1. Introduction
Osteoarthritis (OA) is a prevalent chronic health condition impacting pain, physical function, mental health, sleep, work participation, and even mortality [
1]. It stands as the costliest condition for privately insured patients in the United States, contributing to over
$6.3 billion in healthcare expenses [
2]. With a projected surge in US adults with arthritis expected to reach 78 million by 2040 [
3], the economic burden on individuals and the healthcare system is poised to escalate, given that OA is the most prevalent form of arthritis [
4].
Primary THAis the gold standard for treating end-stage hip osteoarthritis, providing relief from pain and improved joint function [
5]. Its transformative journey began with the first total hip replacement by Wiles in 1938, evolving significantly with Sir John Charnley’s “low-friction arthroplasty” in the 1960s [
6,
7]. Recognized as “the operation of the century” [
7], THA is considered a safe and effective intervention, despite potential side effects such as infection, dislocation, and pulmonary embolism. Inpatient mortality, the most serious complication, has been documented in up to 3.9% of patients after THA [
8,
9]. While historical literature reports death rates ranging from 0.1 to 0.8% [
10], a significant decline can be attributed to technological advancements and improved preoperative treatment [
11,
12].
This study delves into the national database, exploring variables influencing inpatient mortality rates after hip arthroplasty. The research aims to highlight key findings regarding mortality rates, comorbidities, costs, and other critical parameters, providing valuable insights for the understanding and enhancement of this pivotal surgical intervention. Importantly, our investigation utilizes a more recent dataset (2016–2019) with the ICD-10 coding system, enhancing the relevance and accuracy of our findings compared to an earlier study that employed older data and the ICD-9 coding system [
13].
Research Questions
What are the key predictors of inpatient mortality following primary total hip arthroplasty, and how do comorbidities, surgical delays, and hospital factors influence mortality rates, costs, and length of stay?
2. Methods
Our study utilized the National Inpatient Sample (NIS) dataset from 2016 to 2019, the largest all-payer inpatient database in the world. This dataset provides a comprehensive and nationally representative overview of U.S. hospital admissions across various states. Notably, this is the most recent pre-COVID-19 version of the NIS, ensuring that our findings are not confounded by the significant healthcare system disruptions caused by the pandemic.
2.1. Data Processing and Cohort Refinement
The raw NIS dataset was systematically filtered to include hospitalizations with ICD-10 procedure codes corresponding to primary total hip arthroplasty. Non-elective, trauma-related, and revision procedures were excluded to ensure a purely elective primary THA cohort. Records with missing or implausible demographic data were also removed. After applying these refinement steps, the final analytic sample comprised 327,123 cases, corresponding to 1,635,615 weighted patient discharges. Age was categorized as <64, 65–79, and ≥80 years to reflect commonly used clinical and health-system thresholds (younger adults, Medicare-age patients, and octogenarians who carry disproportionate perioperative risk).
2.2. Definition of Mortality
Inpatient mortality was defined as death occurring during the index hospitalization, based on the NIS variable DIED (coded 1 = died before discharge, 0 = survived). This definition is consistent with prior studies using NIS for perioperative outcomes research [
13].
2.3. Variables Collected
The dataset included detailed information on demographics, comorbidities, hospital characteristics, and inpatient complications classified by ICD-10 codes. Comorbidities were identified using the Charlson Comorbidity Index and individual ICD-10 diagnostic codes. Hospital characteristics included teaching status, bed size, and geographic region. Socioeconomic status was approximated using income quartile data provided in the NIS. Admission day (weekday vs. weekend) and surgical delay (≥1 calendar day from admission to procedure) were derived from standard NIS fields and treated as categorical exposure variables.
2.4. Statistical Analysis
Statistical analyses were performed using SPSS Statistics (version 28) and MATLAB (R2021a). Descriptive statistics summarized patient demographics, comorbidities, and hospital characteristics. Chi-square tests were used for categorical variables, and logistic regression was employed to calculate odds ratios for inpatient mortality. Statistical significance was set at p < 0.01. Cost analyses evaluated mean hospitalization costs across comorbidity and complication groups, while length of stay (LOS) was analyzed using ANOVA to assess differences between patient subgroups.
3. Results
The study analyzed data from a total of 1,635,615 inpatient THA and found an overall mortality rate of 0.04%. As shown in
Table 1, the analysis revealed several statistically significant associations between THA preoperative variables and inpatient mortality. The overall mortality rate was 0.04%. It is noteworthy that the mortality rate increased significantly by 0.15% in patients over 80 years of age. Similarly, the mortality rate for weekend stays was as high as 0.10%. A delay of 1 day or more between admission and surgery was associated with a 0.17% higher mortality rate. Regarding income, the lowest income quartile (0–25%) had a statistically significant mortality rate of 0.06%. In contrast, gender and hospital region did not have a statistically significant effect on inpatient mortality.
Table 2 underscores significant associations between variables and comorbidities with inpatient mortality risk in THApatients. Key findings reveal heightened mortality rates for chronic kidney disease (0.21%) and heart failure (0.30%). Conversely, hypertension (0.02%) is associated with a lower mortality risk compared to the control group (0.06%).
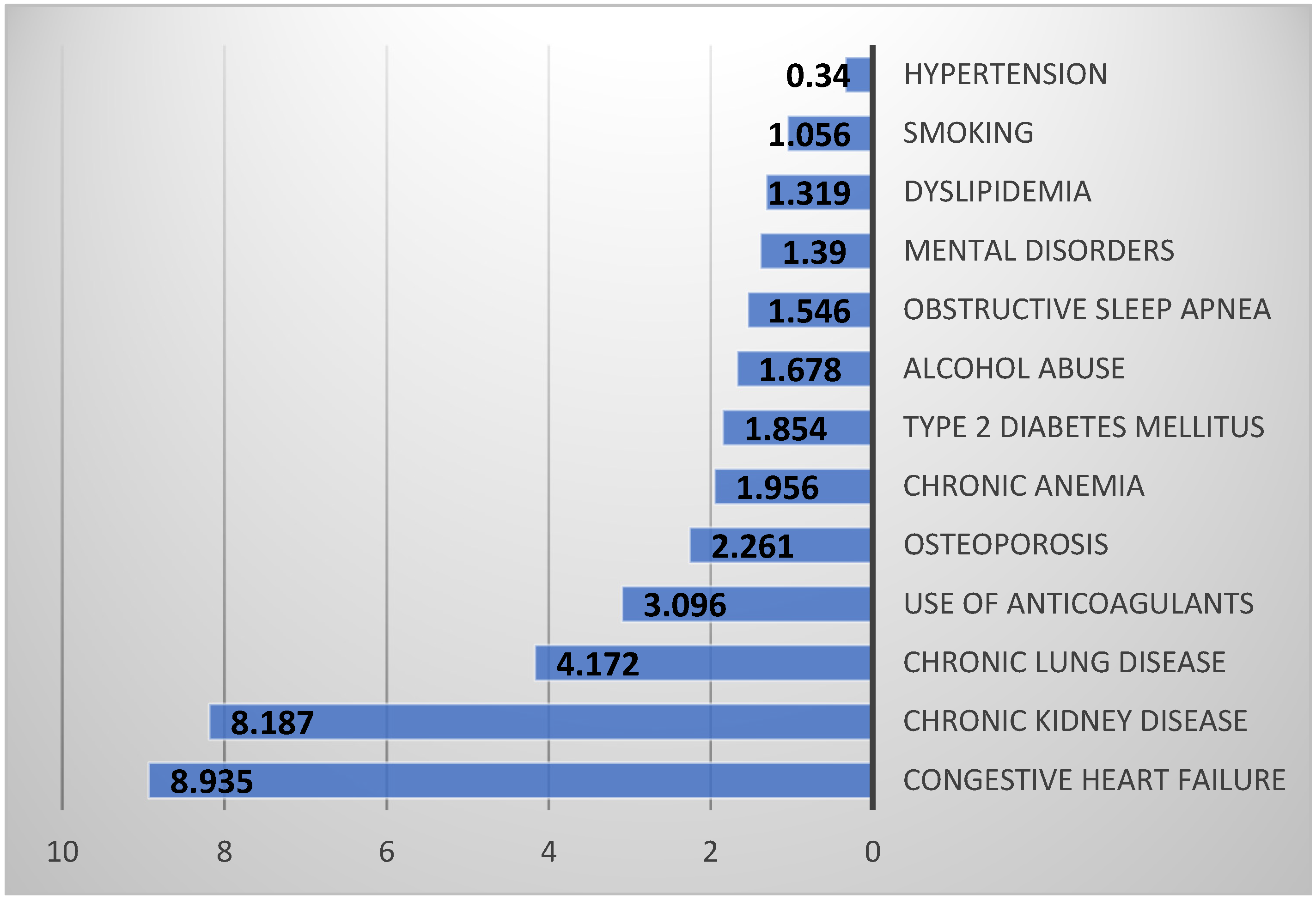
Figure 1 displays significant odds ratios for inpatient mortality in primary THA patients, highlighting the relative risks associated with each diagnostic factor. Notably, congestive heart failure and chronic kidney disease present substantially higher odds ratios of 8.935 and 8.187, indicating a significantly increased risk of inpatient mortality.
Hypertension exhibits an odds ratio of 0.34, suggesting a potential association with lower inpatient mortality risk.
Table 3 provides insights into mortality rates segmented by All Patient Refined Diagnosis-Related Group (APR-DRG) Risk Subclasses in elective THA. APR-DRG Risk Subclasses categorize patients based on the predicted risk of mortality, enabling a more nuanced understanding of outcomes. For patients categorized under “Extreme likelihood of dying,” a high mortality rate of 75.40% was recorded, in stark contrast to other risk subclasses. The differences in mortality rates across these APR-DRG Risk Subclasses were statistically significant.
Table 4 outlines hospital complications in elective THA patients, emphasizing diagnostic factors like acute renal failure, exsanguination anemia, and pulmonary embolism, along with their associated mortality rates. For instance, acute renal failure occurred in 1.78% of patients, with a 0.91% mortality rate. Blood loss anemia affected 17.94% of patients, with a 0.11% mortality rate. Although pulmonary embolism is rare (0.08% occurrence), it carries a notably high mortality rate of 3.46%. Statistically significant differences in mortality rates are evident for each inpatient complication type.
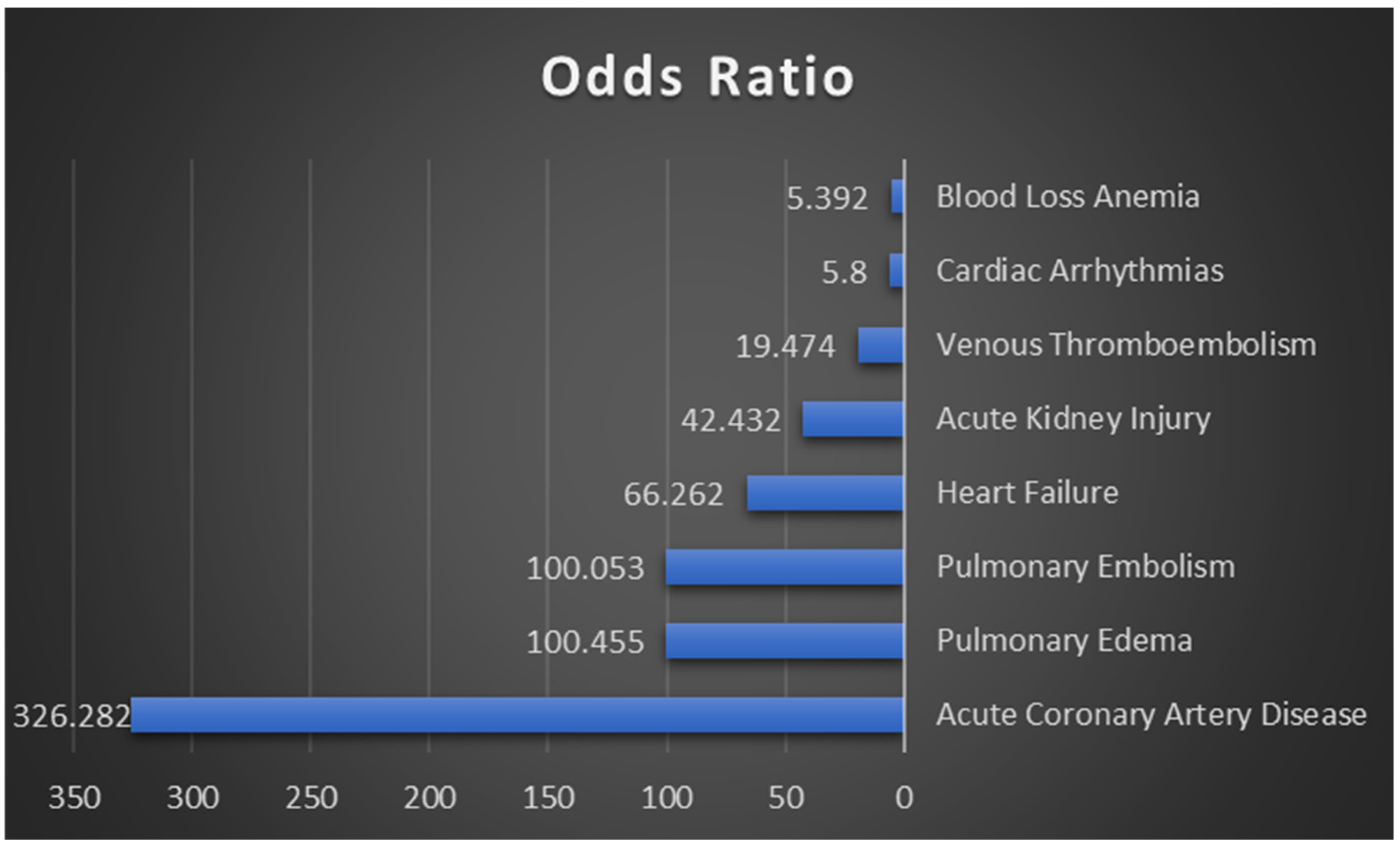
Figure 2 depicts odds ratios for inpatient mortality in primary THA patients, emphasizing diagnostic factors. Acute Coronary Artery Disease exhibits the highest odds ratio at 326.282, indicating an exceptionally high likelihood of mortality. Other significant factors include Pulmonary Edema, Pulmonary Embolism, Heart Failure, and Acute Kidney Injury.
Table 5 reveals the influence of comorbidities, complications, and age on average costs for elective THA patients. For instance, acute coronary artery disease substantially raises the average cost from
$63,603.94 to
$140,793.58. Similarly, patients with heart failure incur an average cost of
$132,671.84 compared to
$63,605.86 for those without heart failure. The presence of pulmonary embolism and pulmonary edema is also associated with notably higher average costs. Age contributes to cost variation, with patients aged 80 and older incurring an average cost of
$66,180.77, surpassing other age groups.
As evidenced by
Table 6, the average length of stay in the hospital varied significantly across age categories for patients undergoing elective Total Hip Arthroplasty (THA). Patients aged over 80 had a statistically significant longer average stay of 2.68 days, compared to 2.02 days for those aged 65–79 and 1.9 days for patients under 64.
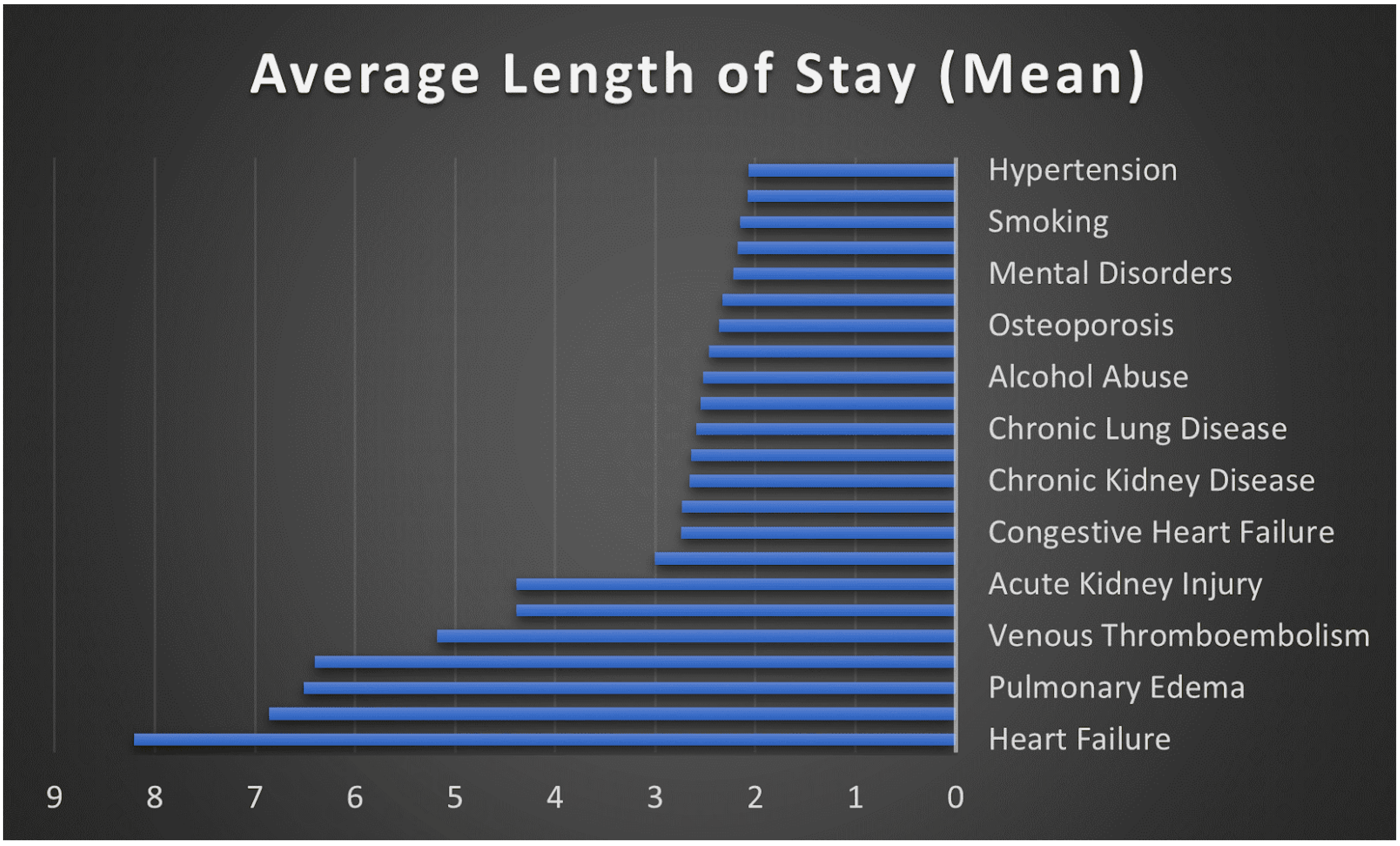
Figure 3 elucidates the statistically significant relationship between various comorbidities and complications and the average length of stay in days for patients undergoing elective THA. Notably, conditions such as acute renal failure and heart failure markedly increased the length of stay to 4.39 and 8.21 days, respectively. Similarly, acute complications like pulmonary embolism resulted in an average stay of 6.86 days.
5. Conclusions
Using the largest pre-COVID nationwide cohort of elective THA cases, we found that inpatient mortality, while rare (0.04%), is concentrated among octogenarians and patients with CHF or CKD. System-level factors such as weekend admission and surgical delay ≥ 1 day were associated with markedly higher risk, identifying actionable targets for process improvement. Complications—including pulmonary embolism, heart failure, and acute coronary events—were not only linked to mortality but also drove substantial increases in cost and length of stay. These findings provide a contemporary baseline for perioperative risk stratification and underscore the economic benefit of preventing complications. Future research should integrate longitudinal follow-up and rehabilitation data to capture the full spectrum of outcomes after THA and guide more comprehensive quality-improvement strategies.