of asynchronous telehealth e-consultation between primary care and subspecialty care providers depend on the nature and framework of the local implementation, the breadth of available subspecialties, and the ability of the primary care physician to follow through on the recommendation provided by the subspecialist. Asynchronous virtual care is recognized for providing scale, value, and efficiency. Tracking volume, turnaround time, and quality variables involved in service delivery are critically important in ensuring patient satisfaction, programmatic success, and sustainability. |
| 43 | Telehealth Use in Geriatrics Care during the COVID-19 Pandemic-A Scoping Review and Evidence Synthesis [40] | USA, UK, Italy, Canada, Australia, France, Spain, Switzerland, Germany, Ireland, Israel, Japan, South Korea, Netherlands, New Zealand, Poland, Chile, Mexico, China, India | 2021 | Conducted a scoping review and evidence synthesis for telehealth use in geriatric care to summarize learning from these new data. | A Scoping Review and Evidence Synthesis | 79 articles were in-cluded | The articles provide some evidence of effective provision of preventive, curative, and rehabilitative telehealth services for older people, but they highlight a greater focus on curative services and are mostly concentrated in high-income countries. We identified convenience and affordability as the strengths of telehealth use in geriatric care. Weaknesses identified include the inability of telehealth to cater to the needs of older people with specific physical and cognitive limitations. While the threats of increasing inequity and the lack of standardization in the provision of age-friendly telehealth services remain, identified opportunities for technologic advancements driven by simplicity and user-friendliness for older people. |
| 44 | Application and implementation of telehealth services designed for the elderly population during the COVID-19 pandemic: A systematic review [66] | Singapore, Poland, Italy, Tunisia, Turkey, Netherlands, USA, Ireland | 2022 | Explore the availability, application, and implementation of telehealth services during the COVID-19 era, designed for the aged population (age 65 and more). | Systematic review | 11 articles were included | Among the telehealth services, there were services aimed for triage and control during the outbreak of the COVID-19 pandemic, remote monitoring and treatment, follow-ups online meetings for patients residing in health centers, and application of online services. |
| 45 | Telemedicine in the primary care of older adults: a systematic mixed studies review [86] | Ireland, USA, Spain, UK, Netherlands, Poland, Portugal, Switzerland, China, Sweden, New Zealand, Scotland | 2023 | Explore the effects of TM and the determinants of its use in primary care for older adults. | Systematic mixed studies review | 20 articles were included | They used either phone, videoconference or both. Among studies reporting positive outcomes in TM experience, ‘user habit or preferences’ was the most cited barrier and ‘location and travel time’ was the most cited facilitator. Only one study reported negative outcomes in TM experience and reported ‘comfort with patient communication’ and ‘user interface, intended use or usability’ as barriers, and ‘technology skills and knowledge’ and ‘location and travel time’ as facilitators. Among studies reporting positive outcomes in service use and usability, no barrier or facilitator was cited more than once. Only one study reported a positive outcome in health-related and behavioral outcomes |
| 46 | Facilitators and barriers to the adoption of telehealth in older adults: an integrative review [64] Comment: This scientific article is included because it provides a pre-pandemic comparison for the barriers and facilitators of telehealth in OP. | USA, UK, Germany, Netherlands, Austria, France, Denmark, Norway, Canada | 2014 | Identified the current telehealth technologies that are available to older adults with a discussion on the facilitators of and barriers to those technologies. | Integrative review | 14 articles were in-cluded | 50% of the studies did not specifically address facilitators of and barriers to adopting telehealth with older adults. Also, studies in this population did not address caregivers’ perceptions on the facilitators of and barriers to telehealth. |
References
- Huenchuan, S. Envejecimiento, Personas Mayores y Agenda 2030 Para el Desarrollo Sostenible: Perspectiva Regional y de Derechos Humanos; CEPAL: Santiago, Chile, 2018; pp. 1–259. Available online: https://repositorio.cepal.org/server/api/core/bitstreams/431e4d95-46d9-4de6-a0a6-d41b1cb7d0b9/content (accessed on 1 September 2025).
- Naciones Unidas. Se Acaba la Emergencia Por la Pandemia, Pero el COVID Continua. 2023. Available online: https://news.un.org/es/story/2023/05/1520732 (accessed on 1 September 2025).
- Pinazo, S. Psychosocial impact of COVID-19 on older people: Problems and challenges. Rev. Esp. Geriatr. Gerontol. 2020, 55, 249–252. [Google Scholar] [CrossRef]
- Roschel, H.; Artioli, G.; Gualano, B. Risk of Increased Physical Inactivity During COVID-19 Outbreak in Older People: A Call for Actions. J. Am. Geriatr. Soc. 2020, 68, 1126–1128. [Google Scholar] [CrossRef]
- McGarrigle, L.; Todd, C. Promotion of Physical Activity in Older People Using mHealth and eHealth Technologies: Rapid Review of Reviews. J. Med. Internet Res. 2020, 22, e22201. [Google Scholar] [CrossRef] [PubMed]
- Mukhtar, S. Psychological impact of COVID-19 on older adults. Curr. Med. Res. Pract. 2020, 10, 201–202. [Google Scholar]
- Manca, R.; De Marco, M.; Venneri, A. The Impact of COVID-19 Infection and Enforced Prolonged Social Isolation on Neuropsychiatric Symptoms in Older Adults With and Without Dementia: A Review. Front. Psychiatry 2020, 11, 585540. [Google Scholar] [CrossRef]
- Damiot, A.; Pinto, A.; Turner, J.; Gualano, B. Immunological Implications of Physical Inactivity among Older Adults during the COVID-19 Pandemic. Gerontology 2020, 66, 431–438. [Google Scholar] [CrossRef]
- Oh-Park, M.; Lew, H.; Raghavan, P. Telerehabilitation for Geriatrics. Phys. Med. Rehabil. Clin. N. Am. 2021, 32, 291–305. [Google Scholar] [CrossRef]
- Broche, Y.; Fernández, E.; Reyes, D. Psychological consequences of quarantine and social isolation during COVID-19 pandemic. Rev. Cuba. Salud Pública. 2021, 46, 1–14. [Google Scholar]
- Soto, M.; Ramos, M.; Camargo, L.; Calizaya, J.; Caldichoury, N.; López, N. The impact of SARS-CoV-2 on emotional state among older adults in Latin America. Int. Psychogeriatr. 2021, 33, 193–194. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.; Webster, R.; Smith, L.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Murukesu, R.; Singh, D.; Shahar, S.; Subramaniam, P. Physical Activity Patterns, Psychosocial Well-Being and Coping Strategies Among Older Persons with Cognitive Frailty of the “WE-RISE” Trial Throughout the COVID-19 Movement Control Order. Clin. Interv. Aging 2021, 16, 415–429. [Google Scholar] [CrossRef]
- United Nations. Policy Brief: The Impact of COVID-19 on Older Persons; United Nations: New York, NY, USA, 2020; pp. 1–16. [Google Scholar]
- Hill, J.; Harrington, A.; Adeoye, P.; Campbell, N.; Holden, R. Going Remote-Demonstration and Evaluation of Remote Technology Delivery and Usability Assessment With Older Adults: Survey Study. JMIR mHealth uHealth 2021, 9, e26702. [Google Scholar] [CrossRef]
- Nicol, G.; Piccirillo, J.; Mulsant, B.; Lenze, E. Action at a Distance: Geriatric Research during a Pandemic. J. Am. Geriatr. Soc. 2020, 68, 922–925. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Mental Health and Psychosocial Considerations During the COVID-19 Outbreak; WHO: Geneva, Switzerland, 2020; pp. 1–6. Available online: https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf (accessed on 1 September 2025).
- Dillon, J.; Wick, J. Telehealth: Moving Older People Along the Adoption Trajectory. Sr. Care Pharm. 2023, 38, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Salud de Chile. Programa Nacional de Telesalud. En El Contexto de Redes Integradas de Servicios de Salud; Ministerio de Salud: Santiago, Chile, 2018; pp. 1–76. [Google Scholar]
- Stephens, J.; Greenberg, G. Asynchronous Telehealth. Prim. Care Clin. Off. Pract. 2022, 49, 531–541. [Google Scholar] [CrossRef]
- Joughin, A.; Ibitoye, S.; Crees, A.; Shipway, D.; Braude, P. Developing a virtual geriatric perioperative medicine clinic: A mixed methods healthcare improvement study. Age Ageing 2021, 50, 1391–1396. [Google Scholar] [CrossRef] [PubMed]
- Davoodi, N.; Chen, K.; Zou, M.; Li, M.; Jiménez, F.; Wetle, T.; Goldberg, E. Emergency physician perspectives on using telehealth with older adults during COVID-19: A qualitative study. J. Am. Coll. Emerg. Physicians Open 2021, 2, e12577. [Google Scholar] [CrossRef]
- Khanassov, V.; Ilali, M.; Ruiz, A.; Rojas, L.; Sourial, R. Telemedicine in primary care of older adults: A qualitative study. BMC Prim. Care 2024, 25, 259. [Google Scholar] [CrossRef]
- Quesada, M.; Carmona, A.; Chami, S.; Caballero, A.; Fernández, O.; Cañadas, G.; Romero, J. Telemedicine in Elderly Hypertensive and Patients with Chronic Diseases during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 6160. [Google Scholar] [CrossRef]
- Tan, S.; Lee, C.; Yong, C.; Ding, Y. Scoping review: Facilitators and barriers in the adoption of teledentistry among older adults. Gerodontology 2021, 38, 351–365. [Google Scholar] [CrossRef]
- Lai, Y.; Chen, W.; Hsu, L.; Fu, C. The Effect of a Tele-Health Intervention Program on Home-Dwelling Persons with Dementia or MCI and on Their Primary Caregivers during the Stay-at-Home-Order Period in the COVID-19 Pandemic Outbreak: Evidence from Taiwan. Healthcare 2022, 10, 969. [Google Scholar] [CrossRef]
- Banerjee, D.; Vajawat, B.; Varshney, P.; Rao, T. Perceptions, Experiences, and Challenges of Physicians Involved in Dementia Care During the COVID-19 Lockdown in India: A Qualitative Study. Front. Psychiatry 2021, 11, 615758. [Google Scholar] [CrossRef] [PubMed]
- Quail, Z.; Bolton, L.; Massey, K. Digital delivery of non-pharmacological intervention programmes for people living with dementia during the COVID-19 pandemic. BMJ Case Rep. 2021, 14, e242550. [Google Scholar] [CrossRef]
- Schwartz, H.; Har, I.; Wenhoda, T.; Halperin, I. Staying physically active during the COVID-19 quarantine: Exploring the feasibility of live, online, group training sessions among older adults. Transl. Behav. Med. 2021, 11, 314–322. [Google Scholar] [CrossRef]
- Mukamal, R.; Dias, L.; Sarti, T.; Nunes, R.; Rego, G. The role of telemedicine in enhancing palliative care for older adults: Opportunities and challenges. BMC Geriatr. 2025, 25, 474. [Google Scholar] [CrossRef]
- Rainsford, S.; Hall, S.; Phillips, C. Effectiveness of telehealth palliative care Needs Rounds in rural residential aged care during the COVID-19 pandemic: A hybrid effectiveness-implementation study. Aust. J. Rural Health 2021, 30, 108–114. [Google Scholar] [CrossRef]
- Choi, N.; DiNitto, D.; Marti, C.; Choi, B. Telehealth Use Among Older Adults During COVID-19: Associations With Sociodemographic and Health Characteristics, Technology Device Ownership, and Technology Learning. J. Appl. Gerontol. 2022, 41, 600–609. [Google Scholar] [CrossRef]
- Smith, K.; Torous, J.; Cipriani, A. Teaching Telepsychiatry Skills: Building on the Lessons of the COVID-19 Pandemic to Enhance Mental Health Care in the Future. JMIR Ment. Health 2022, 9, e37939. [Google Scholar] [CrossRef] [PubMed]
- Chuen, V.; Dholakia, S.; Kalra, S.; Watt, J.; Wong, C.; Ho, J. Geriatric care physicians’ perspectives on providing virtual care: A reflexive thematic synthesis of their online survey responses from Ontario. Age Ageing 2024, 53, afad231. [Google Scholar] [CrossRef] [PubMed]
- Esfandiari, E.; Miller, W.; Ashe, M. The Effect of Telehealth Interventions on Function and Quality of Life for Older Adults with Pre-Frailty or Frailty: A Systematic Review and Meta-Analysis. J. Appl. Gerontol. 2021, 40, 1649–1658. [Google Scholar] [CrossRef]
- Dong, M.; Steuwe, S.; Barry, L.; Siegel, C. The Use of Telemedicine in Older Patients with Gastrointestinal Diseases. Curr. Treat. Options Gastroenterol. 2022, 20, 594–604. [Google Scholar] [CrossRef]
- Masterson, R.; Dodson, J.; Bidwell, J.; Breathett, K.; Lyles, C.; Harmon, C.; Ooi, S.; Yancy, C.; Kitsiou, S. Telehealth and Health Equity in Older Adults with Heart Failure: A Scientific Statement from the American Heart Association. Circ. Cardiovasc. Qual. Outcomes 2023, 16, E000123. [Google Scholar] [CrossRef]
- Elbaz, S.; Cinalioglu, K.; Sekhon, K.; Gruber, J.; Rigas, C.; Bodenstein, K.; Naghi, K.; Lavin, P.; Greenway, K.; Vahia, I.; et al. A Systematic Review of Telemedicine for Older Adults With Dementia During COVID-19: An Alternative to In-person Health Services? Front. Neurol. 2021, 12, 761965. [Google Scholar] [CrossRef]
- Dervan, K.; Mulkerrin, G.; McDonnell, T.; Mulkerrin, E. Technology and Specialist Care for Older Patients in the Post Covid-19 Era. JAR Life 2020, 9, 35–39. [Google Scholar] [CrossRef]
- Doraiswamy, S.; Jithesh, A.; Mamtani, R.; Abraham, A.; Cheema, S. Telehealth Use in Geriatrics Care during the COVID-19 Pandemic—A Scoping Review and Evidence Synthesis. Int. J. Environ. Res. Public Health 2021, 18, 1755. [Google Scholar] [CrossRef]
- Chueke, D. Persisting Barriers to the Adoption of Telemedicine in Latin America After the COVID-19 Pandemic. Telehealth Med. Today 2023, 8, 1–5. [Google Scholar] [CrossRef]
- Garcia, S.; Marti, M.; Malek, V.; Pacheco, A.; Luna, D.; Plazzotta, F.; Nelson, J.; Tejerina, L.; Bagolle, A.; Savignano, M.; et al. Barriers and facilitators to the implementation of telemedicine in the Americas. Rev. Panam. Salud Pública 2021, 45, e131. [Google Scholar] [CrossRef]
- Grant, M.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Info. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef] [PubMed]
- Chigbu, U.; Atiku, S.; Du Plessis, C. The Science of Literature Reviews: Searching, Identifying, Selecting, and Synthesising. Publications 2023, 11, 2. [Google Scholar] [CrossRef]
- Pizarro-Mena, R.; Rotarou, E.; Chavarro, D.; Wachholz, P.; López, M.; Perdomo, C.; Parra, S.; Barrientos, I.; Retamal, F.; Riveros, G. Comprehensive Gerontological Assessment: An Update on the Concept and Its Evaluation Tools in Latin America and the Caribbean—A Literature Review. Int. J. Environ. Res. Public Health 2024, 21, 1697. [Google Scholar] [CrossRef]
- Colegio de Kinesiólogos de Chile. Practical Telerehabilitation Guide for Physical Therapy; Colegio de Kinesiólogos de Chile: Santiago, Chile, 2020; pp. 1–181. [Google Scholar]
- Centro Nacional en Sistemas de Información en Salud. Telemedicina Durante La Epidemia de COVID-19 En Chile. Guía de Buenas Prácticas y Recomendaciones; Centro Nacional en Sistemas de Información en Salud: Santiago, Chile, 2020; pp. 1–19. [Google Scholar]
- Organización Panamerican a de la Salud. Marco de Implementación de Un Servicio de Telemedicina; Organización Panamerican a de la Salud: Washington, DC, USA, 2016; pp. 1–82. [Google Scholar]
- De Fátima, A.; Fernández, A. Desarrollo de la Telesalud en América Latina. Aspectos Conceptuales y Estado Actual; Naciones Unidas Comisión Económica para América Latina y el Caribe: Santiago, Chile, 2013; pp. 1–614. [Google Scholar]
- Organización Panamericana de la Salud. COVID-19: Salud Digital Facilitando la Telerehabilitación; Organización Panamericana de la Salud: Washington, DC, USA, 2020; pp. 1–4. [Google Scholar]
- Sixsmith, A. COVID-19 and AgeTech. Qual. Ageing Older Adults 2020, 21, 247–252. [Google Scholar] [CrossRef]
- Ministerio de Salud de Chile. Exempt Resolution N° 161. Program: More Self-Reliant Older Adults; Ministerio de Salud de Chile: Santiago, Chile, 2021; pp. 1–26. [Google Scholar]
- Mendoza, C.; Jiménez, R.; Montalvo, R.; Rodríguez, A. Situación y Retos de la Gerontología en Latinoamérica; Universidad Autónoma de Tlaxcala: Tlaxcala, México, 2023; ISBN 987-607-545-091-9. [Google Scholar]
- Ministerio de Salud de Chile. Actualización Manual de Geriatría Para Médicos; Ministerio de Salud de Chile: Santiago, Chile, 2019; pp. 1–444. [Google Scholar]
- Barrera, E.; Sarasola, A.; Sarasola, J. Telegerontologia, Robótica y entrevistas holográficas: Gerontologia y tecnologias emergentes. In IDOSO 4.0. Envelhecer em Tempos de Futuro; Carioca, V., Fernandes, A., Eds.; RVJ—Editores: Castelo Branco, Portugal, 2021; pp. 129–151. ISBN 978-989-53072-2-7. [Google Scholar]
- Tieppo, A.; Wen, C.; Mukamal, R.; Júnior, R. Guia de Telegeriatría. Soc. Bras. Geriatr. Gerontol. 2023, 1–84. [Google Scholar]
- Boriani, G.; Maisano, A.; Bonini, N.; Albini, A.; Imberti, J.; Venturelli, A.; Menozzi, M.; Ziveri, V.; Morgante, V.; Camaioni, G.; et al. Digital literacy as a potential barrier to implementation of cardiology tele-visits after COVID-19 pandemic: The INFO-COVID survey. J. Geriatr. Cardiol. 2021, 18, 739–747. [Google Scholar] [CrossRef]
- Programa Convive Digital de VTR, Criteria. Radiografía Digital Personas Mayores: Seniors Tech. 2021. Available online: https://www.vtr.com/radiografia-digital (accessed on 1 September 2025).
- Qin, W. Technology Learning and the Adoption of Telehealth Among Community-Dwelling Older Adults During the COVID-19 Outbreak. J. Appl. Gerontol. 2022, 41, 165–1656. [Google Scholar] [CrossRef]
- Lee, K.; Hyun, K.; Mitchell, J.; Saha, T.; Oran, N.; Krejci, C. Exploring Factors Enhancing Resilience Among Marginalized Older Adults During the COVID-19 Pandemic. J. Appl. Gerontol. 2022, 41, 610–618. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, E.; Lin, M.; Burke, L.; Jiménez, F.; Davoodi, N.; Merchant, R. Perspectives on Telehealth for older adults during the COVID-19 pandemic using the quadruple aim: Interviews with 48 physicians. BMC Geriatr. 2022, 22, 188. [Google Scholar] [CrossRef] [PubMed]
- Kalicki, A.; Moody, K.; Franzosa, E.; Gliatto, P.; Ornstein, K. Barriers to telehealth access among homebound older adults. J. Am. Geriatr. Soc. 2021, 69, 2404–2411. [Google Scholar] [CrossRef] [PubMed]
- Franzosa, E.; Gorbenko, K.; Brody, A.; Leff, B.; Ritchie, C.; Kinosian, B.; Sheehan, O.; Federman, A.; Ornstein, K. “There Is Something Very Personal About Seeing Someone’s Face”: Provider Perceptions of Video Visits in Home-Based Primary Care During COVID-19. J. Appl. Gerontol. 2021, 40, 1417–1424. [Google Scholar] [CrossRef]
- Foster, M.; Sethares, K. Facilitators and barriers to the adoption of telehealth in older adults: An integrative review. Comput. Inform. Nurs. 2014, 32, 523–533. [Google Scholar] [CrossRef]
- Weiss, E.; Malik, R.; Santos, T.; Ceide, M.; Cohen, J.; Verghese, J.; Zwerling, J. Telehealth for the cognitively impaired older adult and their caregivers: Lessons from a coordinated approach. Neurodegener. Dis. Manag. 2020, 11, 83–89. [Google Scholar] [CrossRef]
- Haimi, M.; Gesser, A. Application and implementation of telehealth services designed for the elderly population during the COVID-19 pandemic: A systematic review. Health Inform. J. 2022, 28, 14604582221075560. [Google Scholar] [CrossRef]
- Brodoehl, S.; Wagner, F.; Klingner, C.; Srowig, A.; Finke, K. Telemedicine Care of Dementia Patients During the COVID-19 Pandemic. Fortschr. Neurol. Psychiatr. 2023, 91, 444–454. [Google Scholar] [CrossRef]
- Hajela, N.; Kwon, B.; Penson, K.; Lee, A. Telehealth Implementation and Teaching Strategies during COVID-19 and beyond in Gait, Balance, and Mobility Clinic for Community-Dwelling Older Adults. Top. Geriatr. Rehabil. 2023, 39, 240–252. [Google Scholar] [CrossRef]
- Chen, K.; Davoodi, N.; Strauss, D.; Li, M.; Jiménez, F.; Guthrie, K.; Goldberg, E. Strategies to Ensure Continuity of Care Using Telemedicine with Older Adults during COVID-19: A Qualitative Study of Physicians in Primary Care and Geriatrics. J. Appl. Gerontol. 2022, 41, 2282–2295. [Google Scholar] [CrossRef]
- Alexander, K.; Hamlin, P.; Tew, W.; Trevino, K.; Tin, A.; Shahrokni, A.; Meditz, E.; Boparai, M.; Amirnia, F.; Sun, S.; et al. Development and implementation of an interdisciplinary telemedicine clinic for older patients with cancer—Preliminary data. J. Am. Geriatr. Soc. 2023, 71, 1638–1649. [Google Scholar] [CrossRef] [PubMed]
- Pizarro-Mena, R.; Duran, S.; Causa, M.; Rios, C.; Parra, S. Perceived Facilitators and Barriers, From the Perspective of Users, of a Multicomponent Intervention in Older People Using an Asynchronous Telehealth Modality During the COVID-19 Pandemic: A Qualitative Research. J. Aging Res. 2025, 2025, 6839569. [Google Scholar] [CrossRef] [PubMed]
- Mann, D.; Chen, J.; Chunara, R.; Testa, P.; Nov, O. COVID-19 transforms health care through telemedicine: Evidence from the field. J. Am. Med. Inform. Assoc. 2020, 27, 1132–1135. [Google Scholar] [CrossRef]
- Ufholz, K.; Sheon, A.; Bhargava, D.; Rao, G. Telemedicine Preparedness among Older Adults with Chronic Illness: Survey of Primary Care Patients. JMIR Form. Res. 2022, 6, e35028. [Google Scholar] [CrossRef]
- Abdallah, L.; Stolee, P.; Lopez, K.; Whate, A.; Boger, J.; Tong, C. The Impact of COVID-19 on Older Adults’ Perceptions of Virtual Care: Qualitative Study. JMIR Aging 2022, 5, e38546. [Google Scholar] [CrossRef]
- Callisaya, M.; Lee, A.; Khushu, A. Rapid implementation of telehealth in geriatric outpatient clinics due to COVID-19. Intern. Med. J. 2021, 51, 1151–1155. [Google Scholar] [CrossRef] [PubMed]
- Reyes, E.; Silvis, J.; Gandhi, M.; Shi, Y.; Greene, M. Telehealth access and experiences of older adults with HIV during the COVID-19 pandemic: Lessons for the future. J. Am. Geriatr. Soc. 2024, 72, 2816–2824. [Google Scholar] [CrossRef]
- Barriga, F.; Ccami, F.; Alarcon, A.; Copa, J.; Yauri, J.; Oporto, B.; Quispe, C. Satisfaction of health personnel and patients with a telehealth service in a hospital in Peru. Rev. Peru. Med. Exp. Salud Publica. 2022, 39, 415–424. [Google Scholar] [CrossRef]
- Romero-Albino, Z.; Tenorio-Mucha, J.; Cuba-Fuentes, M. Psychosocial telemonitoring and teleorientation for older adults in the Social Security (EsSalud) during the first six months of the COVID-19 pandemic in Peru. Rev. del Cuerpo Médico Hosp. Nac. Almanzor Aguinaga Asenjo 2022, 15, 392–396. [Google Scholar] [CrossRef]
- Diniz, C.; Coelho, L.; De Almeida, S.; De Aguiar, V.; De Amorim, C.; Corrêa, M.; De Moraes, R.; Barbosa, P.; Gontijo, E.; Ribeiro, A.; et al. Understanding the Personal Barriers of Elderly Patients for Carrying out Teleconsultations During COVID-19 Pandemic: An Observational Study. Telemed. J. E. Health 2024, 30, 2712–2720. [Google Scholar] [CrossRef] [PubMed]
- Hernández, C.; Jimenez, M.; Morales, A.; de la O-Murillo, A.; Soto, E. Providing geriatric oncology care using telemedicine for older patients with cancer during the COVID-19 pandemic in Mexico. Ecancermedicalscience 2023, 17, 1528. [Google Scholar] [CrossRef] [PubMed]
- Beltrán, V.; Von Marttens, A.; Acuña, P.; Sanzana, C.; Rueda, S.; Alvarado, E.; Flores, M.; Cerda, A.; Venegas, B. Implementation of a Teledentistry Platform for Dental Emergencies for the Elderly in the Context of the COVID-19 Pandemic in Chile. Biomed Res. Int. 2022, 2022, 6889285. [Google Scholar] [CrossRef]
- Caldichoury, N.; Soto, M.; Camargo, L.; Porto, M.; Herrera, J.; Shelach, S.; Rivera, C.; Ramos, M.; Gargiulo, P.; López, N. Clinical utility of Phototest via teleneuropsychology in Chilean rural older adults. Dement. Neuropsychol. 2022, 16, 316–323. [Google Scholar] [CrossRef]
- Chávarri, Y.; Ramos, W.; Covarrubias, A.; Sánchez, S.; Quiroz, P.; Alcocer, N.; Del Pilar Milke, M.; Carrillo, M.; Morales, A.; Medina, M.; et al. Providing Supportive and Palliative Care Using Telemedicine for Patients with Advanced Cancer During the COVID-19 Pandemic in Mexico. Oncologist 2021, 26, e512–e515. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez, M.; Mauro, J.; Asecio, J.; Acevedo, F.; Herrada, J.; Torres, C.; Delgado, C.; Fasce, G. Implementation of a virtual telehealth course for Chilean older adults and health students. Rev. Med. Chil. 2023, 151, 61–71. [Google Scholar] [CrossRef]
- Brandão, L.; Bauer, M.; Haas, A.; Silveira, R.; Alves, C.; Souza, D.; Beber, B.; Oliveira, W. Playing remotely in times of crisis: A program to overcome social isolation. Int. J. Geriatr. Psychiatry 2022, 37, 1–12. [Google Scholar] [CrossRef]
- Ilali, M.; Le Berre, M.; Vedel, I.; Khanassov, V. Telemedicine in the primary care of older adults: A systematic mixed studies review. BMC Prim. Care 2023, 24, 152. [Google Scholar] [CrossRef]
- Chen, W.; Flanagan, A.; Nippak, P.; Nicin, M.; Sinha, S. Understanding the Experience of Geriatric Care Professionals in Using Telemedicine to Care for Older Patients in Response to the COVID-19 Pandemic: Mixed Methods Study. JMIR Aging 2022, 5, e34952. [Google Scholar] [CrossRef]
- Watt, J.; Fahim, C.; Straus, S.; Goodarzi, Z. Barriers and facilitators to virtual care in a geriatric medicine clinic: A semi-structured interview study of patient, caregiver and healthcare provider perspectives. Age Ageing 2022, 51, afab218. [Google Scholar] [CrossRef] [PubMed]
- Jarvis, M.; Padmanabhanunni, A.; Chipps, J. An Evaluation of a Low-Intensity Cognitive Behavioral Therapy mHealth-Supported Intervention to Reduce Loneliness in Older People. Int. J. Environ. Res. Public Health 2019, 16, 1305. [Google Scholar] [CrossRef] [PubMed]
- Kharicha, K.; Manthorpe, J.; Iliffe, S.; Chew, C.; Cattan, M.; Goodman, C.; Kirby, M.; Whitehouse, J.; Walters, K. Managing loneliness: A qualitative study of older people’s views. Aging Ment. Health 2021, 25, 1206–1213. [Google Scholar] [CrossRef]
- Oche, O.; Dobyns, R.; Lin, C.; Kennelty, K.A. Determining the Factors that Impede or Facilitate the Utilization of Telemedicine (Video Visits) for Geriatric Patients. Telemed. Rep. 2022, 3, 156–165. [Google Scholar] [CrossRef]
- Hunter, I.; Lockhart, C.; Rao, V.; Tootell, B.; Wong, S. Enabling Rural Telehealth for Older Adults in Underserved Rural Communities: Focus Group Study. JMIR Form. Res. 2022, 6, e35864. [Google Scholar] [CrossRef] [PubMed]
- Nene, S.; Rauch, M.; Belanger, D.; Bennett, R.; Berry, G.; Saad, N.; Wall, M.; Morais, J.A.; Morin, S.N. Personalized Telehealth: Redesigning Complex Care Delivery for the 65+ During the COVID Pandemic: A Survey of Patients, Caregivers, and Health-care Providers. Can. Geriatr. J. 2023, 26, 150–175. [Google Scholar] [CrossRef]
- Haimi, M.; Goren, U.; Grossman, Z. Barriers and challenges to telemedicine usage among the elderly population in Israel in light of the COVID-19 era: A qualitative study. Digit. Health 2024, 10, 20552076241240236. [Google Scholar] [CrossRef]
- Mao, A.; Tam, L.; Xu, A.; Osborn, K.; Sheffrin, M.; Gould, C.; Schillinger, E.; Martin, M.; Mesias, M. Barriers to Telemedicine Video Visits for Older Adults in Independent Living Facilities: Mixed Methods Cross-sectional Needs Assessment. JMIR Aging 2022, 5, e34326. [Google Scholar] [CrossRef]
- Man, R.; Ho, A.; Lee, E.; Fenwick, E.; Aravindhan, A.; Ho, K.; Wei Tan, G.; Wei Tan, D.; Wong, T.; Yeo, K.; et al. Awareness and attitudes of elderly Southeast Asian adults towards telehealth during the COVID-19 pandemic: A qualitative study. Singap. Med. J. 2023, 66, 256–264. [Google Scholar] [CrossRef]
- Calvo, M.; Román, C.; Basualto, P.; Bannen, G.; Chamorro, M. Experience in the use of videos for the promotion of physical exercise at home in online mode in older adults in Chile during the COVID-19 pandemic. Rev. Esp. Geriatr. Gerontol. 2022, 57, 79–84. [Google Scholar] [CrossRef]
- Wardlow, L.; Leff, B.; Biese, K.; Roberts, C.; Archbald, L.; Ritchie, C.; DeCherrie, L.; Sikka, N.; Gillespie, S. Development of telehealth principles and guidelines for older adults: A modified Delphi approach. J. Am. Geriatr. Soc. 2023, 71, 371–382. [Google Scholar] [CrossRef]
- Hawley, H.; Boulton, E.; Hall, A.; Pfeiffer, K.; Todd, C. Older adults’ perceptions of technologies aimed at falls prevention, detection or monitoring: A systematic review. Int. J. Med. Inform. 2014, 83, 416–426. [Google Scholar] [CrossRef]
- Moretti, F.; Scazufca, M.; Nakamura, C.; Souza, C.; Seward, N.; Araya, R.; Moreno, D. Use of WhatsApp by older adults screened for depression in socioeconomically deprived areas of Guarulhos, São Paulo State, Brazil: Challenges and possibilities for telehealth. Cad. Saude Publica. 2023, 38, e00093422. [Google Scholar] [CrossRef] [PubMed]
- De Luca, R.; Torrisi, M.; Bramanti, A.; Maggio, M.; Anchesi, S.; Andaloro, A.; Caliri, S.; De Cola, M.; Calabrò, R. A multidisciplinary Telehealth approach for community dwelling older adults. Geriatr. Nurs. 2021, 42, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Aslan, A.; Mold, F.; van Marwijk, H.; Armes, J. What are the determinants of older people adopting communicative e-health services: A meta-ethnography. BMC Health Serv. Res. 2024, 24, 60. [Google Scholar] [CrossRef]
- Ali, M.; Alam, K.; Taylor, B.; Ashraf, M. Examining the determinants of eHealth usage among elderly people with disability: The moderating role of behavioural aspects. Int. J. Med. Inform. 2021, 149, 104411. [Google Scholar] [CrossRef] [PubMed]
- Dykgraaf, S.; Desborough, J.; Sturgiss, E.; Parkinson, A.; Dut, G.; Kidd, M. Older people, the digital divide and use of telehealth during the COVID-19 pandemic. Aust. J. Gen. Pract. 2022, 51, 721–724. [Google Scholar] [CrossRef]
- Dong, Q.; Liu, T.; Liu, R.; Yang, H.; Liu, C. Effectiveness of Digital Health Literacy Interventions in Older Adults: Single-Arm Meta-Analysis. J. Med. Internet Res. 2023, 25, e48166. [Google Scholar] [CrossRef]
- Pichan, C.; Anderson, C.; Min, L.; Blazek, M. Geriatric Education on Telehealth (GET) Access: A medical student volunteer program to increase access to geriatric telehealth services at the onset of COVID-19. J. Telemed. Telecare 2023, 29, 816–824. [Google Scholar] [CrossRef]
- Chung, G.; Ellimoottil, C.; Mccullough, J. The Role of Social Support in Telehealth Utilization Among Older Adults in the United States During the COVID-19 Pandemic. Telemed. Rep. 2021, 2, 273–276. [Google Scholar] [CrossRef]
- Steinman, L.; Chavez, E.; Chadwick, K.; Mayotte, C.; Johnson, S.; Kohn, M.; Kelley, J.; Denison, P.; Montes, C.; Spencer, L.; et al. Remote Evidence-Based Health Promotion Programs During COVID: A National Evaluation of Reach and Implementation for Older Adult Health Equity. Health Promot. Pract. 2024, 25, 475–491. [Google Scholar] [CrossRef] [PubMed]
- Brownson, R.; Colditz, G.; Proctor, E. Dissemination and Implementation Research in Health: Translating Science to Practice, 2nd ed.; Oxford University Press: Oxford, UK, 2017. [Google Scholar]
- Pinnock, H.; Barwick, M.; Carpenter, C.; Eldridge, S.; Grandes, G.; Griffiths, C.; Rycroft, J.; Meissner, P.; Murray, E.; Patel, A.; et al. Standards for Reporting Implementation Studies (StaRI) Statement. BMJ 2017, 356, i6795. [Google Scholar] [CrossRef]
- Lee, K.; Jeong, G.; Yim, J. Consideration of the Psychological and Mental Health of the Elderly during COVID-19: A Theoretical Review. Int. J. Environ. Res. Public Health 2020, 17, 8098. [Google Scholar] [CrossRef]
- Roque, N.; Boot, W. A New Tool for Assessing Mobile Device Proficiency in Older Adults: The Mobile Device Proficiency Questionnaire. J. Appl. Gerontol. 2018, 37, 131–156. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Liu, L.; Goodarzi, Z.; Watt, J. Diagnostic accuracy of eHealth literacy measurement tools in older adults: A systematic review. BMC Geriatr. 2023, 23, 181. [Google Scholar] [CrossRef]
- Verdugo, C.; Pizarro, R. Effects of physical exercise on quality of life in older people. Literature review. Mem. Del Inst. Investig. En Cienc. La Salud 2022, 20, 118–134. [Google Scholar] [CrossRef]
- Gagnon, C.; Olmand, M.; Dupuy, E.; Besnier, F.; Vincent, T.; Grégoire, C.; Lévesque, M.; Payer, M.; Bérubé, B.; Breton, J.; et al. Videoconference version of the Montreal Cognitive Assessment: Normative data for Quebec-French people aged 50 years and older. Aging Clin. Exp. Res. 2022, 34, 1627–1633. [Google Scholar] [CrossRef]
- Watt, J.; Lane, N.; Veroniki, A.; Vyas, M.; Williams, C.; Ramkissoon, N.; Thompson, Y.; Tricco, A.; Straus, S.; Goodarzi, Z. Diagnostic accuracy of virtual cognitive assessment and testing: Systematic review and meta-analysis. J. Am. Geriatr. Soc. 2021, 69, 1429–1440. [Google Scholar] [CrossRef]
- Parra-Soto, S.; Duran-Aguero, S.; Vargas-Silva, F.; Vázquez-Morales, K.; Pizarro-Mena, R. Social Outbreak in Chile, and Its Association with the Effects Biological, Psychological, Social, and Quality of Life. Int. J. Environ. Res. Public Health 2023, 20, 7096. [Google Scholar] [CrossRef] [PubMed]
- Hao, X.; Qin, Y.; Lv, M.; Zhao, X.; Wu, S.; Li, K. Effectiveness of telehealth interventions on psychological outcomes and quality of life in community adults during the COVID-19 pandemic: A systematic review and meta-analysis. Int. J. Ment. Health Nurs. 2023, 32, 979–1007. [Google Scholar] [CrossRef] [PubMed]
- Mendoza, P.; Mendoza, J. Telemedicine: Expected challenges in Chile based on the experience in the United States during the pandemic. Rev. Med. Chil. 2021, 149, 1198–1204. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).