Gait-Based Screening for Cognitive Impairment in Older Adults: A Fast and Objective Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Recruitment
2.2. Cognitive Function Assessment
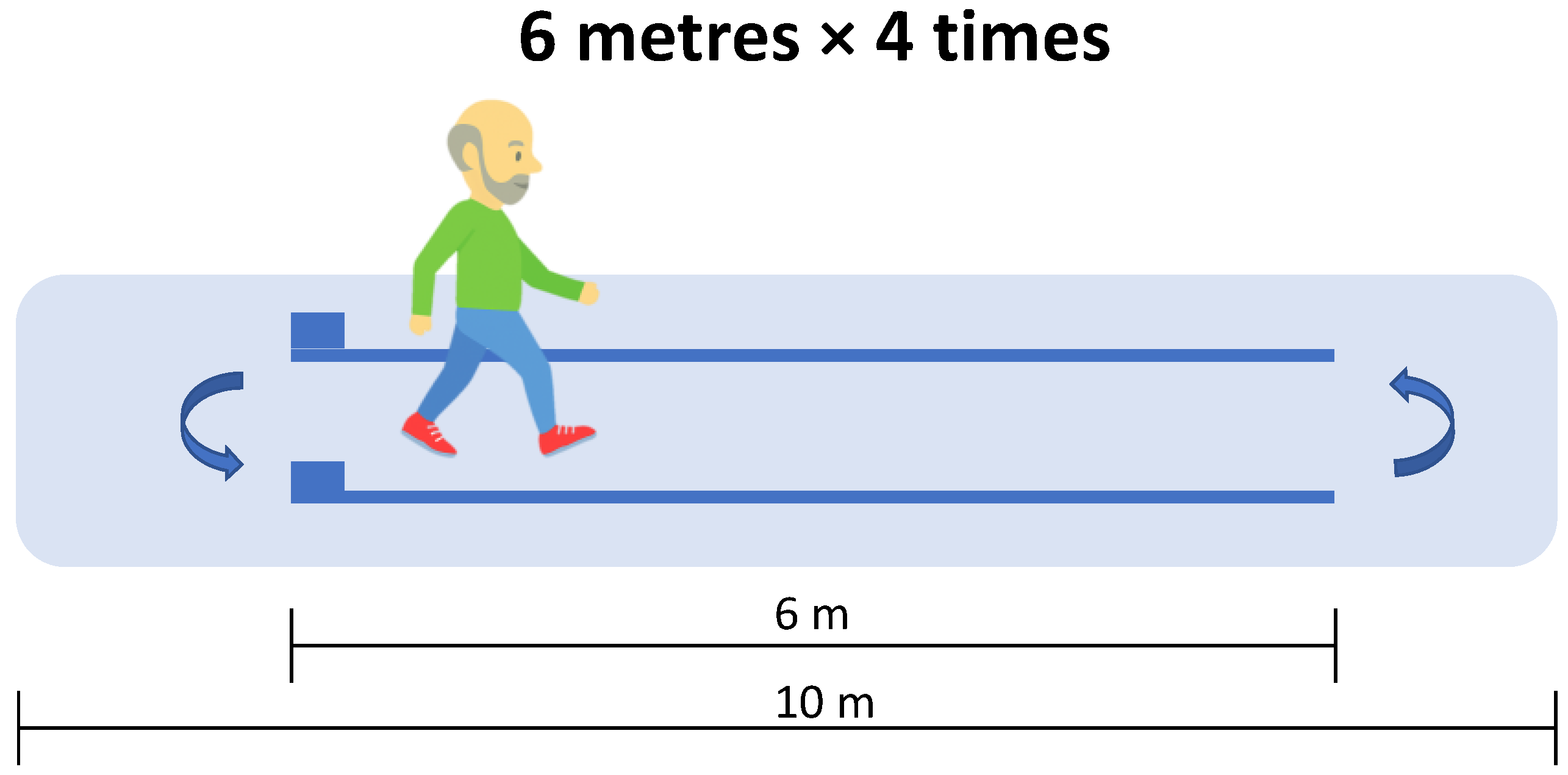
2.3. Gait Analysis
2.4. Statistical Analysis
3. Results
3.1. Descriptive Data
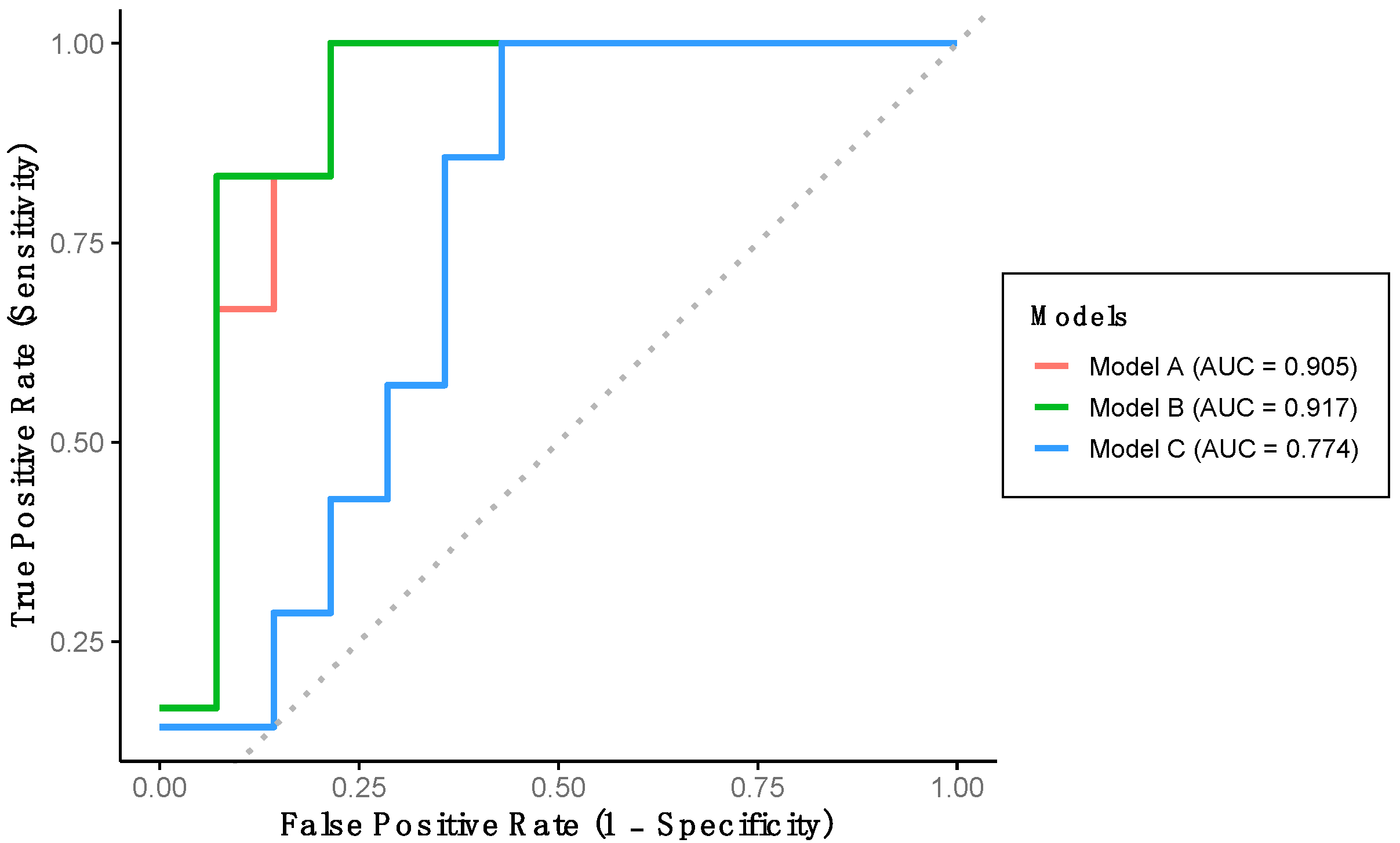
3.2. Algorithm Development Through Logistic Regression Models
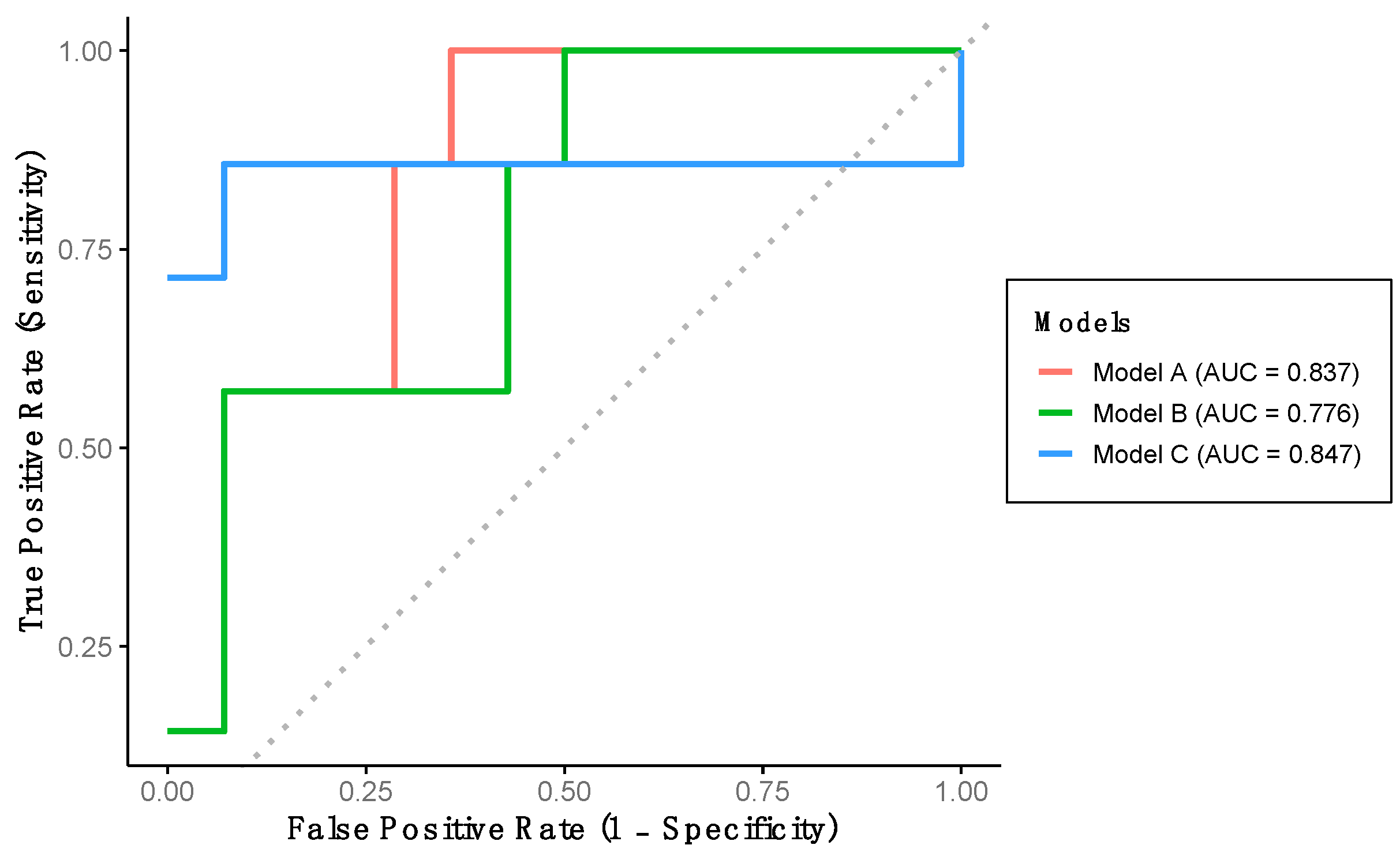
3.3. Validation of Classification Models Using an Independent Dataset
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Abbreviation | Meaning |
| AD | Alzheimer’s disease |
| AUC-ROC | Area under the receiver operating characteristic curve |
| CDT | Clock drawing test |
| HCF | High cognitive function |
| IQ | Informant questionnaire |
| IMUs | Inertial measurement units |
| LCF | Low cognitive function |
| MCI | Mild cognitive impairment |
| MMSE | Mini-Mental state examination |
| MoCA | Montreal cognitive assessment |
| SD | Standard deviation |
References
- Ismail, Z.; Ahmad, W.I.W.; Hamjah, S.H.; Astina, I.K. The Impact of Population Ageing: A Review. Iran. J. Public Health 2021, 50, 2451–2460. [Google Scholar] [CrossRef]
- World Health Organization. The UN Decade of Healthy Ageing 2021–2030 in a Climate-Changing World; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Gaspar-Silva, F.; Trigo, D.; Magalhaes, J. Ageing in the Brain: Mechanisms and Rejuvenating Strategies. Cell. Mol. Life Sci. 2023, 80, 190. [Google Scholar] [CrossRef]
- Tony Wyss, C. Ageing, Neurodegeneration and Brain Rejuvenation. Nature 2016, 10, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Murman, D.L. The Impact of Age on Cognition. Semin. Hear. 2015, 36, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Gjøra, L.; Strand, B.H.; Bergh, S.; Borza, T.; Brækhus, A.; Engedal, K.; Johannessen, A.; Kvello-Alme, M.; Krokstad, S.; Livingston, G.; et al. Current and Future Prevalence Estimates of Mild Cognitive Impairment, Dementia, and Its Subtypes in a Population-Based Sample of People 70 Years and Older in Norway: The HUNT Study. J. Alzheimer’s Dis. 2021, 79, 1213–1226. [Google Scholar] [CrossRef]
- Galvin, J.E. Screening for Mild Cognitive Impairment: There Is the Will but Is There a Way? J. Prev. Alzheimer’s Dis. 2020, 7, 144–145. [Google Scholar] [CrossRef]
- Sabbagh, M.N.; Boada, M.; Borson, S.; Chilukuri, M.; Dubois, B.; Ingram, J.; Iwata, A.; Porsteinsson, A.P.; Possin, K.L.; Rabinovici, G.D.; et al. Early Detection of Mild Cognitive Impairment (MCI) in Primary Care. J. Prev. Alzheimer’s Dis. 2020, 7, 165–170. [Google Scholar] [CrossRef]
- Arevalo-Rodriguez, I.; Smailagic, N.; Roqué-Figuls, M.; Ciapponi, A.; Sanchez-Perez, E.; Giannakou, A.; Pedraza, O.L.; Bonfill Cosp, X.; Cullum, S. Mini-Mental State Examination (MMSE) for the Early Detection of Dementia in People with Mild Cognitive Impairment (MCI). Cochrane Database Syst. Rev. 2021, 2021, CD010783. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Strategy on Human Resources for Health: Workforce 2030; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Sabbagh, M.N.; Boada, M.; Borson, S.; Doraiswamy, P.M.; Dubois, B.; Ingram, J.; Iwata, A.; Porsteinsson, A.P.; Possin, K.L.; Rabinovici, G.D.; et al. Early Detection of Mild Cognitive Impairment (MCI) in an At-Home Setting. J. Prev. Alzheimer’s Dis. 2020, 7, 171–178. [Google Scholar] [CrossRef]
- Zhao, H.; Cao, J.; Xie, J.; Liao, W.H.; Lei, Y.; Cao, H.; Qu, Q.; Bowen, C. Wearable Sensors and Features for Diagnosis of Neurodegenerative Diseases: A Systematic Review. Digit. Health 2023, 9, 20552076231173569. [Google Scholar] [CrossRef]
- Zhao, H.; Wang, R.; Qi, D.; Xie, J.; Cao, J.; Liao, W.H. Wearable Gait Monitoring for Diagnosis of Neurodegenerative Diseases. Measurement 2022, 202, 111839. [Google Scholar] [CrossRef]
- Piau, A.; Wild, K.; Mattek, N.; Kaye, J. Current State of Digital Biomarker Technologies for Real-Life, Home-Based Monitoring of Cognitive Function for Mild Cognitive Impairment to Mild Alzheimer Disease and Implications for Clinical Care: Systematic Review. J. Med. Internet Res. 2019, 21, e12785. [Google Scholar] [CrossRef] [PubMed]
- Jehu, D.A.; Langston, R.; Sams, R.; Young, L.; Hamrick, M.; Zhu, H.; Dong, Y. The Impact of Dual-Tasks and Disease Severity on Posture, Gait, and Functional Mobility among People Living with Dementia in Residential Care Facilities: A Pilot Study. Sensors 2024, 24, 2691. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Ha, S.W.; Jeong, D.E.; Lee, J.; Kim, D.; Min, J.Y.; Min, K.B. Association Between the Loss of Gait Harmony and Cognitive Impairment: Cross-Sectional Study. JMIR Public Health Surveill. 2023, 9, e46264. [Google Scholar] [CrossRef]
- Jeong, Y.; Kang, J.; Kim, B.C.; Lee, K.H.; Song, J.-I.; Gwak, J. Early Alzheimer’s Disease Diagnosis Using Wearable Sensors and Multilevel Gait Assessment: A Machine Learning Ensemble Approach. IEEE Sens. J. 2023, 23, 10041–10053. [Google Scholar] [CrossRef]
- Jung, S.; Michaud, M.; Oudre, L.; Dorveaux, E.; Gorintin, L.; Vayatis, N.; Ricard, D. The Use of Inertial Measurement Units for the Study of Free Living Environment Activity Assessment: A Literature Review. Sensors 2020, 20, 5625. [Google Scholar] [CrossRef]
- Rudisch, J.; Jöllenbeck, T.; Vogt, L.; Cordes, T.; Klotzbier, T.J.; Vogel, O.; Wollesen, B. Agreement and Consistency of Five Different Clinical Gait Analysis Systems in the Assessment of Spatiotemporal Gait Parameters. Gait Posture 2021, 85, 55–64. [Google Scholar] [CrossRef]
- Fritz, S.; Lusardi, M. Walking Speed: The Sixth Vital Sign. J. Geriatr. Phys. Ther. 2009, 32, 2–5. [Google Scholar] [CrossRef]
- Skillbäck, T.; Blennow, K.; Zetterberg, H.; Skoog, J.; Rydén, L.; Wetterberg, H.; Guo, X.; Sacuiu, S.; Mielke, M.M.; Zettergren, A.; et al. Slowing Gait Speed Precedes Cognitive Decline by Several Years. Alzheimer’s Dement. 2022, 18, 1667–1676. [Google Scholar] [CrossRef]
- Abellan Van Kan, G.; Rolland, Y.; Andrieu, S.; Bauer, J.; Beauchet, O.; Bonnefoy, M.; Cesari, M.; Donini, L.M.; Gillette-Guyonnet, S.; Inzitari, M.; et al. Gait Speed at Usual Pace as a Predictor of Adverse Outcomes in Community-Dwelling Older People an International Academy on Nutrition and Aging (IANA) Task Force. J. Nutr. Health Aging 2009, 13, 881–889. [Google Scholar] [CrossRef]
- Kim, S.W.; Kim, D.H.; Hong, J.Y.; Mun, K.R.; Jung, D.; Hong, I.; Mc Ardle, R.; Seong, J.K.; Baek, M.S. Gait Impairment Associated with Neuroimaging Biomarkers in Alzheimer’s Disease. Sci. Rep. 2025, 15, 5539. [Google Scholar] [CrossRef]
- Verghese, J.; Mahoney, J.R.; Ayers, E.; Ambrose, A.; Wang, C.; Holtzer, R. Computerised Cognitive Remediation to Enhance Mobility in Older Adults: A Single-Blind, Single-Centre, Randomised Trial. Lancet Healthy Longev. 2021, 2, e571–e579. [Google Scholar] [CrossRef]
- Marusic, U.; Verghese, J.; Mahoney, J.R. Does Cognitive Training Improve Mobility, Enhance Cognition, and Promote Neural Activation? Front. Aging Neurosci. 2022, 14, 845825. [Google Scholar] [CrossRef] [PubMed]
- Lobo, A.; Saz, P.; Marcos, G.; Día, J.; De-la-Cámara, C.; Ventura, T.; Morales-Asín, F.; Fernando-Pascual, L.; Montañés, J.; Aznar, S. Revalidation and Standardization of the Cognition Mini-Exam (First Spanish Version of the Mini-Mental Status Examination) in the General Geriatric Population. Med. Clin. 1999, 112, 767–774. [Google Scholar]
- Lienhard, K.; Schneider, D.; Maffiuletti, N.A. Validity of the Optogait Photoelectric System for the Assessment of Spatiotemporal Gait Parameters. Med. Eng. Phys. 2013, 35, 500–504. [Google Scholar] [CrossRef]
- Mandrekar, J.N. Receiver Operating Characteristic Curve in Diagnostic Test Assessment. J. Thorac. Oncol. 2010, 5, 1315–1316. [Google Scholar] [CrossRef]
- May Peel, N.; John Alapatt, L.; Vanessa Jones, L.; Eleanor Hubbard, R. The Association between Gait Speed and Cognitive Status in Community-Dwelling Older People: A Systematic Review and Meta-Analysis. J. Gerontol. A Biol. Sci. Med. Sci. 2019, 74, 943–948. [Google Scholar] [CrossRef]
- Tomita, Y.; Tanaka, S.; Takahashi, S.; Takeuchi, N. Detecting Cognitive Decline in Community-Dwelling Older Adults Using Simple Cognitive and Motor Performance Tests. Geriatr. Gerontol. Int. 2020, 20, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Wu, J.; Tian, Q.; Liu, X.; Yu, W.; Lu, Y. Gait Speed as a Superior Screening Indicator for Mild Cognitive Impairment Compared to Walk Ratio and Dual-Task Cost: A Cross-Sectional Study. Eur. Geriatr. Med. 2025, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kostic, E.; Kwak, K.; Kim, D. Changes in Sensory, Postural Stability and Gait Functions Depending on Cognitive Decline, and Possible Markers for Detection of Cognitive Status. BMC Med. Inform. Decis. Mak. 2022, 22, 252. [Google Scholar] [CrossRef]
- LaRoche, D.P.; Greenleaf, B.L.; Croce, R.V.; McGaughy, J.A. Interaction of Age, Cognitive Function, and Gait Performance in 50-80-Year-Olds. Age 2014, 36, 9693. [Google Scholar] [CrossRef]
- Savica, R.; Wennberg, A.M.V.; Hagen, C.; Edwards, K.; Roberts, R.O.; Hollman, J.H.; Knopman, D.S.; Boeve, B.F.; Machulda, M.M.; Petersen, R.C.; et al. Comparison of Gait Parameters for Predicting Cognitive Decline: The Mayo Clinic Study of Aging. J. Alzheimer’s Dis. 2017, 55, 559–567. [Google Scholar] [CrossRef]
- O’Caoimh, R.; Timmons, S.; Molloy, D.W. Screening for Mild Cognitive Impairment: Comparison of “MCI Specific” Screening Instruments. J. Alzheimer’s Dis. 2016, 51, 619–629. [Google Scholar] [CrossRef]
- Lorente Aznar, T.; Olivera Pueyo, F.J.; Benabarre Ciria, S.; Rodríguez Torrente, M.; Solans Aisa, B.; Giménez Baratech, A.C. Diagnostic Yield of Cognitive Tests Applied in Primary Care. Consistency and Validity of Screening Tests. Aten. Primaria 2010, 42, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Drake, M.; Butman, J.; Fontan, L.; Lorenzo, J.; Harris, P.; Allegri, R.F.; Ollari, J.A. [Screening for Mild Cognitive Impairment: Usefulness of the 7-Minute Screen Test]. Actas Esp. Psiquiatr. 2003, 31, 252–255. [Google Scholar] [PubMed]
- Villarejo, A.; Puertas-Martín, V. Usefulness of Short Tests in Dementia Screening. Neurol. (Engl. Ed.) 2011, 26, 425–433. [Google Scholar] [CrossRef]
- Biel, M.; Grondys, K.; Androniceanu, A.M. A Crisis in the Health System and Quality of Healthcare in Economically Developed Countries. Int. J. Environ. Res. Public Health 2022, 20, 469. [Google Scholar] [CrossRef]
- Deveugele, M.; Derese, A.; Van Den Brink-Muinen, A.; Bensing, J.; de Maeseneer, J. Consultation Length in General Practice: Cross Sectional Study in Six European Countries. BMJ 2002, 325, 472. [Google Scholar] [CrossRef]
- Cruz-Jimenez, M. Normal Changes in Gait and Mobility Problems in the Elderly. Phys. Med. Rehabil. Clin. N. Am. 2017, 28, 713–725. [Google Scholar] [CrossRef] [PubMed]
- Iwakura, M.; Okura, K.; Shibata, K.; Kawagoshi, A.; Sugawara, K.; Takahashi, H.; Shioya, T.; Wakasa, M. Gait Characteristics and Their Associations with Clinical Outcomes in Patients with Chronic Obstructive Pulmonary Disease. Gait Posture 2019, 74, 60–65. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; Muir, S.W.; Hall, M.; Doherty, T.J.; Kloseck, M.; Beauchet, O.; Speechley, M. Gait Variability Is Associated with Frailty in Community-Dwelling Older Adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2011, 66A, 568–576. [Google Scholar] [CrossRef] [PubMed]
- Blumen, H.M.; Jayakody, O.; Verghese, J. Gait in Cerebral Small Vessel Disease, Pre-Dementia, and Dementia: A Systematic Review. Int. J. Stroke 2023, 18, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Burtscher, J.; Moraud, E.M.; Malatesta, D.; Millet, G.P.; Bally, J.F.; Patoz, A. Exercise and Gait/Movement Analyses in Treatment and Diagnosis of Parkinson’s Disease. Ageing Res. Rev. 2024, 93, 102147. [Google Scholar] [CrossRef] [PubMed]
| Overall | LCF | HCF | Effect Size (95% CI) | p-Value | |
|---|---|---|---|---|---|
| N | 42 | 14 | 28 | ||
| Age, years | 72.38 (8.33) | 78.07 (8.25) | 69.54 (6.88) | −8.54 (−13.40, −3.67) | 0.001 |
| Males, % | 38.1 [16] | 42.9 [6] | 35.7 [10] | 0.74 (0.20, 2.75) | 0.653 |
| Height, cm | 160.21 (8.54) | 156.75 (9.53) | 161.94 (7.60) | 5.19 (−0.29, 10.66) | 0.063 |
| Weight, kg | 68.95 (12.12) | 64.79 (12.20) | 71.04 (11.75) | 6.25 (−1.86, 14.37) | 0.116 |
| MMSE, points | 25.31 (5.82) | 18.50 (5.23) | 28.71 (1.49) | 1.42 (7.16, 13.27) | <0.001 |
| Gait speed, m/s | 1.04 (0.26) | 0.87 (0.25) | 1.13 (0.23) | 0.26 (0.11, 0.41) | 0.002 |
| Cadence, steps/min | 107.77 (17.83) | 105.92 (28.05) | 108.69 (10.05) | 2.77 (−13.75, 19.29) | 0.641 |
| Stride length, cm | 117.61 (21.14) | 102.86 (18.01) | 124.98 (18.79) | 22.11 (9.84, 34.38) | <0.001 |
| Stance time, s | 0.830 (0.300) | 0.968 (0.472) | 0.762 (0.122) | −0.21 (−0.39, −0.02) | 0.034 |
| Stance time, % | 67.30 (6.40) | 69.99 (9.64) | 65.95 (3.44) | −4.04 (−8.12, 0.05) | 0.053 |
| Swing time, s | 0.369 (0.082) | 0.343 (0.127) | 0.381 (0.045) | 0.38 (−0.36, 0.11) | 0.158 |
| Swing time, % | 32.70 (6.41) | 30.02 (9.65) | 34.04 (3.47) | 4.02 (−0.76, 8.12) | 0.054 |
| Single support, s | 0.368 (0.082) | 0.343 (0.126) | 0.381 (0.445) | 0.39 (−0.04, 0.11) | 0.149 |
| Single support, % | 33.66 (5.73) | 31.42 (9.07) | 34.69 (2.92) | 3.27 (−0.52, 7.06) | 0.089 |
| Double support, s | 0.346 (0.076) | 0.360 (0.094) | 0.338 (0.066) | −0.02 (−0.07, 0.03) | 0.394 |
| Double support, % | 30.93 (4.86) | 31.92 (4.82) | 30.47 (4.90) | −1.45 (−4.76, 1.86) | 0.382 |
| Contact phase, s | 0.076 (0.023) | 0.069 (0.023) | 0.080 (0.023) | 0.01 (−0.01, 0.03) | 0.161 |
| Contact phase, % | 9.92 (3.50) | 8.25 (3.46) | 10.76 (3.26) | 2.51 (0.31, 4.71) | 0.027 |
| Foot flat, s | 0.427 (0.107) | 0.414 (0.147) | 0.433 (0.083) | 0.02 (−0.07, 0.11) | 0.595 |
| Foot flat, % | 55.12 (13.91) | 50.32 (20.14) | 57.51 (8.97) | 7.19 (−1.83, 16.22) | 0.115 |
| Propulsive phase, s | 0.330 (0.357) | 0.490 (0.562) | 0.250 (0.147) | −0.24 (−0.47, −0.01) | 0.039 |
| Propulsive phase, % | 34.98 (15.81) | 41.45 (22.80) | 31.75 (9.84) | −9.70 (−19.83, 0.43) | 0.060 |
| Gait ratio | 2.033 (0.434) | 2.160 (0.532) | 1.974 (0.377) | −0.19 (−0.48, 0.11) | 0.205 |
| Overall | TD | VD | Effect Size (95% CI) | p-Value | |
|---|---|---|---|---|---|
| N | 42 | 21 | 21 | ||
| Age, years | 72.38 (8.33) | 70.29 (6.92) | 74.48 (9.22) | 4.19 (−0.89, 9.27) | 0.104 |
| Males, % | 38.1 [16] | 47.6 [10] | 28.6 [6] | 0.44 (0.12, 1.58) | 0.204 |
| Height, cm | 160.21 (8.54) | 160.5 (7.57) | 159.92 (9.60) | −0.57 (−5.97, 4.82) | 0.831 |
| Weight, kg | 68.95 (12.12) | 70.40 (10.38) | 67.50 (13.75) | −2.90 (−10.50, 4.70) | 0.446 |
| MMSE, points | 25.31 (5.82) | 26.05 (4.97) | 24.57 (6.61) | −1.48 (−5.12, 2.17) | 0.418 |
| Gait speed, m/s | 1.04 (0.26) | 1.07 (0.27) | 1.02 (0.26) | −0.05 (−0.22, 0.11) | 0.523 |
| Cadence, steps/min | 107.77 (17.83) | 106.57 (11.53) | 108.96 (22.71) | 2.38 (−8.85, 13.62) | 0.670 |
| Stride length, cm | 117.61 (21.14) | 119.39 (20.20) | 115.83 (22.39) | −3.56 (−16.86, 9.74) | 0.592 |
| Stance time, s | 0.830 (0.300) | 0.778 (0.118) | 0.883 (0.406) | 0.10 (−0.08, 0.29) | 0.264 |
| Stance time, % | 67.30 (6.40) | 66.07 (2.98) | 68.52 (8.48) | 2.46 (−1.51, 6.42) | 0.218 |
| Swing time, s | 0.369 (0.082) | 0.388 (0.032) | 0.349 (0.110) | −0.04 (−0.09, 0.01) | 0.127 |
| Swing time, % | 32.70 (6.41) | 33.93 (3.00) | 31.48 (8.49) | −2.45 (−6.42, 1.52) | 0.219 |
| Single support, s | 0.368 (0.082) | 0.388 (0.031) | 0.349 (0.109) | −0.04 (−0.09, 0.01) | 0.116 |
| Single support, % | 33.66 (5.73) | 34.54 (2.52) | 32.73 (7.78) | −1.82 (−5.44, 1.80) | 0.316 |
| Double support, s | 0.346 (0.076) | 0.354 (0.088) | 0.337 (0.063) | −0.02 (−0.06, 0.03) | 0.485 |
| Double support, % | 30.93 (4.86) | 30.67 (5.02) | 31.20 (4.81) | 0.52 (−2.58, 3.63) | 0.735 |
| Contact phase, s | 0.076 (0.023) | 0.082 (0.024) | 0.070 (0.021) | −0.01 (−0.03, 0.01) | 0.093 |
| Contact phase, % | 9.92 (3.50) | 10.76 (3.28) | 9.09 (3.59) | −1.67 (−3.81, 0.47) | 0.123 |
| Foot flat, s | 0.427 (0.107) | 0.444 (0.100) | 0.410 (0.114) | −0.03 (−0.10, 0.03) | 0.313 |
| Foot flat, % | 55.12 (13.91) | 57.37 (9.53) | 52.87 (17.17) | −4.50 (−13.16, 4.16) | 0.300 |
| Propulsive phase, s | 0.330 (0.357) | 0.252 (0.119) | 0.408 (0.484) | 0.16 (−0.06, 0.38) | 0.160 |
| Propulsive phase, % | 34.98 (15.81) | 31.89 (10.50) | 38.08 (19.55) | 6.20 (−3.59, 15.98) | 0.208 |
| Gait ratio | 2.033 (0.434) | 1.971 (0.285) | 2.098 (0.550) | 0.13 (−0.15, 0.40) | 0.356 |
| AUC-ROC (95% CI) | p-Value | Cut-Off Value | Accuracy | Sensitivity | Specificity | |
|---|---|---|---|---|---|---|
| TRAINING DATA | ||||||
| Model A | 90.5 (77.0, 1.0) | <0.001 | 0.2567 | 85.0% | 71.4% | 92.3% |
| Model B | 91.7 (78.8, 1.0) | <0.001 | 0.2552 | 85.0% | 71.4% | 92.3% |
| Model C | 77.4 (57.0, 97.8) | 0.009 | 0.1925 | 65.0% | 40.0% | 73.3% |
| VERIFICATION DATA | ||||||
| Model A | 83.7 (66.4, 1.0) | <0.001 | - | 81.0% | 57.1% | 92.9% |
| Model B | 77.6 (56.7, 98.4) | 0.010 | - | 81.0% | 57.1% | 92.9% |
| Model C | 84.7 (58.9, 1.0) | 0.008 | - | 66.7% | 85.7% | 57.1% |
| OVERALL DATA | ||||||
| Model A | 86.3 (75.2, 97.4) | <0.001 | - | 80.5% | 76.9% | 82.1% |
| Model B | 84.3 (72.1, 96.5) | <0.001 | - | 82.9% | 76.9% | 85.7% |
| Model C | 81.0 (65.3, 96.8) | <0.001 | - | 70.7% | 92.3% | 60.7% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perez-Lasierra, J.L.; Azpíroz-Puente, M.; Morita-Hernandez, M.; Gómez-Bernal, A.; Alfaro-Santafé, J.-V.; Alfaro-Santafé, J. Gait-Based Screening for Cognitive Impairment in Older Adults: A Fast and Objective Approach. Healthcare 2025, 13, 2450. https://doi.org/10.3390/healthcare13192450
Perez-Lasierra JL, Azpíroz-Puente M, Morita-Hernandez M, Gómez-Bernal A, Alfaro-Santafé J-V, Alfaro-Santafé J. Gait-Based Screening for Cognitive Impairment in Older Adults: A Fast and Objective Approach. Healthcare. 2025; 13(19):2450. https://doi.org/10.3390/healthcare13192450
Chicago/Turabian StylePerez-Lasierra, Jose Luis, Marina Azpíroz-Puente, Martin Morita-Hernandez, Antonio Gómez-Bernal, José-Víctor Alfaro-Santafé, and Javier Alfaro-Santafé. 2025. "Gait-Based Screening for Cognitive Impairment in Older Adults: A Fast and Objective Approach" Healthcare 13, no. 19: 2450. https://doi.org/10.3390/healthcare13192450
APA StylePerez-Lasierra, J. L., Azpíroz-Puente, M., Morita-Hernandez, M., Gómez-Bernal, A., Alfaro-Santafé, J.-V., & Alfaro-Santafé, J. (2025). Gait-Based Screening for Cognitive Impairment in Older Adults: A Fast and Objective Approach. Healthcare, 13(19), 2450. https://doi.org/10.3390/healthcare13192450






