Effects of Virtual Reality Use on Children with Cerebral Palsy and Its Applications in Health: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
- Population: children between 4 and 18 years of age with a diagnosis of cerebral palsy at any level of Gross Motor Function Classification System (GMFCS) who could follow instructions and who had no severe visual or auditory limitations.
- Interventions: VR, excluding treadmill, lokomat, and equine therapy simulator equipment.
- Comparison of interventions: this review included studies that had applied some type of VR versus conventional therapy, another intervention, or no intervention but without combining interventions in each group.
- Primary outcome measures included: functionality (motor function, balance, gait, and manual function). Activities and participation, motivation and/or satisfaction.
2.2. Exclusion Criteria
2.3. Search Methods
2.4. Study Selection
2.5. Data Extraction
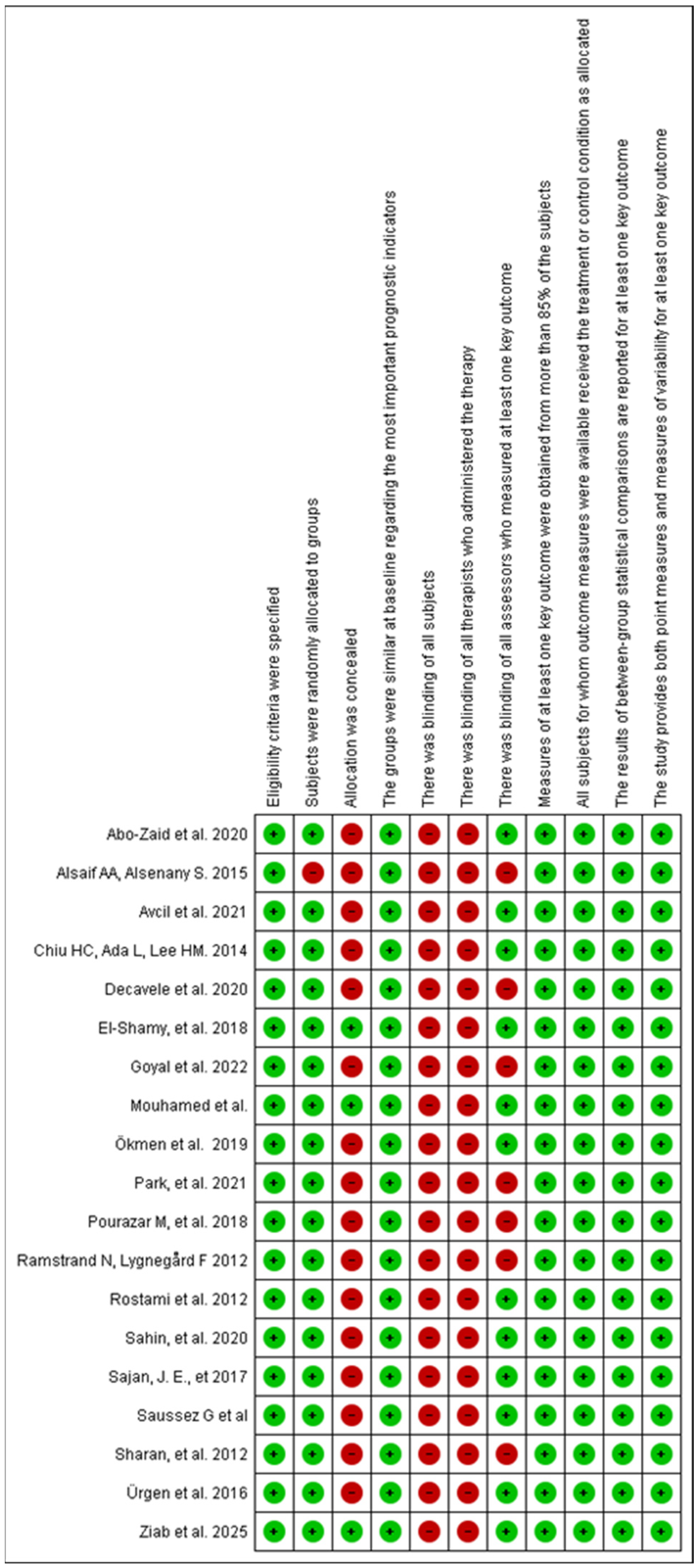
2.6. Assessment of Risk of Bias and Methodological Quality
2.7. Certainty Assessment
3. Results
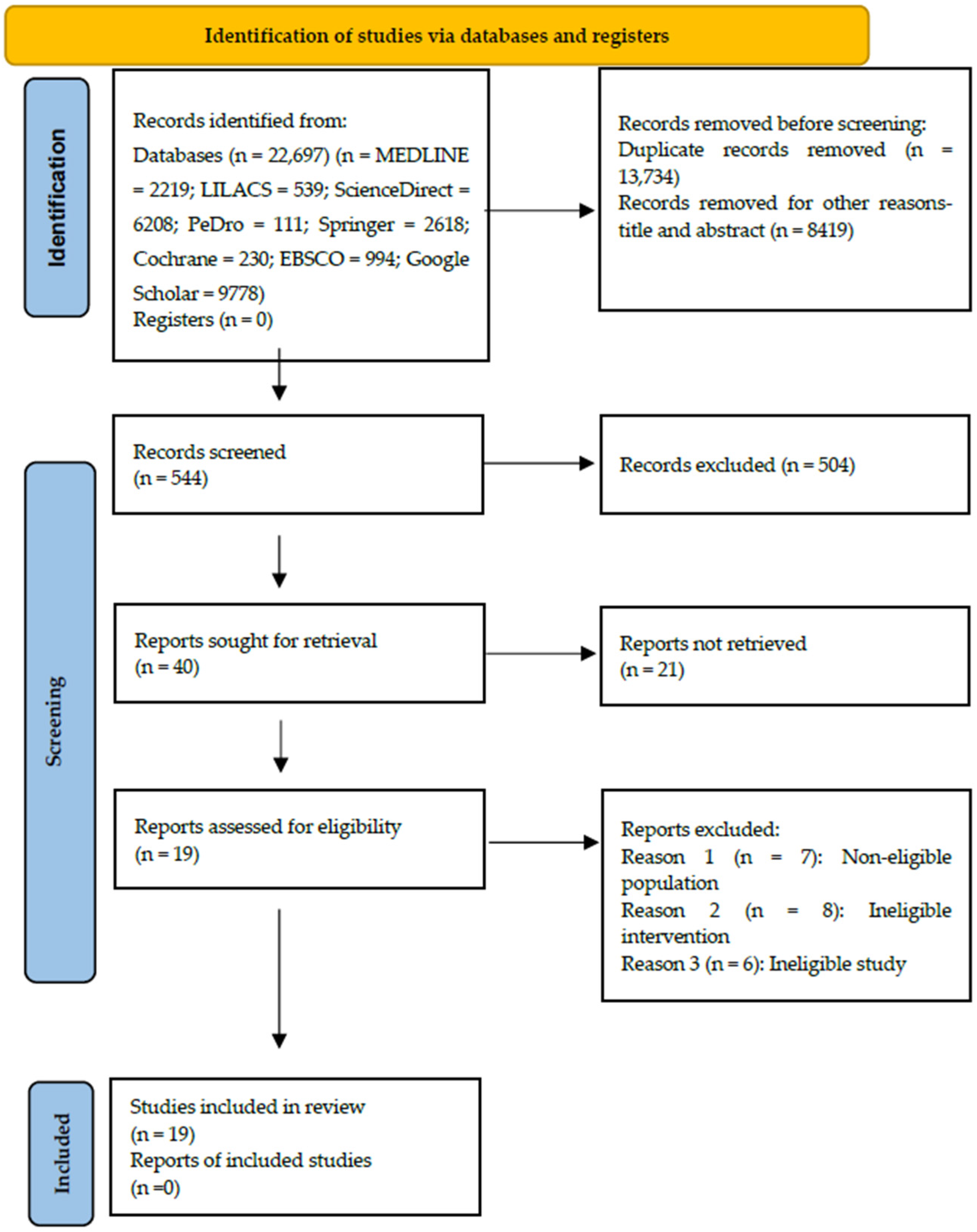
3.1. Identification of Studies
3.2. Characteristics of the Studies Included
3.3. Characteristics of the Population
3.4. Characteristics of the Intervention
3.5. Quality of the Evidence
3.6. Effect of Interventions on Measures of Functionality
3.6.1. Motor Function
3.6.2. Balance
3.6.3. Gait
3.6.4. Manual Function
3.6.5. Quality of Life Measures
Activities and Participation
Motivation and/or Satisfaction
Quality of Life
4. Discussion
4.1. Comparison with Other Reviews
4.2. Strengths and Weaknesses
4.3. Implications for Practice and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Search Strategies
References
- Albesa, S.A.; Nova Díaz, D.M.; Aznal Sáinz, E. Cerebral Palsy: New Challenges in the Era of Rare Diseases. An. Sist. Sanit. Navar. 2023, 46, e1038. [Google Scholar] [CrossRef]
- Park, M.S.; Kim, S.J.; Chung, C.Y.; Kwon, D.G.; Choi, I.H.; Lee, K.M. Prevalence and Lifetime Healthcare Cost of Cerebral Palsy in South Korea. Health Policy 2011, 100, 234–238. [Google Scholar] [CrossRef]
- Lopes, J.B.P.; Duarte, N.A.C.; Lazzari, R.D.; Oliveira, C.S. Virtual Reality in the Rehabilitation Process for Individuals with Cerebral Palsy and Down Syndrome: A Systematic Review. J. Bodyw. Mov. Ther. 2020, 24, 479–483. [Google Scholar] [CrossRef]
- Perez-Marcos, D. Virtual Reality Experiences, Embodiment, Videogames and Their Dimensions in Neurorehabilitation. J. Neuroeng. Rehabil. 2018, 15, 113. [Google Scholar] [CrossRef]
- Fandim, J.V.; Saragiotto, B.T.; Porfírio, G.J.M.; Santana, R.F. Effectiveness of Virtual Reality in Children and Young Adults with Cerebral Palsy: A Systematic Review of Randomized Controlled Trial. Braz. J. Phys. Ther. 2021, 25, 369–386. [Google Scholar] [CrossRef]
- Ravi, D.K.; Kumar, N.; Singhi, P. Effectiveness of Virtual Reality Rehabilitation for Children and Adolescents with Cerebral Palsy: An Updated Evidence-Based Systematic Review. Physiotherapy 2017, 103, 245–258. [Google Scholar] [CrossRef]
- Liu, C.; Wang, X.; Chen, R.; Zhang, J. The Effects of Virtual Reality Training on Balance, Gross Motor Function, and Daily Living Ability in Children with Cerebral Palsy: Systematic Review and Meta-Analysis. JMIR Serious Games 2022, 10, e38972. [Google Scholar] [CrossRef]
- World Health Organization (WHO). International Classification of Functioning, Disability and Health: ICF: Short Version. 2001. Available online: https://apps.who.int/iris/handle/10665/43360 (accessed on 2 February 2025).
- Ministerio de Salud (MinSalud). Modelo de Acción Integral Territorial (MAITE). 2019. Available online: https://minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/resolucion-2626-de-2019.pdf?ID=20138 (accessed on 16 February 2025).
- Chen, Y.; Fanchiang, H.C.D.; Howard, A. Effectiveness of Virtual Reality in Children with Cerebral Palsy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Phys. Ther. 2018, 98, 63–77. [Google Scholar] [CrossRef] [PubMed]
- Levac, D.; Huber, M.E.; Sternad, D. Learning and Transfer of Complex Motor Skills in Virtual Reality: Implications for Pediatric Rehabilitation. Phys. Ther. 2021, 101, pzaa220. [Google Scholar] [CrossRef]
- Fang, E.; Guan, H.; Du, B.; Ma, X.; Ma, L. Effectiveness of virtual reality for functional disorders in cerebral palsy: An overview of systematic reviews and meta-analyses. Front. Neurol. 2025, 16, 1582110. [Google Scholar] [CrossRef]
- Hao, J.; Huang, B.; Remis, A.; He, Z. The Application of Virtual Reality to Home-Based Rehabilitation for Children and Adolescents with Cerebral Palsy: A Systematic Review and Meta-Analysis. Physiother. Theory Pract. 2023, 40, 1588–1608. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Schünemann, H.; Brożek, J.; Guyatt, G.; Oxman, A. (Eds.) GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations; The GRADE Working Group: Hamilton, ON, Canada, 2013; Available online: https://gdt.gradepro.org/app/handbook/handbook.html (accessed on 26 September 2025).
- Chiu, H.C.; Ada, L.; Lee, H.M. Upper Limb Training Using Wii Sports Resort for Children with Hemiplegic Cerebral Palsy: A Randomized, Single-Blind Trial. Clin. Rehabil. 2014, 28, 1015–1024. [Google Scholar] [CrossRef] [PubMed]
- El-Shamy, S.M.; El-Banna, M.F. Effect of Wii Training on Hand Function in Children with Hemiplegic Cerebral Palsy. Physiother. Theory Pract. 2020, 36, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Abo-Zaid, N.A.; Helmy, N.A.; Elsayed, N.I.; Mohammed, A.H. Wii Sport versus Task-Oriented Training on Gait in Unilateral Cerebral Palsy: A Randomized Controlled Trial. J. Hum. Sport Exerc. 2021, 16, 522–531. [Google Scholar] [CrossRef]
- Decavele, S.; Ortibus, E.; Van Campenhout, A.; Molenaers, G.; Jansen, B.; Omelina, L.; Franki, I. The Effect of a Rehabilitation Specific Gaming Software Platform to Achieve Individual Physiotherapy Goals in Children with Severe Spastic Cerebral Palsy: A Randomized Crossover Trial. Games Health J. 2020, 9, 376–385. [Google Scholar] [CrossRef]
- Şahin, S.; Köse, B.; Aran, O.T.; Bahadlr Aǧce, Z.; Kaylhan, H. The Effects of Virtual Reality on Motor Functions and Daily Life Activities in Unilateral Spastic Cerebral Palsy: A Single-Blind Randomized Controlled Trial. Games Health J. 2020, 9, 45–52. [Google Scholar] [CrossRef]
- Avcil, E.; Tarakci, D.; Arman, N.; Tarakci, E. Upper Extremity Rehabilitation Using Video Games in Cerebral Palsy: A Randomized Clinical Trial. Acta Neurol. Belg. 2021, 121, 1053–1060. [Google Scholar] [CrossRef]
- Ökmen, B.M.; Aslan, M.D.; Nakipoğlu Yüzer, G.F.; Özgirgin, N. Effect of Virtual Reality Therapy on Functional Development in Children with Cerebral Palsy: A Single-Blind, Prospective, Randomized-Controlled Study. Turk. J. Phys. Med. Rehabil. 2019, 65, 371–378. [Google Scholar] [CrossRef]
- Ramstrand, N.; Lygnegård, F. Can Balance in Children with Cerebral Palsy Improve Through Use of an Activity Promoting Computer Game? Technol. Health Care 2012, 20, 501–510. [Google Scholar] [CrossRef]
- Urgen, M.; Akbayrak, T.; Gunel, M.; Cankaya, O.; Guchan, Z.; Turkyilmaz, E. Investigation of the Effects of the Nintendo Wii-Fit Training on Balance and Advanced Motor Performance in Children with Spastic Hemiplegic Cerebral Palsy: A Randomized Controlled Trial. Int. J. Ther. Rehabil. Res. 2016, 5, 146. [Google Scholar] [CrossRef]
- Rostami, H.R.; Arastoo, A.A.; Nejad, S.J.; Mahany, M.K.; Malamiri, R.A.; Goharpey, S. Effects of Modified Constraint-Induced Movement Therapy in Virtual Environment on Upper-Limb Function in Children with Spastic Hemiparetic Cerebral Palsy: A Randomised Controlled Trial. NeuroRehabilitation 2012, 31, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H.; Son, S.M.; Choi, J.Y. Effect of Posture Control Training Using Virtual Reality Program on Sitting Balance and Trunk Stability in Children with Cerebral Palsy. NeuroRehabilitation 2021, 48, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Sajan, J.E.; John, J.A.; Grace, P.; Sabu, S.S.; Tharion, G. Wii-Based Interactive Video Games as a Supplement to Conventional Therapy for Rehabilitation of Children with Cerebral Palsy: A Pilot, Randomized Controlled Trial. Dev. Neurorehabilit. 2017, 20, 361–367. [Google Scholar] [CrossRef]
- Pourazar, M.; Mirakhori, F.; Hemayattalab, R.; Bagherzadeh, F. Use of Virtual Reality Intervention to Improve Reaction Time in Children with Cerebral Palsy: A Randomized Controlled Trial. Dev. Neurorehabilit. 2018, 21, 515–520. [Google Scholar] [CrossRef]
- Alsaif, A.A.; Alsenany, S. Effects of Interactive Games on Motor Performance in Children with Spastic Cerebral Palsy. J. Phys. Ther. Sci. 2015, 27, 2001–2003. [Google Scholar] [CrossRef]
- Sharan, D.; Ajeesh, P.S.; Rameshkumar, R.; Mathankumar, M.; Paulina, R.J.; Manjula, M. Virtual Reality-Based Therapy for Postoperative Rehabilitation of Children with Cerebral Palsy. Work 2012, 41 (Suppl. S1), 3612–3615. [Google Scholar] [CrossRef]
- Saussez, G.; Bailly, R.; Araneda, R.; Paradis, J.; Ebner-Karestinos, D.; Klöcker, A.; Sogbossi, E.S.; Riquelme, I.; Brochard, S.; Bleyenheuft, Y. Efficacy of Integrating a Semi-Immersive Virtual Device in the HABIT-ILE Intervention for Children with Unilateral Cerebral Palsy: A Non-Inferiority Randomized Controlled Trial. J. Neuroeng. Rehabil. 2023, 20, 98. [Google Scholar] [CrossRef]
- Mouhamed, H.A.; Abo-Zaid, N.A.; Khalifa, H.A.; Ali, M.E.; Elserty, N.S.; Behiry, M.A.; Heneidy, W.E. Efficacy of Virtual Reality on Balance Impairment in Ataxic Cerebral Palsy Children: Randomized Controlled Trial. Eur. J. Phys. Rehabil. Med. 2024, 60, 949–955. [Google Scholar] [CrossRef]
- Goyal, C.; Vardhan, V.; Naqvi, W. Non-Immersive Virtual Reality as an Intervention for Improving Hand Function and Functional Independence in Children with Unilateral Cerebral Palsy: A Feasibility Study. Cureus 2022, 14, e26085. [Google Scholar] [CrossRef]
- Ziab, H.; Saleh, S.; Talebian, S.; Olyaei, G.; Mazbouh, R.; Sarraj, A.R.; Hadian, M.R. Effectiveness of Virtual Reality Training Compared to Balance-Specific Training and Conventional Training on Balance and Gross Motor Functions of Children with Cerebral Palsy: A Double-Blinded Randomized Controlled Trial. J. Pediatr. Rehabil. Med. 2024, 17, 353–368. [Google Scholar] [CrossRef] [PubMed]
- Meneses Castaño, C.; Penagos, P.; Jaramillo, B.Y. Effectiveness of Robotic Technology and Virtual Reality for the Rehabilitation of Motor Function in Cerebral Palsy: Systematic Review. Rehabilitación 2023, 57, 100752. [Google Scholar] [CrossRef]
- Komariah, M.; Hidayat, R.; Maulana, S.; Setiawan, D.; Mustika, R.; Nugraha, B. Effectivity of Virtual Reality to Improve Balance, Motor Function, Activities of Daily Living, and Upper Limb Function in Children with Cerebral Palsy: A Systematic Review and Meta-Analysis. Children 2024, 11, 152. [Google Scholar] [CrossRef] [PubMed]
- Velasco Aguado, J.; Espada, M.C.; Muñoz-Jiménez, J.; Ferreira, C.C.; Gámez-Calvo, L. Physical Exercise Interventions Using Virtual Reality in Children and Adolescents with Cerebral Palsy: Systematic Review. Healthcare 2025, 13, 189. [Google Scholar] [CrossRef] [PubMed]
- da Silva Ribeiro, D.C.; Silva, R.; Lima, V.; de Sousa Neto, B.M.; Lindquist, A.R.R. Effectiveness of Virtual Reality Interventions of the Upper Limb in Children and Young Adults with Cerebral Palsy: A Systematic Review with Meta-Analysis. Braz. J. Phys. Ther. 2021, 25, 271–286. [Google Scholar] [CrossRef]
- Warnier, N.; Lambregts, S.; Van de Port, I. Effect of Virtual Reality Therapy on Balance and Walking in Children with Cerebral Palsy: A Systematic Review. Dev. Neurorehabilit. 2020, 23, 502–518. [Google Scholar] [CrossRef]
- Cano de la Cuerda, R. Nuevas Tecnologías en Neurorrehabilitación; Editorial Médica Panamericana: Madrid, Spain, 2018. [Google Scholar]
- Amirthalingam, J.; Paidi, G.; Alshowaikh, K.; Jayarathna, I.; Salibindla, D.B.A.M.R.; Karpinska-Leydier, K.; Ergin, H.E. Virtual Reality Intervention to Help Improve Motor Function in Patients Undergoing Rehabilitation for Cerebral Palsy, Parkinson’s Disease, or Stroke: A Systematic Review of Randomized Controlled Trials. Cureus 2021, 13, e16763. [Google Scholar] [CrossRef]
- Alrashidi, M.; Wadey, C.A.; Tomlinson, R.J.; Buckingham, G.; Williams, C.A. The Efficacy of Virtual Reality Interventions Compared with Conventional Physiotherapy in Improving the Upper Limb Motor Function of Children with Cerebral Palsy: A Systematic Review of Randomised Controlled Trials. Disabil. Rehabil. 2023, 45, 1773–1783. [Google Scholar] [CrossRef]
- Shoukat, F.; Ur Rehman, S.S.; Ahmed, A. Effects of Physical Exercise Intervention on Improving Physical Functioning and Quality of Life among the Geriatric Population: A Systematic Review of Randomized Controlled Trials. J. Pak. Med. Assoc. 2024, 74, 1481–1487. [Google Scholar] [CrossRef]
- Qian, J.; McDonough, D.J.; Gao, Z. The Effectiveness of Virtual Reality Exercise on Individuals’ Physiological, Psychological and Rehabilitative Outcomes: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 4133. [Google Scholar] [CrossRef] [PubMed]
- Yun, H.; Park, M.; Lee, H.; Choi, E.K. Healthcare Interventions for Children Using Nonimmersive Virtual Reality: A Mixed Methods Systematic Review. J. Pediatr. Health Care 2024, 38, 703–716. [Google Scholar] [CrossRef]
- Cuschieri, S. The CONSORT Statement. Saudi J. Anaesth. 2019, 13 (Suppl. S1), S27–S30. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better Reporting of Interventions: Template for Intervention Description and Replication (TIDieR) Checklist and Guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef] [PubMed]
| Study | Population | Age (Years) | GMFCS | RV Intervention | Group Control | Duration | Place |
|---|---|---|---|---|---|---|---|
| Abo-Zaid et al. (2021) [19] | 60 children with hemiplegic CP | 8–12 | I–II | Nintendo Wii—Nintendo Co., Ltd., Kioto (Kyoto), Japan | NDT | 60 min/3 days/16 weeks | Clinical setting |
| AlSaif AA, Alsenany S. (2015) [30] | 40 children with spastic diplegia CP | 6–10 | III | Nintendo Wii—Nintendo Co., Ltd., Kioto (Kyoto), Japan | Not reported | 20 min/1 day/12 weeks | At home |
| Avcil et al. (2021) [22] | 30 children with CP hemiplegia, diplegia, and dyskinetic type | 8–12 | Range I–IV | Nintendo Wii—Nintendo Co., Ltd., Kioto (Kyoto), Japan | NDT-based upper extremity rehabilitation | 20 min/3 days/8 weeks | Clinical setting |
| Chiu HC, Ada L, Lee HM. (2014) [17] | 62 children with hemiparesis CP | 5–13 | Range I–V | Nintendo Wii—Nintendo Co., Ltd., Kioto (Kyoto), Japan | Conventional physiotherapy | 3 days/6 weeks | At home |
| Decavele et al. (2020) [20] | 32 children with hemiparesis CP | 6–15 | III–IV | Nintendo Wii and Xbox Kinect—Nintendo Co., Ltd., Kioto (Kyoto), Japan/Microsoft Corporation, Redmond, WA, USA | Conventional physiotherapy | 45 min/2 days/12 weeks | Rehabilitation center |
| El-Shamy SM et al. (2018) [18] | 40 children with hemiparesis CP | 8–12 | Range I–III | Nintendo Wii—Nintendo Co., Ltd., Kioto (Kyoto), Japan | Conventional physiotherapy | 60 min/3 days/12 weeks | Clinical setting |
| Ökmen et al. (2019) [23] | 41 children with hemiplegia, diplegia, quadriplegia, dyskinetic and mixed CP | 5–15 | Range I–III | PlayStation—Sony Interactive Entertainment Inc., San Mateo, CA, USA | NDT and conventional physiotherapy | 60 min/3 days/4 weeks | Clinical setting |
| Park SH et al. (2021) [27] | 20 children with diplegia and spastic quadriplegia CP | 6–18 | III–IV | Nintendo Wii—Nintendo Co., Ltd., Kioto (Kyoto), Japan | Arm reach training in the sitting position | 40 min/2 days/4 weeks | Clinical setting |
| Pourazar et al. (2018) [29] | 30 children with CP. | 7–12 | Range I–III | Xbox Kinect—Microsoft Corporation, Redmond, WA, USA | Conventional physiotherapy | 20 sessions/6 weeks | Rehabilitation center |
| Ramstrand N, Lygnegård F. (2012) [24] | 18 children with hemiplegic or diplegic CP | 8–17 | I–II | Nintendo Wii—Nintendo Co., Ltd., Kioto (Kyoto), Japan | Without intervention | 30 min/5 days/5 weeks | At home |
| Rostami et al. (2012) [26] | 32 children with spastic hemiparesis CP | 6–11 | Does not report. | Biometrics Ltd. E-Link—Biometrics Ltd., Gwent, UK | Group CIMT, Group combined VR and modified CIMT, Group control (conventional therapy) | 90 min/3 days/4 weeks | Rehabilitation center |
| Şahin et al. (2020) [21] | 60 children with spastic hemiparesis CP | 7–16 | I–II | Xbox Kinect—Microsoft Corporation, Redmond, WA, USA | NDT | 45 min/2 days/8 weeks | Clinical setting |
| Sajan et al. (2017) [28] | 20 children with CP | 5–20 | I–IV | Nintendo Wii—Nintendo Co., Ltd., Kioto (Kyoto), Japan | Conventional therapy | 45 min/6 days/3 weeks | Clinical setting |
| Sharan et al. (2012) [31] | 29 children with CP | 8–15 | Does not report. | Nintendo Wii—Nintendo Co., Ltd., Kioto (Kyoto), Japan | Not reported | 3 days/3 weeks | At home |
| Ürgen et al. (2016) [25] | 30 children with spastic hemiplegic CP | 7–14 | I–II | Nintendo Wii—Nintendo Co., Ltd., Kioto (Kyoto), Japan | Not reported | 45 min/2 days/9 weeks | Rehabilitation center |
| Saussez G et al. (2023) [32] | 40 children with CP | 5–18 | I–II | REAtouch®—Mobility Research Inc. (LiteGait), Tempe, AZ, USA | HABIT-ILE | 90 h spread over 10–12 consecutive days. | HABIT-ILE camps |
| Mouhamed et al. (2024) [33] | 64 children with ataxic cerebral palsy | 9–14 | I–II | Nintendo Wii (balance board)—Nintendo Co., Ltd., Kioto (Kyoto), Japan | Conventional physiotherapy | 3 sessions/week for 3 months (60 min/session) | Clinical setting |
| Goyal et al. (2022) [34] | 10 unilateral CP | 6–10 | Range I–III | NIVR—Non-Immersive Virtual Reality (generic term) | Occupational therapy | 5 sessions per week for 4 weeks (20 sessions) | Clinical setting |
| Ziab et al., 2025 [35] | 46 children with CP | 4–12 | I–II | Xbox Kinect—Microsoft Corporation, Redmond, WA, USA | Conventional physiotherapy | 18 sessions (3/week, 6 weeks) | Rehabilitation Centers |
| Certainty Evaluation | ||||||
|---|---|---|---|---|---|---|
| № de Studies | Study Design | Risk of Bias | Inconsistency | Indirect Evidence | Inaccuracy | Quality of Evidence |
| Gross Motor Function measured with GMFM | ||||||
| 3 | randomized trials | not serious | not serious | not serious | serious a | Low |
| Gross Motor Function measured with BOTMP | ||||||
| 2 | randomized trials | serious b | not serious | serious c | serious a | Very Low |
| Gross Motor Function measured with GMPM, PEDI, mABC-2, BOTMP-SF and PMDS-2 | ||||||
| 4 | randomized trials | serious b | not serious | not serious | serious a | Low |
| Balance measured with PBS | ||||||
| 4 | randomized trials | not serious | serious d | not serious a | serious a | Low |
| Balance measured with TCMS, mFRT, SRT, DRT, BR, PE and TUG | ||||||
| 6 | randomized trials | not serious | not serious | not serious | serious a | Low |
| March measured with 3DMA, PC1 min, FMS | ||||||
| 3 | randomized trials | serious b | not serious | not serious | serious a | Low |
| Manual Function measured with MMDT, DEI, JTTHF, MACS, BFMF, QUEST | ||||||
| 5 | randomized trials | serious e | serious d | not serious | serious a | Very Low |
| Motivation and/or satisfaction measured with DMQ and level of motivation-satisfaction | ||||||
| 2 | randomized trials | serious a | serious d | not serious | serious a | Very Low |
| Activities and participation measured with GMFCS, WeeFim and level of participation | ||||||
| 3 | randomized trials | serious a | serious d | not serious | serious a | Very Low |
| Quality of life measured with CHAQ | ||||||
| 1 | randomized trials | not serious | not serious | not serious | serious a | Low |
| Dimension/Domain | Instruments/Measures Used |
|---|---|
| Motor function | Gross Motor Function Measure (GMFM) [20,25,35] Gross Motor Performance Measure (GMPM) [25] Pediatric Evaluation of Disability Inventory (PEDI) [25] Movement Assessment Battery for Children-2 (mABC-2) [30] Peabody Developmental Motor Scale (PDMS-2) [18] Bruininks–Oseretsky Test of Motor Proficiency (BOTMP) [26,30] BOTMP Short Form (BOTMP-SF) [21] |
| Balance | Pediatric Balance Scale (PBS) [20,25,28,31,33,35] Trunk Control Measurement Scale (TCMS) [27] Modified Functional Reach Test (mFRT) [27] Simple Reaction Time, Discriminant Reaction Time (DRT) [28] Static Posturography (PE) [26] Timed Up and Go (TUG) [25] Reactive Balance (BR) [24] |
| Gait/Ambulation | 3D Motion Analysis (3DMA) [19] 1 min Walk Test [30] 6 min Walk Test [32] Functional Mobility Scale (FMS) [19,23] |
| Manual skills/Manual Function | Minnesota Manual Dexterity Test (MMDT) [22] Duruöz Hand Index (DHI) [22] Jebsen–Taylor Test of Hand Function (JTTHF) [17,32] MACS (Manual Ability Classification System) [33] Bimanual Fine Motor Function (BFMF) [23] 9-Hole Peg Test (9HPT) [34] Quality of Upper Extremity Skills Test (QUEST) [28] |
| Activities/Participation/Quality of Life | GMFCS (Gross Motor Function Classification System) [23] WeeFIM (Wee Functional Independence Measure) [21,34] Childhood Health Assessment Questionnaire [22] |
| Motivation/Satisfaction | Mastery Motivation Questionnaire (DMQ) [20] Author-designed motivation/satisfaction survey [31]. |
| Study | Outcome Measures | Main Results |
|---|---|---|
| Abo-Zaid et al. (2021) [19] | 3DMA | Swing Phase (%) Pre G1: 47.08 ± 1.99 Post: G1: 44.92 ± 1. Pre: G2: 47.38 ± 2.20 Post: G2: 45.87 ± 1.50 Cadence (steps/min) Pre G1: 83.91 ± 3.621 Post G1: 87.13 ± 3.025 Pre G2: 82.72 ± 4.874 Post G2: 84.40 ± 3.965 |
| AlSaif AA, Alsenany S. (2015) [30] | mABC-2, BOTMP, PC1 min Walk test | mABC-2 Pre G1: 38.3 ± 5.42 Post G1: 44.1 ± 5.21 Pre G2: 38.9 ± 5.27 Post G2: 39.1 ± 5.16 BOTMP Pre G1: 2.23 ± 0.47 Post G1: 3.78 ± 0.39 Pre G2: 2.82 ± 0.51 Post G2: 3.12 ± 0.66 1 min WT Pre G1: 90.1 ± 7.21 Post G1: 98.8 ± 6.75 Pre G2: 91.1 ± 6.93 Post G2: 91.8 ± 6.82 |
| Avcil et al. (2021) [22] | MMDT, CHAQ, DEI, DM | MMDT Pre G1: 508.82 ± 303.34 Post G1: 346.53 ± 188.19 Pre G2: 450.93 ± 447.51 Post G2: 385.73 ± 412.27 CHAQ Pre G1: 1.70 ± 0.57 Post G1: 1.37 ± 0.54 Pre G2: 2.31 ± 0.67 Post G2: 1.87 ± 0.68 |
| Chiu HC, Ada L, Lee HM. (2014) [17] | Coordination, 9HPT, JTTHF | Coordination Pre G1: 0.26 ± 0.18 Post G1: 0.28 ± 0.20 Pre G2: 0.30 ± 0.22 Post G2: 0.28 ± 0.21 9HPT Pre G1: 0.10 ± 0.09 Post G1: 0.12 ± 0.10 Pre G2: 0.12 ± 0.10 Post G2: 0.13 ± 0.11 JTTHF Pre G1: 0.21 ± 0.14 Post G1: 0.26 ± 0.18 Pre G2: 0.22 ± 0.15 Post G2: 0.27 ± 0.20 |
| Decavele et al. (2020) [20] | GAS, TCMS, PBS, GMFM-88, DMQ | GAS Pre G1: 29.9 Post G1: 38.4 p =< 0.001 Pre G1: 27.9 Post G1: 30.0 p = 0.007 TCMS Pre G1: 37.8 Post G1: 42.3 p =< 0.001 Pre G2: 35.1 Post G2: 33.1 p = 0.124 GMFM Pre G1: 52.9 Post G1: 54.4 p =< 0.001 Pre G2: 45.0 Post G2: 44.1 p = 0.317 PBS Pre G1: 22.8 Post G1: 24.1 p = 0.01 Pre G2: 18.9 Post G2: 18.5 p = 0.264 DMQ G1: 76.8 G2: 79.8 |
| El-Shamy SM et al. (2018) [18] | MAS, DM, PMDS-2 | MAS Pre G1: 2.5 ± 0.6 Post G1: 1.6 ± 0.3 DM Pre G1: 8.7 ± 1.9 Post G1: 11 ± 1.5 Pre G2: 8.5 ± 1.6 Post G2: 9.2 ± 1.2 PMDS-2 Pre G1: 3 Post G1: 3 Pre G2: 2 Post G2: 2 |
| Ökmen et al. (2019) [23] | BFMF, GMFCS, FMS | BFMF Pre G1: 3 Post G1: 2 p = 0.001 * Pre G2: 2.5 Post G2: 2.5 p = 0.317 GMFCS Pre G1: 3 Post G1: 3 p = 0.005 * Pre G2: 3 Post G2: 3 FMS Pre G1: 2 Post G1: 2.5 p = 0.003 * Pre G2: 3 Post G2: 3 p = 0.17 |
| Park SH et al. (2021) [27] | Software Wii Balance Board, mFRT, TCMS | Velocity Pre G1: 7.25 ± 4.99 (cm/s) Post G1: 5.68 ± 4.51 p = 0.005 Pre G2: 6.78 ± 5.19 Post G2: 6.41 ± 5.21 p = 0.169 mFRT: Pre G1: 16.02 ± 4.52 Post G1: 21.05 ± 6.34 p = 0.005 TCMS Pre G1: Pre 19.5 ± 9.67 Post G1: 27.4 ± 10.86 p = 0.005 Pre G2: 17.3 ± 7.7 Post G2: 22.3 ± 9.17 p = 0.005 |
| Pourazar et al. (2018) [29] | SRT y DRT | SRT Pre G1: 0.605 ± 0.133 Post G1: 0.343 ± 0.156 Pre G2: 0.610 ± 0.265 Post G2: 0.576 ± 0.236 DRT Pre G1: 0.936 ± 0.292 Post G1: 0.568 ± 0.177 Pre G2: 0.952 ± 0.289 Post G2: 0.884 ± 0.343 |
| Ramstrand N, Lygnegård F. (2012) [24] | mSOt y BR | Stable support (eyes open) Pre G1: 2.34 Post G1: 2.21 Pre G2: 2.34 Post G2: 2.17 Stable support (eyes closed) Pre G1: 2.70 Post G1: 2.59 Pre G2: 2.70 Post G2: 2.59 |
| Rostami et al. (2012) [26] | BOTMP | Amount of use Pre G1: 0.66 ± 0.37 Post G1: 2.37 ± 0.45 Pre G2: 0.74 ± 0.24 Post G2: 2.54 ± 0.51 Quality of movement Pre G1: 0.53 ± 0.31 Post G1: 2.26 ± 0.24 Pre G2: 0.59 ± 0.28 Post G2: 2.21 ± 0.19 |
| Şahin et al. (2020) [21] | BOTMP-SF y WeeFIM | BOTMP-SF Pre G1: 35.46 ± 20.29 Post G1: 69.96 ± 34.42 0.0001 * Pre G2: 36.36 ± 19.83 45.10 ± 18.14 0.028 * WeeFIM Pre G1: 103.06 ± 15.04 Post G1: 112.96 ± 10.20 0.0001 * Pre G2: 102.56 ± 14.88 Post G2: 104.70 ± 13.67 0.012 * |
| Sajan et al. (2017) [28] | PE, PBS, QUEST, BBT, TVPS-3. | Sway velocity eyes open (mm/s) Pre G1: 137.67 ± 179.52 Post G1: 83.06 ± 67.73 Pre G2: 137.66 ± 96.06 Post G2: 127.93 ± 86.33 PBS Pre G1: 15.70 ± 14.77 Post G1: 18.7 ± 16.33 Pre G2: 20.44 ± 19.1 Post G2: 25.00 ± 17.71 BBT Pre G1: 46.9 ± 16.39 Post G1: 55.2 ± 19.70 Pre G2: 59.33 ± 27.77 Post G2: 68.00 ± 27.09 QUEST Pre G1: 72.86 ± 22.57 Post G1: 76.38 ± 19.72 Pre G2: 86.83 ± 9.78 Post G2: 88.45 ± 9.30 TVPS: Pre G1: 32.10 ± 9.60 Post G1: 36.50 ± 9.63 Pre G2: 37.30 ± 13.20 Post G2: 43.44 ± 14.93 Walk Pre G1: 12.61 ± 19.73 Post G1: 20.61 ± 28.42 Pre G2: 23.89 ± 33.23 Post G2: 34.31 ± 39.98 |
| Sharan et al. (2012) [31] | MACS, PBS, level of participation, motivation, and child satisfaction. | MACS: Pre G1: 1.71 ± 0.99 Post G1: 1.43 ± 0.65 p < 0.05 * Pre G2: 2.20 ± 1.21 Post G2: 1.73 ± 0.80 p < 0.01 * PBS: Pre G1: 35.57 ± 12.67 Post G1: 45.00 ± 8.73 p < 0.001 * Pre G2: 26.40 ± 14.63 Post G2: 36.07 ± 14.38 p < 0.001 * |
| Ürgen et al. (2016) [25] | GMFM, GMPM, TUG, PBS, PEDI | GMFM: Pre G1: 91.89 ± 3.80 Post G1: 96.05 ± 2.43 Pre G2: 87.95 ± 6.04 Post G2: 90.92 ± 5.04 GMPM Pre G1: 197.20 ± 15.42 Post G1: 206.00 ± 15.51 Pre G2: 185.13 ± 24.89 Post G2: 190.40 ± 22.65 TUG Pre G1: 6.48 ± 0.85 Post G1: 6.26 ± 0.67 Pre G1: 6.60 ± 0.82 Post G1: 6.55 ± 0.71 PBS Pre G1: 50.07 ± 2.86 Post G1: 53.80 ± 1.61 Pre G2: 48.47 ± 3.50 Post G2: 49.27 ± 3.12 PEDI G1: 180.07 ± 12.36 G2: 181.73 ± 8.18 |
| Saussez G et al. (2023) [32] | AHA, JTTHF, BBT, MFPT, 6MW, ABILHAND-Kids, ACTIVLIM-CP, PEDI, ABILOCO-Kids, COPM. | AHA Pre G1: 54.9 ± 18 Post G1: 58.4 ± 29 p = 0.002 Pre G2: 58.3 ± 16 Post G2: 60.3 ± 16 p = 0.039 BBT Pre G1: 20.8 ± 13 Post G1: 21.7 ± 13 p = 0.092 Pre G2: 22 ± 11 Post G2: 23.1 ± 11 p = 0.029 JTTHF Pre G1: 419 ± 358 Post G1: 364 ± 333 Pre G2: 412 ± 344 Post G2: 367 ± 344 6MWT Pre G1: 467 ± 90 469 ± 101 Post G1: 469 ± 101 Pre G2: 478 ± 106 Post G2: 479 ± 117 |
| Mouhamed et al. (2024) [33] | PBS, OASI, APSI, MLSI | PBS: Pre G1: 22.34 ± 3.21 Post G1: 41.38 ± 2.72 Pre G2: 23.78 ± 3.89 Post G2: 36.03 ± 2.85 OASI Pre G1: 5.40 ± 0.56 Post G1: 3.32 ± 0.77 Pre G2: 5.55 ± 0.47 Post G2: 4.36 ± 0.64 APSI Pre G1: 5.21 ± 0.55 Post G1: 3.47 ± 0.36 Pre G2: 5.13 ± 0.58 Post G2: 3.76 ± 0.38 MLSI Pre G1: 4.60 ± 0.35 Post G1: 3.04 ± 0.42 |
| Goyal et al. (2022) [34] | 9HPT, BBT, ABILHAND-Kids, WeeFIM | 9HPT Pre G1: 55.80 ± 6.01 Post G1: 39.80 ± 4.43 Pre G2: 56.80 ± 7.19 Post G2: 51.40 ± 6.58 BBT Pre G1: 15.60 ± 3.50 Post G1: 26.60 ± 2.30 Pre G2: 14.00 ± 3.53 Post G2: 17.80 ± 5.01 ABILHAND Kids Pre G1: 50.40 ± 6.54 Post G1: 64.00 ± 3.00 Pre G2: 44.40 ± 7.36 Post G2: 47.80 ± 5.93 WeeFIM Pre G1: 28.60 ± 7.36 Post G1: 35.40 ± 7.23 Pre G2: 25.80 ± 5.80 Post G2: 27.20 ± 5.16 |
| Ziab et al., 2025 [35] | GMFM (D y E), PBS, FTSTST, COM (UCOM y LCOM) | GMFM (D) G1: 6.50 p = 0.000 G2: −1.40 p = 0.01 GMFM (E G1: −7.07P= 0.000 G2: −2.40 p = 0.000 PBBS: G1: −9.14 p = 0.000 G2: −0.87P= 0.000 FTSTST G1: 9.21 p = 0.000 G2: 1.40 p = 0.000 LUCOM G1: 6.68 p = 0.000 G2: 0.26 p = 0.25 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mesa-Burbano, A.E.; Fernández-Polo, M.A.; Hurtado-Sánchez, J.S.; Betancur-Bedoya, S.P.; Quiguanas-López, D.M.; Ordoñez-Mora, L.T. Effects of Virtual Reality Use on Children with Cerebral Palsy and Its Applications in Health: A Systematic Review. Healthcare 2025, 13, 2571. https://doi.org/10.3390/healthcare13202571
Mesa-Burbano AE, Fernández-Polo MA, Hurtado-Sánchez JS, Betancur-Bedoya SP, Quiguanas-López DM, Ordoñez-Mora LT. Effects of Virtual Reality Use on Children with Cerebral Palsy and Its Applications in Health: A Systematic Review. Healthcare. 2025; 13(20):2571. https://doi.org/10.3390/healthcare13202571
Chicago/Turabian StyleMesa-Burbano, Angie Estefania, María Alejandra Fernández-Polo, John Steven Hurtado-Sánchez, Silvia Patricia Betancur-Bedoya, Diana Maritza Quiguanas-López, and Leidy Tatiana Ordoñez-Mora. 2025. "Effects of Virtual Reality Use on Children with Cerebral Palsy and Its Applications in Health: A Systematic Review" Healthcare 13, no. 20: 2571. https://doi.org/10.3390/healthcare13202571
APA StyleMesa-Burbano, A. E., Fernández-Polo, M. A., Hurtado-Sánchez, J. S., Betancur-Bedoya, S. P., Quiguanas-López, D. M., & Ordoñez-Mora, L. T. (2025). Effects of Virtual Reality Use on Children with Cerebral Palsy and Its Applications in Health: A Systematic Review. Healthcare, 13(20), 2571. https://doi.org/10.3390/healthcare13202571









