Activity Intensity and All-Cause Mortality Following Fall Injury Among Older Adults: Results from a 12-Year National Survey
Abstract
1. Introduction
2. Methods
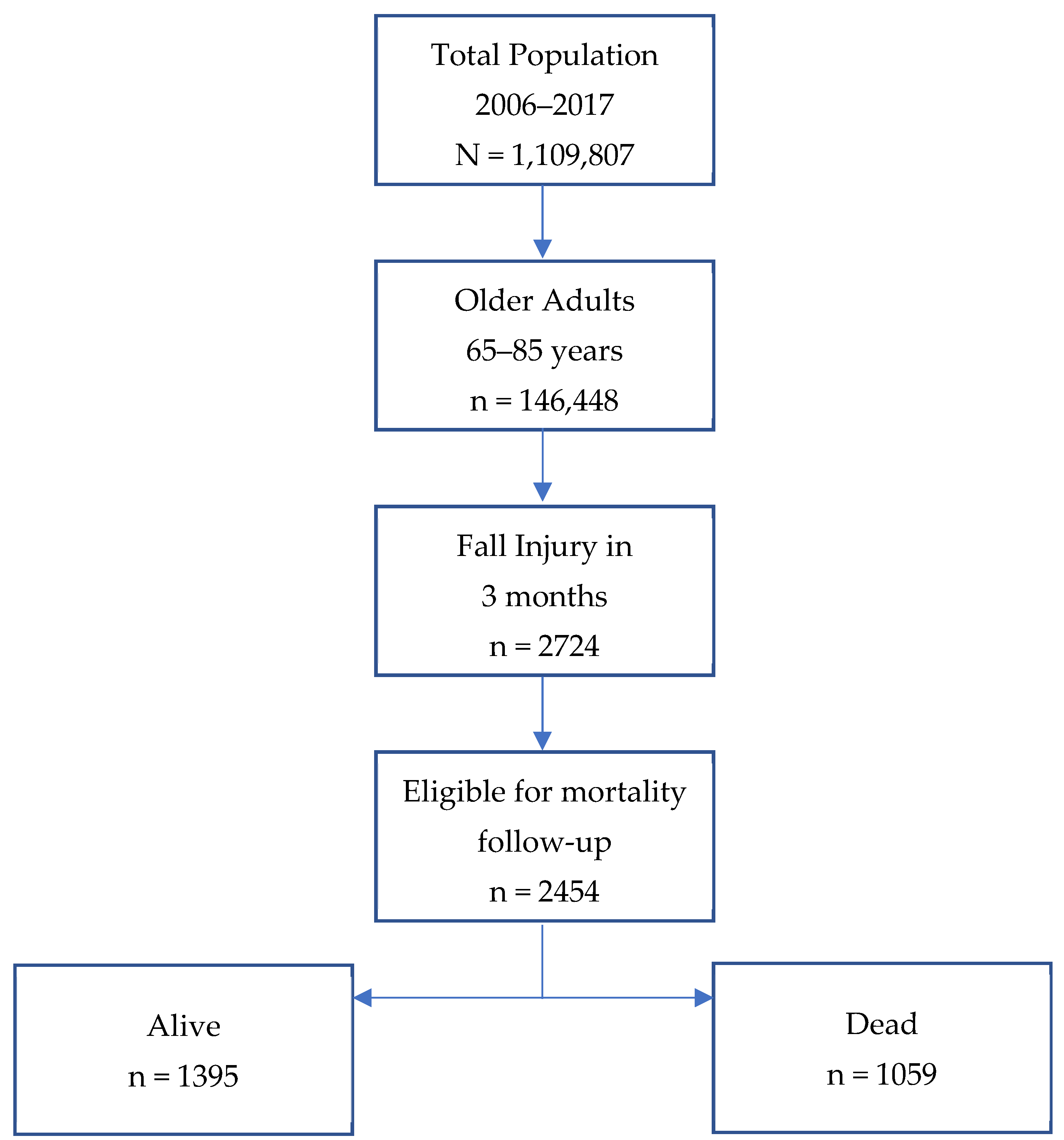
2.1. Study Population
2.2. Inclusion and Exclusion Criteria
2.3. Outcome Variable
2.4. Predictor Variable
2.5. Potential Confounders
2.6. Handling of Missing Data
2.7. Data Analysis
2.8. Ethical Concerns
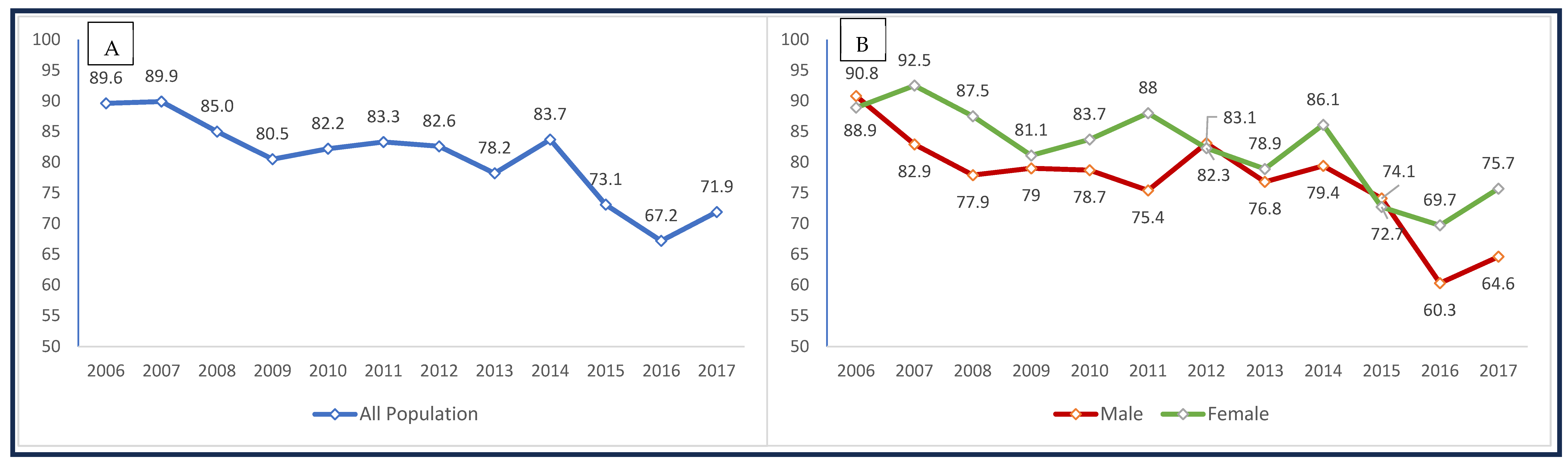
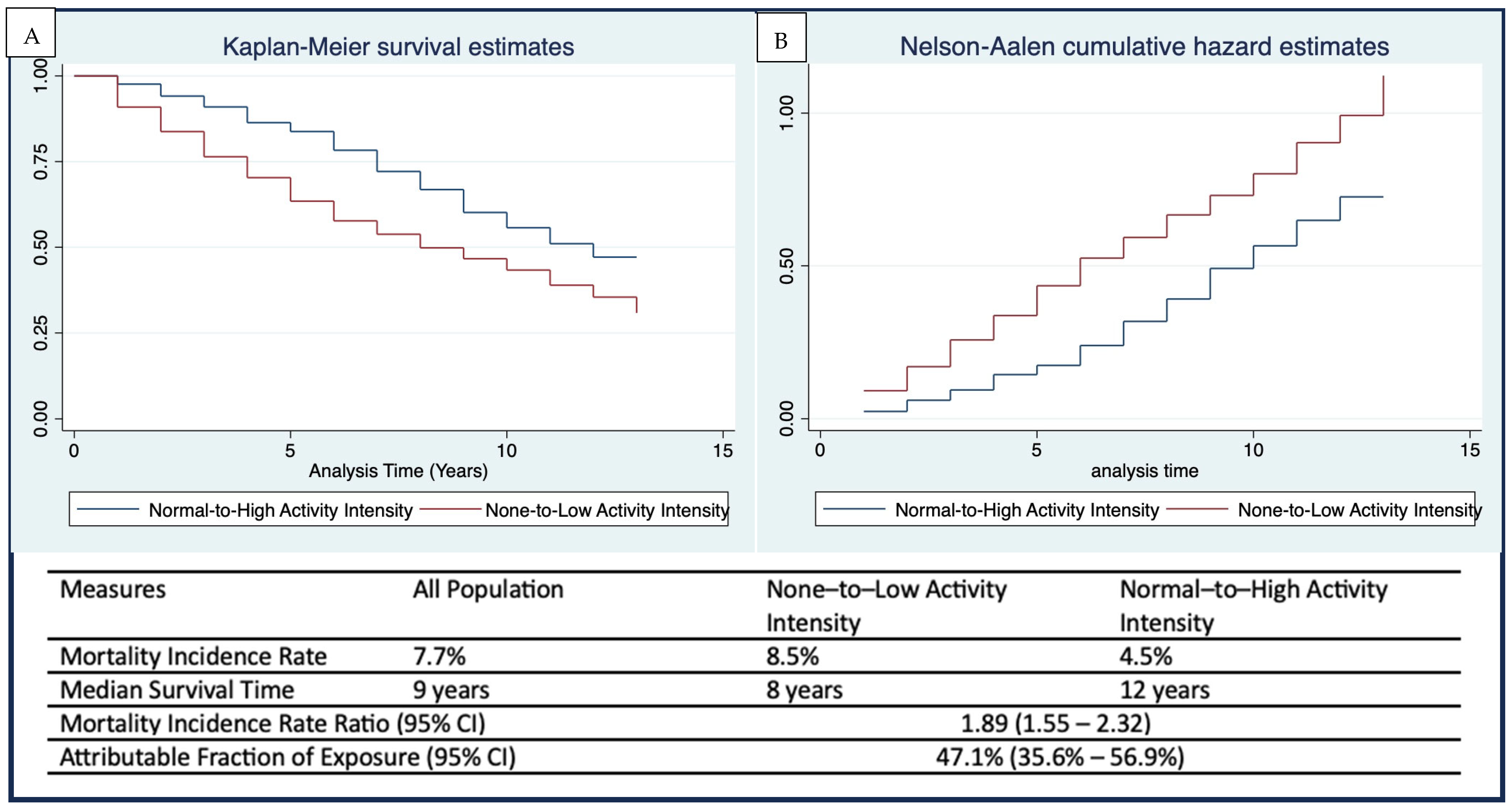
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MET | Metabolic Equivalent of Task |
| IPUMS | Integrated Public Use Microdata Series |
| NHIS | National Health Interview Survey |
| IRR | Incidence Rate Ratio |
| HR | Hazard Ratio |
| CI | Confidence Interval |
| US | United States |
References
- Centers for Disease Control and Prevention. Older Adult Falls Data. Available online: https://www.cdc.gov/falls/data-research/index.html (accessed on 5 October 2025).
- Fuller, G.F. Falls in the elderly. Am. Fam. Physician 2000, 61, 2159–2168, 2173–2174. [Google Scholar]
- Centers for Disease Control and Prevention. Facts About Falls. Available online: https://www.cdc.gov/falls/data-research/facts-stats/index.html (accessed on 5 October 2025).
- Centers for Disease Control and Prevention. About Older Adult Fall Prevention. Available online: https://www.cdc.gov/falls/about/index.html (accessed on 5 October 2025).
- Crane, M.A.; Lam, A.; Christmas, C.; Gemmill, A.; Romley, J.A. Epidemiology of mortality attributed to falls in older adults in the US, 1999–2020. J. Am. Geriatr. Soc. 2024, 72, 303–307. [Google Scholar] [CrossRef]
- Sadaqa, M.; Németh, Z.; Makai, A.; Prémusz, V.; Hock, M. Effectiveness of exercise interventions on fall prevention in ambulatory community-dwelling older adults: A systematic review with narrative synthesis. Front. Public Health 2023, 11, 1209319. [Google Scholar] [CrossRef]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.M.; Lamb, S.E. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2012, 2012, Cd007146. [Google Scholar] [CrossRef]
- Paillard, T.; Lafont, C.; Costes-Salon, M.C.; Rivière, D.; Dupui, P. Effects of brisk walking on static and dynamic balance, locomotion, body composition, and aerobic capacity in ageing healthy active men. Int. J. Sports Med. 2004, 25, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Palvanen, M.; Kannus, P.; Piirtola, M.; Niemi, S.; Parkkari, J.; Järvinen, M. Effectiveness of the Chaos Falls Clinic in preventing falls and injuries of home-dwelling older adults: A randomised controlled trial. Injury 2014, 45, 265–271. [Google Scholar] [CrossRef] [PubMed]
- National Institute on Aging. Falls and Fractures in Older Adults: Causes and Prevention. Available online: https://www.nia.nih.gov/health/falls-and-falls-prevention/falls-and-fractures-older-adults-causes-and-prevention (accessed on 15 November 2024).
- Sherrington, C.; Fairhall, N.J.; Wallbank, G.K.; Tiedemann, A.; Michaleff, Z.A.; Howard, K.; Clemson, L.; Hopewell, S.; Lamb, S.E. Exercise for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2019, 1, Cd012424. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; van der Velde, N.; Martin, F.C.; Petrovic, M.; Tan, M.P.; Ryg, J.; Aguilar-Navarro, S.; Alexander, N.B.; Becker, C.; Blain, H.; et al. World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing 2022, 51, afac205. [Google Scholar] [CrossRef] [PubMed]
- Avola, M.; Mangano, G.R.A.; Testa, G. Rehabilitation strategies for patients with femoral neck fractures in sarcopenia: A narrative review. J. Clin. Med. 2020, 9, 3115. [Google Scholar] [CrossRef]
- Meléndez-Ortega, A. Osteoporosis, falls and exercise. Eur. Rev. Aging Phys. Act. 2007, 4, 61–70. [Google Scholar] [CrossRef][Green Version]
- Benedetti, M.G.; Furlini, G.; Zati, A.; Letizia Mauro, G. The Effectiveness of Physical Exercise on Bone Density in Osteoporotic Patients. Biomed. Res. Int. 2018, 2018, 4840531. [Google Scholar] [CrossRef]
- Cauley, J.A.; Giangregorio, L. Physical activity and skeletal health in adults. Lancet Diabetes Endocrinol. 2020, 8, 150–162. [Google Scholar] [CrossRef]
- Greenwood-Hickman, M.A.; Rosenberg, D.E.; Phelan, E.A.; Fitzpatrick, A.L. Participation in Older Adult Physical Activity Programs and Risk for Falls Requiring Medical Care, Washington State, 2005–2011. Prev. Chronic Dis. 2015, 12, E90. [Google Scholar] [CrossRef]
- Sherrington, C.; Michaleff, Z.A.; Fairhall, N.; Paul, S.S.; Tiedemann, A.; Whitney, J.; Cumming, R.G.; Herbert, R.D.; Close, J.C.T.; Lord, S.R. Exercise to prevent falls in older adults: An updated systematic review and meta-analysis. Br. J. Sports Med. 2017, 51, 1750–1758. [Google Scholar] [CrossRef]
- Papalia, G.F.; Papalia, R.; Diaz Balzani, L.A.; Torre, G.; Zampogna, B.; Vasta, S.; Fossati, C.; Alifano, A.M.; Denaro, V. The Effects of Physical Exercise on Balance and Prevention of Falls in Older People: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 2595. [Google Scholar] [CrossRef] [PubMed]
- Thompson, P.D.; Arena, R.; Riebe, D.; Pescatello, L.S. ACSM’s New Preparticipation Health Screening Recommendations from ACSM’s Guidelines for Exercise Testing and Prescription, Ninth Edition. Curr. Sports Med. Rep. 2013, 12, 215–217. [Google Scholar] [CrossRef]
- Blewett, L.A.; Drew, J.A.R.; King, M.L.; Williams, K. IPUMS Health Surveys: National Health Interview Survey, Version 6.4 [NHIS]; IPUMS: Minneapolis, MN, USA, 2019. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. About the National Health Interview Survey. Available online: https://www.cdc.gov/nchs/nhis/about/index.html (accessed on 5 October 2025).
- National Center for Health Statistics. National Health Interview Survey. Available online: https://ftp.cdc.gov/pub/Health_Statistics/nchs/Dataset_Documentation/NHIS/2018/ (accessed on 14 March 2020).
- Integrated Public Use Microdata Series. IRCAUSE. Available online: https://nhis.ipums.org/nhis-action/variables/IRCAUSE#description_section (accessed on 16 November 2024).
- National Center for Health Statistics. NCHS Data Linked to NDI Mortality Files. Available online: https://www.cdc.gov/nchs/data-linkage/mortality.htm (accessed on 5 October 2022).
- Wu, S.; Fisher-Hoch, S.P.; Reininger, B.; McCormick, J.B. Recommended Levels of Physical Activity Are Associated with Reduced Risk of the Metabolic Syndrome in Mexican-Americans. PLoS ONE 2016, 11, e0152896. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Physical Activity Questionnaire (GPAQ) Analysis Guide; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Jeong, S.W.; Kim, S.H.; Kang, S.H.; Kim, H.J.; Yoon, C.H.; Youn, T.J.; Chae, I.H. Mortality reduction with physical activity in patients with and without cardiovascular disease. Eur. Heart J. 2019, 40, 3547–3555. [Google Scholar] [CrossRef]
- Jetté, M.; Sidney, K.; Blümchen, G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin. Cardiol. 1990, 13, 555–565. [Google Scholar] [CrossRef] [PubMed]
- Althubaiti, A. Information bias in health research: Definition, pitfalls, and adjustment methods. J. Multidiscip. Healthc. 2016, 9, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Little, R.J. A test of missing completely at random for multivariate data with missing values. J. Am. Stat. Assoc. 1988, 83, 1198–1202. [Google Scholar] [CrossRef]
- Azur, M.J.; Stuart, E.A.; Frangakis, C.; Leaf, P.J. Multiple imputation by chained equations: What is it and how does it work? Int. J. Methods Psychiatr. Res. 2011, 20, 40–49. [Google Scholar] [CrossRef]
- McNeish, D. Exploratory Factor Analysis With Small Samples and Missing Data. J. Pers. Assess. 2017, 99, 637–652. [Google Scholar] [CrossRef]
- Dray, S.; Josse, J. Principal component analysis with missing values: A comparative survey of methods. Plant Ecol. 2015, 216, 657–667. [Google Scholar] [CrossRef]
- Blewett, L.A.; Drew, J.A.R.; King, M.L.; Williams, C.W.K. User Note—Sampling Weights. Available online: https://nhis.ipums.org/nhis/userNotes_weights.shtml (accessed on 12 August 2020).
- Botman, S.L.; Jack, S.S. Combining National Health Interview Survey Datasets: Issues and approaches. Stat. Med. 1995, 14, 669–677. [Google Scholar] [CrossRef]
- SAS Institute Inc. SAS 9.4, version 9.4; SAS Institute Inc.: Cary, NC, USA, 2019.
- StataCorp. Stata Statistical Software, Release 16; StataCorp LLC: College Station, TX, USA, 2017.
- IPUMS Health Surveys. Frequently Asked Questions (FAQ): Data Limitations and Cautions to Users. Available online: https://nhis.ipums.org/nhis-action/faq#:~:text=Because%20the%20NHIS%20data%20are,these%20data%20for%20genealogical%20research. (accessed on 12 April 2021).
- Office of Sponsored Programs. Does Your Research Involving Secondary or Existing Data, Documents or Biological Specimens Require Review by the NYU IRB Office? 2025. Available online: https://www.nyu.edu/content/dam/nyu/research/documents/IRB/IRBDecisionTree.pdf (accessed on 5 October 2025).
- Appeadu, M.K.; Bordoni, B. Falls and Fall Prevention in the Elderly; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Thomas, E.; Battaglia, G.; Patti, A.; Brusa, J.; Leonardi, V.; Palma, A.; Bellafiore, M. Physical activity programs for balance and fall prevention in elderly: A systematic review. Medicine 2019, 98, e16218. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Y.-J.; Meng, Q.; Su, C.-H. Mechanism-Driven Strategies for Reducing Fall Risk in the Elderly: A Multidisciplinary Review of Exercise Interventions. Healthcare 2024, 12, 2394. [Google Scholar] [CrossRef]
- Zhou, J.; Tang, R.; Wang, X.; Ma, H.; Li, X.; Heianza, Y.; Qi, L. Frailty Status, Sedentary Behaviors, and Risk of Incident Bone Fractures. J. Gerontol. A Biol. Sci. Med. Sci. 2024, 79, glae186. [Google Scholar] [CrossRef]
- Berg, R.L.; Cassells, J.S. Falls in older persons: Risk factors and prevention. In The Second Fifty Years: Promoting Health and Preventing Disability; National Academies Press: Washington, DC, USA, 1992. [Google Scholar]
- Anderson, E.; Durstine, J.L. Physical activity, exercise, and chronic diseases: A brief review. Sports Med. Health Sci. 2019, 1, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of exercise is a major cause of chronic diseases. Compr. Physiol. 2012, 2, 1143–1211. [Google Scholar] [CrossRef] [PubMed]
- Warburton, D.E.; Nicol, C.W.; Bredin, S.S. Health benefits of physical activity: The evidence. CMAJ 2006, 174, 801–809. [Google Scholar] [CrossRef]
- Crews, R.T.; Yalla, S.V.; Fleischer, A.E.; Wu, S.C. A growing troubling triad: Diabetes, aging, and falls. J. Aging Res. 2013, 2013, 342650. [Google Scholar] [CrossRef]
- Neri, S.G.R.; Oliveira, J.S.; Dario, A.B.; Lima, R.M.; Tiedemann, A. Does Obesity Increase the Risk and Severity of Falls in People Aged 60 Years and Older? A Systematic Review and Meta-analysis of Observational Studies. J. Gerontol. A Biol. Sci. Med. Sci. 2020, 75, 952–960. [Google Scholar] [CrossRef]
- Ylitalo, K.R.; Karvonen-Gutierrez, C.A. Body mass index, falls, and injurious falls among U.S. adults: Findings from the 2014 Behavioral Risk Factor Surveillance System. Prev. Med. 2016, 91, 217–223. [Google Scholar] [CrossRef]
- Bourke, R.; Doody, P.; Pérez, S.; Moloney, D.; Lipsitz, L.A.; Kenny, R.A. Cardiovascular Disorders and Falls Among Older Adults: A Systematic Review and Meta-Analysis. J. Gerontol. A Biol. Sci. Med. Sci. 2024, 79, glad221. [Google Scholar] [CrossRef]
- Alessy, S.A.; Malkin, J.D.; Finkelstein, E.A.; AlAhmed, R.; Baattaiah, B.A.; Evenson, K.R.; Rakic, S.; Cetinkaya, V.; Herbst, C.H.; Al-Hazzaa, H.M.; et al. Effectiveness of Interventions Promoting Physical Activity and Reducing Sedentary Behavior in Community-Dwelling Older Adults: An Umbrella Review With Application to Saudi Arabia. J. Epidemiol. Glob. Health 2023, 13, 361–373. [Google Scholar] [CrossRef]
- Di Pumpo, M.; Miatton, A.; Riccardi, M.T.; Graps, E.A.; Baldo, V.; Buja, A.; Damiani, G. Digital Health Interventions to Promote Physical Activity in Community-Dwelling Older Adults: A Systematic Review and Semiquantitative Analysis. Int. J. Public Health 2025, 69, 1607720. [Google Scholar] [CrossRef]
- McMahon, S.K.; Lewis, B.A.; Guan, W.; Wyman, J.F.; Rothman, A.J. Community-based intervention effects on older adults’ physical activity and falls: Protocol and rationale for a randomized optimization trial (Ready Steady3.0). Contemp. Clin. Trials 2021, 101, 106238. [Google Scholar] [CrossRef] [PubMed]
- Meredith, S.J.; Cox, N.J.; Ibrahim, K.; Higson, J.; McNiff, J.; Mitchell, S.; Rutherford, M.; Wijayendran, A.; Shenkin, S.D.; Kilgour, A.H.M.; et al. Factors that influence older adults’ participation in physical activity: A systematic review of qualitative studies. Age Ageing 2023, 52, afad145. [Google Scholar] [CrossRef] [PubMed]
- Tappen, R.; Vieira, E.R.; Gropper, S.S.; Newman, D.; Horne, C. Sustaining or Declining Physical Activity: Reports from an Ethnically Diverse Sample of Older Adults. Geriatrics 2021, 6, 57. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans Midcourse Report: Implementation Strategies for Older Adults; Department of Health and Human Services: Washington, DC, USA, 2023.
- Gupta, R.; Vaqar, S. National guidelines for physical activity. In StatPearls [Internet]; StatPearls: Treasure Island, FL, USA, 2022. [Google Scholar]
- Barnett, D.W.; Barnett, A.; Nathan, A.; Van Cauwenberg, J.; Cerin, E. Built environmental correlates of older adults’ total physical activity and walking: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 103. [Google Scholar] [CrossRef]
- Portegijs, E.; Lee, C.; Zhu, X. Activity-friendly environments for active aging: The physical, social, and technology environments. Front. Public Health 2022, 10, 1080148. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention; National Center for Health Statistics. Participation in Leisure-Time aerobic and Muscle-Strengthening Activities That Meet the Federal 2008 Physical Activity Guidelines for Americans Among Adults Aged 18 and Over, by Selected Characteristics: United States, Selected Years 1998–2018; CDC: Atlanta, GA, USA, 2019.
- Tivity Health. Silver Sneakers. Available online: https://tools.silversneakers.com/ (accessed on 5 October 2025).
- de Almeida, S.I.L.; Gomes da Silva, M.; Marques, A. Home-Based Physical Activity Programs for People With Dementia: Systematic Review and Meta-Analysis. Gerontologist 2020, 60, 600–608. [Google Scholar] [CrossRef] [PubMed]
- Whiteley, S. Total Survey Error & Institutional Research: A Case Study of the University Experience Survey. In Proceedings of the 2014 Australasian Association for Institutional Research (AAIR) Forum, Melbourne, Australia, 19–21 November 2014. [Google Scholar]
- Elixhauser, A.; Steiner, C.; Harris, D.R.; Coffey, R.M. Comorbidity measures for use with administrative data. Med. Care 1998, 36, 8–27. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- IPUMS Health Surveys. 2018 NHIS Questionnaire—Sample Adult. Available online: https://nhis.ipums.org/nhis-action/source_documents/survey_form_ih2018_sa_tag.xml (accessed on 17 August 2025).
| Variable | All Population Unweighted Count (Weighted %) N = 2454 | None-to-Low Activity Unweighted Count (Weighted %) n = 1990 (80.8) | Normal-to-High Activity Unweighted Count (Weighted %) n = 464 (19.2) | p-Value |
|---|---|---|---|---|
| Mean Age (95% CI) | 76.6 (76.3, 76.9) | 77.0 (77.6, 77.4) | 74.9 (74.2, 75.7) | |
| Age Category | ||||
| 65–74 years | 1026 (41.1) | 772 (38.7) | 254 (51.5) | <0.001 |
| 75–84 years | 851 (34.7) | 710 (35.2) | 141 (32.3) | |
| 85 years and older | 577 (24.2) | 508 (26.1) | 69 (16.2) | |
| Sex | ||||
| Male | 784 (31.6) | 609 (30.2) | 175 (37.2) | 0.012 |
| Female | 1670 (68.4) | 1381 (69.8) | 289 (62.8) | |
| Race/Ethnicity | ||||
| Non-Hispanic White | 1962 (85.2) | 1581 (85.2) | 381 (85.3) | 0.929 |
| Non-Hispanic Black | 200 (6.4) | 169 (6.5) | 31 (5.9) | |
| Hispanic | 173 (5.0) | 145 (5.0) | 28 (5.2) | |
| Other Races | 119 (3.3) | 95 (3.2) | 24 (3.7) | |
| Born in the US | ||||
| Yes | 2196 (90.8) | 1781 (90.8) | 415 (90.8) | 0.998 |
| No | 258 (9.2) | 209 (9.2) | 49 (9.2) | |
| Educational Attainment | ||||
| High school or less | 1302 (52.1) | 1126 (55.8) | 176 (36.4) | <0.001 |
| Some college or AA | 640 (26.0) | 491 (24.4) | 149 (32.6) | |
| Bachelor’s degree | 296 (12.8) | 219 (11.9) | 77 (16.6) | |
| Postgraduate | 216 (9.1) | 154 (7.9) | 62 (14.4) | |
| Marital Status | ||||
| Single | 104 (4.5) | 83 (4.1) | 21 (6.0) | 0.034 |
| Married | 994 (41.0) | 807 (41.2) | 187 (40.1) | |
| Divorced | 359 (13.8) | 273 (12.9) | 86 (17.8) | |
| Widowed | 997 (40.7) | 827 (41.8) | 170 (36.0) | |
| Poverty Level | ||||
| Poor | 2186 (90.9) | 1760 (90.8) | 426 (91.4) | 0.676 |
| Not Poor | 268 (9.1) | 230 (9.2) | 38 (8.6) | |
| Smoking Status | ||||
| Never Smoked | 1613 (65.8) | 1389 (69.9) | 224 (48.4) | <0.001 |
| Current Smoker | 155 (6.2) | 123 (6.0) | 32 (6.9) | |
| Former Smoker | 686 (28.0) | 478 (24.1) | 208 (44.7) | |
| No Available Care | ||||
| Yes | 27 (1.1) | 21 (1.0) | 6 (1.3) | 0.675 |
| No | 2427 (98.9) | 1969 (99.0) | 458 (98.7) | |
| No Accessible Care | ||||
| Yes | 124 (5.1) | 85 (4.4) | 39 (7.8) | 0.011 |
| No | 2330 (94.9) | 1905 (95.6) | 425 (92.2) | |
| No Affordable Care | ||||
| Yes | 98 (3.9) | 82 (4.1) | 16 (3.0) | 0.352 |
| No | 2356 (96.1) | 1908 (95.6) | 448 (97.0) | |
| Health Coverage | ||||
| Yes | 6 (0.2) | 5 (0.2) | 1 (0.4) | 0.393 |
| No | 2448 (99.8) | 1985 (99.8) | 463 (99.6) | |
| Activity Limitations | ||||
| Yes | 1625 (65.2) | 1420 (70.3) | 205 (43.6) | <0.001 |
| No | 829 (34.8) | 570 (29.7) | 259 (56.4) | |
| Index of chronic disease | ||||
| None | 820 (33.9) | 781 (40.0) | 39 (7.7) | <0.001 |
| 1–2 | 762 (31.1) | 522 (25.6) | 240 (54.4) | |
| 3–4 | 663 (26.6) | 512 (25.9) | 151 (29.8) | |
| 5 or more | 209 (8.4) | 175 (8.5) | 34 (8.1) | |
| Repeat Fall Injury | ||||
| Yes | 136 (5.6) | 122 (6.2) | 14 (3.0) | 0.020 |
| No | 2318 (94.4) | 1868 (93.8) | 450 (97.0) | |
| Self-rated health | ||||
| Poor | 391 (15.7) | 375 (18.3) | 16 (4.6) | <0.001 |
| Fair | 604 (24.3) | 534 (26.6) | 70 (14.8) | |
| Good to Excellent | 1459 (60.0) | 1081 (55.1) | 378 (80.6) | |
| Mortality Status | ||||
| Dead | 1059 (45.3) | 941 (50.0) | 118 (25.4) | <0.001 |
| Alive | 1395 (54.7) | 1049 (50.0) | 346 (74.6) |
| Variable | Dead Unweighted Count (Weighted %) | Alive Unweighted Count (Weighted %) | p-Value * |
|---|---|---|---|
| Mean Age (95% CI) | 79.5 (79.0, 79.9) | 74.2 (73.8, 74.6) | |
| Age Category | |||
| 65–74 years | 259 (23.4) | 767 (55.9) | <0.001 |
| 75–84 years | 401 (37.5) | 450 (32.3) | |
| 85 years and older | 399 (39.1) | 178 (11.8) | |
| Sex | |||
| Male | 411 (36.7) | 373 (27.7) | <0.001 |
| Female | 648 (63.3) | 1022 (72.7) | |
| Race/Ethnicity | |||
| Non-Hispanic White | 871 (87.6) | 1091 (83.3) | 0.023 |
| Non-Hispanic Black | 80 (0.1) | 120 (0.1) | |
| Hispanic | 68 (0.0) | 105 (0.1) | |
| Other Races | 40 (0.0) | 79 (0.0) | |
| Born in the US | |||
| Yes | 976 (93.3) | 1220 (88.8) | <0.001 |
| No | 83 (6.7) | 175 (11.2) | |
| Educational Attainment | |||
| High school or less | 622 (58.7) | 680 (46.7) | 0.011 |
| Some college or AA | 239 (22.5) | 401 (28.8) | |
| Bachelor’s degree | 120 (11.9) | 176 (13.5) | |
| Postgraduate | 78 (6.9) | 138 (11.0) | |
| Marital Status | |||
| Single | 38 (4.1) | 66 (4.8) | <0.001 |
| Married | 403 (37.6) | 591 (43.8) | |
| Divorced | 113 (9.7) | 246 (17.3) | |
| Widowed | 505 (48.6) | 492 (34.1) | |
| Poverty Level | |||
| Poor | 107 (8.3) | 161 (9.8) | 0.179 |
| Not Poor | 952 (91.7) | 1234 (90.2) | |
| Smoking Status | |||
| Never Smoked | 687 (66.1) | 926 (65.5) | 0.002 |
| Current Smoker | 79 (6.8) | 76 (5.7) | |
| Former Smoker | 293 (27.1) | 393 (28.8) | |
| No Available Care | |||
| Yes | 13 (1.2) | 14 (1.0) | 0.477 |
| No | 1046 (98.8) | 1381 (99.0) | |
| No Accessible Care | |||
| Yes | 51 (4.9) | 73 (5.3) | 0.581 |
| No | 1008 (95.1) | 1322 (94.7) | |
| No Affordable Care | |||
| Yes | 39 (3.6) | 59 (4.2) | 0.333 |
| No | 1020 (96.4) | 1336 (95.8) | |
| No Health Coverage | |||
| Yes | 1 (0.1) | 5 (0.3) | 0.127 |
| No | 1058 (99.9) | 1390 (99.7) | |
| Activity Limitations | |||
| Yes | 868 (81.4) | 757 (51.8) | <0.001 |
| No | 191 (18.6) | 638 (48.2) | |
| Index of chronic disease | |||
| None | 376 (35.8) | 444 (32.2) | <0.001 |
| 1–2 | 277 (27.1) | 485 (34.5) | |
| 3–4 | 292 (27.0) | 371 (26.3) | |
| 5 or more | 114 (10.1) | 95 (7.0) | |
| Repeat Fall Injury | |||
| Yes | 71 (7.0) | 65 (4.4) | 0.004 |
| No | 988 (93.0) | 1330 (95.6) | |
| Self-rated health | |||
| Poor | 258 (24.4) | 133 (8.5) | <0.001 |
| Fair | 304 (28.1) | 300 (21.1) | |
| Good to Excellent | 497 (47.5) | 962 (70.4) | |
| Activity intensity | |||
| None-to-Low | 941 (89.3) | 1049 (73.9) | <0.001 |
| Normal-to-High | 118 (10.7) | 346 (26.1) |
| Variable | Unadjusted Hazard Risk Ratio (95% CI) | Adjusted Hazard Risk Ratio (95% CI) |
|---|---|---|
| Activity Intensity | ||
| None-to-Low | 1.99 (1.62–2.44) | 1.50 (1.20–1.87) |
| Normal-to-High | Ref | Ref |
| Age Category | ||
| 65–74 years | Ref | Ref |
| 75–84 years | 2.30 (1.94–2.74) | 2.16 (1.81–2.58) |
| 85 years and older | 4.53 (3.77–5.44) | 4.06 (3.33–4.95) |
| Sex | ||
| Male | Ref | Ref |
| Female | 0.74 (0.64–0.86) | 0.64 (0.54–0.75) |
| Race/Ethnicity | ||
| Non-Hispanic White | Ref | Ref |
| Non-Hispanic Black | 0.93 (0.72–1.19) | 0.82 (0.66–1.09) |
| Hispanic | 0.73 (0.55–0.97) | 0.84 (0.70–1.16) |
| Other Races | 0.65 (0.43–0.97) | 0.61 (0.40–0.94) |
| Born in the US | ||
| Yes | 1.76 (1.31–2.37) | 1.76 (1.29–2.41) |
| No | Ref | Ref |
| Educational Attainment | ||
| High school or less | Ref | Ref |
| Some college or AA | 1.20 (0.86–1.67) | 1.35 (1.00–1.83) |
| Bachelor’s degree | 1.10 (0.81–1.48) | 1.08 (0.81–1.44) |
| Postgraduate | 1.40 (1.08–1.83) | 1.16 (0.90–1.51) |
| Marital Status | ||
| Single | Ref | Ref |
| Married | 0.84 (0.56–1.25) | 0.86 (0.57–1.31) |
| Divorced | 0.71 (0.46–1.09) | 0.75 (0.48–1.18) |
| Widowed | 1.34 (0.84–1.86) | 0.88 (0.58–1.34) |
| Poverty Level | ||
| Poor | 0.91 (0.73–1.12) | 0.82 (0.64–1.05) |
| Not Poor | Ref | Ref |
| Smoking Status | ||
| Never Smoked | Ref | Ref |
| Current Smoker | 1.34 (1.04–1.72) | 1.50 (1.13–1.99) |
| Former Smoker | 1.05 (0.90–1.23) | 1.10 (0.92–1.32) |
| No Available Care | ||
| Yes | 1.09 (0.68–1.76) | 0.71 (0.33–1.54) |
| No | Ref | Ref |
| No Accessible Care | ||
| Yes | 1.07 (0.78–1.46) | 1.08 (0.78–1.50) |
| No | Ref | Ref |
| No Affordable Care | ||
| Yes | 0.84 (0.61–1.17) | 0.82 (0.56–1.20) |
| No | Ref | Ref |
| No Health Coverage | ||
| Yes | 0.17 (0.02–1.34) | 0.32 (0.04–2.79) |
| No | Ref | Ref |
| Activity Limitations | ||
| Yes | 3.03 (2.56–3.59) | 2.00 (1.66–2.41) |
| No | Ref | Ref |
| Index of chronic disease | ||
| None | Ref | Ref |
| 1–2 | 0.97 (0.82–1.14) | 1.06 (0.88–1.29) |
| 3–4 | 1.22 (1.03–1.45) | 1.05 (0.85–1.29) |
| 5 or more | 1.67 (1.34–2.09) | 1.47 (1.13–1.91) |
| Repeat Fall Injury | ||
| Yes | 1.59 (1.25–2.03) | 0.95 (0.71–1.27) |
| No | Ref | Ref |
| Self-rated health | ||
| Poor | 2.67 (2.24–3.19) | 2.07 (1.68–2.54) |
| Fair | 1.74 (1.49–2.03) | 1.41 (1.19–1.68) |
| Good to Excellent | Ref | Ref |
| Variable | Unweighted Count (Weighted %) | Unadjusted Hazard Risk Ratio (95% CI) | Adjusted Hazard Risk Ratio (95% CI) |
|---|---|---|---|
| Activity Intensity | |||
| None | 1732 (70.3) | 2.01 (1.63–2.47) | 1.46 (1.15–1.83) |
| Low | 258 (10.6) | 1.85 (1.41–2.41) | 1.69 (1.29–2.22) |
| Normal-to-High | 464 (19.1) | Ref | Ref |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adeyemi, O.; Chippendale, T.; Ogedegbe, O.; Boatright, D.; Chodosh, J. Activity Intensity and All-Cause Mortality Following Fall Injury Among Older Adults: Results from a 12-Year National Survey. Healthcare 2025, 13, 2530. https://doi.org/10.3390/healthcare13192530
Adeyemi O, Chippendale T, Ogedegbe O, Boatright D, Chodosh J. Activity Intensity and All-Cause Mortality Following Fall Injury Among Older Adults: Results from a 12-Year National Survey. Healthcare. 2025; 13(19):2530. https://doi.org/10.3390/healthcare13192530
Chicago/Turabian StyleAdeyemi, Oluwaseun, Tracy Chippendale, Olugbenga Ogedegbe, Dowin Boatright, and Joshua Chodosh. 2025. "Activity Intensity and All-Cause Mortality Following Fall Injury Among Older Adults: Results from a 12-Year National Survey" Healthcare 13, no. 19: 2530. https://doi.org/10.3390/healthcare13192530
APA StyleAdeyemi, O., Chippendale, T., Ogedegbe, O., Boatright, D., & Chodosh, J. (2025). Activity Intensity and All-Cause Mortality Following Fall Injury Among Older Adults: Results from a 12-Year National Survey. Healthcare, 13(19), 2530. https://doi.org/10.3390/healthcare13192530






